Abstract
The objective of the study was to design a virtual reality (VR) training to induce perturbation in older adults similar to a slip and examine the effect of the training on kinematic and muscular responses in older adults. Twenty-four older adults were involved in a laboratory study and randomly assigned to two groups (virtual reality training and control). Both groups went through three sessions including baseline slip, training, and transfer of training on slippery surface. The training group experienced twelve simulated slips using a visual perturbation induced by tilting a virtual reality scene while walking on the treadmill and the control group completed normal walking during the training session. Kinematic, kinetic, and EMG data were collected during all the sessions. Results demonstrated the proactive adjustments such as increased trunk flexion at heel contact after training. Reactive adjustments included reduced time to peak activations of knee flexors, reduced knee coactivation, reduced time to trunk flexion, and reduced trunk angular velocity after training. In conclusion, the study findings indicate that the VR training was able to generate a perturbation in older adults that evoked recovery reactions and such motor skill can be transferred to the actual slip trials.
Index Terms: Falls, Elderly, Electromyography, Fall Prevention Training, Virtual Reality
I. Introduction
FALL accidents are one of the most serious problems leading to unintentional injuries and fatalities. Slip-induced falls are responsible for 87% of all hip fractures, leading to a loss of functional independence and increase in fear for future falls in adults aged 65 years and older [1]. Current proactive intervention strategies for older adults (i.e., strength, endurance, balance training) have produced inconsistent results on the success of these exercise programs [2]. One of the reasons for such inconsistency in the effectiveness of the existing fall prevention exercises could be that they do not target the specific neuromuscular skills required for fall prevention.
There is an increasing application of virtual reality (VR) environments to investigate various aspects of human balance and control [3, 4]. VR is an excellent approach to generate simulated, interactive, and multi-dimensional environments on a Head Mounted Display (HMD) or on a computer monitor. One of the primary benefits of adopting VR is that individuals can be challenged in a safe environment, while keeping control over stimulus delivery and measurement [5]. Balance rehabilitation using VR follows the principle of ego-motion which states that varying VR environments induces a visual-vestibular sensory conflict, thus perturbing the natural stance requiring reactive responses taken to maintain stability [6].
VR training has been applied to the rehabilitation of various motor functions in patients with vestibular disorders [7], to improve mobility in individuals with impaired spatial abilities and, to train balance control [8]. Recently, VR environments have been used to promote gait training. Fung et al. [9] used a treadmill and motion coupled VR system for gait training in older adults with movement disorders. With repeated practice, participants were able to improve gait speed and were able to avoid obstacle collision. Similarly, Nyberg et al. [4] demonstrated changes in walking speed and stride length, and balance reactions in individuals when exposed to an immersive VR environment.
Recently, VR environments were used to investigate the risk of falling associated with aging [10]. It was found that visual motion induced greater joint angle displacements in the joints of the lower limb in the older adults compared to younger counterparts. These results indicate a strong influence of visual feedback in older adults to maintain balance [10]. In general, older adults tend to rely more on visual feedback for postural control and recovering from a slip-induced fall [11, 12]. Similarly, Bugnariu et al. [13] observed that when the virtual environment was manipulated to provide distorted visual perception, older adults took more steps to maintain upright stance and had delayed onset of muscle activity. This may be due to the impairments of sensory organization in older adults [13, 14]. Additionally, older adults initiated balance reactions by activating their neck muscles first, suggesting an excessive reliance on visual inputs or need for head stabilization.
Currently, no studies are available that aims to improve recovery reactions in older adults using VR training. Based on previous findings, if a VR environment is created to induce repeated virtual slips via visual-vestibular conflict, individuals may elicit recovery responses similar to an actual slip. Therefore, there is a need to develop a VR training program targeting slip-induced falls, and to evaluate whether the training results can be transferred to an actual slip. There is also a gap in knowledge regarding the neuromuscular mechanism to recover from such VR perturbations.
The objective of the study was to design a virtual reality training to induce perturbation in older adults similar to a slip and examine the training effect on kinematic and muscular responses in older adults. The specific aims for the study were: 1) To evaluate the effect of virtual reality training in improving angular and muscular responses in older adults when exposed to an actual slippery surface, and 2) To quantify the angular and muscular changes during the VR training.
II. Methods
A. Subjects
A laboratory study was conducted involving 24 healthy older adults (>65 years, 12 male, and 12 female). Their demographics are summarized in Table 1.
