Abstract
Background:
Diagnosis of coronary artery disease (CAD) in early stages is vital in decreasing mortality by reducing the risk factors. The aim of this study was to investigate the association between erectile dysfunction (ED) and CAD.
Methods:
A total of 200 patients were divided into four groups according to their angiography results: Group 1 (G1, n = 59): patients with one-vessel disease (1-VD); Group 2 (G2, n = 40): patients with two-vessel disease (2-VD); Group 3 (G3, n = 50): patients with three-vessel disease (3-VD); and controls (C, n = 51) without any coronary disease. The International Index of Erectile Function (IIEF) was completed for all the patients to assess their sexual function and ED in the last 6 months.
Results:
Mean age of the participants was 57.69 ± 12.466 years. The prevalence of ED in the CAD patients was significantly higher than that of the controls (75.16% vs. 60.8%; p value = 0.041). There was a significant direct correlation between the number of involved vessels in the CAD patients and ED severity (r: 0.183; p value = 0.010), and the ED rate increased with age.
Conclusion:
In conclusion, ED severity correlated with the number of involved vessels documented by coronary angiography. Consequently, ED may be considered a possible marker for the development of atherosclerosis and CAD.
Keywords: Erectile dysfunction, Coronary artery disease, Men, Vascular diseases
Introduction
Coronary artery disease (CAD) is the leading cause of mortality and years of life lost worldwide as well as in Iran.1 In our country, about 46% of deaths are due to cardiovascular diseases and it imposes a high burden on the society.2 Prevention and early diagnosis of CAD could, therefore, decrease the disease morbidity and burden.
Atherosclerosis is a chronic systemic disease that involves cardiac and peripheral arteries and is the leading cause of death and loss of productive life years the world over. Exposure to the known atherosclerosis risk factors begins the process with endothelial dysfunction and leads to intima-media thickening and development of atheromatous plaques, causing vascular lumen stenosis and obstruction.3 These events remain asymptomatic until a critical lumen becomes so stenotic that it cannot supply sufficient blood to the related organ, giving rise to ischemic symptoms. Thus, these processes tend to become symptomatic earlier in small vessels with smaller diameters such as penile vessels and lead to symptoms such as erectile dysfunction (ED). Indeed, CAD and ED may be regarded as the end-organ disease of atherosclerosis in the two organs.3
ED, defined as the inability to achieve and maintain an erection sufficient for satisfactory sexual performance,4 is a frequent disorder affecting over 50% of men aged between 40 and 70 years5 and approximately 322 million men around the globe.5, 6 Moreover, ED is believed to be a manifestation of atherosclerotic vascular disease.5, 7 ED can, therefore, be deemed the primary and early manifestation of subclinical systemic atherosclerotic vascular disorder.3
Patients with CAD are at increased risk for ED as a result of psychological problems primarily or secondary to heart issues and also due to drugs such as beta blockers.8–10 The existence of common risk factors such as obesity, cigarette smoking, hypercholesterolemia, metabolic syndrome, and sedentary lifestyle11–13 and similar pathophysiology4, 14 have strengthened the idea that there is an association between ED and advanced atherosclerotic CAD.7, 9
Up to now, many studies have investigated the relation between CAD and ED and have confirmed this association15–17 while the relation between the severity of ED and the number of occluded coronary arteries in patients with myocardial infarction has been studied by only a few studies.18, 19 Therefore, there is still a gap in our knowledge of this field of science. What is more, no research has been previously done on this issue in Iran.
The aim of this study was to investigate the association between ED and CAD and also between the severity of ED and the number of occluded coronary vessels.
Methods
In this case-control study, 200 male patients referred for coronary angiography to Madani Heart Center in Khorram Abad between February and July 2010 were included. Patients with a history of surgery for pelvic trauma, psychiatric disease, and percutaneous or surgical myocardial revascularization procedures as well as those with unfavorable penile anatomy for sexual act and diseases that could alter sexual activity such as liver cirrhosis, renal failure, thyroid disease, and spinal cord injuries were excluded.
