Abstract
The purpose of this randomized, double-blind clinical study was to evaluate the effectiveness of a larger-bore compared with a standard-bore dental local anesthetic needle of the same gauge in reducing pain during inferior alveolar (IA) and long buccal (LB) nerve block injections. Twenty active duty military or Department of Defense beneficiaries undergoing dental treatment were anesthetized using a split-mouth design with 4 anesthetic dental injections. Both sides of the mouth received IA nerve block and LB nerve injections, one using the 27-gauge large-bore Septoject XL needle and other using a 27-gauge standard-bore Septoject needle. Patients rated the pain experienced with each method using a visual analogue scale (VAS). The IA injection mean VAS score and standard deviation were 38.9 ± 22.7 mm and 37.1 ± 22.4 mm, respectively, for the larger and standard-bore needles. The LB injection mean VAS score and standard deviation were 33.5 ± 22.8 mm and 35.1 ± 19.6 mm, respectively, for the larger and standard-bore needles. The data were analyzed with a paired t test (α = .05). No significant difference was found between the IA (P = .70) or LB injections (P = .73). The use of a larger-bore 27-gauge needle did not reduce pain on injection compared with the standard-bore 27-gauge needle.
Key Words: Bore size, Needle, Pain
Since its inception, the field of dental medicine has had the challenge of trying to create a painless experience for the patient. The fear of pain attributed to anesthetic needle injection has been cited as an obstacle in providing appropriate dental care.1–3 A variety of patient management techniques have been attempted to improve patient comfort during dental anesthetic administration, including but not limited to smaller gauge needle sizes, slow computer-regulated administration, distraction techniques, vibrating devices, and topical agents (refrigerants and anesthetics). Characteristics of pain associated with injections have been described as (1) irritation from the antiseptic used on the skin, (2) properties of the parenteral formulation, (3) sensitivity of the tissue at the injection site, (4) mechanical trauma caused by needle penetration into the tissue, and (5) distension resulting from discharge of the contents of the syringe.4,5
Several clinical studies have shown that the application of topical anesthetic to dry oral mucosa for at least 2 minutes is effective in the reduction of injection pain.6–11 Other studies did not find a significant difference between the use of topical anesthetic when compared with placebo or other methods.12–15 The effectiveness of the application of topical anesthesia may also depend on the site of injection. For example, the pterygotemporal depression is the entrance site for the needle in an inferior alveolar (IA) nerve block injection. At this site, the use of topical anesthetic produced a slight but not substantially relevant reduction of pain.6,9
Several studies investigating the most common size gauge needles in dentistry (ie, 25, 27, and 30 gauge) have shown that there is no statistical or clinical difference in pain perception based on needle gauge.5,16,17 It has been hypothesized that the needle's bevel sharpness is most important in pain avoidance, not the gauge of the needle. Sharp needles produce less trauma to the tissue wall, resulting in less pain.18–20
Recently, Septodont introduced a series of dental needles of the same gauge as commonly used dental needles but that incorporated a larger internal bore. Septoject XL is marketed as a single-use, 27-gauge stainless-steel dental needle that has a unique feature of an enlarged bore. Septodont claims that the “enlarged bore (43% wider than a standard needle) reduces the level of pressure during injection, thus leading to less pain for the patient.”21 The Septoject XL has the same triple-bevel needle design with a polished and siliconized cannula as standard-bore Septoject needles, and they are available in the same length and same external diameter (27 gauge). Both Septoject and Septoject XL are indicated for the routine administration of dental local anesthetics.
The purpose of this study was to evaluate the subjective reduction of pain during IA and long buccal (LB) injections with use of the 27-gauge Septoject XL Block and Septoject XL Infiltration dental needles (Septodont, Lancaster, Penn) compared with the standard-bore 27-gauge dental local anesthetic needles (Septoject long and Septoject short) that were used as a control. The IA and LB injections were selected as these are commonly used in dentistry and have been used in similar investigations in the past. The patients' experienced pain was evaluated through the use of a visual analogue scale (VAS). The VAS is a 1 to 10 rating scale, with 0 being no pain and 10 being worst possible pain. The VAS has been shown to be a reliable, consistent self-reporting technique used to measure subjective phenomena in an experimental setting, specifically a patient's level of pain.22–24 The null hypothesis to be tested was that there would be no significant difference in VAS pain scores based on needle bore size.