Table 1. Participants’ Demographics (mean/SD).
| Group | ||
|---|---|---|
| Control | Training | |
| Age (yrs) | 74.2/5.8 | 70.5/6.6 |
| Body Mass (kg) | 69.6/9.5 | 67.8/8.0 |
| Stature (cm) | 169.4/9.2 | 167.1/11.5 |
Informed consent was approved by local Institutional Review Board (IRB) and was obtained from the participants. Participants were randomly placed into a control group (n = 12), and a VR training (VRT) group (n = 12).
B. Apparatus
An instrumented treadmill (Nordick, T7 si, NY, USA) was utilized to conduct the virtual reality training. As illustrated in Figure 1, the virtual reality scene was rendered on a head mounted display (HMD, Glasstron LDI-100B Sony, with a 28° horizontal field of view in each eye). The HMD had two 0.7-inch liquid crystal display screens whose images combine to give the effect of viewing a 30-inch screen 1.2 m away. The HMD was lightweight (120mg) and had a resolution of 832(H) × 624(V). Any peripheral vision of the external environment was blocked by the foam blinders attached to the HMD. A typical downtown VR scene was generated (Figure 1) with buildings, light poles, road, pavement, street signs, etc. The scene was shown at a frame rate of 64 Hz. The HMD was equipped with a tracker (Fastrak, Polhemus, VT, USA), which allowed participants to rotate their head and feel the virtual environment in all directions (6 dof-X, Y, Z, pitch, yaw, and roll). The virtual slip was created by perturbations (tilts) in the pitch plane of the VR scene at random intervals. The lights in the laboratory were turned off during the training trials.
Figure 1.
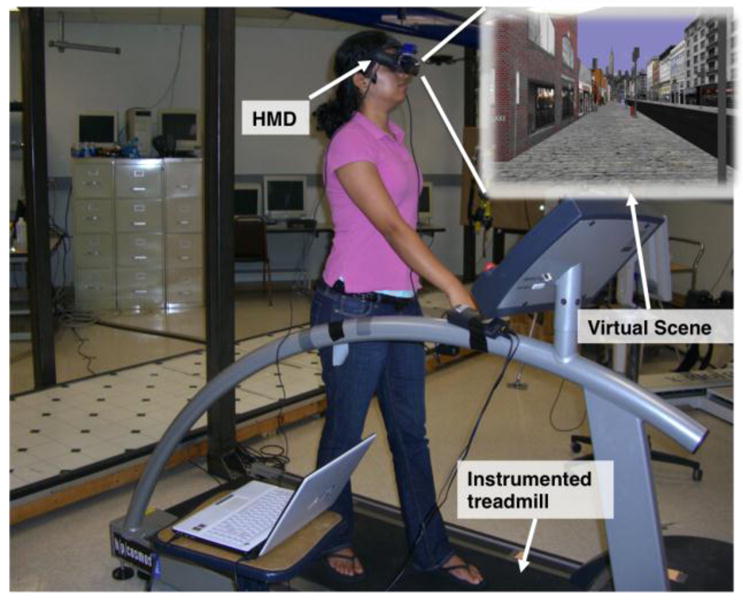
Experimental set-up of the virtual reality training including the instrumented treadmill and the head mounted display (HMD) along with the virtual scene.
The slip trials were conducted on 15 m long walkway embedded with two force plates (Type 45550-08, Bertec). The slippery surface was covered with a 1:1 water and jelly mixture to reduce the coefficient of friction (COF) (dynamic COF = 0.12) of the floor surface. Participants were unaware of the position of this surface as the force plates were covered with the same vinyl as the walkway. This is a standardized protocol used in several previous slip and fall studies [11, 15].
A six-camera optical motion capture system (Qualisys, Sweden) was used to measure full-body kinematics at a sampling rate of 100 Hz. A full-body biomechanical model [16] with 24 reflective markers was adopted in the study. Kinetic data were measured at 1000 Hz by the force plates (embedded on the walkway). An eight-channel EMG telemetry Myosystem 2000 (Noraxon, USA), was used to record bilateral temporal activations from vastus lateralis (VL), medial hamstring (MH), tibialis anterior (TA), and medial gastrocnemius (MG) muscles of the lower extremity. The EMG data were sampled at 1000Hz. The force plates and EMG system were connected to a 16 bit, 64 analog-input, DAQ card (PCI-6031E, 100kS/s, NI, USA). The data collection from the Qualysis, force plates, and EMG system was synchronized using a customized LabVIEW program. Participants were protected by an overhead fall-arresting harness throughout the experiment [16]. Uniform clothes and athletic shoes were provided to all participants.
