Abstract
Two subtypes of the corticotropin-releasing factor (CRF) receptor, CRF1 and CRF2, differentially modulate brain functions such as anxiety and memory. To facilitate the analysis of their differential involvement, we developed a CRF1-specific peptidic agonist by synthesis of chimeric peptides derived from human/rat CRF, ovine CRF (oCRF), and sauvagine (Svg). High affinity to the CRF-binding protein was prevented by introduction of glutamic acid in the binding site of the ligand. The resulting chimeric peptide, [Glu21,Ala40][Svg1–12]×[human/rat CRF14–30]×[Svg30–40], named cortagine, was analyzed pharmacologically in cell culture by using human embryonic kidney-293 cells transfected with cDNA coding for CRF1 or CRF2, in autoradiographic experiments, and in behavior experiments using male C57BL/6J mice for its modulatory action on anxiety- and depression-like behaviors with the elevated plus-maze test and the forced swim test (FST), respectively. We observed that cortagine was more selective than oCRF, frequently used as CRF1-specific agonist, in stimulating the transfected cells to release cAMP. Cortagine's specificity was demonstrated in autoradiographic experiments by its selective binding to CRF1 of brain sections of the mouse. After injection into the brain ventricles, it enhanced anxiety-like behavior on the elevated plus-maze at a lower dose than oCRF. Whereas at high doses, oCRF injected into the lateral intermediate septum containing predominantly CRF2 increased anxiety-like behavior as CRF2-specific agonists do, cortagine did not. In contrast to its anxiogenic actions, cortagine reduced significantly the immobility time in the FST as described for antidepressive drugs. Thus, cortagine combines anxiogenic properties with antidepressive effects in the FST.
Corticotropin-releasing factor (CRF), a 41-residue peptide hormone (1), is the major regulator of the hypothalamus–pituitary–adrenal axis (2), modulates important brain functions such as anxiety, learning, food intake, and locomotion, and is involved in anxiety and mood disorders (3, 4). CRF acts through two G protein-dependent CRF receptor subtypes, CRF1 and CRF2, derived from two separate genes (reviewed in ref. 5) and binds with high affinity to a binding protein (CRFBP), which serves as a pharmacologically significant reservoir of endogenous CRF (6, 7). Several CRF1 and CRF2 splice variants have been identified (5, 8). In rodents, only the splice variants CRF1α, CRF2α, and CRF2β are of physiological relevance (5). CRF1α and CRF2α are produced in brain tissue, whereas CRF2β is mainly located in blood vessels (9).
CRF1 and CRF2 participate differentially in various biological functions (3). Thus, activation of the hypothalamus–pituitary–adrenal axis in response to a stressful stimulus is mainly achieved through CRF1 (10). It was demonstrated by gene deletion experiments that anxiety-like behavior is enhanced predominantly through CRF1 (11, 12), whereas it is reduced through CRF2 (10, 13). Pharmacological experiments discriminating between regional actions of CRF1 and CRF2 revealed that CRF2 of the lateral intermediate septum mediates stress-induced enhancement of anxiety-like behavior (14), whereas CRF2 accessed through the brain ventricles is anxiolytic (13). In contrast, CRF1 accessed by CRF via the brain ventricles enhances anxiety-like behavior (15). Several natural CRF-like peptides with different CRF receptor subtype specificity have been characterized. Thus, human/rat CRF (h/rCRF) and ovine CRF (oCRF) exhibit preference for CRF1, whereas urocortin (Ucn)I (16) is a nonselective ligand (3, 5). Recently, UcnII (17, 18) and UcnIII (18, 19) were identified on the basis of homology analysis of data derived from genomic sequence databases and characterized as highly CRF2-selective agonists. In contrast, no natural agonists with a similar selectivity for CRF1 have been identified to date, and no peptidic CRF1-specific agonist has been synthesized.
At this time, oCRF is the agonist of choice for the selective stimulation of CRF1 in behavioral experiments, because it preferentially binds to CRF1. oCRF's binding constants for CRF1 and CRF2 differ by two orders of magnitude (20, 21). However, because of the high local agonist concentration that often occurs when drugs are directly administered into the animal brain, the use of oCRF for the stimulation of CRF1 is accompanied by unwanted CRF2-mediated side effects (C.T. and J.S., unpublished data). In addition, displacement of endogenous ligand from CRFBP (6) by applied CRF agonists may release CRF-like peptides and thus interfere with the desired selective stimulation of CRF1. To facilitate further elucidation of the physiological role of CRF1, we developed a selective and potent CRF1 agonist on the basis of a chimeric peptide strategy.
Methods
Peptide Synthesis. Peptides were synthesized, purified, and characterized as described in refs. 22 and 23.
Binding Assays and Measurement of Intracellular cAMP Accumulation. Crude membrane fractions were prepared from human embryonic kidney-293 (HEK-293) cells stably transfected with cDNA encoding either rat CRF1α (rCRF1) or mouse CRF2β (mCRF2β) (22). Rat CRFBP (rCRFBP) was produced by HEK-293 cells stably transfected with cDNA encoding rCRFBP C-terminally fused to a His6 sequence (23). Ligand binding analysis was performed with scintillation proximity assays (21, 24). For competition binding assays of rCRF1 and rCRFBP, [125I-Tyr0]h/rCRF was used as radiolabeled peptide, whereas [125I-Tyr0]sauvagine (Svg) was used in a binding assay for mCRF2β. The HEK-293 cells were plated into 24-well cell culture plates (25). Intracellular cAMP was determined with the Biotrak cAMP 125I scintillation proximity assays system (Amersham Pharmacia Biosciences) according to the manufacturer's manual. Stock solutions of peptides were prepared in 10 mM aqueous acetic acid except for oCRF and cortagine, which were dissolved in PBS (pH 7.4).
