Abstract
Qualitative research can explore parts of the subjective patient experience that cannot be detailed with quantitative methods such as surveys. Unfortunately this powerful methodology is underutilized in Plastic Surgery, a specialty where subjective outcomes are more important than traditional outcomes indicators. Qualitative research can be used to add depth to patient satisfaction questionnaires or other quantitative measures. Qualitative methodology can also be used to explore complex issues such as why patients choose to undergo cosmetic surgery or to detail patient experiences following reconstructive surgery. We explain the basics of qualitative research including asking the appropriate research question, applying steps to collect data, data analysis and practical applications of the results.
Keywords: evidence-based medicine, qualitative research
The rise of evidence-based medicine has prompted Plastic Surgery to reexamine the introduction and incorporation of innovative research methodology to this specialty. Unlike other specialties in which mortality can be used as the ultimate indicator, Plastic Surgery has a distinct disadvantage when it comes to measuring objective outcomes. The marriage of art and science that makes Plastic Surgery so unique also makes it difficult to quantify the results. The experiences of our patients are, nonetheless, important to explore to help the continual efforts toward improving care.
The use of patient satisfaction as an outcome metric in both the reconstructive and cosmetic avenues of the Plastic Surgery field is gaining popularity, but because there are no validated Plastic Surgery satisfaction questionnaires, most of those used are ad hoc tools and consist of only a few questions.(1) These methods of measuring patient satisfaction and quality of life raise an abundance of questions. Perhaps the most vexing question is: what does it all mean? Inventories and questionnaires, which often use 5-point Likert scale response choices, can provide a wealth of knowledge, but these response scales may obscure the richness of a patient’s medical experience, for example, issues regarding breast reconstruction choices or a parent’s struggle in deciding whether to proceed with reconstruction for giant melanocytic nevus.(2)
Qualitative research provides “color” to the “black and white” of quantitative research. Quantitative methodology can indicate that patients are merely “somewhat satisfied” with the amount of pre-operative information provided, but it cannot explain why patients feel this way or what to do about it. Furthermore, quantitative methodology is often inadequate for exploring emotional or complex issues such as how patients make decisions or their feelings about outcomes.(3) Qualitative methodology is ideal for exploring these complex topics. Patients are allowed to express their thoughts and feelings, rather than simply checking a box. This “in their own word” concept is central to qualitative research.(3)
Qualitative research in Plastic Surgery
An informal MEDLINE search revealed that there have been relatively few published qualitative studies of Plastic Surgery topics. Of the 11 studies we identified, 8 pertained to breast surgery, primarily breast reconstruction after mastectomy.(4-11) Only 3 of the 11 qualitative studies were published in surgical journals: one each in Annals of Plastic Surgery, British Journal of Plastic Surgery and Plastic and Reconstructive Surgery.(9, 11, 12) The rest were published in nursing, psychiatric or psychology journals. Clearly there is a need to bring qualitative methodology to a variety of topics, both reconstructive and aesthetic, in the Plastic Surgery specialty.
But planning a qualitative study can be daunting; it is completely different than planning a quantitative study. Data collection takes much more time than administering a survey. Special training may be needed to collect the data. The results are often not immediately apparent and the data analysis can be difficult. The whole process is time-consuming. But when well executed, the results can bring far more insight into the patient experience than any other form of research.
The goal of this paper is to provide a practical overview of qualitative methodology. This is by no means an exhaustive exploration of the topic. Qualitative methodology is deeply rooted in theory and covering each of these theories is beyond the scope of this article.
Clinical questions suitable for qualitative methodology
Qualitative research is ideal to explore psychosocial issues of Plastic Surgery, such as patient satisfaction. This methodology cannot predict patient satisfaction, but can help explain why a particular patient is satisfied.(13) Qualitative research is also helpful to explore complex issues surrounding a patient’s decision to undergo elective cosmetic surgery or to better understand how patients and their families make treatment decisions. Another possible qualitative topic could be experiences during recovery from surgery. Any issue that cannot easily be quantified, or about which little is known, is a good candidate for qualitative research.
