Abstract
Background:
Male migrants act as a bridge for transmitting infection from core risk groups to general population and hence this group becomes essential for the HIV control program. Migrant workers constitute a large proportion of workforce in India and HIV/AIDS epidemic in them would cause huge economic losses.
Objectives:
The aim of this study was to ascertain the HIV-risk behavior among male migrant factory workers.
Materials and Methods:
This was a cross-sectional facility based survey conducted in 2011. Male migrant workers aged ≥18 years, who were born outside Haryana, who had moved to current location after 15 years of age, who had worked in the current factory for at least one year, who were willing to participate and able to give valid consent were eligible. A consecutive sampling was done. Descriptive, bivariate and multiple logistic regression analyses were done.
Results:
A total of 755 male subjects completed the interview. About 21.5% had experienced non-spousal sexual intercourse in last one year. Nearly 60% did not use a condom at the last non-spousal sex. Factors associated with recent non-spousal sex were being unmarried, younger age at migration, recent migration to Haryana, greater number of places migrated and lesser total duration of migration and those associated with non-use of condom at the last non-spousal sex were older age, lower education, lesser number of places migrated and lower level of HIV/AIDS knowledge.
Conclusion:
Unprotected, recent non-spousal sex was common among male migrants, which could increase their HIV/AIDS vulnerability.
Keywords: Factory workers, HIV/AIDS risk behaviour, India, migrant workers
Introduction
The overall velocity of Human Immunodeficiency Virus/Acquired Immunodeficiency Disease Syndrome (HIV/AIDS) epidemic appears to have stabilized both globally and in India, but the numbers of new infections are still high.(1,2) The Indian National AIDS Control Programme (NACP) places highest priority on preventive efforts among high risk groups including male migrants and long distance truckers. Male migrants are specifically known as ‘bridge’ population because they act as a bridge for transmission between core risk groups like Female Sex Workers (FSWs) and the low risk general population, who are mostly their spouses. HIV prevalence among male migrants was estimated to be 0.99% in 2008-09, which was three times higher than the general population.(3)
HIV/AIDS shows its adverse impact on businesses in several ways and causes reduction in profits.(4) International Labour Organisation (ILO) estimates that over 90% of people with HIV are adults of working age.(5) Workplace offers a valuable entry point, which could facilitate access to prevention services.(6,7)
In India, there has been a constant increase in the efflux of adult males from less developed rural areas to urban areas for better livelihood. These migrant males are considered to have higher HIV risk behavior. The socially isolated situations under which male migrants work result in behaviors such as unsafe sex that increase risk of exposure. Where there are still opportunities early action will reap tremendous savings.(8) In keeping with this, India has also committed itself to the control of HIV/AIDS in workplaces as evidenced by the policy document ‘National policy on HIV/AIDS and the world of work’,(7) which aims at preventing transmission of HIV infection among workers. The aim of this study was to ascertain the HIV-risk behavior among male migrant factory workers and to assess its association with selected socio-demographic variables.
Materials and Methods
This was a facility based cross-sectional survey conducted in two factories located at Ballabgarh block of Haryana in 2011. Male migrant workers aged 18 years or above, who were born outside Haryana, who had moved to current location after 15 years of age, who had worked in the current factory for at least one year, who were willing to participate and able to give valid consent were eligible for inclusion in the study. Face-to-face interview was conducted using pretested semi-structured questionnaire. Two dependent variables were included for the analysis, separately: Recent, non-spousal sex (i.e. in the last 1 year) and non-use of condom at the last (i.e. most recent) non-spousal sex that represented HIV-risk behavior. ‘Recent’ means in the last 1 year, and ‘Ever’ means lifetime experience and ‘last non-spousal sex’ means the most recent non-spousal sex. Main independent variables identified from the literature review and considered here include age, residence, marital status, education, migration characteristics and HIV knowledge variables. HIV/AIDS knowledge score was assessed by 22 questions on transmission routes, preventive methods and curative services available. This was converted into a score out of 22 and was classified based on proportion of the maximum possible score obtained, into three categories as ≥80% (comprehensive), 50% to 79% (moderate) and ≤49% (poor). The question asked for assessing non-spousal sex was ‘Have you ever had sex with a person other than your wife (for married men) or any person (for unmarried men)?’ and the options were ‘Yes, in the last one year’, ‘Yes, but not in the last one year’ and ‘No’. For sample size calculation, we assumed that the prevalence of unprotected recent non-spousal sex (last one year) was 15%. For an absolute precision of 3%, alpha error of 5%, power of 80% and non-response rate of 20%, the final sample size was calculated as 710 using the formula n = 4pq/d*d. The sampling strategy adopted was the one similar to that used in HIV sentinel surveillance(9) activities in India i.e., consecutive sampling. Workers attending the factory clinic were approached to take part in the study in a consecutive manner and not more than 20 interviews were conducted in a single day. Ethical approval was obtained from the Ethics Committee of the All India Institute of Medical Sciences, New Delhi. Informed written consent was obtained from all the participants. The interview was conducted in a separate room within the clinic and privacy was ensured during the interviews. No information on the person's identification, such as name or employee number, was collected to ensure confidentiality.