METHODS
The patient sample for this study consisted of 20 active duty or Department of Defense beneficiaries 18 years of age or older who were undergoing routine dental treatment that required bilateral IA and LB nerve blocks. The patients were selected from a pool of patients available for treatment at Wilford Hall Ambulatory Surgical Center (WHASC), Dunn Dental Clinic, JBSA-Lackland, Texas. All patients selected were in good general health as indicated by the American Society of Anesthesiologists I or II classification. The Institutional Review Board at WHASC approved the protocol and the informed consent document. All subjects signed an informed consent document prior to any study-related procedures being conducted. Routine operative or periodontal scaling and root planing with local anesthesia in bilateral posterior areas of the mandible were the specific treatments selected for the study. Dental patients with a chronic pain condition were excluded from this study. The sample size of 20 subjects provided 80% power to detect a 0.75 standard deviation when using a paired t test to compare the VAS scores for the 2 treatments (α = .05).
A randomized, double-blind, split-mouth design was conducted with 4 anesthetic dental injections inside the patient's mouth using 2% lidocaine with 1:100,000 epinephrine (Henry Schein, Melville, NY) after application of a topical anesthetic gel. The patients received a total of 2 IA nerve injections and 2 LB nerve injections with a 5-minute interval between sides. One side of the mouth received the IA nerve injection using the 27-gauge Septoject XL Block and the LB nerve injection with Septoject XL Infiltration. To serve as a control, the other side received the same injections using the 27-gauge standard-bore needles, Septoject long needle and Septoject short needle, using the same injection technique. The sequence of treatment for each patient was randomized using a block design to determine the order of the needles and which side was injected first. The subjects were randomized such that 10 received injections with the large bore first and 10 received injections with the standard bore first. Also, the study was designed such that 10 subjects were injected on left side first and the other 10 were injected on the right side first.
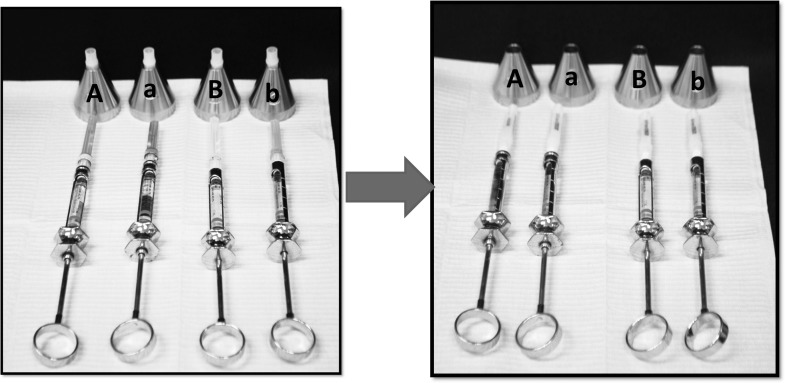
The primary investigator (PI) used sterilized metal syringes that were prescored using a bur measured with a digital caliper. The portion of the syringe that carried the anesthetic cartridge was divided into quarters and scored at each quarter. The syringes were arranged as shown in Figure 1. The PI loaded the 4 scored syringes with the anesthetic cartridges and attached each of the different types of needle. The 4 loaded syringes were laid on a patient napkin on the counter, and the PI left the room. Needle-stick protectors were permanently scored with “A” and “a” and “B” and “b.” The uppercase letters designated long needles, and the lowercase letter designated a short needle. The letter “A/a” was used to represent the needles to be used during the first series of injections, and the letter “B/b” was used to represent the needles to be used in the second series of injections. Because the manufacturer's needle caps are also color coded by bore size and length, the associate investigator removed the color-coded caps and placed each syringe in the mounted needle-stick protector according to the predetermined randomized design. Other than the capitalized or lowercase letters on the needle-stick protector signifying which needles were long or short, the PI and the patient were unaware of the bore size of the needle.