The development of qualitative research questions is undertaken following one of many theories. There are many theories to base your qualitative research project on, many more than can be examined in this paper. We will focus instead on grounded theory, the theory we have the most experience with and find to be most useful in clinical research.
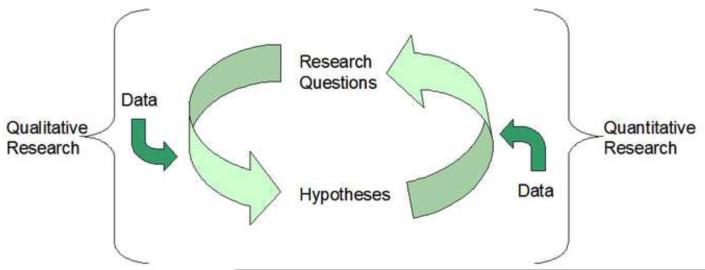
The main tenant of grounded theory is that the “truth” will unfold as the data are analyzed.(3) This means that data collection is begun with no hypotheses. There is certainly an aim, but there are no preconceived notions about what the data will reveal. A hypothesis about how certain concepts interact and relate to one another is allowed to emerge through the process of data analysis. This hypothesis can be tested using quantitative methods. This leads to a cycle between qualitative and quantitative research. (Figure 1) Qualitative research leads to hypotheses, which can be tested with quantitative research. The findings from quantitative research may lead to answers, but more likely lead to additional research questions, which can be further explored with qualitative research.
Figure 1.
The cycle between qualitative and quantitative research.
Qualitative methodology can also be used to provide more detail to a theory that has been tested using quantitative methods. This can make the theory more compelling by adding personal insights to make the theory more human.
Types of qualitative research
Data collection in qualitative research can take two distinct forms: observation or interaction.(14) Observational research, such as ethnography, is the wheelhouse of cultural anthropology, providing rich information about the interactions and relationships of a particular family, professional or social group. Observational research has the flavor of “a fly on the wall” analogy, in which the observer passively records the interactions amongst the study subjects to distill the dynamics of these exchanges into understandable concepts. This methodology is rooted in social science theories and its utility to clinical research is limited. Thus we will focus this guide on interactional research: interviews and focus groups.
Interviews
One-on-one interviews make up the bulk of qualitative research. Speaking individually with participants, either in a structured or unstructured manner, allows for follow-up questions and elaboration that a survey simply cannot provide. Interviews are a good way to discover potentially modifiable factors for improving the patient experience.(15) The level of detail that emerges is determined by the “structuredness” of the interview. (Figure 2)
Figure 2.
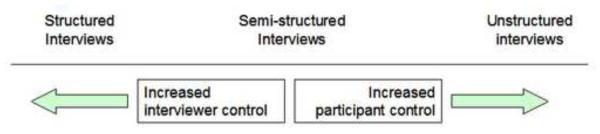
The interviewer and participant control vary with the “structuredness” of the interview
Structured
Structured interviews take the form of a series of open-ended survey questions, allowing participants to respond freely, but with only limited follow-up. (16) In these types of interviews, the interviewer asks participants ordered questions from a prepared list. Questions may require some follow-up comments, but the interviewer does not allow the participant to venture off-topic. Structured interviews are useful for drawing out details on a topic for which much is known, rather than for exploring new topics. They are also appealing when specific information is desired, because the interviewer controls the flow of the discussions.
Semi-structured
Semi-structured interviews allow for much more elaboration than structured interviews, but still allow the interviewer to introduce the topics. An interview guide is developed that lists the topics to be covered and possible questions to pose. (16) Participants are almost always probed to see if they have more information to provide after they finish responding. Participants are also allowed to digress to a certain degree. Often these digressions contain useful information or can spawn additional questions.
The balance of the ability of participants to discuss matters that are important to them and interviewer control make semi-structured interviews a favorite amongst researchers for virtually any type of research question. We recently completed a qualitative study of the recovery experience following type III-B or III-C tibial fracture in which we used semi-structured interviews.(17) We developed our interview guide to cover topics such as injury information, physical recovery, the injury’s effects on work, social and family life and questions about participants’ experiences with medical care. The interviewer got the interview started with the general question, “Could you please tell me a little bit about your lower leg injury, such as how and when it occurred?” Participants would respond to this question and often provide information that lead into additional questions in the interview guide, but not necessarily in the order we had intended. The interviewer assured that all topics were covered, while allowing the participants to talk about other topics related to their injury that interested them, which included some topics that we did not anticipate. Several participants mentioned the increased difficult with sexual activity following their injury. Through the use of semi-structured interviews, we discovered topics that we would have not thought to include in the interview guide.
