Abstract
Achieving adequate pulpal anesthesia in mandibular teeth is always a challenge. Supplementary injections and using drugs in combination are some methods implemented to overcome this hurdle. In this randomized clinical trial, use of meperidine in conjunction with lidocaine in intraligamentary injection did not exhibit significant improvement in anesthesia.
Key Words: Periodontal ligament, Meperidine, Irreversible pulpitis, Dental anesthesia
The failure rate of the inferior alveolar nerve block (IANB) in some experimental studies has been reported up to 75%.1–4 This lack of success has even increased to a maximum of 81% in some recent studies.5–7 To overcome this shortcoming, dental clinicians have actively sought measures to improve the patients' anesthesia during different dental procedures. Apart from the anatomical variations mentioned in the applied anatomy of injections,8 several authors have attempted to modify the anesthetic technique,9–12 and others have compared different anesthetic agents13 or their concentrations14 to improve their efficacy.
Activating the opioid receptors peripherally in inflammatory conditions has become a new trend in research to manage postoperative pain.15 Synergy between local anesthetics and opioids has become an interesting field of research recently.16 Opioids are frequently added to local anesthetics in a variety of surgical procedures, eg, intrathecal application for minor surgery.17 Meperidine or its derivatives, eg, pethidine (meperidine chloride) or norpethidine (Pethidine Intermediate B) are agonists of μ-opioid receptors, which block the pathway of pain signals to the trigeminal nucleus. They also activate peripheral opioid receptors and block sodium channels.17–22 Despite controversy regarding the use of meperidine as an anesthetic,22 recent studies have demonstrated its benefits over prilocaine in arthroscopy with local anesthesia,16 nasal packing removal,23 etc.
However, only a few studies have investigated the dental anesthetic efficacy of such combinations.24,25 The effect of the addition of meperidine to lidocaine in IANB for pain management in normal teeth24 and also in teeth with irreversible pulpitis25 has been studied. The aim of our study was to compare the efficacy of local anesthetics with and without meperidine for intraligamentary supplemental injection for teeth with irreversible pulpitis. Our null hypothesis stated that the addition of meperidine to standard lidocaine with epinephrine does not improve the efficacy of supplemental intraligamentary anesthesia in teeth with symptomatic irreversible pulpitis. The specific objectives were to randomly allocate volunteers with complete soft tissue anesthesia following an IANB, yet having positive pulp response, into 2 groups, and then compare the efficacy of lidocaine with epinephrine plus meperidine with that of lidocaine with epinephrine plus an equal volume of sterile water for supplemental periodontal ligament anesthesia.
METHODS
Inclusion and Exclusion Criteria
Sixty volunteer patients, aged 18–65 years, with symptomatic irreversible pulpitis and moderate to severe spontaneous pain in their first or second mandibular molars participated in this double-blind, randomized clinical trial research. Patients were referred to the Endodontic Clinic at Azad Tehran Dental School for root canal treatment. Our local board of research ethics peer reviewed and approved the study protocol. All subjects signed written informed consents upon receiving a thorough description of study aim and setting. The subjects were otherwise systemically healthy, were not taking any medications affecting their pain perception (benzodiazepines or barbiturates) during the previous 48 hours, and had no history of allergy to any local anesthetics or opioids. They also were allowed to leave the study whenever they wanted. The authors excluded pregnant or nursing women, patients with necrotic pulps, and those with moderate to advanced periodontal disease. The included teeth must have shown prolonged responses to cold, hot, electric pulp test (EPT), and pain to percussion with no specific periapical radiographic lesion.