Statistical analysis
All analyses were done using Stata/IC 11.1 (StataCorp LP, College Station, TX). Data were described in terms of proportions, means, Standard Deviations (SD), median, Inter Quartile Range (IQR) and 95% Confidence Intervals (CI) wherever applicable. Multivariable logistic regression was done by backward stepwise method. The P value for entry of variable into the model was kept at 0.20 and P value for removal was kept at 0.05. The variables retained in the final model were presented with adjusted odds ratios (aOR) and 95% CIs. Statistical significance was set at P value less than 0.05.
Results
Socio-demographic characteristics and HIV/AIDS knowledge
A total of 767 men were approached for participation and 755 completed the interview. Site 1 contributed 547 and site 2 contributed 208 participants. Distribution of source states was as follows: Bihar-45.4%, Uttar Pradesh-37.2%, Rajasthan - 13.2% and others-4.1%. The mean (SD) age of the participants was 31.4 (8.2) years. Nearly 90% were literate and almost 90% were semi-skilled workers. Three-fourth of the men were married, but among them nearly half were not staying with their spouses at the current residence. The mean (SD) age at migration was 21.8 (4.9) years, mean (SD) number of places migrated for work related purposes was 3.6 (2.9), and mean (SD) total duration of migration was 9.5 (6.7) years. Only 40% of participants had a comprehensive HIV/AIDS knowledge.
Experience of non-spousal sex
Nearly 90% of men were sexually experienced. The median age at first sexual intercourse was 18 years (IQR 13 to 31). Nearly half (45.5%) of the participants had experienced non-spousal sexual intercourse (ever), among whom nearly half (47%) had involved in such behavior in the last one year i.e., recent non-spousal sex and this proportion was higher in unmarried persons as compared to married persons. Eighty-five percent of men who reported non-spousal sex (ever) also reported having non-spousal sex in their hometown. Nearly one fourth of those reporting non-spousal sex (ever) also reported having paid money for sex in the last one year, which was higher among unmarried men as compared to married men [Table 1].
Table 1.