Unstructured
Unstructured interview, as the name would imply, are simply free-form discussions, bordering on casual conversation. The interviewer prepares a general question that describes the overarching research concept and then allows the participant to respond and talk about any topics they choose.(16) The interviewer responds to lulls in the conversation as any interested listener would, asking the participant follow-up questions, but never introducing a new topic. Unstructured interviews are useful when there is little known about a topic.
Focus groups
Although the focus group technique was conceived by a social scientist,(18) this method quickly became a powerful tool of marketing departments everywhere. But whether for marketing or in medicine, focus group technique takes similar form. A focus group is essentially a group semi-structured interview involving 6-12 member of the population in question who gather and are lead by a moderator through a discussion of a particular topic. The idea of focus groups is that group members will talk amongst themselves and feed off of each other’s ideas and input. The moderator keeps the discussion focused and ensures that all participants get a chance to speak and that the group is not being dominated by one person. Focus groups can be used to identify popular views on healthcare issues or community interventions.(15)
Analyzing qualitative data
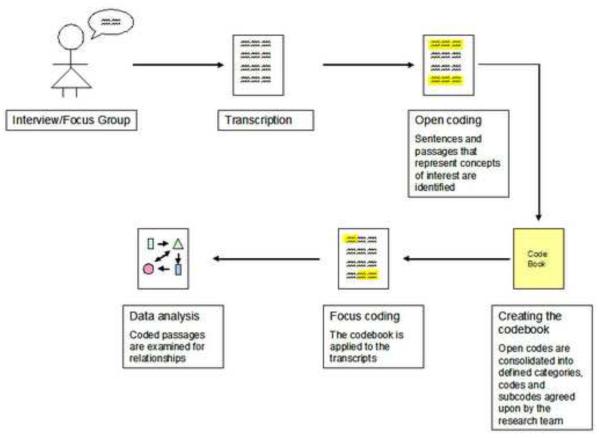
Regardless of which data collection technique is used, interviews or focus groups should be audio or video recorded. This allows the interviewer to minimize note-taking to focus attention on the participant for a more conversational feel. This can put the participant at ease, resulting in richer detail. Following the framework of grounded theory, data analysis should take place in a step-wise fashion.(3) (Figure 3) One note before we detail the steps of data analysis: The data analysis process benefits from the participation of multiple individuals. Qualitative methodology, unlike quantitative methodology, is based on the idea that each individual researcher will lend his/her own point-of-view to the data. Thus, the more members of the research team who are involved in the data analysis process, the more complete the data analysis can be.
Figure 3.
Illustrated steps to qualitative data analysis
A step-wise approach to qualitative data analysis
Step 1: Transcription
Audio or video recording of the interviews or focus groups should be transcribed verbatim, which should include all verbal filler (such as “um” or “you know”) and grammatical errors, as well as indicating long pauses, laughter and changes in tone or volume of voice. For video recordings, note body language or facial expressions. If there are spots where participants are unintelligible, note those as well. After transcription, each interview should be listened to by someone who did not do the original transcription, to check for accuracy and to try to decipher unintelligible words or phrases.
Step 2: Open coding
Once the transcripts are finalized, coding can begin. There are several computer programs that can help organize the transcripts and codes, by combining the coding of several individuals, sorting and ranking codes, and searching for passages or key words. These programs can be extremely helpful, but they are often quite expensive. Unless the researcher will be performing multiple, large-scale qualitative studies, one can probably get by doing it the “old fashion” way. For our study of lower limb trauma, we did not use a software package, so we will describe the data analysis process as we achieved it.