According to Rattan et al,26 who assessed the effectiveness of peripheral administration of fentanyl with lidocaine in inflamed dentoalveolar tissues, the mean pain on percussion was measured to be 19 ± 4.37 units and 15.3 ± 3.62 units respectively in the control and the fentanyl groups (α = .05, β = .2). Our sample size27 was then calculated as
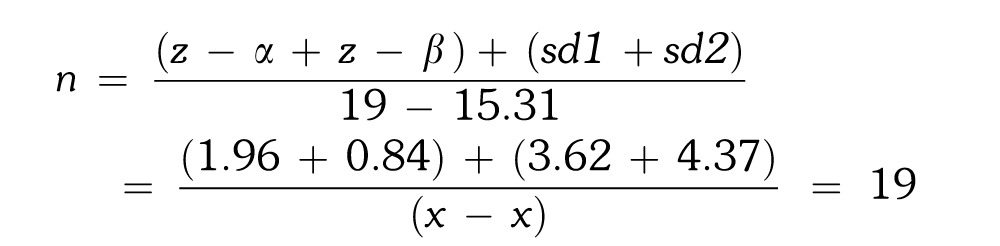 |
A minimum of 19 patients per groups was calculated and modified, based on a 30% loss to follow-up probability, to the following:
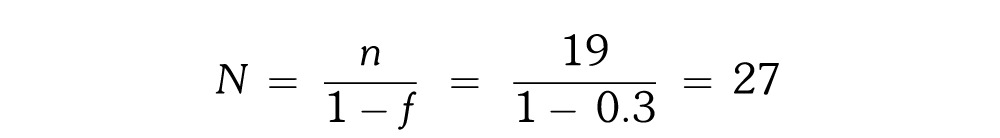 |
We then rounded to 30 per group, which accounted for a total of 60 included patients.
For simple randomization,28 a suitable table was used with random integers from 0 to 99 read from an arbitrary place. For equal allocation, we took odd and even numbers to determine the opioid or nonopioid treatments, respectively. The clinical staff who were not a part of the project performed the random allocation and coded the 2 solutions to blind both the participants and the investigators.29 The inclusion of the patients in the study (participant enrollment) was conducted by the author who visited and treated the patients.
The subjects received an IANB injection of 1.8 mL of lidocaine 2% with 1 : 100,000 epinephrine after a confirmed positive response to the pulp tester. After 5 minutes, if the expected lip anesthesia was not present, the subjects received another IANB injection. When lip anesthesia was again not achieved after 5 more minutes, the subject left the study but received full proper treatment. The authors then examined all the subjects with lip anesthesia by EPT to record the initial sensitivity of the teeth. Having merely lip anesthesia is considered a sign of soft tissue anesthesia but not necessarily established pulpal anesthesia. The subjects then specified their pain perception on a Heft-Parker Visual Analogue Scale (HP-VAS) where 0 to less than 54 represented mild pain (including faint, weak, and mild pain sensation), 54 to less than 114 represented moderate pain, and more than 114 represented severe pain (including strong, intense, and maximum pain sensation). Only those patients with moderate to severe pain entered the study. Participation was based on sequential sampling until the inclusion of 60 patients was reached.
There were no financial or personal relationships with other people or organizations that could inappropriately influence the conduct or result of this study. The study was self-funded by the authors.
Study Groups
Control group (lidocaine + sterile water)
Thirty patients received intraligamentary injections of 0.4 mL lidocaine 2% with 1 : 100,000 epinephrine (Daropaksh) and 0.4 mL sterile distilled water.
Meperidine group
Thirty patients received intraligamentary injections of 0.4 mL lidocaine 2% with 1 : 100,000 epinephrine (Daropaksh) and 0.4 mL of 5% meperidine (20 mg).
Study Solutions
The authors followed the same protocol for the preparation of the study solutions as in previous reports.24,25 The clinical staff who were not a part of the project coded the 2 solutions to blind the authors.
Study Setting
After recording HP-VAS of the patients and their range of responses to EPT maximum output, the senior author utilized an intraligamentary syringe ERGOJECT (Anthogyr; Pearson Dental Supplies) to administer solutions via a 27-gauge 3.175-cm (1¼-in) standard short needle (Monoject; Sherwood Services) using the appropriate 5-mL syringe with an aspirating handle (Becton Dickinson & Co). The needle penetrated the periodontal ligament adjacent to the mesiobuccal and the distobuccal areas of each tooth to deliver 0.2 mL of the solution in each location over a 10-second period. One minute after injection, another practitioner recorded the response of the target teeth to the maximum output of EPT (Sybron Endo) every 4 minutes over a period of 17 minutes (minutes 1, 5, 9, 13, and 17). Success of intraligamentary injection was defined as 2 consecutive “no” responses to a maximum EPT output of 80, or an “up to mild pain” score on the HP-VAS during the treatment. The contralateral first or second molar (or any other posterior virgin tooth) was selected as the unanesthetized control to ensure that the pulp tester was operating properly and that the subject was responding appropriately during each experiment.