HIV-risk behavior among male migrant workers in selected factories of Faridabad
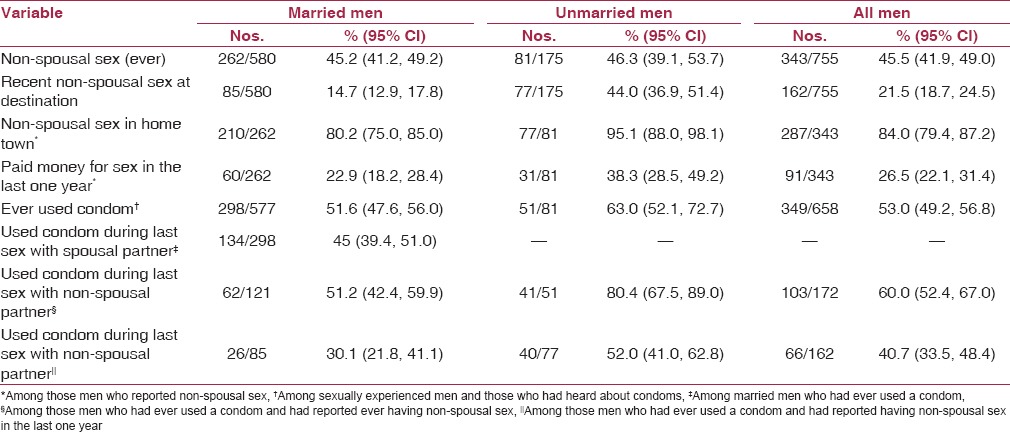
Condom use pattern
Among participants who were sexually experienced, only 53% had ever used a condom, which was higher in unmarried men as compared to married men. Among married men who had used a condom, more than half did not use condom at the last sex with spousal partner. Among men who reported ever use of condom and experience of non-spousal sex (ever), 40% did not use a condom at the last sex with a non-spousal partner and this percentage was higher among married men as compared to unmarried men. Among men who reported ever use of condom and experience of non-spousal sex (recent), nearly 60% did not use a condom at the last sex with a non-spousal partner and this percentage was much higher among married men as compared to unmarried men [Table 1]. Among married men who had used a condom, only half (48.3%) reported using condoms always or most times during sex with spousal partner. The major reason given by them for not using condom during sex with spousal partner was ‘didn’t think it was necessary’ followed by ‘don’t like them’ and ‘partner objected’. The major reason given by them for not using a condom during sex with a non-spousal partner was ‘there was no time’ followed by ‘didn’t think of it’, ‘didn’t think it was necessary’ and ‘don’t like them’. The major reason given by unmarried men for not using a condom during sex with a non-spousal partner was ‘don’t like them’ and ‘partner objected’ (data not shown). The mean (SD) time reported by the participants to get a condom close to their house or workplace was 22.2 (7.4) minutes.
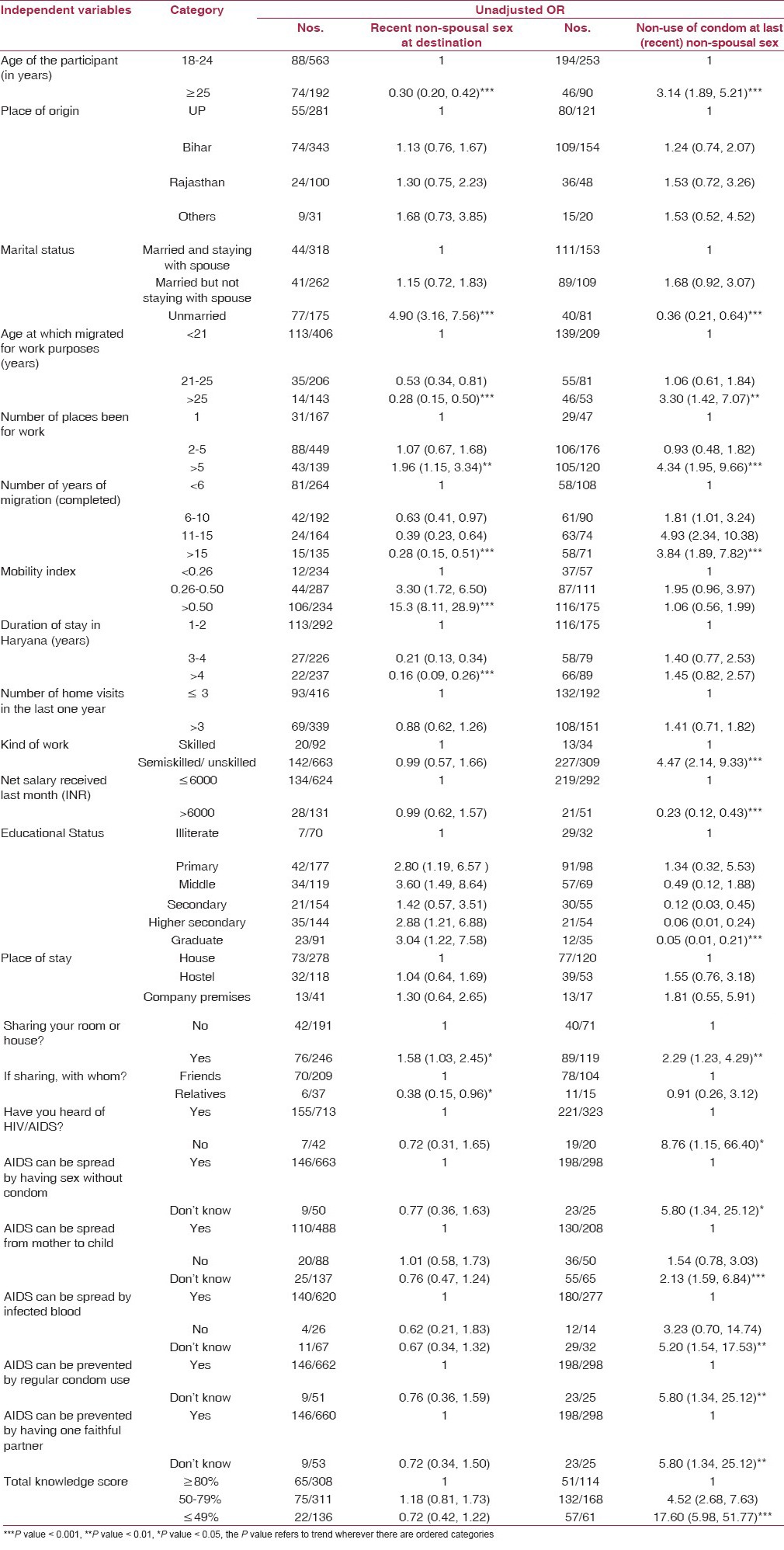
Bivariate analysis