The first type of coding that will be done is open coding. Open coding is the process of identifying sentences or passages in the transcripts that represent the concepts of interest.(19) One needs not be judicious during open coding. Any passage that seems interesting should be noted; there will be an opportunity to “weed out” unnecessary information later. Open coding should be performed by as many members of the research team as possible. At least two people need to be involved in open coding. Passages of interest should be indicated in some way (such as highlighting) and the general tone of the passages should be given a memorable name, or open code.(19) For instance, when a participant talked about his/her occupation or ability to work, we highlighted that passage and noted it as “work.” Some passages may fit into multiple categories; the discussion of ability to work, mentioned above, could also be noted as “physical functioning.”
The basic idea of open coding is to separate the “possibly interesting” from the “truly uninteresting.” In the next steps we will explain how to refine the results further, but right now quantity is much better than quality. After open coding is completed, each research team member should generate a list of all the open codes they created and a few passages that best exemplify that open code.
Step 3: Creation of the codebook
When open coding has been completed, all research team members should meet to discuss their open code list. It helps to have a white board for this process. One team member will begin by listing the open codes, followed by other team members who will add codes that do not already appear on the list. Once a large list of open codes is created, the team should discuss which codes are related, which codes can be collapsed and which codes can be eliminated altogether.
Conceptual ordering, the categorizing and ranking of ideas, is useful when developing the codebook. This process involves listing the topics mentioned and noting how often they are mentioned. There is no need at this point to develop relationships between codes, that will take place at a higher level of analysis.(20)
The codes that will be included in the codebook can be found using thematic analysis, the process of noting themes among the interviews and grouping those themes into larger thematic sections.(8) The codebook will take these themes and give them named codes for identification. These codes should represent the main themes of the interviews or focus groups and should apply to the majority of the transcripts. Try to not get too specialized. The codes should be organized into categories, codes and sub-codes. For example, our qualitative study of severe tibial fractures generated 3 categories, 22 codes and 14 sub-codes.
After all the team has agreed on the codes, definitions of the codes need to be created. These definitions will describe what types of passages should be tagged with a code, and which should not. The idea is to create definitions so clear that someone who has never seen either can sit down with a transcript and the codebook and satisfactorily code the transcript. It may take some discussion to get all group members to agree as to what should be included and excluded from each code. Code definitions need not be exhaustive, but provide just enough detail that there is little ambiguity as to what a particular passages should be coded as. We have included a section of the codebook used for our lower limb trauma study in Appendix A.
Step 4: Focus coding
Once the codebook has been completed, focus coding can begin. Using the rules established by the codebook, the transcripts are reread and passages that fit one of the decided upon codes or sub-codes are indicated and labeled.(19) All passages should be listed in a separate document with its code, identifier for transcript and page or line number. We used the Excel program for this process. Each passage was included with the code (and sub-code, if applicable), participant identification number, transcript page number and other variables for participant demographics and injury information.
After all team members have coded all transcripts, the team should meet to go through each of the passages to agree upon the appropriate code. Once the research team has agreed upon all passages and all codes, the actual data analysis can begin.
Step 5: Data analysis
As we have previously mentioned, there are a host of qualitative methodology theories, and each one has its own method of data analysis. But all the methods share some of the same features. The first step in qualitative data analysis is content analysis. This is similar to conceptual ordering, as explained in Step 3. The codes are analyzed to see which appeared the most frequently.(19) This will give an idea of where to begin to look for connections between codes, either temporally or conceptually. Finally, the relationships between codes are examined. The ultimate goal of analysis is dependant on the particular qualitative methodology being used. When using grounded theory, the goal is to develop a hypothesis of how different concepts (codes) relate to each other. This will lead to the construction of a conceptual framework, detailing how the different concepts related to one another.(21) This hypothesis can then be tested, if desired, using quantitative methodology.