C. Procedure
The entire study involved three sessions: baseline measure, training acquisition, and transfer of training, on three separate days. All participants went through a slip trial (Slip1) on the slippery floor surface in the first session. On a separate day (about two weeks later), the VRT group went though the virtual reality training on the treadmill while the control group performed normal walking on the walkway. In the third session, both groups went through another slip trial (Slip2).
Baseline Measure (Session 1)
After attaching the markers and the EMG electrodes, participants were asked to walk on the walkway for approximately10 minutes at a self-selected pace to familiarize them with the harness and the lab environment. A metronome was used to record and regulate participants’ self-selected pace to ensure consistent walking speed between sessions. The starting point of their walking was adjusted so that their right foot lands on the second force plate, which was switched to a slippery surface later. The baseline data were measured from five normal walking trials before inducing the slip. Participants were instructed to maintain their balance and continue walking even if they experience a slip. Subsequently, an actual slippery surface was introduced without participants’ awareness and the data were collected to represent Slip1.
Training Acquisition (Session 2)
The control group underwent normal walking for 10–15 min during their second session. Data was collected from three normal walking trials during the experiment. The training group went through the virtual reality training in their second session (Figure 2). Following the training, participants walked on the treadmill at a self-selected pace for 5 minutes with harness. The initial baseline gait data (kinematic and EMG) on the treadmill was collected to represent treadmill walking without VR (TW). Afterwards, they were asked to wear the HMD with the virtual scene shown. The HMD was adjusted in a way that the participants were able to look straight ahead. After a comfortable HMD fit was achieved, the visual scene started moving and the treadmill speed was programed to match the visual scene (keeping both at the comfortable pace of participants). Participants were asked to walk for 15 minutes with the HMD and were allowed to freely rotate their head to feel the virtual environment, allowing for habituation of the VR scene. During this period, data were collected at 5, 10, and 15 min to represent walking on the treadmill with VR (VR1, VR2, and VR3). Following the habituation, participants were informed that a slip may or may not be induced. They were instructed that in case of a slip, they should try to recover their balance and keep walking. A sudden virtual slip was induced by tilting the VR environment from 0° to 25° in the pitch plane at a speed of 60°/s. The experimenter manually induced the virtual slip by pressing a computer key at random intervals during the heel contacts of the right foot. The choice of the perturbation velocity and the displacement of the VR scene were based on a pilot study [17] to evaluate the speed and tilt at which older adults may experience perturbation.
Figure 2. Illustration of training session for VRT group (TW1-2: walking without VR; VR1-5: walking with VR; T1-T12: VR slip).
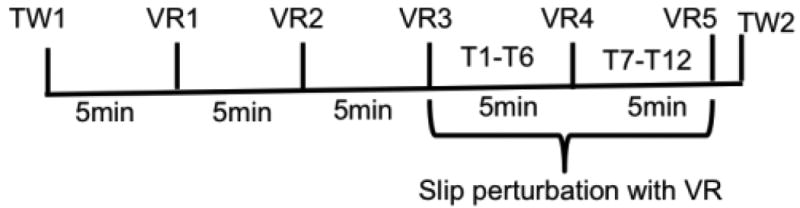
The training paradigm was designed to include principles known to enhance motor learning such as variability and randomization [18, 19], progressive overload [20], and individualization [21]. The training session consisted of 24 trials, with two blocks of slips and no slips, followed by random variations of slips and no slips. After the first block of 3 repeated slips (T1–T3), the speed of the virtual scene tilt was adjusted. Depending on whether the participants successfully recovered from the perturbation, the tilt speed was increased or decreased by 12°/s (20% of the initial velocity) for the next block of slip trials (T4–T6). It was believed that the decrease in velocity would provide a better opportunity for successful recovery if failed recoveries were observed, whereas the increase in speed would provide greater challenge after successful recovery. Such adjustment has shown to improve motor learning [2, 22]. The last 12 trials included a random combination of 6 slip trials (T7–T12) and various no slip trials.
Kinematics and EMG data were measured during all the slip trials to represent T1–T12. Data were also recorded after block 1 and block 2 to represent normal walking with VR on the treadmill (VR4 and VR5). In addition, data were recorded at the end of the training session without the HMD to represent treadmill walking without VR (TW2).
Transfer of Training (Session 3)
Session 3 was performed on the following day after the second session to avoid any confounding effects due to cyber sickness. For each subject, efforts have been made to schedule session 2 and 3 around the same time period of the day to ensure consistent duration between training acquisition and transfer of training. The transfer of training was evaluated on an actual slippery surface similar to the baseline measure. Briefly, participants were asked to walk on the walkway at a pace that was matched with their pace during the first session using a metronome. The kinematic, kinetic, and EMG data were measured prior to inducing the slip, representing the normal walking trials. Following the normal walking trials, a slippery floor surface was introduced without participants’ awareness (Slip2).
