Abstract
Although, historically, the norepinephrine system has attracted the majority of attention in the study of the stress response, the dopamine system has also been consistently implicated. It has long been established that stress plays a crucial role in the pathogenesis of psychiatric disorders. However, the neurobiological mechanisms that mediate the stress response and its effect in psychiatric diseases are not well understood. The dopamine system can play distinct roles in stress and psychiatric disorders. It is hypothesized that, even though the dopamine (DA) system forms the basis for a number of psychiatric disorders, the pathology is likely to originate in the afferent structures that are inducing dysregulation of the DA system. This review explores the current knowledge of afferent modulation of the stress/DA circuitry, and presents recent data focusing on the effect of stress on the DA system and its relevance to psychiatric disorders.
Keywords: dopamine, stress, psychiatric disorders, hippocampus, amygdala
1. Introduction
Stress is generally defined as any stimulus that may create a challenge to the homeostasis of an organism (for review, see [1]). Thus, stressful stimuli elicit many physiological brain responses designed to react to a possible danger. Indeed, activation of the hypothalamic–pituitary–adrenal (HPA) axis, which triggers the ‘fight-or-flight’ response, is the major neuroendocrine and physiological stress response to a threat from a dangerous situation [2]. The HPA axis is a network of brain and peripheral systems; it contains the hypothalamus, which releases corticotropin-releasing factor (CRF) and projects to the anterior pituitary, which secretes adrenocorticotropic hormone (ACTH). The end product of HPA axis activation (i.e. the release of glucocorticoids by the adrenal gland) serves to alert an organism to environmental and physiological changes and to maintain homeostasis [3]. Therefore, the organism needs this stress response in order to survive such situations; however, stress and inadequate adrenocortical activity can be detrimental because it can precipitate a number of pathological conditions, such as drug abuse [4], and major depressive [5] or psychotic [6] disorders. The HPA axis is controlled by a diverse set of afferents, and in particular by limbic system-associated regions such as the prefrontal cortex (PFC), the nucleus accumbens (NAc), the amygdala and the hippocampus [7]. Another core neuroendocrine response to stressful stimuli is the activation of the autonomic nervous system, which results in a rapid release of noradrenaline in the brain, by activation of locus coeruleus (LC) neurons. The HPA axis and the LC–norepinephrine (NE) system are the two main brain networks that are systematically associated with stress. However, it has become more and more evident that the dopamine (DA) system plays a key role in the response to stress, and in particular in the pathological response observed in many psychiatric disorders. The DA system plays a major role in the processing of natural and artificial rewards. Indeed, it has been proposed that mesolimbic DA mediates the hedonic aspects of rewarding stimuli [8], and that it acts as a learning signal for behavioural reinforcement [9]. Numerous studies have also reported that DA release is increased in response to aversive stimuli in animals, which suggests that DA is likely to be involved in motivation and attention processes underlying the behavioural response to relevant stimuli, whether aversive or rewarding [10,11]. Disruption in the DA system has been implicated in numerous psychiatric and neurological disorders, including schizophrenia, Parkinson's disease, drug abuse and major depressive disorders (MDDs). Although many studies have defined the basic and pathological function of the DA system in the brain, unravelling the complex afferent modulation of DA neuron activity is crucial to finding adequate and effective therapeutic approaches to treat several disorders. Indeed, many disorders are more likely to originate in afferent structures involved in the control of the DA system. This review summarizes current knowledge of afferent modulation of the stress/DA circuitry, and presents recent data focusing on the effect of stress on the DA system and its relevance to psychiatric disorders.
2. Stress and norepinephrine system
The catecholaminergic system has been repeatedly linked to stress responses. In particular, the LC–NE system plays a critical role in the regulation of behavioural states, including the stress responses, and may serve to enhance the state of arousal in order to adapt to challenging situations (for review, see [3]). The LC–NE system is activated by a large variety of stressors, including restraint [12], footshocks [13] and social stress [14]. In particular, after stress exposure, there is an increase in the activity of LC neurons [15], as well as an increase in the NE turnover in regions to which LC neurons project [16]. Lesions of the LC fail to prevent HPA axis hyperactivity in response to chronic stress but attenuate neuroendocrine hormonal responses to acute restraint stress [17], suggesting that the LC–NE system promotes physiological responses to stress. Moreover, activation of LC neurons with CRF has the same behavioural effect as acute stress [18]. However, the LC does not project directly to the HPA axis but also to various stress-related structures such as the amygdala and the hippocampus, which in turn send projections to the HPA axis [19]. The ventral subiculum of the hippocampus (vSub), the primary output of the hippocampus, receives dense innervation from the LC–NE system [20] and is implicated in the processing of contextual information [21]. As such, the vSub is a key structure in the stress response, because the context in which the stressor takes place is essential to effectively guide the adaptive response of an organism [22]. This is consistent with an increase in the expression of Fos in the hippocampus in rats exposed to various stressors, including restraint, swim and novelty stress [23]. Studies have shown that the LC–NE system is a potent modulator of vSub neuron activity, inducing an inhibition or activation of vSub neurons, which can contribute to stress adaptation [24]. Moreover, footshocks activate the majority of neurons in the vSub, which is correlated with responses to LC stimulation in vSub neurons [25]. The vSub innervates several limbic forebrain structures, such as the PFC and the amygdala, that in turn have projections to hypothalamic paraventricular neurons, suggesting that the vSub has an upstream influence on limbic stress integration [26], which might affect homeostasis. The amygdala, and in particular the basolateral nucleus (BLA), which also receives a strong LC projection [19], is similarly activated during stress [27], and reciprocal activation exists between vSub and BLA inputs [25]. Levels of NE increase in the BLA during stress exposure [28], and the BLA neurons themselves respond to stressful stimuli that have been shown to also activate LC neurons [29]. Maintained or repeated stressors produce morphological effects on the hippocampus and BLA, such as dendritic atrophy in the hippocampus, and increases in dendrites and spine density in the BLA [30]. A strong correlation exists between synaptic plasticity and morphological changes in spines [31]. For example, acute stress induces an increase in adrenergic-dependent long-term potentiation in the BLA [32], which suggests that dysfunctional stress integration, as observed in psychiatric disorders, may involve dysregulation in this circuitry. As mentioned, the mPFC is also a crucial component in the responses to stressful stimuli. It is selectively activated by psychological and social stressors [33], and is known to modulate neuroendocrine function during stress via modulation from the LC–NE system [34]. Moreover, long-term potentiation in the BLA–PFC pathway is inhibited by prior exposure to inescapable stress [35], as well as disruption of synaptic plasticity in the PFC–BLA pathway [36], suggesting that these reciprocal interactions might also play a significant role in the stress response.
Although, historically, the NE system is associated with stress responses, several studies have also implicated the DA system in the stress response.
3. The dopamine system
Neurochemical studies have demonstrated that the DA system is activated by maintained stressful stimuli [37]. Repeated restraint stress alters the response of the mesolimbic DA system to a stressor, and repeated stressors such as tail-pinch facilitate the acquisition of self-administration of psychostimulants such as cocaine and amphetamine (for review, see [37]). Neonatal lesions of the ventral tegmental area (VTA) alter the normal hormonal response to stress in adults, indicating that the DA system may have an influence on the HPA axis [38]. The electrophysiological state of the DA system of the VTA has been extensively studied (for review, see [39,40]). Thus, in vivo studies show that half of the DA neurons located in the VTA are inactive and not firing spontaneously [41]. These neurons are held at a constant hyperpolarized, inactive state via an inhibitory GABAergic influence from the ventral pallidum (VP). Indeed, inactivation of pallidal afferents releases the neurons from GABAergic inhibition, enabling them to fire spontaneously [42]. Of those that are firing spontaneously, two types of pattern are observed and regulated by different systems. Thus, DA neurons display an irregular, single-spike firing pattern (or ‘tonic’ activity), as well as a burst firing pattern (or ‘phasic’ activity) [43,44]. The phasic pattern is dependent on glutamatergic afferent input [44], in particular those arising from the pedunculopontine tegmentum (PPTg) [45]. Phasic burst firing is believed to be the behaviourally salient output of the DA system that modulates goal-directed behaviour (for review, see [39]), and phasic changes in bursting occur in response to a conditioned stimulus, or after a primary reward, and have been shown to mediate prediction error response in conscious primates [46] and rats [47]. Although spontaneous motor behaviour is absent and sensory processing is dampened in anaesthetized animals, and burst discharge to a stimulus response is non-existent, as shown during the deep sleep phase in cats [48], burst properties and tonic discharge and their regulation are comparable with those observed in behaving animals [49,50]. It should be noted that in anaesthetized rats, burst discharge has been observed in response to a visual stimulus after disinhibition of the superior colliculus [51]. Moreover, in awake behaving animals, spontaneous bursts have the same properties as bursts produced in response to a stimulus [49]. In addition, drugs that block burst firing, such as NMDA antagonists injected into the VTA [52], also interfere with learned responses [53]. Therefore, spontaneous bursts studied in anaesthetized animals are analogous in form and regulation with bursts produced in response to a stimulus in awake behaving animals.