Determination of Maximum Solubility and Isoelectric Point. After dissolving the peptides in artificial cerebrospinal fluid (aCSF; 124 mM NaCl/26.4 mM NaHCO3/10 mM glucose/3.3 mM KCl/2.5 mM CaCl2/2.4 mM MgSO4/1.2 mM KH2PO4) at pH 7.4, the maximum solubility cmax was determined by measurement of the peptide concentration in the supernate of a precipitate (21). The isoelectric point of the peptides was determined by isoelectric focusing with a Bio-Rad IEF cell system using Bio-Rad IEF strips in the pH range 3–10 (21).
Preparation of Peptide Solutions for Behavioral Experiments. All peptides were dissolved in aCSF except for antisauvagine-30 (aSvg-30) (22), which was initially dissolved in 10 mM aqueous acetic acid and diluted with 2× aCSF. The final pH of the peptide solutions was 7.4. The exact peptide concentrations of the injection solutions were determined by amino acid analysis as described in ref. 22.
Animals. Nine-week-old male C57BL/6J mice (Centre D'Elevage Janvier, Le Genest Saint Isle, France) were individually housed in Macrolon cages as recommended by the Society for Laboratory Animal Science (Hannover, Germany). All experiments were carried out in accordance with the European Council Directive (86/609/EEC) with the permission of the District Government of Braunschweig, State of Lower Saxony, Germany, which is in full agreement with the American Psychological Association (Washington, DC) ethical guidelines. All efforts were made to minimize animal suffering. The number of mice per group was 9–11.
Autoradiography. Coronal sections (20 μm) of CRF1+/+ and CRF1-/- mice (provided by Wylie Vale, The Salk Institute for Biological Studies, La Jolla, CA) were thawed to room temperature and allowed to dry for 20 min. The sections were preincubated for 1 min in incubation buffer (PBS supplemented with 10 mM MgCl2/2 mM EGTA/0.1% BSA, pH 7.0) and then incubated for 40 min at room temperature in incubation buffer containing 200 pM [125I-Tyr0]Svg, a nonspecific CRF receptor ligand. Selective displacement was achieved with 1 μM cortagine at CRF1 or mouse UcnII at CRF2. Nonspecific binding was determined by addition of 1 μM Svg. The slides were then washed for 2 min with ice-cold PBS supplemented with 0.01% Triton X-100 at pH 7.0 and water. Slides were dried rapidly under a stream of cold air and exposed to Biomax MR film (Kodak) for 4 days at -80°C.
Behavioral Experiments. Anxiety-like behavior of C57BL/6J mice cannulated in the lateral ventricles or lateral intermediate septal area (14) was examined 30 min after injection of the CRF1 agonist under investigation for 5 min in the elevated plus-maze (EPM) test (26). The CRF2-selective antagonist aSvg-30 in aCSF or aCSF alone was injected 45 min before the EPM test. The behavior of the mice was recorded by a video camera connected to a computer and analyzed by the software videomot 2 (TSE, Bad Homburg, Germany). The time spent, distance crossed, and number of entries into the open arms, closed arms, and center were recorded. Shift of preference from the open to the closed arms was interpreted as an increase of anxiety-like behavior. Locomotor activity was determined with this test by the distance traveled.
For the forced swim test (FST), C57BL/6J mice cannulated in the lateral ventricles were subjected to swim sessions in individual glass cylinders (height, 39 cm; diameter, 21.7 cm) containing water 15-cm deep at 23–25°C. On day 1, all animals were placed in the cylinder for a preswim session of 15 min. On the test day 24 h later (day 2), the mice were subjected to a test swim session for 6 min. The water was changed between subjects. All test swim sessions were recorded by a video camera positioned directly above the cylinder. A competent observer blind to treatment scored the videotapes. The behavioral measure scored was the duration of immobility, defined as time spent still or only using righting movements to keep the head above water. An increase in immobility time was interpreted as an increase of depression-like behavior. In all behavioral experiments, the injections were carried out bilaterally, and the cannula placement was confirmed for each mouse by histological examination of the brains after methylene blue injection (14). The behavioral data are expressed as mean ± SEM and were analyzed by using two- and one-way ANOVA, with the Bonferroni–Dunn test applied, post hoc, for individual between-group comparisons at the P < 0.05 level of significance.