Bivariate analysis showed that factors that were significantly associated with experience of recent non-spousal sex were younger age (<25 years), being unmarried, younger age at migration, greater number of places migrated, lesser total migration duration, higher mobility and recent migration to Haryana [Table 2]. Factors that were found to be significantly associated with non-use of condom at last non-spousal sex were older age, being married, older age at migration, greater number of places migrated, greater total migration duration, lower education, being semiskilled/unskilled worker, lower income, having a roommate and lower level of HIV/AIDS knowledge [Table 2].
Table 2.
Bivariate analyses — effect of independent variables on the experience of recent non-spousal sex at destination and non-use of condom at last non-spousal sex among male migrant workers in selected factories of Faridabad
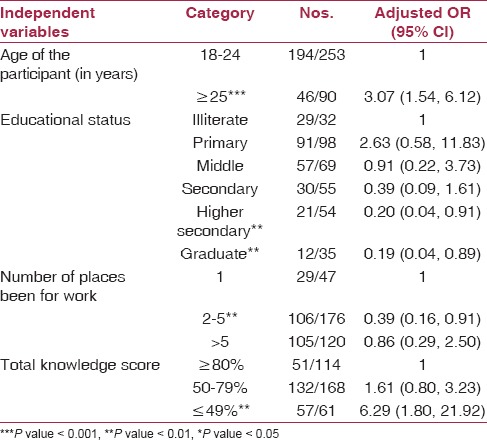
Multivariable analysis
Factors independently associated with experience of recent non-spousal sex were being unmarried, younger age at migration, recent migration to Haryana, greater number of places migrated and lesser total duration of migration [Table 3]. It is important to note that the HIV/AIDS knowledge was not significantly associated with this outcome. The model had a good fit to the data as assessed by the area under the ROC curve (0.8) and the goodness of fit chi square test (P value = 0.07). Factors independently associated with non-use of condom at the last non-spousal sex were older age, lower education, lesser number of places migrated and lower level of HIV/AIDS knowledge [Table 4]. The model had a good fit to the data as assessed by the area under the ROC curve (0.8) and the goodness of fit chi square test (P value = 0.21).
Table 3.