The study was performed in accordance with the Declaration of Helsinki and was approved by the Ethics Committee of Khorram Abad University of Medical Sciences. Written informed consent was obtained from all the participants before enrollment.
A detailed history, including family history of CAD, history of diabetes, smoking, and use of opium, was taken. All the patients underwent complete physical examination and laboratory tests, including lipid profile, fasting glucose, and free-plasma testosterone levels. The definition of each of the CAD risk factors (mentioned above) is presented in Table 1.
Table 1.
Risk factors definition assessed in the study
| Risk factor | Definition |
|---|---|
| Hypertension | Blood pressure > 140/90 mmHg in three consecutive readings, at rest |
| Diabetes | Fasting glucose level > 7.0 mmol/L (> 125 mg/dL) |
| Obesity | Body mass index (BMI) ≥ 30 kg/m2 |
| Family history of CAD | Parents with CAD at age < 55 (father) or < 65 (mother) |
| Smoking | At least ten cigarettes a day |
| Hyperlipidemia | |
| TG > 200 mg/dL | |
| HDL < 25 mg/dL | |
| LDL > 160 mg/dL |
CAD, Coronary artery disease; TG, Triglyceride; HDL, High density lipoprotein; LDL, Low density lipoprotein
ED was evaluated using the erectile function domain of the International index of erectile function-erectile function domain (IIEF-EFD), which includes six questions about sexual activity in the past 6 months. Each question is scored 0 to 5. A score of 26 or less was considered as impairment of erectile function.20 According to the IIEF scores, the patients were diagnosed with mild (score: 17 to 25), moderate (11 to 16), and severe (10 or less) ED. The questionnaires were analyzed in a blinded mode, independently of the results of the coronary endothelial function testing.
Diagnostic coronary angiography was performed in all patients by standard technique. The observers and analyzers were not aware of the results of the patients’ IIEF-EFD questionnaire. Significant angiographic stenosis was defined as > 50% diameter stenosis involving either one major epicardial vessel at any site or any collaterals with > 3 mm diameter. Four groups of patients were considered according to the angiographic results: Group 1 (G1, n = 59): patients with one-vessel disease (1-VD); Group 2 (G2, n = 40): patients with two-vessel disease (2-VD); Group 3 (G3, n = 50): patients with three-vessel disease (3-VD); and controls (C, n = 51) without any significant arterial stenosis.
The prevalence of ED and its risk factors were calculated in the study groups.
For all the statistical analyses, SPSS Software (Statistical Package for Social Sciences, Chicago, IL, USA) version 18 for Windows was used. The categorical data were presented as numbers and percentages and the numerical data by mean and standard deviation. Comparisons between the groups from the aspect of ED prevalence and risk factors were done using the chi-squared test. Also, the Kendall tau rank correlation test was applied, and Gamma coefficient was calculated to find the association between CAD and ED. For the comparison of the numerical data with normal distribution between the two groups, the independent sample t-test was used. The quantitative variables were compared between the CAD groups by the one-way ANOVA if data distribution was normal and by the Kruskal-Wallis if the distribution of data was not normal. As the distribution of the IIEF scores was not normal, the Kruskal-Wallis test was used for the comparison of these data between the four CAD groups. Multiple logistic regression was used for the binomial variables to remove confounding factors such as hypertension, diabetes, hyperlipidemia, cigarette smoking, opium usage, family history, and obesity. Also, univariate analysis of variance was performed. Correlation between CAD and ED severity was assessed using the Spearmen correlation tests. A p value < 0.05 with 95% confidence interval (CI) was considered statistically significant.