Results
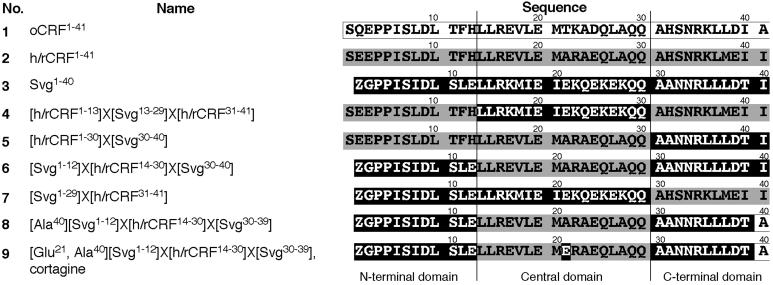
Design of Chimeric Peptides and Analysis of Their Affinity and Biological Potency. For our chimeric peptide strategy we selected oCRF and h/rCRF on the basis of their preferential binding to CRF1 and Svg (27) because of its high hydrophilicity and low isoelectric point (pH 5.1) enhancing solubility in aqueous solution (21). The sequences of oCRF (compound 1, Fig. 1) and h/rCRF (compound 2, Fig. 1) were divided into N-terminal (residues 1–13), central (residues 14–30), and C-terminal (residues 31–40) domains (Fig. 1) on the basis of the recent finding that CRF contains segregated receptor-binding sites at its N terminus and C terminus (28). These domains were used as building blocks and combined with sequences from Svg (compound 3, Fig. 1) to generate different chimeric peptides (Fig. 1). It was observed that compound 5, but not compound 4, exhibited low affinity for CRF2 and high selectivity for CRF1 (Table 1). Therefore, it was concluded that residues 14–30 of h/rCRF were responsible for a decrease in affinity to CRF2. This conclusion was in agreement with the finding that compound 6 containing the central domain of h/rCRF, but not compound 7, was selective for CRF1 (Table 1). On the basis of its low affinity to CRF2, compound 6 was selected for further development. An additional rationale for the selection of compound 6 as lead compound was its N-terminal pyroglutamic acid derived from the Svg sequence (Fig. 1). The presence of this cyclic residue may prevent degradation by major aminopeptidases that require a free α-amino group for their action (29) and thereby increase the stability of compound 6 under in vivo conditions.
Fig. 1.
Development of cortagine as chimeric peptide derived from oCRF, h/rCRF, and Svg. The three main building blocks of the chimeric peptides, the N-terminal, central, and C-terminal domains, are indicated. Sequences derived from h/rCRF, Svg, and oCRF are underlain in gray, black, and white, respectively. Z, pyroglutamic acid.
Table 1. Binding affinites of oCRF, h/rCRF, Svg, and their chimeric analogs.
| IC50, nM
|
|||
|---|---|---|---|
| Compound | rCRF1 | mCRF2β | rCRFBP* |
| 1 | 1.8 (1.1—2.4) | 160 (120—200) | 450 (420—480) |
| 2† | 1.6 (1.3—1.9) | 42 (25—59) | 0.54 (0.38—0.71) |
| 3† | 0.52 (0.29—0.74) | 0.9 (0.72—1.1) | 57 (45—70) |
| 4 | 0.47 (0.18—0.77) | 0.69 (0.45—0.93) | ND |
| 5 | 2.0 (0.80—3.1) | 330 (140—530) | ND |
| 6 | 9.5 (4.8—14) | 700 (490—910) | ND |
| 7 | 1.8 (0.75—2.8) | 0.98 (0.59—1.4) | ND |
| 8 | 1.8 (1.4—2.1) | 400 (360—450) | 1.9 (1.8—2.0) |
| 9‡ | 2.6 (1.6—3.4) | 540 (480—590) | >1,000 |
IC50 values are the mean of at least four experiments performed in duplicate; 95% confidence intervals are given in parentheses. ND, not determined.
The intermediate compounds of the agonist development were not tested for their affinity to rCRFBP
Binding data taken from Eckart et al. (21)
Cortagine
On the basis of the finding that neither Glu-2 of the N-terminal domain nor the central residues Ala-22, Arg-23, and Glu-25 of h/rCRF have a significant influence on receptor selectivity (21, 30), only the C-terminal residues 38, 39, and 41 were considered for amino acid replacements. A comparison of the sequences of oCRF, h/rCRF, and Svg revealed that oCRF binding preferentially to CRF1 shares residues Leu-38 and Asp-39 with the nonselective Svg in equivalent positions (Fig. 1). It was therefore hypothesized that Ala-41 of oCRF may contribute to the binding preference of this ligand. This hypothesis was first tested by the synthesis and characterization of [Ala41]h/rCRF. In comparison with h/rCRF, [Ala41]h/rCRF showed an increase in CRF1 selectivity by a factor of 3 and thus a similar selectivity as oCRF (data not shown). As expected on the basis of this result, a peptide highly selective for CRF1 was obtained when the same replacement was carried out for compound 6 to generate compound 8 (Fig. 1). In comparison with compound 6, compound 8 exhibited a >5-fold increase in affinity to CRF1, whereas only a slight increase of affinity to CRF2 was found (Table 1).
The high affinity of compound 8 to CRFBP (Table 1) was removed by employing the recently reported single amino acid switch concept determining the affinity to CRFBP (21). Accordingly, Ala-21 of compound 8 was replaced by a Glu residue, an exchange that has been shown to decrease the affinity of h/rCRF to CRFBP by two orders of magnitude (21). Compound 9 (Fig. 1), obtained by this change, bound with high affinity to CRF1, whereas the affinity to CRFBP was abolished (Table 1). Replacement of Met-20 with norleucine to prevent the formation of methionine sulfoxide, a modification that is known to abolish the bioactivity of CRF-like peptides (2), resulted in a significant decrease of affinity to CRF1 (data not shown) and was therefore not introduced. We named compound 9, the final product of our development, cortagine. The overall enhanced specificity of cortagine over oCRF was indicated by the ratio of the binding affinities to CRF1 and CRF2 [IC50(mCRF2β)/IC50(rCRF1); Table 1]. For cortagine and oCRF, values of 208 and 89, respectively, were found.