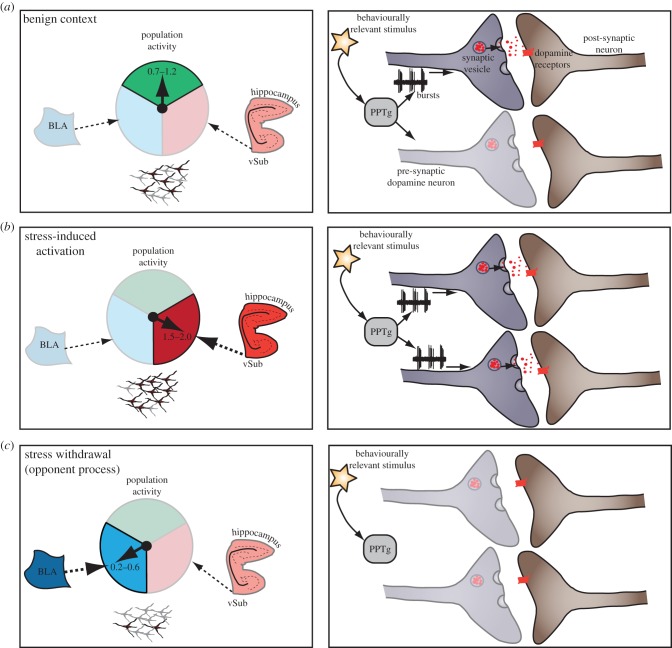
The pacemaker tonic firing activity, in contrast, supplies a baseline DA activity state [42] that determines extrasynaptic DA concentrations. Activation of the vSub induces an increase in the number of spontaneously active DA neurons (i.e. population activity) but has no effect on firing rate or bursting activity [54]. This has been shown to occur via a polysynaptic pathway through the NAc and the VP [55]. Phasic activation of burst firing in DA neurons can only occur in neurons that are depolarized and firing spontaneously; in contrast, a hyperpolarized DA neuron exhibits a magnesium block of the NMDA channel and cannot burst fire upon stimulation by NMDA [56]. Consequently, the vSub controls the number of DA neurons that can be phasically activated by the PPTg by setting the tonic discharge of DA neurons. Therefore, the PPTg provides the ‘signal’, and the vSub is the ‘gain’ of this signal. The vSub plays a role in context-dependent processing and its influence can vary depending on the environment. Thus, in a benign context, relevant stimuli will activate the PPTg, allowing the moderate proportion of DA neurons that are set to be active by the vSub to fire in bursts (figure 1a).
Figure 1.
Dopamine (DA) neuron population activity is regulated by two structures, the ventral subiculum of the hippocampus (vSub) and the basolateral amygdala (BLA). (a) A balance between these circuits that would be present when the subject is in a benign context allows only a small proportion of DA neurons to fire spontaneously (left); in this situation, a behaviourally relevant stimulus that activates the pedunculopontine tegmentum (PPTg) would lead to burst firing in only a small proportion of neurons, resulting in a small dopamine signal. (b) In a stressful situation, the vSub will induce an increase in the number of DA neurons firing spontaneously, allowing a larger dopamine response from a behaviourally relevant stimulus. (c) After stress withdrawal, a hyperactive BLA will induce an inhibition of the DA system, thereby leading to failure to respond to rewarding stimuli.
4. Stressors and environment
Responses to stress are dependent on the context. For example, if a rat is exposed to a stressor, such as during contextual fear conditioning, it will exhibit anxiety-like behaviours when returned to the same environmental context [57]. The effect of a stressor on the DA system varies markedly depending on whether it is physiological, psychological or a noxious stimulus. For example, a single noxious stimulus, such as a footshock delivered in anaesthetized animals, has been shown to induce a transient decrease of DA neuron firing rate [58–60], and in some cases an increase [59,61]. It has later been shown that the transient decrease in the firing rate of DA neurons is located in majority in the medial portion of the VTA, but that a transient excitation is located in the lateral portion [62]. In contrast, when a noxious stimulus is administered repeatedly over a set period of time, a condition which has been shown to increase DA levels at post-synaptic sites in behaving rats [63], a transient increase in DA neuron population activity is induced. Unlike acute noxious stimuli, this increase can be prevented by prior vSub inactivation [62]. When a physical stress is applied to the awake rat, such as acute or restraint stress, there is an increase in DA neuron activity that is also reversed by inactivation of the vSub [62]. Microdialysis studies have also shown that DA is released in the striatum in response to noxious stressors such as electric shock and tail-pinch [64]. Stress has been shown to cross-sensitize with amphetamine, because the acute amphetamine-induced locomotor response, which is correlated with an increased VTA activity [65] and an increased DA release in the NAc, is enhanced [66] in a vSub-dependent manner [62]. Therefore, a stress-induced hyperdopaminergic state is driven by the hippocampus, which is well known for its role in context dependency [21]. This causes the DA system to be placed into a high responsive state to amplify the response to a stimulus when it is delivered in an activating context. Therefore, if a threat or specific situation requiring high vigilance is present, the vSub will set the DA system to a higher level of spontaneous activity, rendering it more reactive to deliver the appropriate response to a significant stimulus (figure 1b).
When a stressor that had caused DA system activation is subsequently removed, the system exhibits an opposite response, a homeostatic event referred to as an opponent process. According to this theory, first described by R. Solomon in 1974 [67], emotions are pairs of opposites. When an emotion, such as fear, is experienced, it will trigger an opposing emotion, such as relief (or withdrawal), after a period of habituation, in order to avoid extreme emotions or withdraw from a threatening situation. With repeated stimulations, the opponent emotion becomes stronger, weakening the experience of the first emotion. Although it has been suggested that acute stress induces persistent increase of DA release in the NAc, recent studies have shown that 24 h after acute restraint stress, the DA neuron population activity in the VTA is markedly decreased [68]. Therefore, the initial activation of DA neurons during stress is followed by a depression of DA activity, in parallel with an attenuated amphetamine-induced locomotor response [68]. Such a sequence of events would be expected to attenuate an emotional reaction. This effect has also been described after chronic cold stress, which induces a decrease of the DA population activity in the VTA [69], indicating that chronic stress induces long-lasting changes in the regulation of neuronal activity of mesolimbic DA neurons. Therefore, the initial DA activity increase during stress predisposes the system to subsequent depression during withdrawal. For example, if the stressor induces fear, an increase in DA activity would facilitate escape and a delayed attenuation would weaken the experience of the primary emotion if the stressor re-occurs. Although the opponent process theory has long been described, the neuronal circuitry underlying the DA activity decrease has only recently begun to be elucidated.
5. The basolateral amygdala
The BLA is a limbic structure thought to attribute an emotional meaning to environmental stimuli by linking sensory processing-related cortical regions to areas involved in the production of emotional responses [70]. The importance of the BLA in the emotional component of the stress response is now clear (for review, see [71]). Stressful stimuli, such as footshock or tail-pinch, induce activation of the amygdala [72,73], and chronic as well as acute stressors increase activity of BLA neurons [74]. Moreover, synaptic plasticity within the amygdala [75] or in the amygdala–nucleus accumbens pathway [76] is also affected by different stressors. Morphologically, chronic [77] and acute [78] stress elicit a robust increase in spine density and dendritic arborization of BLA spiny neurons. In addition, stress can diminish the activity of GABAergic interneurons in the BLA, suggesting a stress-induced increased responsiveness to emotional stimuli [79]. The BLA also receives dense noradrenergic afferents from LC neurons, which are activated by stressful stimuli [80,81]. Furthermore, with repeated stressors, the NE actions in the amygdala become more excitatory in nature [29].