Results
In this study, a total of 200 participants, including 149 patients with CAD and 51 controls, were enrolled. The mean age of all the participants was 57.69 ± 12.466 years (range: 35–82). Among all the participants, 25 (12.5%) were obese [body mass index (BMI) ≥ 30 kg/m2]. Table 2 shows the demographic characteristics of the four study groups and all the participants. ED was found in 143 (71.9%) patients in the whole study population. There were no significant differences between the four study groups in terms of CAD risk factors except for age, hypertension, and diabetes. There were no significant differences between the four groups as regards mean BMI and prevalence of smoking, positive family history of CAD, hyperlipidemia, opium addiction, and ED (Table 2). The prevalence of ED increased with an increase in the number of involved vessels, and there was a significant direct correlation between the number of involved vessels in the CAD patients and ED severity (r: 0.183; p value = 0.010). Also, there was a significant inverse correlation between the severity of CAD and the IIEF scores (r: −0.216; p value = 0.002). In addition, the mean IIEF score was significantly lower in the patients with CAD than in those without CAD without considering the number of involved vessels (p value = 0.029). Comparison of the four CAD groups showed a significantly lower mean IIEF score in the patients with a higher number of involved vessels than in those without CAD (p value = 0.013).
Table 2.
Demographic characteristics of the study population*
| Parameters | No CAD (Controls) | CAD Groups | All participants | P value | ||
|---|---|---|---|---|---|---|
| One-vessel disease | Two-vessel disease | Three-vessel disease | ||||
| Age (y) | 53.43±11.53 | 54.97±1.54 | 60.15±1.70 | 63.38±1.83 | 57.69±12.47 | < 0.001 |
| BMI (kg/m2) | 26.53±3.60 | 26.79±4.41 | 26.81±3.12 | 25.56±2.21 | 26.42±3.53 | 0.329 |
| Family history of CAD | 8 (15.7) | 10 (16.9) | 8 (20.0) | 4 (8.0) | 30 (15.0) | 0.407 |
| Opium usage | 8 (15.7) | 20 (33.9) | 16 (40.0) | 16 (32.0) | 60 (30.0) | 0.060 |
| Smoking | 22 (43.1) | 33 (55.9) | 22 (55.0) | 26 (52.0) | 103 (51.5) | 0.553 |
| Diabetes | 4 (7.8) | 6 (10.2) | 15 (37.5) | 14 (28.0) | 39 (19.5) | < 0.001 |
| Hyperlipidemia | 18 (35.30) | 22 (37.3) | 15 (37.5) | 9 (18.0) | 64 (32.0) | 0.108 |
| Hypertension | 18 (35.30) | 20 (33.9) | 23 (42.5) | 12 (24.0) | 73 (36.5) | 0.011 |
| Body mass | 0.047 | |||||
| Normal BMI | 12 (26.1) | 19 (35.8) | 12 (40.0) | 19 (45.5) | 62 (31.0) | |
| Overweight | 26 (56.5) | 22 (41.5) | 13 (43.3) | 23 (54.8) | 84 (49.1) | |
| Obesity | 8 (17.4) | 12 (22.6) | 5 (16.7) | 0 | 25 (14.6) | |
| Erectile dysfunction | 31 (60.8) | 41 (69.5) | 30 (75.0) | 41 (83.7) | 143 (71.9) | 0.077 |
Data are presented as mean±SD or n (%)
CAD, Coronary artery disease; BMI, Body mass index
The prevalence of ED without considering its severity was significantly higher in the patients with CAD (112 patients, 75.16%) without considering the number of involved vessels than in the control group (31 individuals, 60.8%; p value = 0.041).
Figure 1 depicts the prevalence of ED in the different age groups of CAD patients. In our study, ED prevalence increased by age and ED was diagnosed in more than 91% of the patients and 100% of the controls. Table 3 demonstrates the severity of ED based on the IIEF-EFD scores and the mean scores of the IIEF-EFD in the four study groups. The prevalence of severe ED (IIEF score < 10) was 3.4% in the patients with one-vessel disease and 8.88% in the patients with multi-vessel disease.
Figure 1.