The biological potency of cortagine and oCRF was evaluated by the determination of the EC50 values for intracellular accumulation of cAMP in transfected HEK-293 cells. In agreement with the binding data, the biological potencies of cortagine and oCRF were high at rCRF1 and about one to two orders of magnitude lower at mCRF2β (Table 2). The enhanced selectivity of cortagine was reflected by the ratios of the biological potencies [EC50(mCRF2β)/EC50(rCRF1); Table 2]. Values of 89 and 19 were found for cortagine and oCRF, respectively.
Table 2. Comparison of the pharmacological and physicochemical properties of cortagine and oCRF.
| Biological potency EC50, nM
|
||||
|---|---|---|---|---|
| Peptide | rCRF1 | mCRF2β | cmax, μM | pl* |
| Cortagine | 0.18 (0.10—0.26) | 16 (11—20) | >1,000 | 4.8 |
| oCRF | 0.47 (0.14—0.80) | 8.8 (6.0—12) | >1,000 | 6.4 |
EC50 values are the mean of at least four experiments performed in duplicate; 95% confidence intervals are given in parentheses.
Isoelectric points were determined by isoelectric focusing
By the analysis of the maximal solubility of cortagine, it was determined that cortagine, like oCRF, was soluble at a concentration of up to 1,000 μM (Table 2), so that there was no limitation for behavioral experiments in view of the agonist doses typically used.
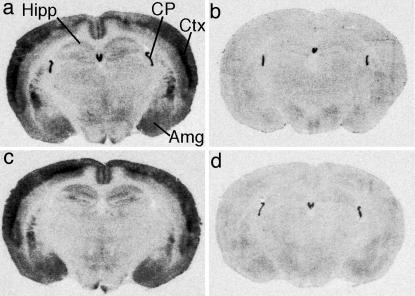
Binding of Cortagine to Native CRF1. Autoradiography of mouse brain sections from CRF1+/+ and CRF1-/- mice was performed to demonstrate cortagine's selectivity for native CRF1 (Fig. 2). The [125I-Tyr0]Svg-binding patterns in the brains of CRF1-/- mice (Fig. 2b) and of CRF1+/+ mice after treatment with cortagine (Fig. 2d) did not significantly differ. CRF receptor visible in the choroid plexus of the brain sections of these animals (Fig. 2 b and d) was identified as CRF2 by displacement with UcnII (Fig. 2c).
Fig. 2.
Autoradiography of CRF receptor subtypes in the mouse brain. (a and b) [125I-Tyr0]Svg-binding (200 pM) on coronal sections at the level of the hippocampus (Hipp) of WT and CRF1-/- mice. (c and d) Selective displacement of CRF2 or CRF1 with UcnII or cortagine, respectively, on brain sections from WT mice. Amg, amygdala; CP, choroid plexus; Ctx, cortex.
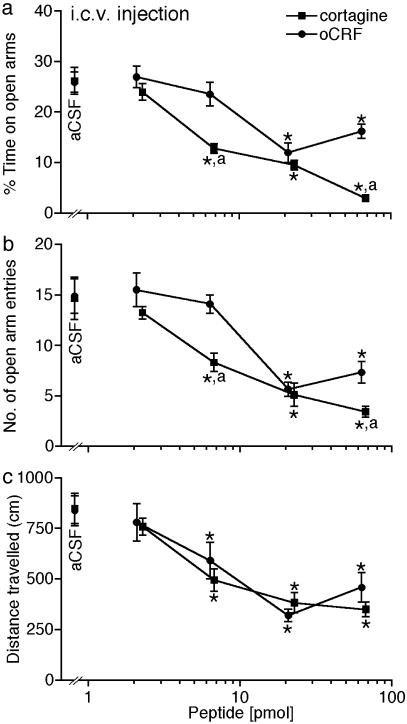
Modulation of Anxiety-Like Behavior by Cortagine. The behavioral effects of cortagine were determined in the EPM test and the FST. It has been demonstrated earlier that activation of CRF1 accessed through the brain ventricles enhances anxiety-like behavior in the EPM test (21), the most frequently used rodent model of anxiety, and suppresses locomotor activity (31) under various conditions. Therefore, we performed a series of behavior experiments with the EPM test. A two-way ANOVA with treatment and dose as between-subject factors indicated significant treatment and dose main effects and significant interaction after administration of peptides intracerebroventricularly (i.c.v.) into the lateral ventricles of male C57BL/6J mice 30 min before testing. The values for the percent time spent in the open arms [F(1, 80) = 16.57, P < 0.05 for treatment; F(4, 80) = 36.68, P < 0.05 for dose; and F(4, 80) = 5.38; P < 0.05 for interaction] (Fig. 3a) and number of open arm entries [F(1, 80) = 10.66, P < 0.05 for treatment; F(4, 80) = 28.27, P < 0.05 for dose; and F(4, 80) = 6.21, P < 0.05 for interaction] (Fig. 3b) revealed a significantly higher anxiogenic potency of cortagine than of oCRF (Bonferroni–Dunn test, P < 0.05, for percent time spent and number of open arm entries of the EPM). The significant interaction was due to differences between the 30-ng doses of cortagine and oCRF in modulating anxiety-like behavior in the EPM test as confirmed by analyses of simple main effects of dose. In particular, 30 ng of cortagine but not of oCRF significantly decreased the percent time spent in the open arms [F(1, 18) = 15.37, P < 0.05] and number of open arm entries [F(1, 18) = 10.89, P < 0.05] of the EPM test. Thus, cortagine was more potent than oCRF under these conditions. Interestingly, the peptides tested did not differ in their ability [F(1, 80) = 0.85, P > 0.05] to reduce locomotor activity (Fig. 3c).