Statistics
The means of HP-VAS values and onset time of the 2 groups were analyzed using Student's t test. For comparison of the success rates of the 2 groups, McNemar's test was used. For comparison of EPT readings, we used the Mann-Whitney U test. The level of significance was established at P < .05.
RESULTS
Of the total of 30 patients in the control group with a median age of 31.4 ± 12.2, there were 13 males and 17 females. Of the 30 patients of the meperidine group with a median age of 37.7 ± 11.2, there were 18 males and 12 females. In total, 31 males and 29 females took part in the study, ranging in age from 18 to 65 years with a median age of 34.5 ± 11.6. All the participants of each group remained in this study, completed the treatment, and were included in the statistical analysis.
All the subjects before treatment responded to the EPT test within a range of 5–6 out of the maximum output of 80 and exhibited profound lip anesthesia following the IANB. None of the subjects needed a second block injection to achieve lip numbness. They all responded to the pulp tester within a range of 7–8 after injection. All of them also showed moderate to severe pain, with a mean of 121.9 ± 35.6 on HP-VAS during initial access cavity preparation, and therefore they needed a supplemental intraligamentary anesthetic injection.
In the control group (lidocaine + sterile water) prior to the PDL injection, 22 subjects (61.7%) responded to EPT on the 17th minute, compared to 15 subjects (50%) of the lidocaine plus meperidine group. No statistically significant differences were found between the 2 groups at the 17th minute regarding success rate (P = .1).
In the control group, after the PDL injection, 22 subjects with previously failed anesthesia reported a mean HP-VAS pain value of 120.4 ± 45.3 upon access cavity preparation, and upon initial file placement, 7 patients were pain free (Table).
Distribution of Different Responses Based on HP-VAS Scale to Stimulus (Access Cavity Preparation and Initial File Placement) Among Patients With Irreversible Pulpitis in the Study Groups
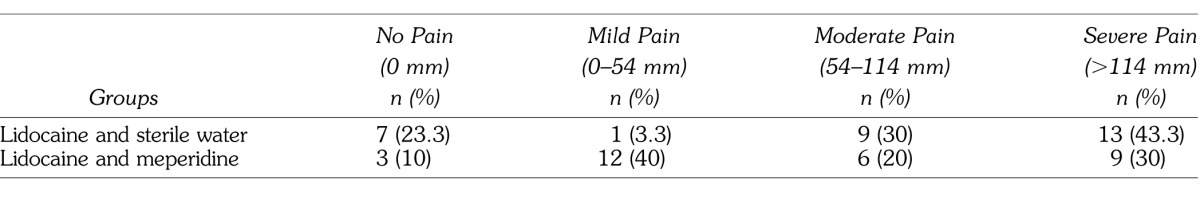
In the meperidine group, after PDL injection, 15 patients with previously failed anesthesia reported a mean HP-VAS pain value of 137.9 ± 34.6 upon access cavity preparation, and upon initial file placement, 12 subjects exhibited mild pain and only 3 subjects were pain free (Table).
No statistically significant differences were found between the 2 study groups in terms of the mean HP-VAS pain values during access cavity preparation (P < .3) and initial file placement (P < .2).
No significant adverse or side effects due to meperidine-containing intraligamentary injections were observed.
DISCUSSION
The findings of the present study suggest that the addition of 0.4 mL meperidine to 2% lidocaine with 1 : 100,000 epinephrine did not improve the anesthetic efficacy of intraligamentary injection for teeth with symptomatic irreversible pulpitis, and therefore we confirmed the null hypothesis.
All the subjects showed profound lip anesthesia (soft tissue anesthesia as opposed to pulp anesthesia) after receiving the initial IANB. Thus, none needed a second IANB injection to attain a numb lip, and all responded positively to the maximum output of pulp tester. The mean initial HP-VAS pain rating for both groups was 121.9 ± 35.6, which correlated to moderate to severe pain and represented irreversible pulpitis.25,30–32
To the best of our knowledge, only 2 studies throughout the dental literature have investigated the comparative efficacy of the local administration of meperidine. Goodman et al24 compared the degree of pulpal anesthesia of normal teeth with and without the addition of meperidine in a prospective, randomized, single-blind, crossover study. All subjects received either 1.8 mL of 2% (36 mg) lidocaine with 1 : 100,000 (18 μg) epinephrine, or 3.6 mL of a combination of 1% (36 mg) lidocaine with 1 : 100,000 (36 μg) epinephrine and 36 mg of meperidine. Successful pulpal anesthesia in the control and the meperidine groups ranged from 8 to 58% and from 0 to 17%, respectively. They concluded that the addition of meperidine significantly decreases the success of the IANB. They also found that the injection of only meperidine with epinephrine resulted in low rates of lip anesthesia and significantly low success of pulpal anesthesia. Bigby et al25 deposited the exact same solutions for their control and meperidine groups in a prospective, randomized, controlled, single-blind clinical trial on mandibular posterior teeth and concluded that the addition of meperidine to lidocaine administered in IANB did not improve the success rate of anesthesia in cases of irreversible pulpitis. Both these findings are in accord with our results.