Therefore, the BLA is a strong candidate for mediating the interactions between the DA system and the stress withdrawal response. Indeed, inhibiting noradrenergic modulation of the BLA with infusion of the beta-adrenergic antagonist propranolol prevents the decrease in VTA DA neuron activity and the stress-induced attenuation of amphetamine locomotor response observed following restraint stress [68]. BLA neurons send projections to multiple structures known to influence VTA DA neuron activity. Indeed, it has been shown that the BLA projects to the VP [82] and the rostromedial tegmental nucleus [83]. Therefore, the amygdala can influence VTA activity via a complex network. The VP is the principal output nucleus connecting the forebrain to the midbrain reward circuitry. Recent studies have shown that the effect of BLA manipulation on DA activity after chronic mild stress (CMS) could be suppressed by inactivation of the VP [84], suggesting that the decrease of DA activity during stress withdrawal is mediated via the amygdala–pallidal pathway. Therefore, during withdrawal from sustained stress, hyperactivity of the BLA would inhibit DA neurons via the VP, decreasing the impact of subsequent behaviourally relevant stimuli (figure 1c).
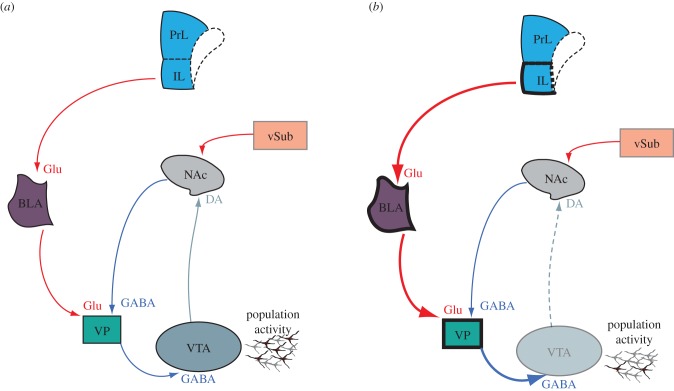
Therefore, the ventral hippocampus and the BLA exert equivalent, but opposite modulatory effects on VTA DA neuron firing and on behavioural response to amphetamine. The DA system is potently regulated by the integration of distinct contextual, emotional and behaviourally salient stimuli, and the output of the DA neurons provides a critical feedback to these systems (especially the NAc) that regulate goal-directed behaviours. Interestingly, it has been shown recently that the infralimbic prefrontal cortex exerts a bidirectional control over DA neuron population activity in the VTA [85] via the BLA and the ventral hippocampus, suggesting a cortical regulation of stress-induced changes in DA activity. Therefore, the balance within this circuit enables an organism to adapt to its environment (figure 1) and, conversely, disruption of this balance can lead to maladaptive responses.
6. Pathological stress response and psychiatric disorders
As reviewed earlier, stressors can cause an acute activation of the DA system mediated by the ventral hippocampal circuit, followed by a withdrawal response with a decrease in the DA system activity driven by the amygdala. However, if this normal acute stress response is prolonged, it can lead to pathological consequences. Indeed, the deleterious consequences of chronic stress are likely to underlie several psychiatric conditions.
(a). Stress and depression
Anhedonia, or loss of interest or pleasure to normally rewarding events, is a major symptom of many neuropsychiatric disorders, including MDD. Although depression has been historically associated with serotonin based on antidepressant drug actions, basic science investigations have consistently linked anhedonia to disruptions in the DA system [86]. Indeed, in rodents, lesions of the DA system result in impairment of brain stimulation reward behaviour [87], and DA blockade with dopamine D2 receptor antagonists disrupts conditioned reward association [88], both leading to anhedonic-like states. In patients with Parkinson's disease, pharmacological data suggest that besides the loss of the nigrostriatal DA system, degeneration of the mesolimbic DA system also occurs [89], which can lead to anhedonia [90]. Moreover, treatment of Parkinson's disease with DA receptor agonists such as pramipexole or l-DOPA relieves anhedonia symptoms [87]. This is consistent with animal models supporting that anhedonia is a complication of Parkinson's disease [87]. The DA system is associated with reward prediction [9] and motivation [91], and it is hypothesized that DA is necessary for the attribution of incentive salience to motivational stimuli, transforming the perception of a reward into a wanted incentive [10]. This is consistent with disruptions of the motivation to seek out pleasurable experiences described in individuals diagnosed with MDD [92].
The unpredictable CMS model, developed by Paul Willner and co-workers in the 1980s [93], is a validated animal model of human depression [94]. This model consists of repeated exposure to a range of different and unpredictable mild stressors over a sustained period of time, inducing anxiety, despair and anhedonia in rodents (for review, see [95]). Activation of VTA DA neurons in rats exposed to CMS can rescue rats with this stress-induced depression-like phenotype [96], particularly as assessed by sucrose preference, which is a recognized indicator of anhedonia in rodents [97]. Moreover, inhibition of VTA DA neurons can acutely induce multiple depression-like behaviours [96]. Using the same model, our laboratory has shown that rats exposed to CMS display an increase in immobility in the behavioural despair forced swim test, and a substantial decrease in DA neuron population activity [84]. This decrease is restored by inactivating either the BLA or the VP. Moreover, activation of the BLA in non-stressed rats decreases DA neuron population activity, similar to what has been described in CMS rats—a state that is also reversed by blocking the VP [84]. This suggests that in depression, the decrease in DA activity is mediated by the BLA–VP pathway. It should be noted that VP neurons receive mono- and polysynaptic projections from the BLA [98], and therefore the effect on DA neurons could be direct or involve intermediary glutamatergic regions. The BLA receives dense projections from the infralimbic PFC (ilPFC). The ilPFC is the rodent homologue of Brodmann area (BA) 25, a region that is known to be activated in humans by acute sadness [99] and is hyperactive in depression [99]. Indeed, therapeutic interventions that are effective in treating MDD in humans restore activity in BA25 [100]. We found that in CMS rats, pharmacological inactivation of the ilPFC results in disinhibition of the DA system, restoring VTA DA neuron population activity to a level comparable with non-stressed animals [101]. It is now generally viewed that MDD is a system-level disorder affecting integrated pathways connecting select cortical, subcortical and limbic structures [102,103]. Therefore, hyperactivity of the ilPFC/BA25, shown to be hyperactive in MDD in humans [104] and in CMS rodents, is inducing inhibition of VTA DA neuron activity via the BLA–VP pathway (figure 2).
Figure 2.
Afferent regulation of the dopamine system. (a) In a normal situation, a balance between the ilPFC → BLA → VP and the vSub → NAc → VP circuit leads to about half of the DA neurons firing spontaneously. (b) Hyperactivity of the ilPFC in major depressive disorders (MDD) leads to activation of the BLA, enhancing the inhibitory influence of the VP on the ventral tegmental area, causing an imbalance between the two circuits, with the result being a large, unopposed decrease of DA population activity, which is proposed to underlie anhedonia.