Figure 1.
Syringe arrangement.
Benzocaine 20% topical gel (Topex, Sultan Dental Products, Hackensack, NJ) was used to anesthetize the sites receiving the IA and LB nerve block injections. The method of application was as follows: (1) the gel was preloaded in a syringe, and 0.1 mL was placed on a cotton-tip applicator; (2) the mucosa at the sites of injection was dried with a 2- × 2-cm gauze; and (3) the gel on the cotton-tip applicator was applied to the mucosa for 2 minutes.
After placement of the topical anesthetic, the PI took the syringe from the “A” needle protector for the first IA injection and the associate investigator provided instruction on which side of the mouth to inject based on the randomized block design. Three quarters of a cartridge was administered over 15 seconds. A metronome application (Mobile Metronome Version 1.2.4) and headphones were used to pace the PI during the delivery of anesthetic. After injection, the patient was allowed to rate the pain experienced using the VAS on a preprinted form. The PI then picked up the syringe marked “a,” and one quarter of the cartridge was administered during the LB block over 5 seconds on the same side. The patient then rated this injection using the VAS on a separate preprinted form. The PI repeated this process on the other side with the syringes seated in needle protectors “B” and “b.”
As stated, the patient's subjective report of injection pain was recorded using the VAS. The VAS is a 100-mm horizontal line with descriptive anchors at each end. The left end was labeled no pain and the right end was labeled worst possible pain. The patient was instructed to mark a vertical line within the 100-mm scale to indicate his or her level of discomfort after each injection. The VAS pain score was calculated by measuring the millimeter distance from the left end of the scale using a digital caliper (Northern Tool, Burnsville, Minn). A larger score translated to a higher pain intensity experienced by the patient. The mean and standard deviation of the VAS values were determined in each group. Data were analyzed with a paired t test (α = .05).
Industry standards for needle gauge have been in place for many years, but not for internal bore sizes. Wittrock and Fischer25 showed there are variations in internal diameters with needles of the same gauge. To assess the difference in bore size, the internal diameter of each needle type used in the study was measured with a measuring microscope (Axio Zoom.V16, Carl Zeiss, Thornwood, NY). The internal diameter of 3 needles per needle type was measured 5 times, and the mean diameter and standard deviation was determined per needle type. The outside diameter of each needle was also measured with a digital micrometer (Northern Tool).
RESULTS
The participant pool was made up of 14 men and 6 women whose ages ranged from 21 to 77 years, with an average age of 43.2 years. Based on study design, 10 patients received injections on the right side first and 10 received treatment on the left side first. Ten patients received injections with the large-bore needles (Septoject XL) first, and 10 received injections with the standard-bore needles (Septoject) first.
The mean VAS score and standard deviation for the IA injection were 38.9 ± 22.7 for the large-bore needles and 37.1 ± 22.4 for the standard-bore needles. For the LB injection, the mean VAS score and standard deviation were 33.5 ± 22.8 for the large-bore needles and 35.1 ± 19.6 for standard-bore needles. No significant difference was found between groups for the IA (P = .70) or the LB injections (P = .73).
As shown in Figure 2, the Septoject XL Block and the Septoject long needles had a mean internal diameter of 250 ± 2 μm and 197 ± 4 μm, respectively. The internal diameter of the large-bore needle was found to be 27% greater than the standard-bore needle, with a 61% greater surface area. Figure 3 demonstrates that the Septoject XL Infiltration and the Septoject short needles had a mean internal diameter of 239 ± 2 μm and 186 ± 10 μm, respectively. The internal diameter of the large-bore needle was 29% greater than the standard-bore needle with a 67% greater surface area. The external diameter of all 4 needle types was consistently 410 μm.
Figure 2.