Despite these recent findings, the application of meperidine in the 1990s literature has been widely supported.22 In a double-blind, randomized clinical study, Armstrong et al33 demonstrated the local anesthetic action of meperidine on peripheral nerves when the possibility of activation with central opiate receptors did not occur. Consistently, Maurette et al34 also found a synergistic effect when meperidine was used in combination with lidocaine for continuous spinal anesthesia. They also discussed that this synergistic effect might be offset by the unacceptable hemodynamic instability that intrathecal meperidine may cause. Yu et al20 suggested a superior anesthetic effectiveness for the combination of bupivacaine and meperidine compared to the bupivacaine alone for spinal anesthesia.
More recent studies have widely expressed that there is a need for far more reliable evidence for the inclusion of meperidine and other similar opioids in local anesthesia.22 For instance, despite the frequent application of additive opioids to local anesthetics for intrathecal anesthesia, there are not enough data for decisive conclusions17 on this technique.
Interaction or even antagonism between multiple sites of local anesthetic receptors,31 the histamine release induced by meperidine,18 or simply the further dilution of lidocaine25 might account for the lower incidence of anesthetic efficacy of the meperidine-added local anesthetics.
Using mouse models, Hassan et al35 found a reduced duration (less than 44%) of inferior orbital nerve block when lidocaine was added to meperidine compared to the nerve block with meperidine alone. On the other hand, mast cells are a potential important site for the histamine-dependent, peripheral actions of meperidine.18 Histamine acts as a vasodilator that is expected to help remove the agent from local sites.25 The concentration used in the present study mostly resembled those of the study of Atbaei and Mortazavi,32 who compared the anesthetic efficacy of the administration of 0.4 mL of 2% (8 mg) lidocaine with 1 : 80,000 (5 μg) epinephrine with that of 0.4 mL of 2% (8 mg) piroxicam combined with 1 : 80,000 (5 μg) epinephrine in postoperative pain management. The dosage used throughout the literature has not been standardized. Kanaa et al30 used 0.18 mL of 2% (3.6 mg) lidocaine plus 1 : 80,000 (2.25 μg) epinephrine with a success rate of 48% for the pain-free treatment of mandibular posterior permanent teeth with irreversible pulpitis. Nusstein et al36 applied 1.4 mL of 2% (28 mg) lidocaine plus 1 : 100,000 (14 μg) epinephrine for the intraligamentary pain management of mandibular posterior teeth with irreversible pulpitis and obtained a 56% success rate. Also, in a double-blind randomized controlled trial, Berlin et al37 compared the anesthetic efficacy of the intraligamentary deposition of 1.4 mL of 2% (28 mg) lidocaine with 1 : 100,000 (14 μg) epinephrine (74% success rate) with that of 1.4 mL of 4% (56 mg) articaine plus 1 : 100,000 (14 μg) epinephrine (86% success rate) on virgin first mandibular permanent molars. The success rate with the intraligamentary injection was lower in the present study (10–23%) compared to others in the literature. This may be attributed to the above-mentioned reasons and the fact that lidocaine in combination with either meperidine or sterile water, which was administered in the present study, contained the lower concentration of effective anesthetic drug. Also the present study has only included symptomatic irreversible pulpitis cases where the least success rates are expected.
Similar studies have mostly delivered the same standard dose of anesthetics but have halved the concentration of the anesthetic. To eliminate such biasing effect, we suggest additional studies with the application of long-lasting anesthetics, higher concentrations of the standard anesthetic, and higher concentrations of the epinephrine portion.