Therefore, there is a balance between two separate circuits that activate or attenuate DA neuron responsivity: the ilPFC → BLA → VP inhibit the DA system [84,101], whereas the vSub → NAc → VP activate the DA system [54,55]. It has been shown that acute (footshocks) and repeated/sustained (restraint) stress activates the vSub [24,25,62], which induces an increase in DA neuron population activity [62]. The consequence of stress on the DA system might therefore be related to its predictable or unpredictable nature [105,106]. The CMS is an unpredictable procedure that always leads to depressive- and anxiety-like behaviour [107], but predictable CMS such as repeated restraint stress over a prolonged period of time leads to hippocampal activation, possibly via NE [68], which in turn activates DA neuron firing. Moreover, animals show conditioned place preference for a context previously paired with predictable shocks to the one paired with the same intense unpredictable ones [108]. In humans, the inability to control a stressful event has been proposed to contribute to depression. In animals, inescapable stress is known to lead to learned helplessness, and is a well-established model of behavioural depression. Approximately half of animals exposed to uncontrollable stress developed learned helplessness (i.e. a decreased propensity to escape subsequent stressors) [109]. The other half, which do not demonstrate learned helplessness, may therefore have undergone alternate adaptations that protect them from the detrimental effects of inescapable stress. It has been shown recently that rats that exhibit helplessness have a decrease of VTA DA population activity, in particular in the medial regions, whereas non-helpless animals have DA activity comparable with control animals despite receiving the same number of shocks [110]. This is consistent with a previous study showing that chronic stress selectively decreases DA neuron population activity in the medial and central tracks of the VTA [111]. Moreover, animals exhibiting helplessness behaviour show dopamine depletion in the caudate nucleus and nucleus accumbens, consistent with altered dopamine functioning of the mesolimbic pathway in this model [112]. In the learned helplessness model, disruption of synaptic plasticity in the vSub–NAc pathway, which is DA-dependent [113,114], suggests that with unpredictable stressors, the vSub → NAc → VP circuit is attenuated, whereas it is activated with predictable stressors. Moreover, ketamine, an NMDA antagonist and a novel fast-acting antidepressant [115], has been shown to reverse the reduction in DA system activity and restore LTP in the vSub–NAc pathway [110], supposedly via the rapid induction of synaptic proteins in the hippocampus [116], and reversing the stress-induced decrease in spine density [117].
(b). Stress and addiction
There is substantial evidence that a significant association exists between acute or chronic stress and the motivation to abuse addictive substances (for review, see [4,118]). Lasting increases in HPA axis function has been reported with the chronic use of psychostimulants such as cocaine [119], which activate the mesolimbic DA system. Indeed, acute administration of psychostimulants such as cocaine or amphetamine increases mesolimbic DA [120], but chronic use and acute withdrawal downregulates the mesolimbic DA pathway, leading to decreases in basal DA levels [121]. In humans, imaging studies have shown that there is a reduction of DA transmission in the ventral striatum and the frontal cortex in chronic cocaine users during acute and prolonged withdrawal [122], and disruptions of synaptic plasticity in the VTA and the NAc has been shown after acute and chronic cocaine administration [123,124]. Acute administration of psychostimulants also activates brain stress systems such as the HPA axis, which results in increases in plasma ACTH and corticosterone [125]. Irritability, anxiety and emotional distress are common during early abstinence from psychostimulants [126]. This negative affective state has been described after chronic use, and parallels disruptions in the stress response and the DA systems (for review, see [127]). According to the opponent process theory of motivation [128], the positive emotion caused by the reinforcing properties of a drug is followed by secondary compensatory anhedonic processes that are opposite in nature and longer in duration when compared with the initial emotion. Therefore, after chronic use, the negative affective state prevails during withdrawal, leaving the addicted individual in a negative affective state (for review, see [129]), increasing the risk of relapse even after protracted periods of time. This negative state has been observed only after chronic drug use; few studies have focused on the withdrawal-negative phase following acute drug injection. However, it has recently been shown that an acute injection of amphetamine induces a subsequent decrease of DA neuron population activity 18 h after the injection, with this decrease lasting for up to 72 h [130]. Moreover, either ketamine administration or BLA inactivation restores the decrease in DA neuron activity [130], suggesting that hyperactivity in the ilPFC → BLA → VP circuit, as observed in MDD models, might be responsible for the negative withdrawal state that increases the risk of relapse even after an acute injection of a psychostimulant. Therefore, the duration of the negative affective state during withdrawal is likely to be related to the duration of DA system activation. Indeed, these results suggest that chronic drug use should induce a prolonged risk of relapse, probably due to a prolonged decrease in DA neuron activity following withdrawal, whereas acute drug use, which also induces a decrease in DA neuron activity, might be responsible for a shorter withdrawal but will probably drive a drug-naive individual to take additional doses of the drug.
To better understand how drug administration can induce a negative affective state and increase the risk of drug relapse and drug-seeking behaviour, it is therefore crucial to understand the pathophysiological disruptions in the different circuits modulating the DA system, stress–BLA pathways and the stress–vSub system circuit.
7. Conclusion
The DA system can play distinct roles in stress and psychiatric disorders. Indeed, stress-induced hyperactivity in the ventral hippocampus can activate VTA DA neuron activity via a vSub → NAc inhibition of the VP, leading to a disinhibition of VTA DA neurons. However, following stress withdrawal, there is a long-lasting compensatory decrease in DA neuron activity via an ilPFC–BLA excitation of the VP, leading to attenuation of DA neuron activity. Therefore, although the DA system may form the basis of a number of psychiatric disorders, the pathology is more likely to originate in the afferent structures that are dysregulating the DA neurons. Therefore, a therapeutic focus on restoring normal function in these regions is likely to be more effective than manipulating the DA system directly.
Funding statement
This work was supported by a Young Investigator Award from NARSAD—The Brain and Behavior Research Foundation (P.B.) and the United States Public Health Service grant nos. MH057440, MH101180 and DA036328 (A.A.G.)
Competing interest
Dr Belujon reports no competing interests. Dr Grace received funds from Johnson and Johnson, Lundbeck, Pfizer, GSK, Puretech Ventures, Merck, Takeda, Dainippon Sumitomo, Otsuka, Lilly, Roche and Asubio.
References