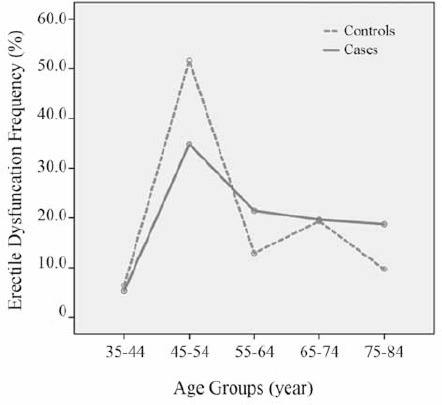
Erectile dysfunction prevalence in the coronary artery disease patients (Cases) and normal (Control) group according to the age decades
Table 3.
Severity of ED based on the IIEF-EFD scores in the study groups*
| Severity of ED | No CAD (controls) | CAD Groups | P value | ||
|---|---|---|---|---|---|
| One-vessel disease | Two-vessel disease | Three-vessel disease | |||
| Erectile function | 0.087 | ||||
| Normal | 20 (39.2) | 18 (30.5) | 10 (25.0) | 8 (16.3) | |
| Mild ED | 27 (52.9) | 31 (52.5) | 24 (60.0) | 32 (65.3) | |
| Moderate ED | 0 | 8 (13.6) | 2 (5.0) | 5 (10.2) | |
| Severe ED | 4 (7.8) | 2 (3.4) | 4 (10.0) | 4 (8.2) | |
| IIEF-EFD score | 23.12±6.520 | 21.58±5.446 | 21.05±6.567 | 20.18±5.667 | 0.013 |
Data are presented as mean±SD or n (%)
ED, Erection dysfunction; IIEF-EFD, International index of erectile function-erectile function domain; CAD, Coronary artery disease
There was a weak positive relationship between the severity of CAD and ED severity (Kendall tau-b value = 0.145, Gamma coefficient = 0.334), which was not significant statistically (p value = 0.056).
When confounding risk factors such as age, hypertension, and diabetes were removed using multiple logistic regression analysis, the significant association between CAD and ED changed to non-significant.
Also, univariate analysis of variance was performed but again no significant association was found between CAD and ED.
Discussion
In this study, the prevalence of ED in the men with angiographically confirmed CAD was higher than that in the control group without CAD and there was an association between ED and CAD. This rate is significantly higher than that in the general male population and diabetic males in Iran. The prevalence of ED in Iranian men aged between 20 and 70 years has been reported to be about 18.8% in the general population and 35.1% in diabetic patients.21, 22 This higher rate in our study can be explained by the presence of further risk factors in our patients other than diabetes.
The mentioned study in Iran reported that the ED rate increased with advanced age.22 As was expected, in the patients with or without CAD, there was an increase in the ED prevalence in the old ages in our study, which confirms the results of previous studies.7, 22, 23 Studies have shown that age is most strongly associated with ED.7
CAD and ED share common risk factors, including diabetes, hypertension, dyslipidemia, obesity, cigarette smoking, and the metabolic syndrome.11–13, 24 Accordingly, the risk factors of CAD are more frequent in men with ED.7, 14 Some studies have provided evidence that ED appears before CAD and other manifestations of this systemic endothelial dysfunction.15–17, 25
As these patients were newly diagnosed with CAD and CAD in most of these patients was in its initial stages, ED was in the early stages too. As a result, the prevalence of mild ED was higher in our patients.
The severity of ED has been found to be related to the degree of atherosclerosis.9 Severe ED (IIEF score < 10) was more frequent in our patients with multi-vessel as compared to the patients with single-vessel disease (8.8% vs. 3.4%).