The pain intensity immediately after injection, access preparation, and initial file placement was not statistically different between the 2 study groups. This was consistent with the findings of the study of Rattan et al26 for the pain intensity prior to and immediately after injection and with those of Brkovic et al38 during the extraction of the third molars. These findings, however, do not support those of Elsharrawy and Elbaghdady39 for pain intensity upon access preparation, pulpotomy, and pulpectomy, which could be because of the lack of a definitive inclusion criterion, such as inclusion of maxillary posterior teeth, in their study.
Consistent with the findings of Brkovic et al,38 the 2 study groups did not show any statistically significant differences in terms of anesthesia depth assessed by EPT. The onset of anesthesia was not different with the addition of meperidine compared to the lidocaine injection with an equal volume of water, which was again consistent with the finding of Brkovic et al.38 Although the present study did not aim at measuring the duration of anesthesia, almost all our patients maintained profound local anesthesia until the 17th minute.
CONCLUSION
Within the limitations of the present study, it appears that the addition of meperidine as an opioid to 2% lidocaine with 1 : 100,000 epinephrine will not improve the anesthetic efficacy of a periodontal ligament injection in patients with irreversible pulpitis for whom an IANB was ineffective despite lip numbness. Further randomized controlled studies on the local administration of opioids alone or in combination of other agents for soft tissue and pulpal anesthesia are highly recommended.
REFERENCES
- 1.Nusstein J, Reader A, Beck FM. Anesthetic efficacy of different volumes of lidocaine with epinephrine for inferior alveolar nerve blocks. Gen Dent. 2002;50:372–375. [PubMed] [Google Scholar]
- 2.Mikesell P, Nusstein J, Reader A, Beck M, Weaver J. A comparison of articaine and lidocaine for inferior alveolar nerve blocks. J Endod. 2005;31:265–270. doi: 10.1097/01.don.0000140576.36513.cb. [DOI] [PubMed] [Google Scholar]
- 3.Ridenour S, Reader A, Beck M, Weaver J. Anesthetic efficacy of a combination of hyaluronidase and lidocaine with epinephrine in inferior alveolar nerve blocks. Anesth Prog. 2001;48:9–15. [PMC free article] [PubMed] [Google Scholar]
- 4.Yonchak T, Reader A, Beck M, Meyers WJ. Anesthetic efficacy of unilateral and bilateral inferior alveolar nerve blocks to determine cross innervation in anterior teeth. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001;92:132–135. doi: 10.1067/moe.2001.115720. [DOI] [PubMed] [Google Scholar]
- 5.Nusstein J, Kennedy S, Reader A, Beck M, Weaver J. Anesthetic efficacy of the supplemental X-tip intraosseous injection in patients with irreversible pulpitis. J Endod. 2003;29:724–728. doi: 10.1097/00004770-200311000-00010. [DOI] [PubMed] [Google Scholar]
- 6.Claffey E, Reader A, Nusstein J, Beck M, Weaver J. Anesthetic efficacy of articaine for inferior alveolar nerve blocks in patients with irreversible pulpitis. J Endod. 2004;30:568–571. doi: 10.1097/01.don.0000125317.21892.8f. [DOI] [PubMed] [Google Scholar]
- 7.Kennedy S, Reader A, Nusstein J, Beck M, Weaver J. The significance of needle deflection in success of the inferior alveolar nerve block in patients with irreversible pulpitis. J Endod. 2003;29:630–633. doi: 10.1097/00004770-200310000-00004. [DOI] [PubMed] [Google Scholar]
- 8.Khoury JN, Mihailidis S, Ghabriel M, Townsend G. Applied anatomy of the pterygomandibular space: improving the success of inferior alveolar nerve blocks. Aust Dent J. 2011;56:112–121. doi: 10.1111/j.1834-7819.2011.01312.x. [DOI] [PubMed] [Google Scholar]