- 1.Pacak K, Palkovits M. 2001. Stressor specificity of central neuroendocrine responses: implications for stress-related disorders. Endocr. Rev. 22, 502–548. ( 10.1210/edrv.22.4.0436) [DOI] [PubMed] [Google Scholar]
- 2.Cullinan WE, Herman JP, Battaglia DF, Akil H, Watson SJ. 1995. Pattern and time course of immediate early gene expression in rat brain following acute stress. Neuroscience 64, 477–505. ( 10.1016/0306-4522(94)00355-9) [DOI] [PubMed] [Google Scholar]
- 3.Chrousos GP. 2009. Stress and disorders of the stress system. Nat. Rev. Endocrinol. 5, 374–381. ( 10.1038/nrendo.2009.106) [DOI] [PubMed] [Google Scholar]
- 4.Belujon P, Grace AA. 2011. Hippocampus, amygdala, and stress: interacting systems that affect susceptibility to addiction. Ann. N.Y. Acad. Sci. 1216, 114–121. ( 10.1111/j.1749-6632.2010.05896.x) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hammen C. 2005. Stress and depression. Annu. Rev. Clin. Psychol. 1, 293–319. ( 10.1146/annurev.clinpsy.1.102803.143938) [DOI] [PubMed] [Google Scholar]
- 6.Lodge DJ, Grace AA. 2011. Developmental pathology, dopamine, stress and schizophrenia. Int. J. Dev. Neurosci. 29, 207–213. ( 10.1016/j.ijdevneu.2010.08.002) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lowry CA. 2002. Functional subsets of serotonergic neurones: implications for control of the hypothalamic–pituitary–adrenal axis. J. Neuroendocrinol. 14, 911–923. ( 10.1046/j.1365-2826.2002.00861.x) [DOI] [PubMed] [Google Scholar]
- 8.Wise RA, Rompre PP. 1989. Brain dopamine and reward. Annu. Rev. Psychol. 40, 191–225. ( 10.1146/annurev.ps.40.020189.001203) [DOI] [PubMed] [Google Scholar]
- 9.Schultz W. 1997. Dopamine neurons and their role in reward mechanisms. Curr. Opin. Neurobiol. 7, 191–197. ( 10.1016/S0959-4388(97)80007-4) [DOI] [PubMed] [Google Scholar]
- 10.Berridge KC, Robinson TE. 1998. What is the role of dopamine in reward: hedonic impact, reward learning, or incentive salience? Brain Res. Brain Res. Rev. 28, 309–369. ( 10.1016/S0165-0173(98)00019-8) [DOI] [PubMed] [Google Scholar]
- 11.Salamone JD, Cousins MS, Snyder BJ. 1997. Behavioral functions of nucleus accumbens dopamine: empirical and conceptual problems with the anhedonia hypothesis. Neurosci. Biobehav. Rev. 21, 341–359. ( 10.1016/S0149-7634(96)00017-6) [DOI] [PubMed] [Google Scholar]
- 12.Makino S, Smith MA, Gold PW. 2002. Regulatory role of glucocorticoids and glucocorticoid receptor mRNA levels on tyrosine hydroxylase gene expression in the locus coeruleus during repeated immobilization stress. Brain Res. 943, 216–223. ( 10.1016/S0006-8993(02)02647-1) [DOI] [PubMed] [Google Scholar]
- 13.Chang MS, Sved AF, Zigmond MJ, Austin MC. 2000. Increased transcription of the tyrosine hydroxylase gene in individual locus coeruleus neurons following footshock stress. Neuroscience 101, 131–139. ( 10.1016/S0306-4522(00)00352-3) [DOI] [PubMed] [Google Scholar]
- 14.Kollack-Walker S, Watson SJ, Akil H. 1997. Social stress in hamsters: defeat activates specific neurocircuits within the brain. J. Neurosci. 17, 8842–8855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Abercrombie ED, Keefe KA, DiFrischia DS, Zigmond MJ. 1989. Differential effect of stress on in vivo dopamine release in striatum, nucleus accumbens, and medial frontal cortex. J. Neurochem. 52, 1655–1658. ( 10.1111/j.1471-4159.1989.tb09224.x) [DOI] [PubMed] [Google Scholar]
- 16.Korf J, Aghajanian GK, Roth RH. 1973. Increased turnover of norepinephrine in the rat cerebral cortex during stress: role of the locus coeruleus. Neuropharmacology 12, 933–938. ( 10.1016/0028-3908(73)90024-5) [DOI] [PubMed] [Google Scholar]
- 17.Ziegler DR, Cass WA, Herman JP. 1999. Excitatory influence of the locus coeruleus in hypothalamic–pituitary–adrenocortical axis responses to stress. J. Neuroendocrinol. 11, 361–369. ( 10.1046/j.1365-2826.1999.00337.x) [DOI] [PubMed] [Google Scholar]
- 18.Butler PD, Weiss JM, Stout JC, Nemeroff CB. 1990. Corticotropin-releasing factor produces fear-enhancing and behavioral activating effects following infusion into the locus coeruleus. J. Neurosci. 10, 176–183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Herman JP, Cullinan WE. 1997. Neurocircuitry of stress: central control of the hypothalamo–pituitary–adrenocortical axis. Trends Neurosci. 20, 78–84. ( 10.1016/S0166-2236(96)10069-2) [DOI] [PubMed] [Google Scholar]
- 20.Oleskevich S, Descarries L, Lacaille JC. 1989. Quantified distribution of the noradrenaline innervation in the hippocampus of adult rat. J. Neurosci. 9, 3803–3815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jarrard LE. 1995. What does the hippocampus really do? Behav. Brain Res. 71, 1–10. ( 10.1016/0166-4328(95)00034-8) [DOI] [PubMed] [Google Scholar]
- 22.Bouton ME, Bolles RC. 1979. Role of conditioned contextual stimuli in reinstatement of extinguished fear. J. Exp. Psychol. Anim. Behav. Process. 5, 368–378. ( 10.1037/0097-7403.5.4.368) [DOI] [PubMed] [Google Scholar]
- 23.Figueiredo HF, Bodie BL, Tauchi M, Dolgas CM, Herman JP. 2003. Stress integration after acute and chronic predator stress: differential activation of central stress circuitry and sensitization of the hypothalamo–pituitary–adrenocortical axis. Endocrinology 144, 5249–5258. ( 10.1210/en.2003-0713) [DOI] [PubMed] [Google Scholar]
- 24.Lipski WJ, Grace AA. 2013. Activation and inhibition of neurons in the hippocampal ventral subiculum by norepinephrine and locus coeruleus stimulation. Neuropsychopharmacology 38, 285–292. ( 10.1038/npp.2012.157) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lipski WJ, Grace AA. 2013. Footshock-induced responses in ventral subiculum neurons are mediated by locus coeruleus noradrenergic afferents. Eur. Neuropsychopharmacol. 23, 1320–1328. ( 10.1016/j.euroneuro.2012.10.007) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Herman JP, Mueller NK. 2006. Role of the ventral subiculum in stress integration. Behav. Brain Res. 174, 215–224. ( 10.1016/j.bbr.2006.05.035) [DOI] [PubMed] [Google Scholar]
- 27.Rosen JB, Fanselow MS, Young SL, Sitcoske M, Maren S. 1998. Immediate-early gene expression in the amygdala following footshock stress and contextual fear conditioning. Brain Res. 796, 132–142. ( 10.1016/S0006-8993(98)00294-7) [DOI] [PubMed] [Google Scholar]
- 28.Galvez R, Mesches MH, McGaugh JL. 1996. Norepinephrine release in the amygdala in response to footshock stimulation. Neurobiol. Learn. Mem. 66, 253–257. ( 10.1006/nlme.1996.0067) [DOI] [PubMed] [Google Scholar]
- 29.Buffalari DM, Grace AA. 2007. Noradrenergic modulation of basolateral amygdala neuronal activity: opposing influences of alpha-2 and beta receptor activation. J. Neurosci. 27, 12 358–12 366. ( 10.1523/JNEUROSCI.2007-07.2007) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lakshminarasimhan H, Chattarji S. 2012. Stress leads to contrasting effects on the levels of brain derived neurotrophic factor in the hippocampus and amygdala. PLoS ONE 7, e30481 ( 10.1371/journal.pone.0030481) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yuste R, Bonhoeffer T. 2001. Morphological changes in dendritic spines associated with long-term synaptic plasticity. Annu. Rev. Neurosci. 24, 1071–1089. ( 10.1146/annurev.neuro.24.1.1071) [DOI] [PubMed] [Google Scholar]
- 32.Sarabdjitsingh RA, Kofink D, Karst H, de Kloet ER, Joels M. 2012. Stress-induced enhancement of mouse amygdalar synaptic plasticity depends on glucocorticoid and ss-adrenergic activity. PLoS ONE 7, e42143 ( 10.1371/journal.pone.0042143) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Thierry AM, Tassin JP, Blanc G, Glowinski J. 1976. Selective activation of mesocortical DA system by stress. Nature 263, 242–244. ( 10.1038/263242a0) [DOI] [PubMed] [Google Scholar]