In the recent largest ED population-based cohort in Australia, the prevalence rates of severe ED were reported to be 2.2% for the age group of 45–54 years, 6.8% for the age group of 55–64 years, 20.2% for the age group of 65–74 years, 50.0% for the age group of 75–84 years, and 75.4% at age > 85 years, which are higher than our findings in CAD patients and controls.23 However, the prevalence of ED in the patients with various severity of CAD was higher than the reported rates in a recent Brazilian study.18 The Brazilian study, conducted on patients with myocardial infarction, found a correlation between the severity of ED and the number of occluded vessels in these patients.18 Our patients did not have myocardial infarction; nonetheless, our results confirmed the same correlation between the severity of ED and the number of involved vessels in the CAD patients as documented by angiography.
An Australian cohort showed that men with severe ED compared to men without it had approximately 1.5 to 2.0 fold risk for ischemic heart disease, peripheral vascular disease, combined cardiovascular events, and all-cause mortality. In contrast, in our study, a significant association between CAD and ED changed to non-significant after adjustment for confounding factor. Most of the observed effects were allied to the confounding factors of age and diabetes. Several limitations may have influenced our results. This may be due to probable recall bias in the accomplishment of the IIEF questionnaire or due to selection bias in selecting individuals with CAD risk factors like diabetes for the control group. Another shortcoming of our study is that patients taking drugs effective on erectile function were not excluded. The high rate of ED in our study may be explained by this fact. Furthermore, some risk factors such as hypertension, diabetes, family history, and age were not uniformly distributed between the groups; there may, therefore, be other possible resources for confounding bias.
Conclusion
There was a significant correlation between ED severity and the number of involved vessels as documented by coronary angiography. Our results showed that ED was not an independent causative risk factor for CAD but it may be considered as an early risk marker for endothelial dysfunction and CAD and a biomarker for the development of atherosclerosis and CAD. Consequently, when a man presents with ED, evaluations for coronary vessel involvement should be recommended.
Acknowledgment
This study was supported by Lorestan University of Medical Sciences.
References
- 1. Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, Abraham J, Adair T, Aggarwal R, Ahn SY, Alvarado M, Anderson HR, Anderson LM, Andrews KG, Atkinson C, Baddour LM, Barker-Collo S, Bartels DH, Bell ML, Benjamin EJ, Bennett D, Bhalla K, Bikbov B, Bin Abdulhak A, Birbeck G, Blyth F, Bolliger I, Boufous S, Bucello C, Burch M, Burney P, Carapetis J, Chen H, Chou D, Chugh SS, Coffeng LE, Colan SD, Colquhoun S, Colson KE, Condon J, Connor MD, Cooper LT, Corriere M, Cortinovis M, de Vaccaro KC, Couser W, Cowie BC, Criqui MH, Cross M, Dabhadkar KC, Dahodwala N, De Leo D, Degenhardt L, Delossantos A, Denenberg J, Des Jarlais DC, Dharmaratne SD, Dorsey ER, Driscoll T, Duber H, Ebel B, Erwin PJ, Espindola P, Ezzati M, Feigin V, Flaxman AD, Forouzanfar MH, Fowkes FG, Franklin R, Fransen M, Freeman MK, Gabriel SE, Gakidou E, Gaspari F, Gillum RF, Gonzalez-Medina