- 9.Woodmansey K. Intraseptal anesthesia: a review of a relevant injection technique. Gen Dent. 2005;53:418–420. [PubMed] [Google Scholar]
- 10.Haas DA. Alternative mandibular nerve block techniques: a review of the Gow-Gates and Akinosi-Vazirani closed-mouth mandibular nerve block techniques. J Am Dent Assoc. 2011;142((suppl 3)):8S–12S. doi: 10.14219/jada.archive.2011.0341. [DOI] [PubMed] [Google Scholar]
- 11.Goldberg S, Reader A, Drum M, Nusstein J, Beck M. Comparison of the anesthetic efficacy of the conventional inferior alveolar, Gow-Gates, and Vazirani-Akinosi techniques. J Endod. 2008;34:1306–1311. doi: 10.1016/j.joen.2008.07.025. [DOI] [PubMed] [Google Scholar]
- 12.Zandi M. Seyedzadeh Sabounchi S. Design and development of a device for facilitation of Gow-Gates mandibular block and evaluation of its efficacy. Oral Maxillofac Surg. 2008;12:149–153. doi: 10.1007/s10006-008-0126-4. [DOI] [PubMed] [Google Scholar]
- 13.Katyal V. The efficacy and safety of articaine versus lignocaine in dental treatments: a meta-analysis. J Dent. 2010;38:307–317. doi: 10.1016/j.jdent.2009.12.003. [DOI] [PubMed] [Google Scholar]
- 14.Kingon A, Sambrook P, Goss A. Higher concentration local anaesthetics causing prolonged anaesthesia. Do they? A literature review and case reports. Aust Dent J. 2011;56:348–351. doi: 10.1111/j.1834-7819.2011.01358.x. [DOI] [PubMed] [Google Scholar]
- 15.Andrés JD, Monzó E. Regional techniques for day surgery: intraarticular anesthesia and analgesia. Tech Reg Anesth Pain Manage. 2000;4:54–61. [Google Scholar]
- 16.Westman L, Valentin A, Engstrom B, Ekblom A. Local anesthesia for arthroscopic surgery of the ankle using pethidine or prilocaine. Arthroscopy. 1997;13:307–312. doi: 10.1016/s0749-8063(97)90026-8. [DOI] [PubMed] [Google Scholar]
- 17.Popping DM, Elia N, Marret E, Wenk M, Tramer MR. Opioids added to local anesthetics for single-shot intrathecal anesthesia in patients undergoing minor surgery: a meta-analysis of randomized trials. Pain. 2012;153:784–793. doi: 10.1016/j.pain.2011.11.028. [DOI] [PubMed] [Google Scholar]
- 18.Akcasu A, Yillar DO, Akkan AG, Kuckhuseyin C. The role of mast cells in the genesis of acute manifestations following the intravenous injection of meperidine in dogs. J Basic Clin Physiol Pharmacol. 2009;20:67–72. doi: 10.1515/jbcpp.2009.20.1.67. [DOI] [PubMed] [Google Scholar]
- 19.Amir R, Argoff CE, Bennett GJ, et al. The role of sodium channels in chronic inflammatory and neuropathic pain. J Pain. 2006;7:S1–S29. doi: 10.1016/j.jpain.2006.01.444. [DOI] [PubMed] [Google Scholar]
- 20.Yu SC. Ngan Kee WD, Kwan AS. Addition of meperidine to bupivacaine for spinal anaesthesia for Caesarean section. Br J Anaesth. 2002;88:379–383. doi: 10.1093/bja/88.3.379. [DOI] [PubMed] [Google Scholar]
- 21.Mert T, Gunes Y, Guven M, Gunay I, Ozcengiz D. Comparison of nerve conduction blocks by an opioid and a local anesthetic. Eur J Pharmacol. 2002;439((1–3)):77–81. doi: 10.1016/s0014-2999(02)01368-7. [DOI] [PubMed] [Google Scholar]
- 22.Latta KS, Ginsberg B, Barkin RL. Meperidine: a critical review. Am J Ther. 2002;9:53–68. doi: 10.1097/00045391-200201000-00010. [DOI] [PubMed] [Google Scholar]
- 23.Karaaslan K, Yilmaz F, Gulcu N, Yigit B, Kocoglu H. The effect of prilocaine and prilocaine plus meperidine infiltration on the pain during nasal packing removal. Rhinology. 2007;45:321–324. [PubMed] [Google Scholar]
- 24.Goodman A, Reader A, Nusstein J, Beck M, Weaver J. Anesthetic efficacy of lidocaine/meperidine for inferior alveolar nerve blocks. Anesth Prog. 2006;53:131–139. doi: 10.2344/0003-3006(2006)53[131:AEOMFI]2.0.CO;2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bigby J, Reader A, Nusstein J, Beck M. Anesthetic efficacy of lidocaine/meperidine for inferior alveolar nerve blocks in patients with irreversible pulpitis. J Endod. 2007;33:7–10. doi: 10.1016/j.joen.2006.09.006. [DOI] [PubMed] [Google Scholar]