- 34.Radley JJ, Williams B, Sawchenko PE. 2008. Noradrenergic innervation of the dorsal medial prefrontal cortex modulates hypothalamo–pituitary–adrenal responses to acute emotional stress. J. Neurosci. 28, 5806–5816. ( 10.1523/JNEUROSCI.0552-08.2008) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Maroun M, Richter-Levin G. 2003. Exposure to acute stress blocks the induction of long-term potentiation of the amygdala–prefrontal cortex pathway in vivo. J. Neurosci. 23, 4406–4409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Laviolette SR, Lipski WJ, Grace AA. 2005. A subpopulation of neurons in the medial prefrontal cortex encodes emotional learning with burst and frequency codes through a dopamine D4 receptor-dependent basolateral amygdala input. J. Neurosci. 25, 6066–6075. ( 10.1523/JNEUROSCI.1168-05.2005) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Piazza PV, Le Moal M. 1998. The role of stress in drug self-administration. Trends Pharmacol. Sci. 19, 67–74. ( 10.1016/S0165-6147(97)01115-2) [DOI] [PubMed] [Google Scholar]
- 38.Feenstra MG, Kalsbeek A, van Galen H. 1992. Neonatal lesions of the ventral tegmental area affect monoaminergic responses to stress in the medial prefrontal cortex and other dopamine projection areas in adulthood. Brain Res. 596, 169–182. ( 10.1016/0006-8993(92)91545-P) [DOI] [PubMed] [Google Scholar]
- 39.Grace AA. 1991. Phasic versus tonic dopamine release and the modulation of dopamine system responsivity: a hypothesis for the etiology of schizophrenia. Neuroscience 41, 1–24. ( 10.1016/0306-4522(91)90196-U) [DOI] [PubMed] [Google Scholar]
- 40.Grace AA, Floresco SB, Goto Y, Lodge DJ. 2007. Regulation of firing of dopaminergic neurons and control of goal-directed behaviors. Trends Neurosci. 30, 220–227. ( 10.1016/j.tins.2007.03.003) [DOI] [PubMed] [Google Scholar]
- 41.Grace AA, Bunney BS. 1984. The control of firing pattern in nigral dopamine neurons: single spike firing. J. Neurosci. 4, 2866–2876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Floresco SB, West AR, Ash B, Moore H, Grace AA. 2003. Afferent modulation of dopamine neuron firing differentially regulates tonic and phasic dopamine transmission. Nat. Neurosci. 6, 968–973. ( 10.1038/nn1103) [DOI] [PubMed] [Google Scholar]
- 43.Grace AA, Bunney BS. 1983. Intracellular and extracellular electrophysiology of nigral dopaminergic neurons. 1. Identification and characterization. Neuroscience 10, 301–315. ( 10.1016/0306-4522(83)90135-5) [DOI] [PubMed] [Google Scholar]
- 44.Grace AA, Bunney BS. 1984. The control of firing pattern in nigral dopamine neurons: burst firing. J. Neurosci. 4, 2877–2890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lodge DJ, Grace AA. 2006. The laterodorsal tegmentum is essential for burst firing of ventral tegmental area dopamine neurons. Proc. Natl Acad. Sci. USA 103, 5167–5172. ( 10.1073/pnas.0510715103) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Schultz W. 1998. Predictive reward signal of dopamine neurons. J. Neurophysiol. 80, 1–27. [DOI] [PubMed] [Google Scholar]
- 47.Pan WX, Schmidt R, Wickens JR, Hyland BI. 2005. Dopamine cells respond to predicted events during classical conditioning: evidence for eligibility traces in the reward-learning network. J. Neurosci. 25, 6235–6242. ( 10.1523/JNEUROSCI.1478-05.2005) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Steinfels GF, Heym J, Strecker RE, Jacobs BL. 1983. Response of dopaminergic neurons in cat to auditory stimuli presented across the sleep-waking cycle. Brain Res. 277, 150–154. ( 10.1016/0006-8993(83)90917-4) [DOI] [PubMed] [Google Scholar]
- 49.Hyland BI, Reynolds JN, Hay J, Perk CG, Miller R. 2002. Firing modes of midbrain dopamine cells in the freely moving rat. Neuroscience 114, 475–492. ( 10.1016/S0306-4522(02)00267-1) [DOI] [PubMed] [Google Scholar]
- 50.Kelland MD, Chiodo LA, Freeman AS. 1990. Anesthetic influences on the basal activity and pharmacological responsiveness of nigrostriatal dopamine neurons. Synapse 6, 207–209. ( 10.1002/syn.890060213) [DOI] [PubMed] [Google Scholar]
- 51.Dommett E, Coizet V, Blaha CD, Martindale J, Lefebvre V, Walton N, Mayhew JE, Overton PG, Redgrave P. 2005. How visual stimuli activate dopaminergic neurons at short latency. Science 307, 1476–1479. ( 10.1126/science.1107026) [DOI] [PubMed] [Google Scholar]
- 52.Overton P, Clark D. 1992. Iontophoretically administered drugs acting at the N-methyl-D-aspartate receptor modulate burst firing in A9 dopamine neurons in the rat. Synapse 10, 131–140. ( 10.1002/syn.890100208) [DOI] [PubMed] [Google Scholar]
- 53.Zellner MR, Kest K, Ranaldi R. 2009. NMDA receptor antagonism in the ventral tegmental area impairs acquisition of reward-related learning. Behav. Brain Res. 197, 442–449. ( 10.1016/j.bbr.2008.10.013) [DOI] [PubMed] [Google Scholar]
- 54.Lodge DJ, Grace AA. 2006. The hippocampus modulates dopamine neuron responsivity by regulating the intensity of phasic neuron activation. Neuropsychopharmacology 31, 1356–1361. ( 10.1038/sj.npp.1300963) [DOI] [PubMed] [Google Scholar]
- 55.Floresco SB, Todd CL, Grace AA. 2001. Glutamatergic afferents from the hippocampus to the nucleus accumbens regulate activity of ventral tegmental area dopamine neurons. J. Neurosci. 21, 4915–4922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Mayer ML, Westbrook GL, Guthrie PB. 1984. Voltage-dependent block by Mg2+ of NMDA responses in spinal cord neurones. Nature 309, 261–263. ( 10.1038/309261a0) [DOI] [PubMed] [Google Scholar]
- 57.Fanselow MS. 2000. Contextual fear, gestalt memories, and the hippocampus. Behav. Brain Res. 110, 73–81. ( 10.1016/S0166-4328(99)00186-2) [DOI] [PubMed] [Google Scholar]
- 58.Grace AA, Bunney BS. 1979. Paradoxical GABA excitation of nigral dopaminergic cells: indirect mediation through reticulata inhibitory neurons. Eur. J. Pharmacol. 59, 211–218. ( 10.1016/0014-2999(79)90283-8) [DOI] [PubMed] [Google Scholar]
- 59.Schultz W, Romo R. 1987. Responses of nigrostriatal dopamine neurons to high-intensity somatosensory stimulation in the anesthetized monkey. J. Neurophysiol. 57, 201–217. [DOI] [PubMed] [Google Scholar]
- 60.Ungless MA, Magill PJ, Bolam JP. 2004. Uniform inhibition of dopamine neurons in the ventral tegmental area by aversive stimuli. Science 303, 2040–2042. ( 10.1126/science.1093360) [DOI] [PubMed] [Google Scholar]
- 61.Brischoux F, Chakraborty S, Brierley DI, Ungless MA. 2009. Phasic excitation of dopamine neurons in ventral VTA by noxious stimuli. Proc. Natl Acad. Sci. USA 106, 4894–4899. ( 10.1073/pnas.0811507106) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Valenti O, Lodge DJ, Grace AA. 2011. Aversive stimuli alter ventral tegmental area dopamine neuron activity via a common action in the ventral hippocampus. J. Neurosci. 31, 4280–4289. ( 10.1523/JNEUROSCI.5310-10.2011) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Saulskaya N, Marsden CA. 1995. Conditioned dopamine release: dependence upon N-methyl-D-aspartate receptors. Neuroscience 67, 57–63. ( 10.1016/0306-4522(95)00007-6) [DOI] [PubMed] [Google Scholar]
- 64.Rouge-Pont F, Piazza PV, Kharouby M, Le Moal M, Simon H. 1993. Higher and longer stress-induced increase in dopamine concentrations in the nucleus accumbens of animals predisposed to amphetamine self-administration: a microdialysis study. Brain Res. 602, 169–174. ( 10.1016/0006-8993(93)90260-T) [DOI] [PubMed] [Google Scholar]
- 65.Lodge DJ, Grace AA. 2008. Amphetamine activation of hippocampal drive of mesolimbic dopamine neurons: a mechanism of behavioral sensitization. J. Neurosci. 28, 7876–7882. ( 10.1523/JNEUROSCI.1582-08.2008) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Pacchioni AM, Cador M, Bregonzio C, Cancela LM. 2007. A glutamate-dopamine interaction in the persistent enhanced response to amphetamine in nucleus accumbens core but not shell following a single restraint stress. Neuropsychopharmacology 32, 682–692. ( 10.1038/sj.npp.1301080) [DOI] [PubMed] [Google Scholar]