D, Halasa YA, Haring D, Harrison JE, Havmoeller R, Hay RJ, Hoen B, Hotez PJ, Hoy D, Jacobsen KH, James SL, Jasrasaria R, Jayaraman S, Johns N, Karthikeyan G, Kassebaum N, Keren A, Khoo JP, Knowlton LM, Kobusingye O, Koranteng A, Krishnamurthi R, Lipnick M, Lipshultz SE, Ohno SL, Mabweijano J, MacIntyre MF, Mallinger L, March L, Marks GB, Marks R, Matsumori A, Matzopoulos R, Mayosi BM, McAnulty JH, McDermott MM, McGrath J, Mensah GA, Merriman TR, Michaud C, Miller M, Miller TR, Mock C, Mocumbi AO, Mokdad AA, Moran A, Mulholland K, Nair MN, Naldi L, Narayan KM, Nasseri K, Norman P, O’Donnell M, Omer SB, Ortblad K, Osborne R, Ozgediz D, Pahari B, Pandian JD, Rivero AP, Padilla RP, Perez-Ruiz F, Perico N, Phillips D, Pierce K, Pope CA, 3rd, Porrini E, Pourmalek F, Raju M, Ranganathan D, Rehm JT, Rein DB, Remuzzi G, Rivara FP, Roberts T, De León FR, Rosenfeld LC, Rushton L, Sacco RL, Salomon JA, Sampson U, Sanman E, Schwebel DC, Segui-Gomez M, Shepard DS, Singh D, Singleton J, Sliwa K, Smith E, Steer A, Taylor JA, Thomas B, Tleyjeh IM, Towbin JA, Truelsen T, Undurraga EA, Venketasubramanian N, Vijayakumar L, Vos T, Wagner GR, Wang M, Wang W, Watt K, Weinstock MA, Weintraub R, Wilkinson JD, Woolf AD, Wulf S, Yeh PH, Yip P, Zabetian A, Zheng ZJ, Lopez AD, Murray CJ, AlMazroa MA, Memish ZA. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012; 380: 2095–20128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Sarrafzadegan N, Rabiei K, Kabir A, Asgary S, Tavassoli A, Khosravi A, Chalian H. Changes in lipid profile of patients referred to a cardiac rehabilitation program. Eur J Cardiovasc Prev Rehabil 2008; 15: 467–472. [DOI] [PubMed] [Google Scholar]
- 3. Montorsi P, Ravagnani PM, Galli S, Salonia A, Briganti A, Werba JP, Montorsi F. Association between erectile dysfunction and coronary artery disease: matching the right target with the right test in the right patient. Eur Urol 2006; 50: 721–731. [DOI] [PubMed] [Google Scholar]
- 4. No authors listed. NIH consensus conference. Impotence. NIH consensus development panel on impotence. JAMA 1993; 270: 83–90. [PubMed] [Google Scholar]
- 5. Feldman HA, Goldstein I, Hatzichristou DG, Krane RJ, McKinlay JB. Impotence and its medical and psychosocial correlates: results of the Massachusetts Male Aging Study. J Urol 1994; 151: 54–61. [DOI] [PubMed] [Google Scholar]
- 6. Ayta IA, McKinlay JB, Krane RJ. The likely worldwide increase in erectile dysfunction between 1995 and 2025 and some possible policy consequences. BJU Int 1999; 84: 50–56. [DOI] [PubMed] [Google Scholar]
- 7. Feldman HA, Johannes CB, Derby CA, Kleinman KP, Mohr BA, Araujo AB, McKinlay JB. Erectile dysfunction and coronary risk factors: prospective results from the Massachusetts Male Aging Study. Prev Med 2000; 30: 328–338. [DOI] [PubMed] [Google Scholar]
- 8. Montorsi P, Ravagnani PM, Galli S, Rotatori F, Briganti A, Salonia A, Dehò F, Montorsi F. Common grounds for erectile dysfunction and coronary artery disease. Curr Opin Urol 2004; 14: 361–365. [DOI] [PubMed] [Google Scholar]
- 9. Solomon H, Man JW, Wierzbicki AS, Jackson G. Relation of erectile dysfunction to angiographic coronary artery disease. Am J Cardiol 2003; 91: 230–231. [DOI] [PubMed] [Google Scholar]
- 10. Greenstein A, Chen J, Miller H, Matzkin H, Villa Y, Braf Z. Does severity of ischemic coronary disease correlate with erectile function? Int J Impot Res 1997; 9: 123–126. [DOI] [PubMed] [Google Scholar]