Multiple logistic regression — independent factors associated with recent non — spousal sex at destination among male migrant workers in selected factories of Faridabad
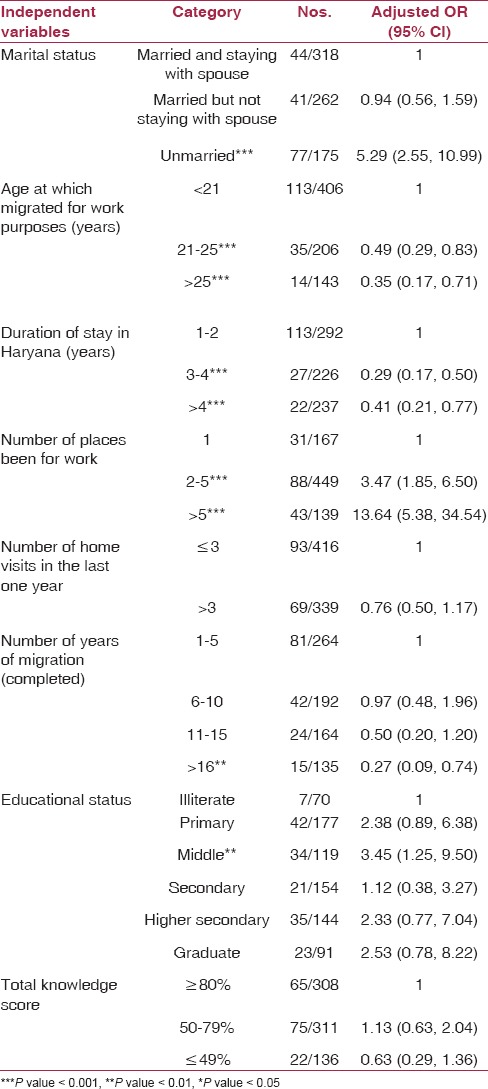
Table 4.
Multiple logistic regression — independent factors associated with non-use of condom at last (recent) nonspousal sex among male migrant workers in selected factories of Faridabad
Discussion
The study population was relatively younger and more literate because men like them were more likely to be employed in such factories. This background is likely to be true for men working in similar setups across a range of factories.
Experience of non-spousal sex
About 88% of men were sexually experienced, which was comparable to that reported (80%) by Deb et al., in a similar study setting, in Kolkata.(10) The median age at first sexual intercourse was 18 years, which was comparable to that reported as by Lurie et al., among migrant workers in South Africa,(11) but lower than that reported by Huy et al., among non-contract worker in Vietnam(12) and National Behavioural Sentinel Surveillance Survey, 2006 (BSS) for the general population.(13) This indicates that this was a sexually active group that had an early sexual initiation as compared to the national survey estimates for general population. About one-fifth of the participants reported having experienced recent non-spousal sexual intercourse (last one year) and this proportion increased to 46% when the reference period was increased to lifetime. A number of studies(14,15,16) reported similar prevalence among male migrants. A slightly higher proportion (24 to 65%) was reported by Halli et al., among workers of various sectors.(17) The BSS, 2006(13) reported a much lower prevalence of 9% among the general population and 6% among the laborer sub group. Similarly, National Family Health Survey, 2005-06 (NFHS-3)(18) also reported a lower prevalence of 6% among all men, 10% among ‘men away from their homes for more than a month’ subgroup and 6% among ‘production workers’ subgroup. This fact suggests that our study population displayed a higher prevalence of risky behavior. The Population Council study(19,20,21,22) reported a prevalence of non-spousal sex of 11 to 41% among married men and 12 to 49% among unmarried men across different study states. Among ‘industrial workers’ subgroup the corresponding figures were 11 to 49% and 10 to 41%. These findings were similar to that of our study results.
A large proportion of men were found to have involved in recent non-spousal sex. Gras et al.,(23) reported that about 23% of male migrants in the Netherlands reported having sex in the country of origin in the last five years. The Population Council study(19,20,21,22) reported that 21 to 34% men in the ‘industrial workers’ subgroup reported non-marital sex in the place of origin. NFHS-3(18) reported that the prevalence of paid sex in the last one year was 0.6% among general population, 1.4% among men in the ‘more than one month away from their homes’ subgroup and 1.1% among ‘production workers’ subgroup. The high prevalence of non-spousal sex in the hometown underscores that these migrant men were actively involved in risky behavior in their hometowns as well, but whether this behavior was acquired pre or post migration could not be answered from this study. If this behavior was acquired post- migration, then the intervention must be targeted at the workplace; otherwise, it should be directed to the places of origin, in the form of migration welfare centers, migration counsellors or via similar mechanisms.