D. Data Reduction
The kinematic and kinetic data were low-pass filtered using a fourth order, zero lag, Butterworth filter at a cut off frequency of 7 Hz [16]. The EMG data were digitally band pass filtered at 10–450 Hz [23], following which they were rectified and low-pass filtered using a fourth order, zero lag, Butterworth filter with a 7 Hz cut off frequency to create a linear envelope [23]. Ground reaction forces were used to identify heel contact (HC) and toe-off (TO) for Slip1 and Slip2. For the training trials on the treadmill, HC and TO were identified using heel kinematics. Subsequent analyses were performed in the stance phase of the slipping foot.
Gait changes in VR environment
To quantify gait changes while walking on the treadmill with VR, angular kinematics (ankle, knee, hip, and trunk) and muscles activations (MG, TA, MH, VL) was assessed from the data that were collected at different time intervals (5, 10, 15, 20, 25 min). The lower extremity 2D sagittal angles were calculated using the marker data [15]. Trunk angle was defined as the angle between the trunk segment (mid point between shoulder and mid point between ASIS) and vertical. Muscle activity onsets of the slipping limb were determined using a threshold of two standard deviations above activity during a quiet period of gait cycle. Ten gait cycles from the normal treadmill walking were used to create a normal ensemble average profile due to the variability in gait during locomotion [24]. Each EMG channel was peak normalized within subject using the ensemble average [25]. The presence of muscle response burst is defined as increase in muscle activity that exceeded or fell below ± 2 SD (either excitatory or inhibitory) for >30 ms [26].
Proactive and reactive changes due to training
To quantify the effects of training, dependent variables were categorized as proactive responses that occur at the heel contact before the slip is initiated, and reactive responses that occur after the slip is initiated in the stance phase (HC to TO). As a descriptive measure, the frequency of falling was defined as the percentage of the number of falls over the total number of falls and successful recoveries for each group.
Reactive responses
The onset activation and the time to peak activation of muscles of the slipping limb (MG, TA, MH, and VL) were used for statistical analyses. The onset activity was determined as described before using a threshold of two standard deviations above activity during a quiet period of gait cycle. Ten control normal walking trials prior to the first slip were used to create the normal ensemble average profile [23]. Peak ankle and knee coactivity, and time to peak ankle and knee coactivity after the slip is initiated were used to quantify effects of training. The power of the EMG activity was determined from the integrated EMG (iEMG), calculated by taking the integral from onset to offset, and normalized to the duration of the activation. Coactivity Index (CI) was calculated based on the ratio of the EMG activity of the antagonist/agonist muscle pairs (TA/MG and VL/MH) using the equation (1) proposed by Rudolph et al. [27]. LowerEMG refers to the less active muscle, and HigherEMG refers to the more active muscle (to avoid division by zero errors). The ratio was multiplied by the sum of activity found in the two muscles. This method provided an estimate of relative activation of the pairs of muscles as well as the magnitude of coactivity.
| (1) |
Peak angles, angular velocity, time to peak angle, and time to peak angular velocities of the slipping limb were calculated to quantify the effect of training on angular kinematics. The lower extremity 2D joint angles and angular velocities were calculated using methods described previously [15].
Proactive Responses
Ankle, knee, hip and trunk angles were calculated at the heel contact to quantify changes in angular kinematics before the slip was initiated. The muscle (MG, TA, MH and VL) onsets of the slipping limb along with ankle and knee coactivity at the heel contact were used to quantify any proactive muscular adjustments.
E. Statistical Analysis
There were two independent variables: group (training vs. control), and training (Pre vs. Post). To investigate the effect of virtual reality training on recovery performance, difference values were calculated between the two slips (Slip2 – Slip1), and a one-way multivariate analysis of variance (MANOVA) was conducted between the two groups including all the dependent measures. If a statistically significant main effect of training was found, subsequent univariate analysis of variance (ANOVA) was conducted to elucidate the effect of training on the dependent measures. All statistical analyses were performed using SPSS 11.5.0 (Chicago, IL) with a significance level of p < 0.05. In order to verify the assumptions of MANOVA and ANOVA, all of the data were evaluated for normality (using Shapiro-Wilk W test), and sphericity (using Bartlett's sphericity test). No significant violation of the assumptions was evident.