- 11. Burke JP, Jacobson DJ, McGree ME, Nehra A, Roberts RO, Girman CJ, Lieber MM, Jacobsen SJ. Diabetes and sexual dysfunction: results from the Olmsted County study of urinary symptoms and health status among men. J Urol 2007; 177: 1438–1442. [DOI] [PubMed] [Google Scholar]
- 12. Saigal CS, Wessells H, Pace J, Schonlau M, Wilt TJ. Predictors and prevalence of erectile dysfunction in a racially diverse population. Arch Intern Med 2006; 166: 207–212. [DOI] [PubMed] [Google Scholar]
- 13. Gades NM, Nehra A, Jacobson DJ, McGree ME, Sauver JL, Jacobsen SJ. Cigarette smoking and erectile dysfunction among Chinese men without clinical vascular disease. Am J Epidemiol 2008; 167: 882–883. [DOI] [PubMed] [Google Scholar]
- 14. Bolona ER, Uraga MV, Haddad RM, Tracz MJ, Sideras K, Kennedy CC, Caples SM, Erwin PJ, Montori VM. Testosterone use in men with sexual dysfunction: a systematic review and meta-analysis of randomized placebo-controlled trials. Mayo Clin Proc 2007; 82: 20–28. [DOI] [PubMed] [Google Scholar]
- 15. Vlachopoulos C, Ioakeimidis N, Stefanadis C. Erectile dysfunction and coronary artery disease: a relationship for disclosure. Hellenic J Cardiol 2008; 48: 1–6. [PubMed] [Google Scholar]
- 16. Billups KL, Bank AJ, Padma-Nathan H, Katz S, Williams R. Erectile dysfunction is a marker for cardiovascular disease: results of the minority health institute expert advisory panel. J Sex Med 2005; 2: 40–50. [DOI] [PubMed] [Google Scholar]
- 17. Sekoranja L, Bianchi-Demicheli F, Gaspoz JM, Mach F. Erectile dysfunction: a potential useful marker for cardiovascular disease. Rev Med Suisse 2006; 2: 774–778. [PubMed] [Google Scholar]
- 18. Canat L, Çiçek G, Atış G, Gürbüz C, Çaşkurlu T. Is there a relatıonshıp between severıty of coronary artery disease and severity of erectile dysfunction? Int Braz J Urol 2013; 39: 465–473. [DOI] [PubMed] [Google Scholar]
- 19. Salem S, Abdi S, Mehrsai A, Saboury B, Saraji A, Shokohideh V, Pourmand G. Erectile dysfunction severity as a risk predictor for coronary artery disease. J Sex Med 2009; 6: 3425–3432. [DOI] [PubMed] [Google Scholar]
- 20. Cappelleri JC, Rosen RC, Smith MD, Mishra A, Osterloh IH. Diagnostic evaluation of the erectile function domain of the International Index of Erectile Function. Urology 1999; 54: 346–351. [DOI] [PubMed] [Google Scholar]
- 21. Safarinejad MR. Prevalence and risk factors for erectile dysfunction in a population-based study in Iran. Int J Impot Res 2003; 15: 246–252. [DOI] [PubMed] [Google Scholar]
- 22. Mofid A, Seyedalinaghi SA, Zandieh S, Yazdani T, Jam S. Prevalence and risk factors of erectile dysfunction in Iranian diabetic men. Acta Med Iran 2009; 47: 309–314. [Google Scholar]
- 23. Banks E, Joshy G, Abhayaratna WP, Kritharides L, Macdonald PS, Korda RJ, Chalmers JP. Erectile dysfunction severity as a risk marker for cardiovascular disease hospitalisation and all-cause mortality: a prospective cohort study. PLOS Medicine 2013; 10: 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Gades NM, Nehra A, Jacobson DJ, McGree ME, Girman CJ, Rhodes T, Roberts RO, Lieber MM, Jacobsen SJ. Association between smoking and erectile dysfunction: a population-based study. Am J Epidemiol 2005; 161: 346–351. [DOI] [PubMed] [Google Scholar]
- 25. Kirby M, Jackson G, Betteridge J, Friedli K. Is erectile dysfunction a marker for cardiovascular disease? Int J Clin Pract 2001; 55: 614–618. [PubMed] [Google Scholar]