Disadvantages of qualitative methodology
There are several important limitations to consider when planning or evaluating qualitative research. Although all research methods are subject to investigator bias, it is especially important in qualitative research. Any preconceived notions of what the data will reveal can influence the way the interview guide is written, the way that the interviewer asks questions and directs the interview or focus group, and in the selection of passages and codes.(22) But this is sometimes seen as a positive, rather than negative. In some of the more theory-based qualitative methodologies, investigators are encouraged to explore and incorporate their biases via “memos” made to themselves after each participant encounter.(23)
To control for bias in the writing of the interview guide or in data analysis, the researcher should incorporate as many team members as possible in the development and data analysis process. An easy way to control for bias is to use an independent interviewer or moderator to conduct the interviews or focus groups. Independent professional interviewer are proficient at putting participants at ease, so that they feel that they can reveal anything to the interviewer without fear of being judged. What makes participants comfortable varies from subject to subject. Participant comfort is most important when the interviewer is a member of a majority population and the participant is a member of a minority or otherwise marginalized population. If this is your situation or if your study covers especially sensitive topics, such as illicit behavior, it may be beneficial to “audition” interviewers with members of the sample population to gauge their comfort.
A good interviewer should also be firm and able to steer the conversation back on track if necessary. This is most important for focus group moderators who must manage multiple personality types to ensure that everyone gets an opportunity to speak. Professional focus group moderators can be used, as they are well versed in this aspect of focus group management.
Another limitation to qualitative research is low generalizability. Because qualitative research seeks to closely examine the experiences of individuals, it does not lend itself to generalization to a larger population. But this was never the intent of qualitative research.(8) This methodology was intended to explore topics on a level that quantitative research cannot,(3) not to speak for the entire population. However, this does not mean that because it is not generalizable, there is nothing to learn from qualitative research. The “roadmap” that is formed by qualitative data analysis helps surgeons to navigate similar situations.(24)
Interpreting and deriving evidence from qualitative research
Are the results valid?
Validity takes on a different meaning in qualitative research. Statistical validity refers to how closely one’s research results reflect reality. But qualitative research believes that everyone has his/her own reality and that all these realities are “correct.”(25) The presence of multiple realities makes it rather difficult to apply the statistical definition of validity, which presumes a singular reality.
Rather than judge the statistical validity of a qualitative study, it would be more beneficial to instead, judge the rigor with which the study was performed. After systematic reviews discovered that articles describing qualitative studies rarely report all factors that affect readers’ ability to critically assess the results, Tong et al. developed the Consolidated Criteria for Reporting Qualitative Research (COREQ) to guide researchers through the qualitative writing process.(15) The criteria include a 32-item checklist which covers factors related to the research team, study design and analysis and findings. (Table 1) When planning a study, using this checklist can ensure that the research will be as rigorous as possible.
Table 1.
Consolidated criteria for reporting qualitative studies (COREQ) checklist
| Domain 1: Research team and reflexivity | |
| Personal characteristics | |
| 1. Interviewer/facilitators | Which author(s) conducted the interview or focus group? |
| 2. Credentials | What were the researcher’s credentials? |
| 3. Occupation | What was their occupation at the time of the study? |
| 4. Gender | What was the researcher’s gender? |
| 5. Experience and training | What experience or training did the researcher have? |
| Relationship with participants | |
| 6. Relationship established | Was a relationship established prior to study commencement? |
| 7. Participant knowledge of this interviewer |
What did the participants know about the researcher? |
| 8. Interviewer characteristics | What characteristics were reported about the interview/facilitator? |
| Domain 2: Study design | |
| Theoretical framework | |
| 9. Methodological orientation and theory |
What methodological orientation was stated to underpin the study? |
| Participant selection | |
| 10. Sampling | How were participants selected? |
| 11. Method of approach | How were participants approached? |
| 12. Sample size | How many participants were in the study? |
| 13. Non-participation | How many people refused to participate or dropped out? Reasons? |
| Setting | |
| 14. Setting of data collection | Where was the data collected? |
| 15. Presence of non-participants | Was anyone else present besides the participants and researchers? |
| 16. Description of sample | What are the important characteristics of the sample? |
| Data collection | |
| 17. Interview guide | Were questions, prompt, guides provided by the authors? Was it pilot tested? |
| 18. Repeat interviews | Were repeat interviews carried out? If yes, how many? |
| 19. Audio/visual recording | Did the research use audio and/or visual recording to collect the data? |
| 20. Field notes | Were field notes made during and/or after the interview or focus group? |
| 21. Duration | What was the duration of the interviews or focus groups? |
| 22. Data saturation | Was data saturation discussed? |
| 23. Transcripts returned | Were transcripts returned to participants for comment and/or correction? |
| Domain 3: Analysis and findings | |
| Data analysis | |
| 24. Number of data coders | How many data coders coded the data? |
| 25. Description of the coding tree | Did authors provide a description of the coding tree? |
| 26. Derivation of themes | Were themes identified in advance or derived from the data? |
| 27. Software | What software, if applicable, was used to manage the data? |
| 28. Participant checking | Did participants provide feedback on the findings? |
| Reporting | |
| 29. Quotations presented | Were participant quotations presented to illustrate the themes/findings? |
| 30. Data and findings consistent | Was there consistency between the data presented and the findings? |
| 31. Clarity of major themes | Were major themes clearly presented in the findings? |
| 32. Clarity of minor themes | Is there a description of diverse cases or discussion of minor themes? |
Can the results be applied to my patients?
