Fetal cardiac tumors are rare conditions and their incidence ranges from 0.08% to 0.2%[1]. However, this percentage during fetal life may be underestimated, given that regression commonly occurs. It should also be noted that atrial tumors may be small or, when located in the septum or ventricular cavity, often mimic an echogenic focus (golf ball sign), thus leading to difficulty in recognizing them through ultrasonographic screening[2].
Among the various histological types, the three commonest types in fetuses, newborns and children are firstly rhabdomyoma (60%) and then teratomas (25%) and fibromas (12%)[1,3,4]. These histological types are benign tumors, since malignant types are extremely rare in fetuses[4] . Rhabdomyomas are the commonest subtypes and present as homogenous hyperechogenic masses that are generally multiple, with variable sizes. They may be intramural or intracavitary, and generally occupy the interventricular septum or right ventricle, close to the moderator band, but they can be located in any cardiac chamber[4]. Rhabdomyomas are hormone-dependent tumor, which explains their well-known capacity for spontaneous regression or reduction, along with their close relationship with tuberous sclerosis[5]. Fibromas rarely present during fetal life, but are generally located in the interventricular septum or the free wall of the left ventricle. They present as large single masses and, differently from rhabdomyomas, do not regress after birth. For this reason, they may cause obstructions[4]. Fibromas require clinical follow-up at birth because they may lead to sudden death. Because they are giant masses, resection may be difficult and therefore heart transplantation is indicated[4,6]. Teratomas generally present as extracardiac masses located close to the aorta and pulmonary artery. They have multicystic formation and may evolve with pericardial effusion[4,6].
Diagnosing cardiac tumors by means of two-dimensional echocardiograms is a fundamental step towards follow-up and prognostic evaluation (Figure 1).
Fig. 1.
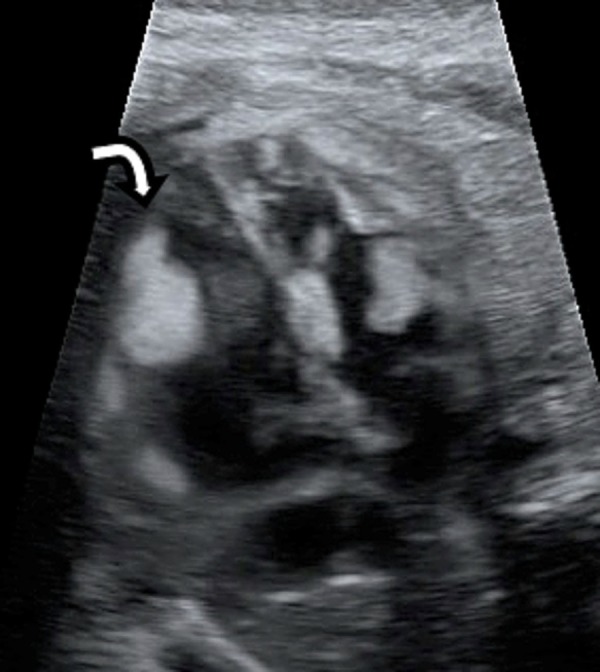
Two-dimensional echocardiographic at 22 weeks of gestation in the “four-chamber” view showing a rhabdomyoma in the internal wall of fetal left ventricle (white arrow)
Three-dimensional echocardiography is now acquiring an important role in detection and evaluation of the characteristics of these masses, and it has the capacity to provide greater precision and efficacy in determining their size and how they compromise adjacent structures[7-9].
Depending on the histological type, location and number of nodules, cardiac tumors have a range of presentations, going from silence to development of severe clinical manifestations, such as arrhythmias and blood flow restrictions due to obstruction of the ventricular cavities or the atrioventricular and semilunar valves, thereby causing valve regurgitation due to changes to the mobility of these valves, depending on the degree of insufficiency, presence of these tumors may lead to a hemodynamic disorder. Alteration of the ventricular ejection fraction, hydrops or congestive heart failure may occur and, if such situations develop, the prognosis will consequently be worse[4].
Rhabdomyomas can often impair the conduction system of the fetal heart and lead to heart rate disorders such as extrasystoles, supraventricular tachycardia or, less commonly, prolongation of the PR space, nonspecific alterations of ST follow-up, Wolf-Parkinson-White syndrome or aberrant atrioventricular conduction[1,5,7,10]. Wacker-Gussmann et al.[1] evaluated the heart rate of 10 fetuses with rhabdomyoma, by means of electrophysiology, and observed that even the asymptomatic fetuses presented conduction disorders.