- 67.Solomon RL, Corbit JD. 1974. An opponent-process theory of motivation. I. Temporal dynamics of affect. Psychol. Rev. 81, 119–145. ( 10.1037/h0036128) [DOI] [PubMed] [Google Scholar]
- 68.Chang CH, Grace AA. 2013. Amygdala beta-noradrenergic receptors modulate delayed downregulation of dopamine activity following restraint. J. Neurosci. 33, 1441–1450. ( 10.1523/JNEUROSCI.2420-12.2013) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Moore H, Rose HJ, Grace AA. 2001. Chronic cold stress reduces the spontaneous activity of ventral tegmental dopamine neurons. Neuropsychopharmacology 24, 410–419. ( 10.1016/S0893-133X(00)00188-3) [DOI] [PubMed] [Google Scholar]
- 70.Aggleton JP. 1993. The contribution of the amygdala to normal and abnormal emotional states. Trends Neurosci. 16, 328–333. ( 10.1016/0166-2236(93)90110-8) [DOI] [PubMed] [Google Scholar]
- 71.Roozendaal B, McEwen BS, Chattarji S. 2009. Stress, memory and the amygdala. Nat. Rev. Neurosci. 10, 423–433. ( 10.1038/nrn2651) [DOI] [PubMed] [Google Scholar]
- 72.Bunney BS, Grace AA. 1978. Acute and chronic haloperidol treatment: comparison of effects on nigral dopaminergic cell activity. Life Sci. 23, 1715–1727. ( 10.1016/0024-3205(78)90471-X) [DOI] [PubMed] [Google Scholar]
- 73.Rosenkranz JA, Buffalari DM, Grace AA. 2006. Opposing influence of basolateral amygdala and footshock stimulation on neurons of the central amygdala. Biol. Psychiatry 59, 801–811. ( 10.1016/j.biopsych.2005.09.013) [DOI] [PubMed] [Google Scholar]
- 74.Buffalari DM, Grace AA. 2009. Anxiogenic modulation of spontaneous and evoked neuronal activity in the basolateral amygdala. Neuroscience 163, 1069–1077. ( 10.1016/j.neuroscience.2009.07.003) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Vouimba RM, Yaniv D, Diamond D, Richter-Levin G. 2004. Effects of inescapable stress on LTP in the amygdala versus the dentate gyrus of freely behaving rats. Eur. J. Neurosci. 19, 1887–1894. ( 10.1111/j.1460-9568.2004.03294.x) [DOI] [PubMed] [Google Scholar]
- 76.Gill KM, Grace AA. 2011. Heterogeneous processing of amygdala and hippocampal inputs in the rostral and caudal subregions of the nucleus accumbens. Int. J. Neuropsychopharmacol. 14, 1301–1314. ( 10.1017/S1461145710001586) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Mitra R, Jadhav S, McEwen BS, Vyas A, Chattarji S. 2005. Stress duration modulates the spatiotemporal patterns of spine formation in the basolateral amygdala. Proc. Natl Acad. Sci. USA 102, 9371–9376. ( 10.1073/pnas.0504011102) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Maroun M, Ioannides PJ, Bergman KL, Kavushansky A, Holmes A, Wellman CL. 2013. Fear extinction deficits following acute stress associate with increased spine density and dendritic retraction in basolateral amygdala neurons. Eur. J. Neurosci. 38, 2611–2620. ( 10.1111/ejn.12259) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Braga MF, Aroniadou-Anderjaska V, Post RM, Li H. 2002. Lamotrigine reduces spontaneous and evoked GABAA receptor-mediated synaptic transmission in the basolateral amygdala: implications for its effects in seizure and affective disorders. Neuropharmacology 42, 522–529. ( 10.1016/S0028-3908(01)00198-8) [DOI] [PubMed] [Google Scholar]
- 80.Aston-Jones G, Chiang C, Alexinsky T. 1991. Discharge of noradrenergic locus coeruleus neurons in behaving rats and monkeys suggests a role in vigilance. Prog. Brain Res. 88, 501–520. ( 10.1016/S0079-6123(08)63830-3) [DOI] [PubMed] [Google Scholar]
- 81.Morilak DA, Barrera G, Echevarria DJ, Garcia AS, Hernandez A, Ma S, Petre CO. 2005. Role of brain norepinephrine in the behavioral response to stress. Prog. Neuro-psychopharmacol. Biol. Psychiatry 29, 1214–1224. ( 10.1016/j.pnpbp.2005.08.007) [DOI] [PubMed] [Google Scholar]
- 82.Yim CY, Mogenson GJ. 1983. Response of ventral pallidal neurons to amygdala stimulation and its modulation by dopamine projections to nucleus accumbens. J. Neurophysiol. 50, 148–161. [DOI] [PubMed] [Google Scholar]
- 83.Lavezzi HN, Zahm DS. 2011. The mesopontine rostromedial tegmental nucleus: an integrative modulator of the reward system. Basal Ganglia 1, 191–200. ( 10.1016/j.baga.2011.08.003) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Chang CH, Grace AA. 2013. Amygdala–ventral pallidum pathway decreases dopamine activity after chronic mild stress in rats. Biol. Psychiatry 76, 223–230. ( 10.1016/j.biopsych.2013.09.020) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Patton MH, Bizup BT, Grace AA. 2013. The infralimbic cortex bidirectionally modulates mesolimbic dopamine neuron activity via distinct neural pathways. J. Neurosci. 33, 16 865–16 873. ( 10.1523/JNEUROSCI.2449-13.2013) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Wise RA. 2008. Dopamine and reward: the anhedonia hypothesis 30 years on. Neurotox. Res. 14, 169–183. ( 10.1007/BF03033808) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Carey RJ. 1986. An examination of parkinsonian versus anhedonia contributions to self-stimulation impairments induced by dopamine dysfunction. Behav. Brain Res. 22, 117–125. ( 10.1016/0166-4328(86)90033-1) [DOI] [PubMed] [Google Scholar]
- 88.Huang AC, Hsiao S. 2002. Haloperidol attenuates rewarding and aversively conditioned suppression of saccharin solution intake: reevaluation of the anhedonia hypothesis of dopamine blocking. Behav. Neurosci. 116, 646–650. ( 10.1037/0735-7044.116.4.646) [DOI] [PubMed] [Google Scholar]
- 89.Javoy-Agid F, Agid Y. 1980. Is the mesocortical dopaminergic system involved in Parkinson disease? Neurology 30, 1326–1330. ( 10.1212/WNL.30.12.1326) [DOI] [PubMed] [Google Scholar]
- 90.Fibiger HC. 1984. The neurobiological substrates of depression in Parkinson's disease: a hypothesis. Can. J. Neurol. Sci. 11(1 Suppl.), 105–107. [DOI] [PubMed] [Google Scholar]
- 91.Salamone JD, Correa M, Mingote S, Weber SM. 2003. Nucleus accumbens dopamine and the regulation of effort in food-seeking behavior: implications for studies of natural motivation, psychiatry, and drug abuse. J. Pharmacol. Exp. Ther. 305, 1–8. ( 10.1124/jpet.102.035063) [DOI] [PubMed] [Google Scholar]
- 92.Der-Avakian A, Markou A. 2012. The neurobiology of anhedonia and other reward-related deficits. Trends Neurosci. 35, 68–77. ( 10.1016/j.tins.2011.11.005) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Willner P, Towell A, Sampson D, Sophokleous S, Muscat R. 1987. Reduction of sucrose preference by chronic unpredictable mild stress, and its restoration by a tricyclic antidepressant. Psychopharmacology 93, 358–364. ( 10.1007/BF00187257) [DOI] [PubMed] [Google Scholar]
- 94.Hill MN, Hellemans KG, Verma P, Gorzalka BB, Weinberg J. 2012. Neurobiology of chronic mild stress: parallels to major depression. Neurosci. Biobehav. Rev. 36, 2085–2117. ( 10.1016/j.neubiorev.2012.07.001) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Willner P. 1997. Validity, reliability and utility of the chronic mild stress model of depression: a 10-year review and evaluation. Psychopharmacology 134, 319–329. ( 10.1007/s002130050456) [DOI] [PubMed] [Google Scholar]
- 96.Tye KM, et al. 2013. Dopamine neurons modulate neural encoding and expression of depression-related behaviour. Nature 493, 537–541. ( 10.1038/nature11740) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Katz RJ. 1982. Animal model of depression: pharmacological sensitivity of a hedonic deficit. Pharmacol. Biochem. Behav. 16, 965–968. ( 10.1016/0091-3057(82)90053-3) [DOI] [PubMed] [Google Scholar]