Fig. 3.
Enhancement of anxiety-like behavior by cortagine. i.c.v. administered 30 ng (6.8 pmol), 100 ng (23 pmol), and 300 ng (68 pmol) of cortagine produced increased anxiety-like behavior and reduced locomotor activity as indicated by the time spent on the open arms (a), number of entries into the open arms (b), and total distance traveled (c) on the EPM. i.c.v. administered 100 ng (21 pmol) and 300 ng (64 pmol) of oCRF also significantly decreased the time spent on the open arms (a), number of entries into the open arms (b), and total distance traveled (c) on the EPM. Statistically significant differences: Bonferroni–Dunn test; *, P < 0.05 vs. control (aCSF injection); a, P < 0.05 vs. oCRF at respective dose.
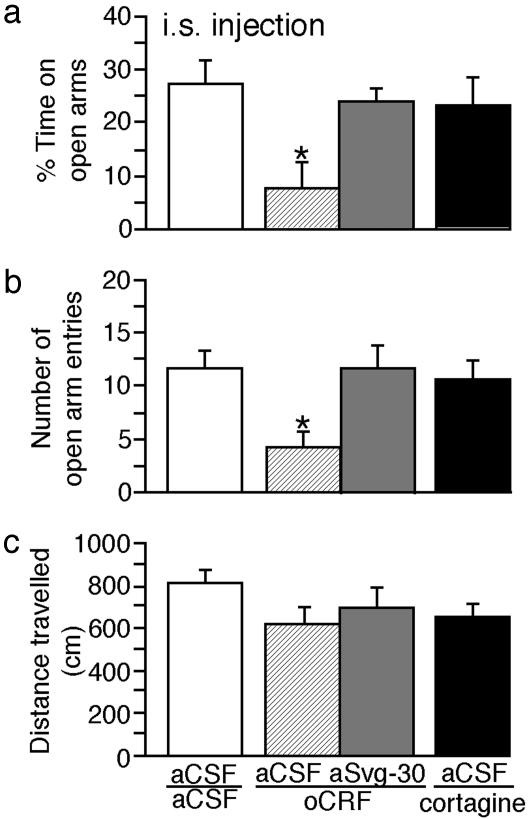
We also investigated the specificity of cortagine by monitoring the EPM behavior of C57BL/6J mice after injection of cortagine into the lateral intermediate septum, which predominantly contains CRF2 (32). Administration of 100 ng (21 pmol) of oCRF, but not of 100 ng (23 pmol) of cortagine into the lateral septum, 30 min before testing in the EPM exerted a profound anxiogenic effect as indicated by a decreased percent time spent in the open arms [F(3, 31) = 7.32, P < 0.05] (Bonferroni–Dunn test, P < 0.05 vs. aCSF) and number of open arm entries [F(3, 31) = 6.34; P < 0.05] (Bonferroni–Dunn test, P < 0.05 vs. aCSF) (Fig. 4 a and b) without affecting the locomotor activity [F(3, 31) = 1.16; P > 0.05] (Fig. 4c) in the EPM. Thus, the differences between the intrinsic in vitro activities of cortagine and oCRF to activate CRF2 (Table 2) were confirmed by the behavioral observations. When 400 ng (110 pmol) of the CRF2-selective antagonist aSvg-30 was injected intraseptally 15 min before the application of 100 ng of oCRF, the anxiogenic action of oCRF in the EPM test was completely prevented. In view of the specificity of aSvg-30 selectively blocking CRF2 (14), it was concluded that the anxiogenic action of oCRF was mediated by septal CRF2.
Fig. 4.
Absence of significant interaction of cortagine with CRF2 of the mouse brain. Cortagine (100 ng, 23 pmol) or oCRF (100 ng, 21 pmol) were applied intraseptally 30 min before EPM. aCSF or aSvg-30 (400 ng, 110 pmol) were administered 45 min before EPM. Time spent on the open arms (a), number of open arm entries (b), and distance traveled (c) during the test are depicted. Statistically significant differences: Bonferroni–Dunn test; *, P < 0.05 vs. control (aCSF/aCSF).