- 26.Rattan V, Arora S, Grover VK. Assessment of the effectiveness of peripheral administration of fentanyl with lidocaine in inflamed dentoalveolar tissues. Int J Oral Maxillofac Surg. 2007;36:128–131. doi: 10.1016/j.ijom.2006.09.007. [DOI] [PubMed] [Google Scholar]
- 27.Zhong B. How to calculate sample size in randomized controlled trial? J Thorac Dis. 2009;1:51–54. [PMC free article] [PubMed] [Google Scholar]
- 28.Altman DG, Bland JM. How to randomize. BMJ. 1999;319:703–704. doi: 10.1136/bmj.319.7211.703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kolahi J, Bang H, Park J. Towards a proposal for assessment of blinding success in clinical trials: up-to-date review. Community Dent Oral Epidemiol. 2009;37:477–484. doi: 10.1111/j.1600-0528.2009.00494.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kanaa MD, Whitworth JM, Meechan JG. A prospective randomized trial of different supplementary local anesthetic techniques after failure of inferior alveolar nerve block in patients with irreversible pulpitis in mandibular teeth. J Endod. 2012;38:421–425. doi: 10.1016/j.joen.2011.12.006. [DOI] [PubMed] [Google Scholar]
- 31.Argueta-Figueroa L, Arzate-Sosa G, Mendieta-Zeron H. Anesthetic efficacy of articaine for inferior alveolar nerve blocks in patients with symptomatic versus asymptomatic irreversible pulpitis. Gen Dent. 2012;60:e39–e43. [PubMed] [Google Scholar]
- 32.Atbaei A, Mortazavi N. Prophylactic intraligamentary injection of piroxicam (feldene) for the management of post-endodontic pain in molar teeth with irreversible pulpitis. Aust Endod J. 2012;38:31–35. doi: 10.1111/j.1747-4477.2010.00274.x. [DOI] [PubMed] [Google Scholar]
- 33.Armstrong PJ, Morton CP, Nimmo AF. Pethidine has a local anaesthetic action on peripheral nerves in vivo. Addition to prilocaine 0.25% for intravenous regional anaesthesia in volunteers. Anaesthesia. 1993;48:382–386. doi: 10.1111/j.1365-2044.1993.tb07008.x. [DOI] [PubMed] [Google Scholar]
- 34.Maurette P, Bonada G, Djiane V, Erny P. A comparison between lidocaine alone and lidocaine with meperidine for continuous spinal anesthesia. Reg Anesth. 1993;18:290–295. [PubMed] [Google Scholar]
- 35.Hassan HG, Youssef H, Renck H. Duration of experimental nerve block by combinations of local anesthetic agents. Acta Anaesthesiol Scand. 1993;37:70–74. doi: 10.1111/j.1399-6576.1993.tb03601.x. [DOI] [PubMed] [Google Scholar]
- 36.Nusstein J, Claffey E, Reader A, Beck M, Weaver J. Anesthetic effectiveness of the supplemental intraligamentary injection, administered with a computer-controlled local anesthetic delivery system, in patients with irreversible pulpitis. J Endod. 2005;31:354–358. doi: 10.1097/01.don.0000140565.88940.60. [DOI] [PubMed] [Google Scholar]
- 37.Berlin J, Nusstein J, Reader A, Beck M, Weaver J. Efficacy of articaine and lidocaine in a primary intraligamentary injection administered with a computer-controlled local anesthetic delivery system. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;99:361–366. doi: 10.1016/j.tripleo.2004.11.009. [DOI] [PubMed] [Google Scholar]
- 38.Brkovic B, Gardasevic M, Roganovic J, Jovic N, Todorovic L, Stojic D. Lidocaine+clonidine for maxillary infiltration anaesthesia: parameters of anaesthesia and vascular effects. Int J Oral Maxillofac Surg. 2008;37:149–155. doi: 10.1016/j.ijom.2007.07.019. [DOI] [PubMed] [Google Scholar]
- 39.Elsharrawy EA, Elbaghdady YM. A double-blind comparison of a supplemental interligamentary injection of fentanyl and mepivacaine with 1 : 200,000 epinephrine for irreversible pulpitis. J Pain Symptom Manage. 2007;33:203–207. doi: 10.1016/j.jpainsymman.2006.07.020. [DOI] [PubMed] [Google Scholar]