III. Results
The frequency of falling for the VRT group was reduced from 50% upon the first unexpected slip (Slip1) during the baseline session to 0% upon the second unexpected slip (Slip2) during the transfer of training session. For the control group, the frequency of falling was reduced from 50% in Slip1 to 25% in Slip2.
Gait changes in virtual reality environment
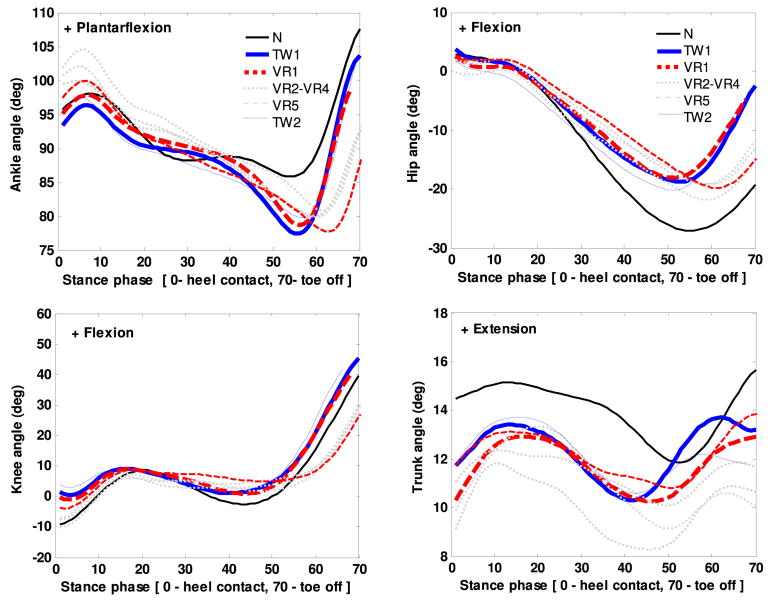
General trends of angles during overground walking and treadmill walking with and without VR are presented in Figure 3. The figure indicates that participants walked with an increased ankle plantarflexion, increased knee flexion and trunk flexion at heel contact on the treadmill as compared to overground walking (Figure 3). In addition, participants further increased their ankle plantarflexion [F(6, 76) = 9.56, p = 0.02], trunk flexion [F (6, 76) = 12.56, p = 0.001], and decreased their knee flexion [F(6, 76) = 10.56, p = 0.02] at heel contact in the VR environment (Figure 3). Post-hoc results indicated no significant differences in the peak angles between the last trial of VR walking (VR5) and TW1, suggesting that angular kinematics was stabilized after VR5.
Figure 3. Ensemble averages of joint angles during normal walking (N), treadmill walking without VR (TW1-2) and with VR (VR1-5).
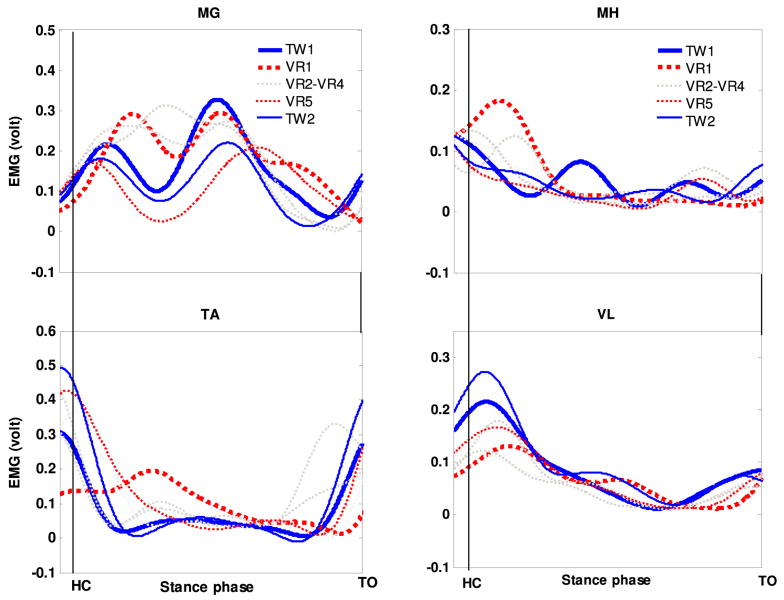
The muscle activation profiles during the stance phase on the treadmill with and without VR are presented in Figure 4. In general, participants walked with an early activation of MG, TA, MH, and VL muscles at the heel contact during VR walking compared to the treadmill walking. Significant differences were only seen in the activation of VL [F (6, 76) = 9.86, p = 0.02] and TA [F (6, 76) = 10.48, p = 0.01] muscles between VR5 and TW1. No significant differences were observed in the activation of MG and MH muscles between VR walking and treadmill walking.