It was interesting to note that HIV/AIDS knowledge was not a significant factor associated with recent non-spousal sex. It is indicated that even though migrant men may have HIV/AIDS knowledge, they still indulged in non-spousal sex. Factors associated with non-spousal sex or commercial or multiple partner sex reported by other authors included lower education,(24,25,26) being married,(26,27) younger age,(24,28) being a contract worker,(28) living without family,(28,29,30) frequent travellers,(24) increased mobility,(27) greater number of jobs held,(27) and lower income.(26) The findings may enable us to devise an intervention plan that is specifically targeted to the factors mentioned above. Young, unmarried, recently migrated and highly mobile men should be given top priority for intervention.
Condom use pattern
Among the sexually experienced men, 47% had never used a condom, which was lower than that reported by Saggurti et al.,(14) and Li et al.,(27) among migrant workers. It was an alarming finding because in spite of large scale IEC (Information, Education and Communication) activities directed to promote the use of condoms, almost half of these men had never used a condom. This requires further detailed investigation as to why men do not prefer to use condom.
Only 45% of married men, who had ever used condoms, did use a condom in the last sex with their spouse. Among men who had reported non-spousal sex in the last one year, only 40% used a condom at last sexual encounter with non-spousal partner. In other words, the prevalence of unprotected non-spousal sex intercourse in this study population was about 60%. The BSS, 2006(13) reported that prevalence of condom use during last sex with non-regular partner was 58% in general population, and 56% among ‘laborer’ subgroup. The NFHS-3(18) reported, a prevalence of 32% among ‘men who stayed more than one month away from their homes’ subgroup and 53% among ‘production workers’ subgroup. Saggurti et al.,(15) reported 11 to 20%, Halli et al.,(17) reported 8 to 68%, Li et al.,(25) reported 36%, Buregyeya et al.,(28) reported 36%, Huy et al.,(12) reported 30% for the same. This shows that this study population had higher risk behavior as compared to other studies. Men who engage in unprotected non-spousal sex are at a high risk for HIV acquisition and thereby require priority attention from policy makers and IEC planners.
Among married participants, who have ever used a condom, about 46% had used condoms consistently, which is in contrast to the 14% reported by the BSS, 2006(13) among general population. The prevalence of inconsistent condom reported in other studies was 42% by Saggurti et al., 2008(14) , 33 to 67% among married men and 27 to 78% among unmarried men in a study by Population Council.(19,20,21,22) Deb et al.,(10) reported that 55% of married men, never used a condom with commercial sex worker. Consistent condom use is more important than ever use of condom with a non-spousal partner, therefore apart from promoting use of condoms, consistent use of condoms should also be emphasized in targeted intervention packages.
The mean time required to obtain a condom was reported as 22 minutes, which was similar to the finding in BSS, 2006(13) in which 80% laborer ‘subgroup’ reported that it took less than 30 minutes to obtain a condom. The widespread availability of condom distribution facilities was probably responsible for this finding. The social marketing strategy adopted for the sale of condoms also must have had an impact on the easy availability of condoms. Engaging in constant informed dialogue with professional associations of industries will probably bring about a positive policy change.
Four factors namely older age, lower education, lesser number of places migrated and having lower HIV/AIDS knowledge were independently associated with non-use of condom during non-spousal sex. Studies have reported that age less than 30 years,(28) being single,(28,31) having a steady partner, higher education(26) were associated with condom use during non-spousal sex. Men who are relatively older, generally tend to be averse to condom use, probably due to inadequate knowledge about HIV/AIDS. Migration related factors were not found to be associated with condom use, like they were with non-spousal sex. This probably means that the process of migration does not play much of a role in the determining condom use pattern. The most important factors that influence condom use during non-spousal sex seem to be the level of education and HIV/AIDS knowledge.
From the several findings of this study, it is possible to discern a chain of interconnected events that explain the vulnerability of migrant men. Young men often migrate alone, leaving behind their families. At the destination, several factors like boredom, lack of entertainment facilities, peer pressure, lack of social support, the cover of anonymity, expendable cash, the biological drive for sex, and the availability of networks of commercial sex workers work together to enable these men to seek non-spousal, casual or multiple partner sex. The lack of comprehensive knowledge regarding HIV/AIDS and aversion to condom use puts them at risk of involving in risky sexual behavior such as unprotected sexual intercourse, thus increasing their vulnerability to HIV infection. To tackle this problem several measures can be adopted such as peer educator programs in factories could be introduced, co-ordination with local Integrated Counselling and Testing Centers (ICTCs) for voluntary counseling and testing can be ensured, regular refreshment courses at workplace and forming alliances with industry associations to provide overall support to HIV/AIDS related activities within factories can be sought.