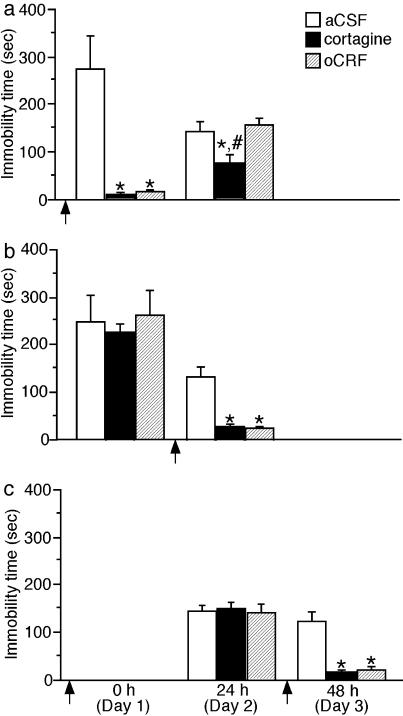
Modulation of the Immobility in the FST. Previous studies have demonstrated that antagonism of CRF1 decreases the immobility time in the FST, a rodent model of depression-like behavior (33, 34). To examine the effect of selective activation of CRF1 on the immobility time, C57BL/6J mice were injected with cortagine and tested in the FST. One group of mice was injected i.c.v. with 300 ng (68 pmol) of cortagine or 300 ng (64 pmol) of oCRF 30 min before the preswim session (day 1) and examined in the test swim session 24 h later (day 2). The second group of mice was exposed to the preswim session without injection (day 1). However, 300 ng (68 pmol) of cortagine or 300 ng (64 pmol) of oCRF was administered 30 min before the test swim session 24 h later (day 2). Interestingly, a two-way ANOVA with treatment and order (prepreswim vs. pretest swim injection) as between-subject factors revealed significant treatment and order main effects and treatment × order interaction for immobility time during the preswim session [F(2, 41) = 10.24, P < 0.05 treatment; F(1, 41) = 19.52, P < 0.05 order; and F(2, 41) = 5.63, P < 0.05 treatment × order] and test swim session [F(2, 41) = 19.93, P < 0.05 treatment; F(1, 41) = 34.07, P < 0.05 order; and F(1, 41) = 10.65, P < 0.05 treatment × order] in the FST. Bonferroni–Dunn post hoc analysis showed that prepreswim or pretest swim treatment with cortagine or oCRF significantly decreased the immobility time during the subsequent swim sessions in comparison with the aCSF treatment (P < 0.05 vs. aCSF) (Fig. 5 a and b). Similarly, prepreswim injection of the two peptides significantly decreased the immobility time during the preswim session (P < 0.05 vs. test swim session), whereas the pretest swim injection exerted a similar effect during the test swim session (P < 0.05 vs. preswim session) (Fig. 5 a and b). Analysis of simple main effects of treatment revealed that injection of cortagine but not oCRF before the preswim session resulted in a significantly reduced immobility time during the test swim session 24 h later [F(2, 22) = 5.94, P < 0.05] (Bonferroni–Dunn test, P < 0.05 vs. oCRF-injected group) (Fig. 5b). No such difference was observed between cortagine and oCRF-pretreated mice during the preswim session [F(2, 22) = 9.65, P < 0.05] (Bonferroni–Dunn test, P > 0.05 cortagine- vs. oCRF-injected group) (Fig. 5a).
Fig. 5.
Immobility time after cortagine application in the FST. (a) Cortagine (300 ng, 68 pmol) or oCRF (300 ng, 64 pmol) was administered i.c.v. 30 min before the 15-min preswim on day 1. The test swim was performed 24 h later (day 2). (b) Mice subjected to the preswim on day 1 without injection were injected on day 2 with the two peptides (doses as in a) and subjected to the 15 min test swim 30 min later. (c) After injection of the two peptides (doses as above), the mice were subjected to the test swim 24 h later (day 2). On day 3, the two peptides were injected 30 min before a retest swim. Injections are indicated by arrows. Statistically significant differences: Bonferroni–Dunn test; *, P < 0.05 vs. control (aCSF); #, P < 0.05 vs. oCRF-injected group.
It had to be considered that the different effects of cortagine and oCRF could be explained by an increased half-life time of cortagine. This possibility was tested by i.c.v. injecting 300 ng (68 pmol) of cortagine and 300 ng (64 pmol) of oCRF, respectively (day 1), 24 h before the test swim session (day 2) (Fig. 5c). As an additional control, the same mice were injected i.c.v. 24 h later with 300 ng of cortagine or oCRF and subjected to a 6-min retest swim 30 min after injection (Fig. 5c). A two-way ANOVA with treatment as between-subject factor and time (day 2 vs. day 3) as within-subject factor revealed significant treatment [F(2, 21) = 7.98, P < 0.05] and time [F(1, 21) = 41.51, P < 0.05] main effects, and treatment × time interaction [F(2, 21) = 92.24; P < 0.05]. The significant interaction was produced by the fact that the groups did not differ on day 2 [F(2, 21) = 0.98, P > 0.05], but differences appeared on day 3 [F(2, 21) = 25.08, P < 0.05] (Bonferroni–Dunn test, P < 0.05 vs. aCSF). These results excluded the possibility that the prolonged action of cortagine was responsible for its differential effects on immobility time in FST.
Discussion
By combining sequences from Svg, h/rCRF, and oCRF, cortagine was developed (Fig. 1). Cortagine's specificity and potency were initially established by its selective and high affinity to CRF1 of transfected HEK-293 cells and its potency to release cAMP from these cells. Cortagine's selective binding to native CRF1 of brain sections of the mouse was demonstrated in autoradiographic experiments with CRF1-deficient mice and their WT littermates (Fig. 2).
Because cortagine did not exhibit high affinity binding to CRFBP, it was excluded that the effective dose of cortagine was decreased by binding to CRFBP and diluted by endogenous CRF-like peptide released from CRFBP.
It has to be considered that rat CRF1 and mouse CRF2β produced by transfected cells and not mouse CRF1 and CRF2α, the predominant splice variant of the rodent brain (9), were used for the pharmacological characterization of cortagine. However, the high affinity of cortagine for mouse CRF1 was demonstrated by its potency to enhance anxiety-like behavior after injection i.c.v. (Fig. 3). It has been earlier established that CRF1 activated by oCRF or h/rCRF injected i.c.v. mediates the enhancement of anxiety-like behaviors (31). The selectivity of cortagine was confirmed when it was injected into the lateral intermediate septum, which contains predominantly CRF2α (32) (Fig. 4). At a dose of 21 pmol, oCRF enhanced anxiety-like behavior, whereas cortagine did not. The data on binding and biopotency, as well as on the modulation of anxiety-like behavior, are in agreement with earlier pharmacological analyses indicating that the splice variants of CRF2 do not differ significantly in their pharmacological profile (5, 19).