Figure 4.
Ensemble average of muscle activation profile of medial gastrocnemius (MG), tibialis anterior (TA), medial hamstring (MH), and vastus lateralis (VL) during treadmill walking without virtual reality (TW1-2) and with virtual reality (VR1-5)
Reactive changes after slip onset
The ANOVA indicated no significant differences in the peak ankle angle between groups. There was a decrease in the peak knee flexion and peak hip flexion angle in the VRT group compared to control, but the differences were not significant (Table 2). The peak ankle, knee, and hip angular velocity after slip-start decreased from Slip1 to Slip2 trials in both VRT and control group, but no significant differences were observed between groups.
Table 2. Joint angles and angular velocity peaks during Slip1&2.
| Variable | Group | |||
|---|---|---|---|---|
|
| ||||
| Training | Control | |||
|
| ||||
| Slip1 | Slip2 | Slip1 | Slip2 | |
| Joint angles (deg) | ||||
| Ankle angle at HC (+= plantar) | 97.25 ± 5.66 | 102.52±4.67 | 95.56 ± 4.29 | 98.56 ± 5.29 |
| Knee angle at HC (+ = flex) | –2.35 ± 3.23 | –2.85 ± 2.89 | –2.46 ± 1.23 | –1.53 ± 0.98 |
| Hip angle at HC (+ = flex) | 13.78 ± 6.23 | 12.03 ± 5.29 | 16.32 ± 5.28 | 18.42 ± 6.39 |
| Trunk angle at HC (+ = ext) | 14.64 ± 4.54 | 10.34 ± 5.56 | 10.34 ± 5.76 | 9.34 ± 3.56 |
| Peak Ankle angle (+ = plantar) | 104.60±6.22 | 105.38±4.26 | 110.32±4.55 | 108.87±6.78 |
| Peak Knee angle (+ = flex) | 30.23 ± 8.45 | 23.04 ± 8.68 | 24.59 ± 5.39 | 21.24 ± 4.38 |
| Peak Hip angle (+ = flex) | 15.44 ± 6.96 | 12.61 ± 5.45 | 18.70 ± 3.47 | 16.42 ± 2.53 |
| Peak Trunk angle (+ = ext)* | 35.44±13.96 | 28.61±10.45 | 38.70±13.47 | 39.42±12.53 |
| Angular velocity (deg/s) | ||||
| Peak Ankle velocity | 89.66±12.16 | 90.66±16.47 | 102.56±22.4 | 95.78±10.45 |
| Peak Knee velocity | 250.34±35.9 | 219.34±6.4 | 255.45±32.4 | 210.29±31.6 |
| Peak Hip velocity | 160.44±22.61 | 125.45±32.55 | 150.4±8.65 | 75.45±10.53 |
| Peak Trunk velocity* | 130.32±13.21 | 100.32±23,81 | 135.32±16.2 | 145.32±23.2 |
Note:
p < 0.05.
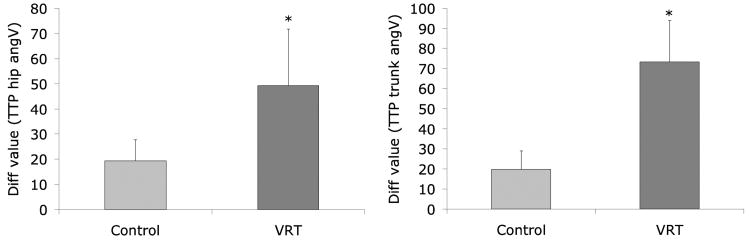
A significant training effect was found in the peak trunk extension after slip-start [F (1, 18) = 12.46, p = 0.01]. Peak trunk extension decreased more from Slip1 to Slip2 in the VRT group compared to control (Figure 5). The peak trunk angular velocity decreased more from Slip1 to Slip2 in the VRT group compared to control [F (1, 18) = 10.46, p = 0.01] (Figure 5). Further analysis revealed a significant effect of group on time to peak angular velocities. The time to peak trunk velocity [F (1, 18) = 10.46, p = 0.02] and hip angular velocity [F (1, 18) = 6.45, p = 0.03] decreased more from Slip1 to Slip2 in the VRT group than control (Figure 6).
Figure 5. Ensemble averages of trunk angle and angular velocity during Slip1 and Slip2 trials.