- 98.Maslowski-Cobuzzi RJ, Napier TC. 1994. Activation of dopaminergic neurons modulates ventral pallidal responses evoked by amygdala stimulation. Neuroscience 62, 1103–1119. ( 10.1016/0306-4522(94)90347-6) [DOI] [PubMed] [Google Scholar]
- 99.Mayberg HS, et al. 1999. Reciprocal limbic-cortical function and negative mood: converging PET findings in depression and normal sadness. Am. J. Psychiatry 156, 675–682. [DOI] [PubMed] [Google Scholar]
- 100.Mayberg HS, Lozano AM, Voon V, McNeely HE, Seminowicz D, Hamani C, Schwalb JM, Kennedy SH. 2005. Deep brain stimulation for treatment-resistant depression. Neuron 45, 651–660. ( 10.1016/j.neuron.2005.02.014) [DOI] [PubMed] [Google Scholar]
- 101.Moreines JL, Owrutsky WL, Grace AA. 2014. Infralimbic prefrontal cortex modulation of dopaminergic system function in chronic mild stress model of depression. Washington, DC: Society for Neuroscience. [Google Scholar]
- 102.Nestler EJ, Barrot M, DiLeone RJ, Eisch AJ, Gold SJ, Monteggia LM. 2002. Neurobiology of depression. Neuron 34, 13–25. ( 10.1016/S0896-6273(02)00653-0) [DOI] [PubMed] [Google Scholar]
- 103.Vaidya VA, Duman RS. 2001. Depresssion: emerging insights from neurobiology. Br. Med. Bull. 57, 61–79. ( 10.1093/bmb/57.1.61) [DOI] [PubMed] [Google Scholar]
- 104.Mayberg HS. 2003. Modulating dysfunctional limbic-cortical circuits in depression: towards development of brain-based algorithms for diagnosis and optimised treatment. Br. Med. Bull. 65, 193–207. ( 10.1093/bmb/65.1.193) [DOI] [PubMed] [Google Scholar]
- 105.Abbott BB, Schoen LS, Badia P. 1984. Predictable and unpredictable shock: behavioral measures of aversion and physiological measures of stress. Psychol. Bull. 96, 45–71. ( 10.1037/0033-2909.96.1.45) [DOI] [PubMed] [Google Scholar]
- 106.Anisman H, Matheson K. 2005. Stress, depression, and anhedonia: caveats concerning animal models. Neurosci. Biobehav. Rev. 29, 525–546. ( 10.1016/j.neubiorev.2005.03.007) [DOI] [PubMed] [Google Scholar]
- 107.Willner P, Mitchell PJ. 2002. The validity of animal models of predisposition to depression. Behav. Pharmacol. 13, 169–188. ( 10.1097/00008877-200205000-00001) [DOI] [PubMed] [Google Scholar]
- 108.Gliner JA. 1972. Predictable versus. unpredictable shock: preference behavior and stomach ulceration. Physiol. Behav. 9, 693–698. ( 10.1016/0031-9384(72)90036-4) [DOI] [PubMed] [Google Scholar]
- 109.Petty F, Kramer GL, Wu J. 1997. Serotonergic modulation of learned helplessness. Ann. N.Y. Acad. Sci. 821, 538–541. ( 10.1111/j.1749-6632.1997.tb48324.x) [DOI] [PubMed] [Google Scholar]
- 110.Belujon P, Grace AA. 2014. Restoring mood balance in depression: ketamine reverses deficit in dopamine-dependent synaptic plasticity. Biol. Psychiatry 76, 927–936. ( 10.1016/j.biopsych.2014.04.014) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Valenti O, Gill KM, Grace AA. 2012. Different stressors produce excitation or inhibition of mesolimbic dopamine neuron activity: response alteration by stress pre-exposure. Eur. J. Neurosci. 35, 1312–1321. ( 10.1111/j.1460-9568.2012.08038.x) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Dunlop BW, Nemeroff CB. 2007. The role of dopamine in the pathophysiology of depression. Arch. Gen. Psychiatry 64, 327–337. ( 10.1001/archpsyc.64.3.327) [DOI] [PubMed] [Google Scholar]
- 113.Belujon P, Grace AA. 2008. Critical role of the prefrontal cortex in the regulation of hippocampus–accumbens information flow. J. Neurosci. 28, 9797–9805. ( 10.1523/JNEUROSCI.2200-08.2008) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Floresco SB, Blaha CD, Yang CR, Phillips AG. 2001. Modulation of hippocampal and amygdalar-evoked activity of nucleus accumbens neurons by dopamine: cellular mechanisms of input selection. J. Neurosci. 21, 2851–2860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Zarate CA, Jr, Singh JB, Carlson PJ, Brutsche NE, Ameli R, Luckenbaugh DA, Charney DS, Manji HK. 2006. A randomized trial of an N-methyl-D-aspartate antagonist in treatment-resistant major depression. Arch. Gen. Psychiatry 63, 856–864. ( 10.1001/archpsyc.63.8.856) [DOI] [PubMed] [Google Scholar]
- 116.Garcia LS, et al. 2008. Chronic administration of ketamine elicits antidepressant-like effects in rats without affecting hippocampal brain-derived neurotrophic factor protein levels. Basic Clin. Pharmacol. Toxicol. 103, 502–506. ( 10.1111/j.1742-7843.2008.00210.x) [DOI] [PubMed] [Google Scholar]
- 117.Li N, Liu RJ, Dwyer JM, Banasr M, Lee B, Son H, Li XY, Aghajanian G, Duman RS. 2011. Glutamate N-methyl-d-aspartate receptor antagonists rapidly reverse behavioral and synaptic deficits caused by chronic stress exposure. Biol. Psychiatry 69, 754–761. ( 10.1016/j.biopsych.2010.12.015) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Sinha R. 2001. How does stress increase risk of drug abuse and relapse? Psychopharmacology 158, 343–359. ( 10.1007/s002130100917) [DOI] [PubMed] [Google Scholar]
- 119.Borowsky B, Kuhn CM. 1991. Monoamine mediation of cocaine-induced hypothalamo–pituitary–adrenal activation. J. Pharmacol. Exp. Ther. 256, 204–210. [PubMed] [Google Scholar]
- 120.Di Chiara G, et al. 2004. Dopamine and drug addiction: the nucleus accumbens shell connection. Neuropharmacology 47(Suppl. 1), 227–241. ( 10.1016/j.neuropharm.2004.06.032) [DOI] [PubMed] [Google Scholar]
- 121.Parsons LH, Smith AD, Justice JB., Jr 1991. Basal extracellular dopamine is decreased in the rat nucleus accumbens during abstinence from chronic cocaine. Synapse 9, 60–65. ( 10.1002/syn.890090109) [DOI] [PubMed] [Google Scholar]
- 122.Volkow ND, Wang GJ, Fowler JS, Logan J, Gatley SJ, Hitzemann R, Chen AD, Dewey SL, Pappas N. 1997. Decreased striatal dopaminergic responsiveness in detoxified cocaine-dependent subjects. Nature 386, 830–833. ( 10.1038/386830a0) [DOI] [PubMed] [Google Scholar]
- 123.Mameli M, Halbout B, Creton C, Engblom D, Parkitna JR, Spanagel R, Luscher C. 2009. Cocaine-evoked synaptic plasticity: persistence in the VTA triggers adaptations in the NAc. Nat. Neurosci. 12, 1036–1041. ( 10.1038/nn.2367) [DOI] [PubMed] [Google Scholar]
- 124.Nestler EJ, Hope BT, Widnell KL. 1993. Drug addiction: a model for the molecular basis of neural plasticity. Neuron 11, 995–1006. ( 10.1016/0896-6273(93)90213-B) [DOI] [PubMed] [Google Scholar]
- 125.Baumann MH, Gendron TM, Becketts KM, Henningfield JE, Gorelick DA, Rothman RB. 1995. Effects of intravenous cocaine on plasma cortisol and prolactin in human cocaine abusers. Biol. Psychiatry 38, 751–755. ( 10.1016/0006-3223(95)00083-6) [DOI] [PubMed] [Google Scholar]
- 126.Mulvaney FD, Alterman AI, Boardman CR, Kampman K. 1999. Cocaine abstinence symptomatology and treatment attrition. J. Subst. Abuse Treat. 16, 129–135. ( 10.1016/S0740-5472(98)00017-8) [DOI] [PubMed] [Google Scholar]
- 127.Koob G, Kreek MJ. 2007. Stress, dysregulation of drug reward pathways, and the transition to drug dependence. Am. J. Psychiatry 164, 1149–1159. ( 10.1176/appi.ajp.2007.05030503) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Solomon RL. 1980. The opponent-process theory of acquired motivation: the costs of pleasure and the benefits of pain. Am. Psychol. 35, 691–712. ( 10.1037/0003-066X.35.8.691) [DOI] [PubMed] [Google Scholar]
- 129.Koob GF, Le Moal M. 2008. Review. Neurobiological mechanisms for opponent motivational processes in addiction. Phil. Trans. R. Soc. B 363, 3113–3123. ( 10.1098/rstb.2008.0094) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Belujon P, Grace AA. 2014. Decrease in dopamine neuron activity following acute amphetamine withdrawal is mediated by the BLA and reversed by ketamine. Washington, DC: Society for Neuroscience. [Google Scholar]