There are certain limitations in this study. Firstly, the consecutive sampling strategy limits generalizability. Since the results closely corroborated by other studies done in similar settings, external validity of this study would be adequate. Secondly, partner related socio-demographic information was not obtained and hence their confounding effect could not be studied. Thirdly, temporality of behavior with respect to pre/post migration status could not be studied. Finally, since much of the information on sexual behavior was self-reported, social desirability bias could not be ruled out.
Conclusion
It can be stated that unprotected recent non-spousal sex was common among male migrants, which increases their HIV/AIDS vulnerability. Promotion of consistent condom use and reduction of non-spousal sex by intensive interpersonal communication and other channels of behavioral change could help in reducing this vulnerability. Intervention must also be targeted at the sites of origin of the migrants for a comprehensive and successful preventive strategy.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.UNAIDS. UNAIDS report on the global AIDS epidemic. Geneva: UNAIDS; 2012. [Google Scholar]
- 2.Technical report, India HIV estimates. New Delhi: NACO; 2010. National AIDS Control Organisation, National Institute of Medical Statistics, Government of India. [Google Scholar]
- 3.HIV Sentinel Surveillance 2010-11, a technical brief. New Delhi: NACO; 2012. National AIDS Control Organisation, Ministry of Health and Family Welfare, Government of India. [Google Scholar]
- 4.Afsar MS. Enhancing Business Response to HIV/AIDS in India: Operational guidelines with estimated cost analysis. New Delhi: International Labour Organization; 2005. [Google Scholar]
- 5.Facts on HIV and Work. Geneva: ILO; 2009. International Labour Organization. [Google Scholar]
- 6.Recommendation concerning HIV and AIDS and the world of work. Geneva: ILO; 2010. International Labour Organization. [Google Scholar]
- 7.National Policy on HIV/AIDS and the world of work. New Delhi: MLE; 2009. Ministry of Labour and Employment, Government of India. [Google Scholar]
- 8.Employers’ handbook on HIV/AIDS, a guide for action. Geneva: IOE; 2002. International Organisation of Employers, UNAIDS. [Google Scholar]
- 9.HIV Sentinel Surveillance and HIV estimation in India, 2007-08. New Delhi: NACO; 2008. National AIDS Control Organisation, Ministry of Health and Family Welfare, Government of India. [Google Scholar]
- 10.Deb AK, Deb M, Saha MK, Chakraborty S, Bhattacharya SK, Detels R. HIV transmission potential among local and migrant factory workers in Kolkata, India. AIDS Behav. 2009;13:928–38. doi: 10.1007/s10461-009-9542-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lurie M, Harrison A, Wilkinson D, Karim S. Circular migration and sexual networking in rural KwaZulu/Natal: Implications for the spread of HIV and other sexually transmitted diseases. Health Transit Rev. 1997;7:17–27. [PubMed] [Google Scholar]
- 12.Huy NV, Dunne MP, Debattista J, Hien NT, Dao Thi Minh An. Association of Human Immunodeficiency Virus (HIV) preventive information, motivation, self-efficacy and depression with sexual risk behaviors among male freelance laborers. J AIDS HIV Res. 2011;3:20–9. [Google Scholar]
- 13.National Behavioural Surveillance Survey (BSS). General population. New Delhi: 2006. National AIDS Control Organisation, Ministry of Health & Family Welfare, Government of India. [Google Scholar]
- 14.Saggurti N, Verma RK, Jain A, RamaRao S, Kumar KA, Subbiah A, et al. HIV risk behaviours among contracted and non-contracted male migrant workers in India: Potential role of labour contractors and contractual systems in HIV prevention. AIDS. 2008;22(Suppl 5):S127–36. doi: 10.1097/01.aids.0000343771.75023.cc. [DOI] [PubMed] [Google Scholar]