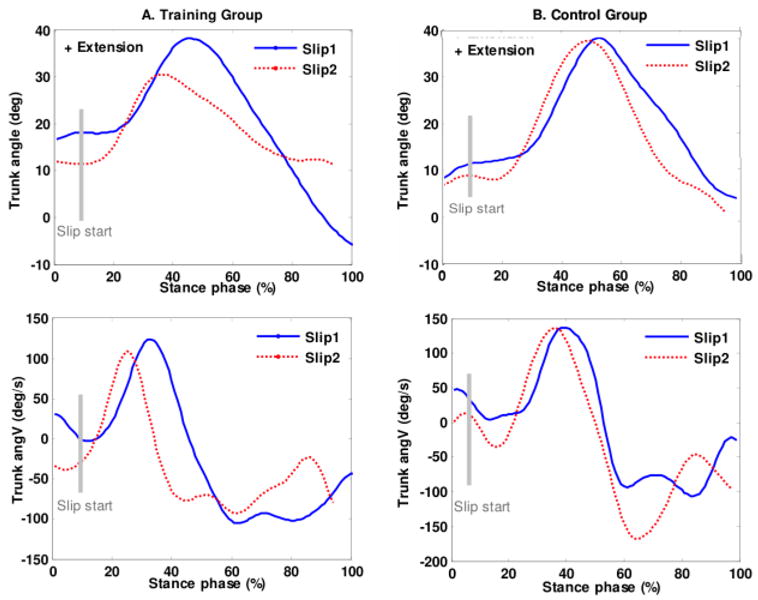
Figure 6.
Difference values (Slip2 – Slip1) of time to peak (TTP) angular velocity (hip and trunk) between control and training group (* p < 0.05).
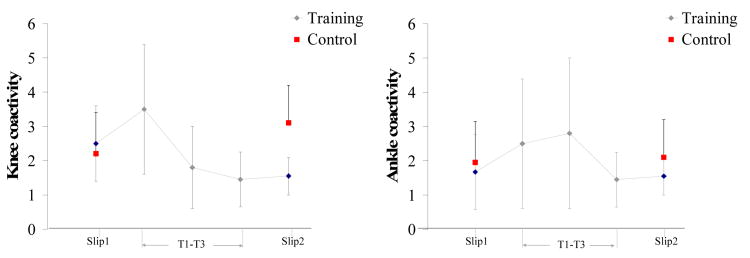
The ANOVA indicated an early onset of MH [F (1, 18) = 12.67, p = 0.01] from Slip1 to Slip2 trial in the VRT group compared control. Early onset of VL muscles was also observed in the training group during Slip2, but the differences between the groups were not significant (Table 3). Along with early onset, the time to peak activation of the MH muscle decreased more from Slip1 to Slip2 [F (1, 18) = 11.55, p = 0.02] in the VRT group compared to control. Peak knee coactivity decreased more from Slip1 to Slip2 in the VRT group compare to control [F (1, 18) = 21.34, p = 0.001]. Peak ankle coactivity increased in the VRT group from the Slip1 to Slip2 trial, but the differences were not significant compared to control. The time to peak knee coactivity decreased more in the VRT group compared to control [F (1, 18) = 9.46, p = 0.01](Table 3).
Table 3. Muscle activity onset after slip-start and the time to peak activations (recovery trials only).
| Variable | Group | |||
|---|---|---|---|---|
|
| ||||
| Training | Control | |||
|
| ||||
| Slip1 | Slip2 | Slip1 | Slip2 | |
| Muscle activation onset (ms) | ||||
| Medial gastrocnemius | 178±35.67 | 180±12.67 | 189±24.29 | 179±25.29 |
| Tibialis anterior | 187±28.26 | 180±11.69 | 188±21.23 | 178±12.98 |
| Medial hamstrings* | 159±14.76 | 138±11.37 | 168±15.28 | 156±16.39 |
| Vastus lateralis | 239±33.54 | 222±14.54 | 245±25.76 | 255±15.99 |
| Time to peak activations (ms) | ||||
| Medial gastrocnemius | 322±15.50 | 310±33.68 | 364±15.39 | 377±34.38 |
| Tibialis anterior | 325±33.96 | 315±28.45 | 378±23.47 | 362±32.53 |
| Medial hamstrings* | 280±13.96 | 210±17.45 | 290±23.47 | 278±22.53 |
| Vastus lateralis | 355±25.35 | 345±16.68 | 369±33.12 | 354±20.73 |
| Coactivations | ||||
| Peak knee coactivity | 2.55±1.19 | 1.57±0.54 | 2.23±1.39 | 2.44±1.44 |
| Peak ankle coactivity | 1.68±0.98 | 1.58±0.45 | 1.95±1.11 | 2.10±0.99 |
| Time to peak knee coactivity* | 300±33.16 | 260±17.45 | 320±44.47 | 310±29.66 |
| Time to peak ankle coactivity | 295±25.35 | 255±36.68 | 319±53.12 | 330±20.55 |
Note:
p < 0.05.