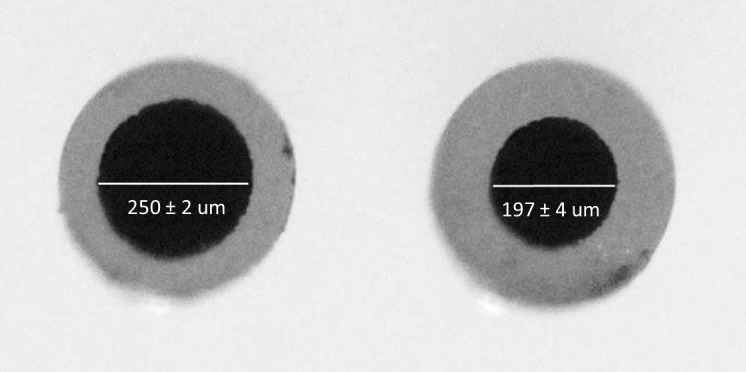
Septoject XL Block and the Septoject long needles internal diameter (Axio Zoom V16 Carl Zeiss, Thornwood, NY).
Figure 3.
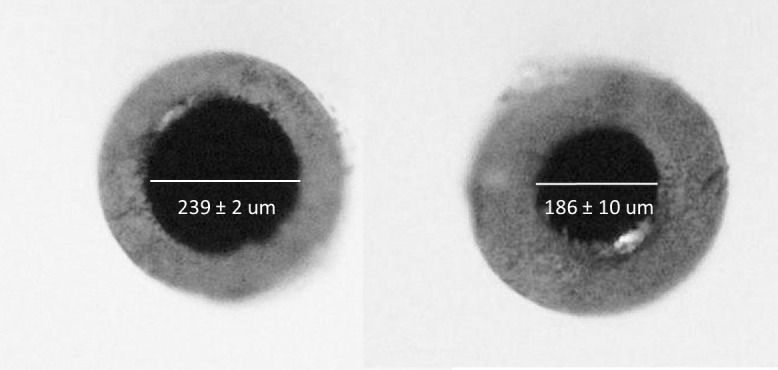
Septoject XL Infiltration and the Septoject short needles internal diameter (Axio Zoom V16 Carl Zeiss, Thornwood, NY).
DISCUSSION
Several studies have investigated pain perception based on the gauge of the needle and found no statistical difference between different gauges.5,16,17 The manufacturer advertises less pain on injection with their larger-bore needles; however, this is the first published study that assessed the effect of needle bore size on pain with anesthetic injections. Septodont reports that the enlarged bore is 43% wider than a standard needle. In this study, measurements of the Septodont large-bore needles were 28% greater with a 64% average increase in surface area than the standard-bore needle types. Septodont claims that the enlarged bore size reduces the level of pain by reducing the level of pressure required to expel the anesthetic during injection. No significant difference was found in the subjective pain experience of subjects between the large-bore needles and the standard-bore needles in this randomized, double-blind, split-mouth clinical trial. Therefore, the null hypothesis was not rejected.
Strengths of this study include the split-mouth design. The same subject experienced injections using both bore sizes and immediately rated the pain after injection. Since the flow rate of the local anesthetic into tissues may influence the pain experienced by subjects, the injection rate was carefully controlled in this study by using an audible metronome to pace the PI in the delivery of the anesthetic over the specific time interval for each of the 2 injection sites.
One limitation of this study is that only 1 time interval was used per injection site (ie, 15 seconds for the IA injection and 5 seconds for the LB injection). It may be possible that other time intervals or rates of injection may have shown a significant effect on the perception of pain between the different bore sizes.
Another potential limitation of this study is that it evaluated the entire pain injection experience, not just the pain during anesthetic deposition. Differentiating the needle penetration experience from the deposition experience may have some merit when investigating new equipment or techniques, but it may not be clinically relevant as patients are not accustomed to separating the 2 experiences.
Pain generated by injections may be caused by the penetration of the needle into the skin and by the solution being deposited into target tissues.26 The Septoject XL manufacturer maintains that the larger bore size produces a less painful injection experience for the patient. While the pressure required to push the plunger during local anesthetic injection may be subjectively lower as perceived by the provider, the soft tissues where the anesthetic is deposited are still distended by the same volume of fluid at a flow rate dictated by the provider. Thus, the ease of pressure combined with the provider's muscle memory may inadvertently increase flow rate and produce rapid fluid distention and a nociceptive response. This investigation attempted to control for operator variability by standardizing the flow rate. It is feasible that any potential benefits of reduced pain using a larger bore size, as used in this study, may be diminished by the pain associated with the original entry of the needle. To control for this and to reflect common practice, standardized application of topical anesthetic was used prior to the intraoral injections. Research has been equivocal in the effectiveness of topical anesthetics in reducing pain on injection, especially in the IA area.6–15 A recent study evaluating the effect of an intraoral vibration device during an IA injection found a significant reduction in the overall pain of injection.27 The vibratory device was present on the tissue before the original penetration of the needle and during the deposition of the anesthetic solution, potentially contributing to the overall reduction of the sensation of pain.