- 15.Saggurti N, Mahapatra B, Swain SN, Jain AK. Male migration and risky sexual behavior in rural India: Is the place of origin critical for HIV prevention programs? BMC Public Health. 2011;11:S6. doi: 10.1186/1471-2458-11-S6-S6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Saggurti N, Mahapatra B, Swain SN, Chawla U, Narang A. Migration and HIV in India: Study of select districts. New Delhi: 2011. [Google Scholar]
- 17.Halli SS, Buzdugan R, Ramesh BM, Gurnani V, Sharma V, Moses S, et al. Assessing HIV risk in workplaces for prioritizing HIV preventive interventions in Karnataka state, India. Sex Transm Dis. 2009;36:556–63. doi: 10.1097/OLQ.0b013e3181a8cdcf. [DOI] [PubMed] [Google Scholar]
- 18.National Family Health Survey (NFHS-3), 2005-06. Vol. 1. Mumbai: IIPS; 2007. International Institute for Population Sciences (IIPS) and Macro International. [Google Scholar]
- 19.Migration/Mobility and vulnerability to HIV among Male Migrant Workers: Karnataka. Bangalore: KHPT; 2008. Karnataka Health Promotion Trust (KHPT) and Population Council. [Google Scholar]
- 20.Migration/Mobility and vulnerability to HIV among male migrant workers: Andhra Pradesh. New Delhi: Population Council; Population Council. [Google Scholar]
- 21.Migration/Mobility and vulnerability to HIV among male migrant workers. Mumbai: TISS; 2008. Tata Institute of Social Sciences (TISS) and Population Council. [Google Scholar]
- 22.Migration/mobility and vulnerability to HIV among male migrant workers: Tamil Nadu. Chidambaram: Annamalai University; 2008. Annamalai University and Population Council. [Google Scholar]
- 23.Gras MJ, Weide JF, Langendam MW, Coutinho RA, van den Hoek A. HIV prevalence, sexual risk behaviour and sexual mixing patterns among migrants in Amsterdam, The Netherlands. AIDS. 1999;13:1953–62. doi: 10.1097/00002030-199910010-00019. [DOI] [PubMed] [Google Scholar]
- 24.Lau JT, Thomas J. Risk behaviours of Hong Kong male residents travelling to mainland China: A potential bridge population for HIV infection. AIDS Care. 2001;13:71–81. doi: 10.1080/09540120020018198. [DOI] [PubMed] [Google Scholar]
- 25.Li L, Morrow M, Kermode M. Vulnerable but feeling safe: HIV risk among male rural-to-urban migrant workers in Chengdu, China. AIDS Care. 2007;19:1288–95. doi: 10.1080/09540120701402855. [DOI] [PubMed] [Google Scholar]
- 26.Borgdorff MW, Barongo LR, Newell JN, Senkoro KP, Devillé W, Velema JP, et al. Sexual partner change and condom use among urban factory workers in northwest Tanzania. Genitourin Med. 1994;70:378–83. doi: 10.1136/sti.70.6.378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Li X, Zhang L, Stanton B, Fang X, Xiong Q, Lin D. HIV/AIDS-related sexual risk behaviors among rural residents in China: Potential role of rural-to-urban migration. AIDS Educ Prev. 2007;19:396–407. doi: 10.1521/aeap.2007.19.5.396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Buregyeya E, Bazeyo W, Moen BE, Michelo C, Fylkesnes K. HIV risk behavior and work in Uganda: A cross-sectional study. East Afr J Public Health. 2008;5:43–8. doi: 10.4314/eajph.v5i1.38976. [DOI] [PubMed] [Google Scholar]
- 29.Mishra A. Risk of sexually-transmitted infections among migrant men: Findings from a survey in Delhi. Asian Pac Migr J. 2004;13:89 106. [Google Scholar]
- 30.Saggurti N, Schensul SL, Verma RK. Migration, mobility and sexual risk behavior in Mumbai, India: Mobile men with non-residential wife show increased risk. AIDS Behav. 2009;13:921–7. doi: 10.1007/s10461-009-9564-8. [DOI] [PubMed] [Google Scholar]
- 31.Organista KC, Balls Organista P, García de Alba JE, Castillo Morán MA, Ureta Carrillo LE. Survey of condom-related beliefs, behaviors, and perceived social norms in Mexican migrant laborers. J Community Health. 1997;22:185–98. doi: 10.1023/a:1025173008088. [DOI] [PubMed] [Google Scholar]