The enhancement of anxiety-like behavior by activation of CRF1 with cortagine and oCRF was accompanied by a large reduction in locomotor activity. The involvement of CRF1 in locomotor activity has also been demonstrated with CRF1-deficient mice, which exhibit hyperlocomotion in the open field (12). However, the differential anxiogenic effects of cortagine and oCRF after intraseptal and intraventricular injections did not correlate with locomotion differences (Figs. 3 and 4). Therefore, we assumed that the locomotor effect represented an independent behavior variable. Such an assumption is consistent with factor analyses of mouse behavior in the EPM test, where indices of anxiety and locomotor activity were loaded on separate factors (35).
Potential effects of cortagine and oCRF on depression-like behaviors were investigated by using the FST, a common animal model of depression, using the immobility time as measure of depression-like behavior (36) (Fig. 5). Surprisingly, we found that both cortagine and oCRF significantly decreased the immobility time when applied immediately before the preswim or the test swim session. Moreover, administration of cortagine, but not oCRF, before the preswim session resulted in a decrease of the immobility time during the test swim session 24 h later. Opposite effects were expected on the basis of the reported findings that antagonism to CRF1 decreases depression-like behavior in rodents as determined by FST (33, 34), as well as in humans (37). It is suggested that the cortagine-induced CRF1 activation decreased the depression-like behavior independently of its possible effects on general activity. Thus, the data presented here confirm the involvement of CRF1 in anxiety- and depression-like behaviors. However, the surprising cortagine effect combining anxiogenic and antidepressive potencies indicates that CRF1-involving processes of anxiety and depression formation are not necessarily positively correlated.
Acknowledgments
Thomas Zeyda and Milos Zarkovic are gratefully acknowledged for helpful discussions. We thank Yu-Wen Li (Bristol-Myers Squibb) for helping to set up autoradiography and Lars van Werven, Cathrin Hippel, Thomas Liepold, and Bodo Zimmermann for expert technical help.
Abbreviations: aSvg-30, antisauvagine-30; CRF, corticotropin-releasing factor; CRF1, CRF receptor subtype 1; CRF2, CRF receptor subtype 2; CRFBP, CRF-binding protein; EPM, elevated plus-maze; FST, forced swim test; h/rCRF, human/rat CRF; i.c.v., intracerebroventricularly; mCRF2β, mouse CRF2β; oCRF, ovine CRF; rCRF1, rat CRF1; rCRFBP, rat CRFBP; Svg, sauvagine; Ucn, urocortin.
References
- 1.Spiess, J., Rivier, J., Rivier, C. & Vale, W. W. (1981) Proc. Natl. Acad. Sci. USA 78, 6517-6521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vale, W. W., Spiess, J., Rivier, C. & Rivier, J. (1981) Science 213, 1394-1397. [DOI] [PubMed] [Google Scholar]
- 3.Eckart, K., Jahn, O., Radulovic, J., Radulovic, M., Blank, T., Stiedl, O., Brauns, O., Tezval, H., Zeyda, T. & Spiess, J. (2002) Recept. Channels 8, 163-177. [PubMed] [Google Scholar]
- 4.Reul, J. M. & Holsboer, F. (2002) Curr. Opin. Pharmacol. 2, 23-33. [DOI] [PubMed] [Google Scholar]
- 5.Perrin, M. H. & Vale, W. W. (1999) Ann. N.Y. Acad. Sci. 885, 312-328. [DOI] [PubMed] [Google Scholar]
- 6.Behan, D. P., Heinrichs, S. C., Troncoso, J. C., Liu, X. J., Kawas, C. H., Ling, N. & De Souza, E. B. (1995) Nature 378, 284-287. [DOI] [PubMed] [Google Scholar]
- 7.Karolyi, I. J., Burrows, H. L., Ramesh, T. M., Nakajima, M., Lesh, J. S., Seong, E., Camper, S. A. & Seasholtz, A. F. (1999) Proc. Natl. Acad. Sci. USA 96, 11595-11600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hillhouse, E. W., Randeva, H., Ladds, G. & Grammatopoulos, D. (2002) Biochem. Soc. Trans. 30, 428-432. [DOI] [PubMed] [Google Scholar]
- 9.Lovenberg, T. W., Chalmers, D. T., Liu, C. & De Souza, E. B. (1995) Endocrinology 136, 4139-4142. [DOI] [PubMed] [Google Scholar]
- 10.Bale, T. L., Contarino, A., Smith, G. W., Chan, R., Gold, L. H., Sawchenko, P. E., Koob, G. F., Vale, W. W. & Lee, K. F. (2000) Nat. Genet. 24, 410-414. [DOI] [PubMed] [Google Scholar]