Management of fetuses with diagnoses of cardiac tumors requires serial echocardiograms, and the approach will vary according to the symptoms. An expectant approach is used in cases of asymptomatic tumors. The echocardiographic evaluation in cases of obstructions should be very detailed, so as to be alert with regard to the presence of reverse flow in the ascending aorta and pulmonary trunk, caused by obstruction of the right and left outlets. Another important sign is increased flow in the circumflex artery, which may nourish the tumor mass[3] . In cases of obstruction of the blood flow, the management should be conservative and preterm delivery should be avoided, except in cases in which the fetus is in the third trimester and presents severe hemodynamic disorders. In these cases, delivery needs to be induced and should be done in a tertiary-level center with a multidisciplinary team, given that immediate surgical resection to relieve the flow sometimes becomes necessary[2,4,6].
In cases of malignant arrhythmias such as supraventricular tachycardia and atrial flutter, drug treatment with anti-arrhythmia agents should be started immediately, remembering that the arrhythmia may often be refractory to treatment. In cases of fetal hydrops, with significant pericardial effusion, intrauterine pericardiocentesis may be necessary[1,4,8].
In summary, attention is drawn to cardiac tumors because of their diversity of forms of clinical manifestations. Early diagnosis by means of fetal echocardiograms is essential, in order to evaluate the prognosis and schedule the best prenatal and delivery management, with the multidisciplinary team.
REFERENCES
- 1.Wacker-Gussmann A, Strasburger JF, Cuneo BF, Wiggins DL, Gotteiner NL, Wakai RT. Fetal arrhythmias associated with cardiac rhabdomyomas. Heart Rhythm. 2014;11(4):677–683. doi: 10.1016/j.hrthm.2013.12.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Croti UA, Mattos SS, Pinto VC, Jr, Aiello VD, Moreira VM. Cardiologia e cirurgia cardiovascular pediátrica. 2nd ed. São Paulo: Roca; 2012. [Google Scholar]
- 3.Niewiadomska-Jarosik K, Stańczyk J, Janiak K, Jarosik P, Moll JJ, Zamojska J, et al. Prenatal diagnosis and follow-up of 23 cases of cardiac tumors. Prenat Diagn. 2010;30(9):882–887. doi: 10.1002/pd.2586. [DOI] [PubMed] [Google Scholar]
- 4.Isaacs H Jr. Fetal and neonatal cardiac tumors. Pediatr Cardiol. 2004;25(3):252–273. doi: 10.1007/s00246-003-0590-4. [DOI] [PubMed] [Google Scholar]
- 5.Carvalho SR, Marcolin AC, Cavalli RC, Crott GC, Mendes MC, Duarte G, et al. Fetal cardiac rhabdomyoma: analysis of five cases. Rev Bras Ginecol Obstet. 2010;32(4):156–162. doi: 10.1590/s0100-72032010000400002. [DOI] [PubMed] [Google Scholar]
- 6.Yinon Y, Chitayat D, Blaser S, Seed M, Amsalem H, Yoo SJ, et al. Fetal cardiac tumors: A single-center experience of 40 cases. Prenat Diagn. 2010;30(10):941–949. doi: 10.1002/pd.2590. [DOI] [PubMed] [Google Scholar]
- 7.Guimarães HA, Filho, Araujo E, Júnior, Pires CR, Costa LL, Nardozza LM, Mattar R. Prenatal sonographic diagnosis of fetal cardiac rhabdomyoma: a case report. Radiol Bras. 2009;42(3):203–205. [Google Scholar]
- 8.Holley DG, Martin GR, Brenner JI, Fyfe DA, Huhta JC, Kleinman CS, et al. Diagnosis and management of fetal cardiac tumors: a multicenter experience and review of published reports. J Am Coll Cardiol. 1995;26(2):516–520. doi: 10.1016/0735-1097(95)80031-b. [DOI] [PubMed] [Google Scholar]
- 9.Geipel A, Krapp M, Germer U, Becker R, Gembruch U. Perinatal diagnosis of cardiac tumors. Ultrasound Obstet Gynecol. 2001;17(1):17–21. doi: 10.1046/j.1469-0705.2001.00314.x. [DOI] [PubMed] [Google Scholar]
- 10.Pipitone S, Mongiovì M, Grillo R, Gagliano S, Sperandeo V. Cardiac rhabdomyoma in intrauterine life: clinical features and natural history. A case series and review of published reports. Ital Heart J. 2002;3(1):48–52. [PubMed] [Google Scholar]