Qualitative research can provide rich detail that quantitative research simply cannot. Using grounded theory, researchers can use these details to develop a hypothesis that can then be tested using quantitative methodology. But perhaps the goal is not to inspire further research, but to directly improve the experiences of patients. Applicable items can be discovered from direct questions (“What would make your experience better?”) but can also be found in the responses to other, often unrelated questions. In our study of lower limb trauma, we asked participants if there was anything the medical staff could have done to improve their recovery experience. Patients almost always responded that there was not, or gave a superficial response such as softer beds or prettier nurses. But during data analysis, we found that several participants who had undergone amputation felt that the doctors were too busy to respond to their questions, so they just did not ask. These participants reported that it would have been nice to discuss practical, as well as emotional, issues with someone who had a similar experience. These were the same patients who responded that they felt nothing was missing from their recovery experience, but clearly there was something the ancillary medical staff such as counselors could have been helpful. Careful data analysis will allowed us to “read between the lines” of simple responses to find what is truly important to patients.
As the practice of medicine moves more into the realm of a patient-centric approach, patient satisfaction will become more important than ever. The use of qualitative methodology can take the traditional 5-point Likert scale survey to a more insightful level. Qualitative methods can help plastic surgeons to better understand the desires and needs of their patients to continue the ultimate goal to deliver the best care possible.
Supplementary Material
Acknowledgments
Supported in part by a Midcareer Investigator Award in Patient-Oriented Research (K24 AR053120) from the National Institute of Arthritis and Musculoskeletal and Skin Diseases (To Dr. Kevin C. Chung).
References
- 1.Clapham P, Pushman A, Chung KC. A systematic review of applying the satisfaction outcome in plastic surgery literature. Plast Reconstr Surg. doi: 10.1097/PRS.0b013e3181d51276. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Watt AJ, Kotsis SV, Chung KC. Risk of melanoma arising in large congenital melanocytic nevi: a systematic review. Plast Reconstr Surg. 2004;113:1968–1974. doi: 10.1097/01.prs.0000122209.10277.2a. [DOI] [PubMed] [Google Scholar]
- 3.Strauss A, Corbin J. Basics of Qualitative Research. Sage Publications; Thousand Oaks, CA: 1998. Introduction. [Google Scholar]
- 4.Abu-Nab Z, Grunfeld EA. Satisfaction with outcome and attitudes towards scarring among women undergoing breast reconstructive surgery. Patient Educ Couns. 2007;66:243–249. doi: 10.1016/j.pec.2006.12.008. [DOI] [PubMed] [Google Scholar]
- 5.Hill O, White K. Exploring women’s experiences of TRAM flap breast reconstruction after mastectomy for breast cancer. Oncol Nurs Forum. 2008;35:81–88. doi: 10.1188/08.ONF.81-88. [DOI] [PubMed] [Google Scholar]
- 6.Klassen AF, Pusic AL, Scott A, et al. Satisfaction and quality of life in women who undergo breast surgery: a qualitative study. BMC Womens Health. 2009;9:11. doi: 10.1186/1472-6874-9-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nissen MJ, Swenson KK, Kind EA. Quality of life after postmastectomy breast reconstruction. Oncol Nurs Forum. 2002;29:547–553. doi: 10.1188/02.ONF.547-553. [DOI] [PubMed] [Google Scholar]