- 11.Smith, G. W., Aubry, J. M., Dellu, F., Contarino, A., Bilezikjian, L. M., Gold, L. H., Chen, R., Marchuk, Y., Hauser, C., Bentley, C. A., et al. (1998) Neuron 20, 1093-1102. [DOI] [PubMed] [Google Scholar]
- 12.Timpl, P., Spanagel, R., Sillaber, I., Kresse, A., Reul, J., Stalla, G. K., Blanquet, V., Steckler, T., Holsboer, F. & Wurst, W. (1998) Nat. Genet. 19, 162-166. [DOI] [PubMed] [Google Scholar]
- 13.Kishimoto, T., Radulovic, J., Radulovic, M., Lin, C. R., Schrick, C., Hooshmand, F., Hermanson, O., Rosenfeld, M. G. & Spiess, J. (2000) Nat. Genet. 24, 415-419. [DOI] [PubMed] [Google Scholar]
- 14.Radulovic, J., Rühmann, A., Liepold, T. & Spiess, J. (1999) J. Neurosci. 19, 5016-5025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Koob, G. F. (1999) Biol. Psychiatry 46, 1167-1180. [DOI] [PubMed] [Google Scholar]
- 16.Vaughan, J., Donaldson, C., Bittencourt, J., Perrin, M. H., Lewis, K., Sutton, S., Chan, R., Turnbull, A. V., Lovejoy, D., Rivier, C., et al. (1995) Nature 378, 287-292. [DOI] [PubMed] [Google Scholar]
- 17.Reyes, T. M., Lewis, K., Perrin, M. H., Kunitake, K. S., Vaughan, J., Arias, C. A., Hogenesch, J. B., Gulyas, J., Rivier, J., Vale, W. W. & Sawchenko, P. E. (2001) Proc. Natl. Acad. Sci. USA 98, 2843-2848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hsu, S. Y. & Hsueh, A. J. W. (2001) Nat. Med. 7, 605-611. [DOI] [PubMed] [Google Scholar]
- 19.Lewis, K., Li, C., Perrin, M. H., Blount, A., Kunitake, K., Donaldson, C., Vaughan, J., Reyes, T. M., Gulyas, J., Fischer, W., et al. (2001) Proc. Natl. Acad. Sci. USA 98, 7570-7575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Behan, D. P., Grigoriadis, D. E., Lovenberg, T., Chalmers, D., Heinrichs, S., Liaw, C. & De Souza, E. B. (1996) Mol. Psychiatry 1, 265-277. [PubMed] [Google Scholar]
- 21.Eckart, K., Jahn, O., Radulovic, J., Tezval, H., van Werven, L. & Spiess, J. (2001) Proc. Natl. Acad. Sci. USA 98, 11142-11147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rühmann, A., Bonk, I., Lin, C. J. R., Rosenfeld, M. G. & Spiess, J. (1998) Proc. Natl. Acad. Sci. USA 95, 15264-15269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jahn, O., Eckart, K., Sydow, S., Hofmann, B. A. & Spiess, J. (2001) Peptides (Tarrytown, NY) 22, 47-56. [DOI] [PubMed] [Google Scholar]
- 24.Hofmann, B. A., Sydow, S., Jahn, O., van Werven, L., Liepold, T., Eckart, K. & Spiess, J. (2001) Protein Sci. 10, 2050-2062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sydow, S., Radulovic, J., Dautzenberg, F. M. & Spiess, J. (1997) Mol. Brain Res. 52, 182-193. [DOI] [PubMed] [Google Scholar]
- 26.Radulovic, J., Kammermeier, J. & Spiess, J. (1998) Behav. Brain Res. 95, 179-189. [DOI] [PubMed] [Google Scholar]
- 27.Montecucchi, P. & Henschen, A. (1981) Int. J. Pept. Protein Res. 18, 113-120. [DOI] [PubMed] [Google Scholar]
- 28.Beyermann, M., Rothemund, S., Heinrich, N., Fechner, K., Furkert, J., Dathe, M., Winter, R., Krause, E. & Bienert, M. (2000) J. Biol. Chem. 275, 5702-5709. [DOI] [PubMed] [Google Scholar]
- 29.Saido, T. C., Iwatsubo, T., Mann, D. M. A., Shimada, H., Ihara, Y. & Kawashima, S. (1995) Neuron 14, 457-466. [DOI] [PubMed] [Google Scholar]
- 30.Brauns, O., Brauns, S., Zimmermann, B., Jahn, O. & Spiess, J. (2002) Peptides (Tarrytown, NY) 23, 881-888. [DOI] [PubMed] [Google Scholar]
- 31.Dunn, A. J. & Berridge, C. W. (1990) Brain Res. Rev. 15, 71-100. [DOI] [PubMed] [Google Scholar]
- 32.Chalmers, D. T., Lovenberg, T. W. & De Souza, E. B. (1995) J. Neurosci. 15, 6340-6350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Griebel, G., Simiand, J., Steinberg, R., Jung, M., Gully, D., Roger, P., Geslin, M., Scatton, B., Maffrand, J. P. & Soubrie, P. (2002) J. Pharmacol. Exp. Ther. 301, 333-345. [DOI] [PubMed] [Google Scholar]
- 34.Bale, T. L. & Vale, W. W. (2003) J. Neurosci. 23, 5295-5301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lister, R. G. (1987) Psychopharmacology (Berlin) 92, 180-185. [DOI] [PubMed] [Google Scholar]
- 36.Porsolt, R. D., Le Pichon, M. & Jalfre, M. (1977) Nature 266, 730-732. [DOI] [PubMed] [Google Scholar]
- 37.Zobel, A. W., Nickel, T., Kunzel, H. E., Ackl, N., Sonntag, A., Ising, M. & Holsboer, F. (2000) J. Psychiatr. Res. 34, 171-181. [DOI] [PubMed] [Google Scholar]