According to Engel,28 pain is an unpleasant experience that is influenced by biological, psychological, and sociological factors. In short, past pain experiences, expectations of pain, and cultural differences can have a significant impact on the pain experience that goes beyond the biological activation of nociceptors. This individualization of the pain experience explains why equal and measurable biologic parameters of pain (i.e., injection flow rate) can produce different subjective pain responses. It may be possible that past injection experience and expectations of pain by subjects negated any benefits attained by increased bore size in this investigation.
The results of this randomized, split-mouth, double-blind clinical study suggest that the use of a large-bore needle did not reduce the overall pain on injection compared with a standard-bore needle.
DISCLOSURE
The views expressed in this study are those of the authors and do not reflect the official policy of the United States Air Force, the Department of Defense, or the United States government. The authors do not have any financial interest in the companies whose materials are discussed in this article.
REFERENCES
- 1.Bernstein DA, Kleinknecht RA, Alexander LD. Antecedents of dental fear. J Public Health Dent. 1979;39:113–124. doi: 10.1111/j.1752-7325.1979.tb02932.x. [DOI] [PubMed] [Google Scholar]
- 2.Milgrom P, Coldwell SE, Getz T, Weinstein P, Ramsay DS. Four dimensions of fear of dental injections. J Am Dent Assoc. 1997;128:756–766. doi: 10.14219/jada.archive.1997.0301. [DOI] [PubMed] [Google Scholar]
- 3.Kosaraju A, Vandewalle K. A comparison of a refrigerant and a topical anesthetic gel as preinjection anesthetics: a clinical evaluation. J Am Dent Assoc. 2009;140:68–72. doi: 10.14219/jada.archive.2009.0020. [DOI] [PubMed] [Google Scholar]
- 4.Ballard BE. Biopharmaceutical considerations in subcutaneous and intramuscular drug administration. J Pharm Sci. 1968;57:357–378. doi: 10.1002/jps.2600570301. [DOI] [PubMed] [Google Scholar]
- 5.Fuller NP, Menke RA, Meyers WJ. Perception of pain to three different intraoral penetrations of needles. J Am Dent Assoc. 1979;99:822–824. doi: 10.14219/jada.archive.1979.0384. [DOI] [PubMed] [Google Scholar]
- 6.Evers H, Haegerstam G. Introduction to Dental Local Anesthesia. 2nd ed. Fribourg Switzerland: Mediglobe SA Publishing; 1990;29–30:59–87. [Google Scholar]
- 7.Kincheloe JE, Mealiea WL, Jr, Mattison GD, Seib K. Psychophysical measurement on pain perception after administration of a topical anesthetic. Quintessence Int. 1991;22:311–315. [PubMed] [Google Scholar]
- 8.Hutchins HS, Jr, Young FA, Lackland DT, Fishburne CP. The effectiveness of topical anesthesia and vibration in alleviating the pain of oral injections. Anesth Prog. 1997;44:87–89. [PMC free article] [PubMed] [Google Scholar]
- 9.Nakanishi O, Haas D, Ishikawa T, Kameyama S, Nishi M. Efficacy of mandibular topical anesthesia varies with the site of administration. Anesth Progress. 1996;43:14–19. [PMC free article] [PubMed] [Google Scholar]
- 10.Rosivack RG, Koenigsberg SR, Maxwell KC. An analysis of the effectiveness of two topical anesthetics. Anesth Progress. 1990;37:290–292. [PMC free article] [PubMed] [Google Scholar]