- 8.Sandham C, Harcourt D. Partner experiences of breast reconstruction post mastectomy. Eur J Oncol Nurs. 2007;11:66–73. doi: 10.1016/j.ejon.2006.05.004. [DOI] [PubMed] [Google Scholar]
- 9.Shakespeare V, Postle K. A qualitative study of patients’ views on the effects of breast-reduction surgery: a 2-year follow-up survey. Br J Plast Surg. 1999;52:198–204. doi: 10.1054/bjps.1999.3106. [DOI] [PubMed] [Google Scholar]
- 10.Wolf L. The information needs of women who have undergone breast reconstruction. Part II: Information giving and content of information. Eur J Oncol Nurs. 2004;8:315–324. doi: 10.1016/j.ejon.2003.12.013. [DOI] [PubMed] [Google Scholar]
- 11.Yueh JH, Houlihan MJ, Slavin SA, et al. Nipple-sparing mastectomy: evaluation of patient satisfaction, aesthetic results, and sensation. Ann Plast Surg. 2009;62:586–590. doi: 10.1097/SAP.0b013e31819fb1ac. [DOI] [PubMed] [Google Scholar]
- 12.Darisi T, Thorne S, Iacobelli C. Influences on decision-making for undergoing plastic surgery: a mental models and quantitative assessment. Plast Reconstr Surg. 2005;116:907–916. doi: 10.1097/01.prs.0000177691.81162.e5. [DOI] [PubMed] [Google Scholar]
- 13.Rusinova K, Pochard F, Kentish-Barnes N, et al. Qualitative research: adding drive and dimension to clinical research. Crit Care Med. 2009;37:S140–146. doi: 10.1097/CCM.0b013e31819207e7. [DOI] [PubMed] [Google Scholar]
- 14.Miller WL, Crabtree BF. Primary care research: a multimethod typology and qualitative road map. In: Crabtree BF, Miller WL, editors. Doing Qualitative Research: Multiple Strategies. Sage Publications; Newbury Park, CA: 1992. [Google Scholar]
- 15.Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19:349–357. doi: 10.1093/intqhc/mzm042. [DOI] [PubMed] [Google Scholar]
- 16.Gillham B. Research Interviewing: The Range of Techniques. Open University Press; Berkshire, England: 2005. The semi-structured interview; pp. 70–79. [Google Scholar]
- 17.Shauver MJ, Aravind MS, Chung KC. A qualitative study of recovery from type III-B and III-C tibial fractures. Plast Reconstr Surg. doi: 10.1097/SAP.0b013e3181d50eba. in submission. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kaufman MT, Robert K. The New York Times. New York, NY: 2003. Merton, versatile sociologist and father of the focus group, dies at 92. [Google Scholar]
- 19.Strauss A, Corbin J. Basics of Qualitative Research. Sage Publications; Thousand Oaks, CA: 1998. Open coding. [Google Scholar]
- 20.Strauss A, Corbin J. Basics of Qualitative Research. Sage Publications; Thousand Oaks, CA: 1998. Description, conceptual ordering and theorizing. [Google Scholar]
- 21.Strauss A, Corbin J. Basics of Qualitative Research. Sage Publications; Thousand Oaks, CA: 1998. Selective coding. [Google Scholar]
- 22.Cohen DJ, Crabtree BF. Evaluative criteria for qualitative research in health care: controversies and recommendations. Ann Fam Med. 2008;6:331–339. doi: 10.1370/afm.818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Strauss A, Corbin J. Basics of Qualitative Research. Sage Publications; Thousand Oaks, CA: 1998. Practical considerations. [Google Scholar]
- 24.Giacomini MK, Cook DJ. Users’ guides to the medical literature: XXIII. Qualitative research in health care A. Are the results of the study valid? Evidence-Based Medicine Working Group. JAMA. 2000;284:357–362. doi: 10.1001/jama.284.3.357. [DOI] [PubMed] [Google Scholar]
- 25.Willis JW. Foundations of Qualitative Research: Interpretative and Critical Approaches. Sage Publications; Thousand Oaks, CA: 2007. Foundational issues: postpositivist and critical perspectives. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.