- 11.Vickers ER, Punnia-Moorthey A. A clinical evaluation of three topical anesthetic agents. Aust Dent J. 1992;37:266–270. [PubMed] [Google Scholar]
- 12.Gill CJ, Orr DL. A double-blind crossover comparison of topical anesthetics. J Am Dent Assoc. 1979;98:213–214. doi: 10.14219/jada.archive.1979.0476. [DOI] [PubMed] [Google Scholar]
- 13.Keller BJ. Comparison of the effectiveness of two topical anesthetics and a placebo in reducing injection pain. Hawaii Dent J. 1985;16:10–11. [PubMed] [Google Scholar]
- 14.Martin MD, Ramsay DS, Whiteny C, Fiset L, Weinstein P. Topical anesthesia: differentiating the pharmacological and psychological contributions to efficacy. Anesth Progress. 1994;41:40–47. [PMC free article] [PubMed] [Google Scholar]
- 15.Roghani S, Duperon DF, Barcohana N. Evaluating the efficacy of commonly used topical anesthetics. Pediatr Dent. 1999;21:197–200. [PubMed] [Google Scholar]
- 16.Mollen AJ, Ficara AJ, Provant DR. Needles—25 gauge versus 27-gauge—can patients really tell? Gen Dent. 1981;29:417–418. [PubMed] [Google Scholar]
- 17.Flanagan T, Wahl MJ, Schmitt MM, Wahl JA. Size doesn't matter: needle gauge and injection pain. Gen Dent. 2007;55:216–217. [PubMed] [Google Scholar]
- 18.Lehtinen R. Penetration of 27- and 30-gauge dental needles. Int J Oral Surg. 1983;12:444–445. doi: 10.1016/s0300-9785(83)80036-2. [DOI] [PubMed] [Google Scholar]
- 19.Forrest JO. A survey of the equipment of local anesthesia. Br Dent J. 1968;124:303–309. [PubMed] [Google Scholar]
- 20.Farsakian LR, Weine FS. The significance of needle gauge in dental injections. Compend Contin Educ Dent. 1991;12:262, 264–268. [PubMed] [Google Scholar]
- 21.Septodont. Septoject XL dental needle. Available at: http://www.septodontusa.com/sites/default/files/SeptojectXL_0.pdf. Accessed September 1, 2012. [Google Scholar]
- 22.Price DD, McGrath PA, Rafii A, Buckingham B. The validation of visual analogue scales as ratio scale measures for chronic and experimental pain. Pain. 1983;17:45–56. doi: 10.1016/0304-3959(83)90126-4. [DOI] [PubMed] [Google Scholar]
- 23.Miller MD, Ferris DG. Measurement of subjective phenomena in primary care research: the visual analogue scale. Fam Pract Res J. 1993;13:15–24. [PubMed] [Google Scholar]
- 24.Price DD, Bush FM, Long S, Harkins SW. A comparison of pain measurement characteristics of mechanical visual analogue and simple numerical rating scales. Pain. 1994;56:217–226. doi: 10.1016/0304-3959(94)90097-3. [DOI] [PubMed] [Google Scholar]
- 25.Wittrock JW, Fischer WE. J. The aspiration of blood through small-gauge needles. Am Dent Assoc. 1968;76:79–81. doi: 10.14219/jada.archive.1968.0014. [DOI] [PubMed] [Google Scholar]
- 26.Burns CA, Ferris G, Feng C, Cooper JZ, Brown MD. Decreasing the pain of local anesthesia: a prospective, double-blind comparison of buffered, premixed 1% lidocaine with epinephrine versus 1% lidocaine freshly mixed with epinephrine. J Am Acad Dermatol. 2006;51:128–131. doi: 10.1016/j.jaad.2005.06.043. [DOI] [PubMed] [Google Scholar]
- 27.DiFelice M, Maller S, Hancock R, Vandewalle K. Effects of a vibratory device on pain from anesthetic injections. Compend Cont Educ Dent. 2014;34:2–5. [PubMed] [Google Scholar]
- 28.Engel GL. The need for a new medical model: a challenge for biomedicine. Science. 1977;196:129–136. doi: 10.1126/science.847460. [DOI] [PubMed] [Google Scholar]