Proactive changes at heel contact before slip onset
No significant differences were observed in the ankle, knee, and hip kinematics at the heel contact before the slip onset between groups. However, participants in the VRT group had an increased trunk flexion at heel contact compared to control group [F (1, 18) = 3.46, p = 0.04] during Slip2 trial. In terms of muscle activation, no significant effect of group was found in the onset of muscles at heel contact. No significant effect was found in the ankle and knee coactivity between groups.
Proactive and reactive strategies during VR training
The proactive changes at heel contact were observed from T1-T12 trials. Participants walked with an increased trunk flexion, ankle plantarflexion (Figure 7), and knee flexion at heel contact from T1 to T2 trial, which reduced by T6 trial and remained unchanged from T6-T12 trials. In terms of muscle activity, participants had an early activation of all the muscles of the slipping limb at heel contact from T1-T2 trial, which remained unchanged until T5 trial. During the subsequent trials, early onset was only seen for VL and TA muscles.
Figure 7. Mean ± 1 SD of peak ankle and knee coactivity from T1- T3 slip training trials (training group), and from Slip1 and Slip2 trials (control and training group).
IV. Discussions
This study explored the use of a novel virtual reality perturbation method in improving motor skills specific to reactive recovery from a slip-induced fall. Overall, the study findings support the use of VR as a perturbation-based fall prevention approach for older adults.
Cautious gait behavior was observed in the angular kinematics and neuromuscular responses during the initial VR walking. Participants walked with an increased ankle plantarflexion, knee flexion and trunk flexion at the heel contact, which is similar to the findings in a previous study [28]. These kinematic changes were coupled with neuromuscular changes such as increased activation of MG and MH muscles during initial walking in the VR. After walking for about 15 min in the VR environment, the kinematic and neuromuscular activations approximated treadmill walking without VR. These results have implications in developing future VR setups for improving gait studies. The habituation time should be considered as one of the important factors while designing a VR locomotion study.
As to reducing fall frequency, the VR slip training in the current study was found to be more effective (from 50% to 0% vs. from 41% to 0%) than the conventional moveable platform training [29]. In terms of angular kinematics, significant differences were only found in the trunk kinematics between the groups. During the Slip1 trial, both training and control group extended their trunk at ∼130°/s before they were able to recover from the slip. However, during the Slip2 trial, participants in the training group extended their trunk at ∼95°/s and were able to quickly reverse their forward trunk rotations by mid-slip. Reducing trunk rotations will have a significant effect in bringing the COM of the body within stability limits [30]. Similar results were found during the VR training trials (T2–T3) where participants were able to reverse their forward trunk rotation after the visual perturbations were induced. Recovery patterns of the lower extremity joints were not evident during the VR training on treadmill. It took about 200- 300 ms for the participants to react to a virtual slip. Therefore, after the slip was induced heel contact, the heel was traveling posterior to the non-slipping foot, and because of which the recovery consisted of a quick forward stepping response of the slipping foot, to avoid falling. However, due to limited data and large variability it is difficult to describe transfer of motor strategies from the training to Slip2 trial.
Several neuromuscular adaptations were also observed in the VRT group after the training. The onset and time to peak activation of the MH muscle of the slipping limb decreased in the VRT group during Slip2 compared to the controls. Slower hamstring activation rate in older adults has been suggested as a potential risk factor for slip-induced falls [31, 32]. The initial muscular reaction to a slip consists of the activation of the hamstring muscle followed by other muscles [23]. This pattern is consistent with the kinematic response to a naturally occurring slip, i.e., primary knee flexion followed by knee extension. Early onset and the reduced time to peak MH activation therefore can help in stabilizing the knee joint during a slip. Further reactive strategies include reduced knee coactivity of the slipping limb in the training group during Slip2 trial. Similar patterns were observed during the VR training, with an initial increase in the coactivity (T2 trial) and then a subsequent decrease (T2–T3). Although implicated, a generalized pattern could not be reported due to the lack of recovery trials. In general, the integrated EMG activity of both MH and VL increased from Slip1 to Slip2 in the training group, with a higher increase in integrated activity of MH after the slip was initiated. No significant differences were seen in the ankle coactivity, suggesting a reliance on knee stability for recovery. Coactivation of agonist and antagonist muscles is important for regulation of joint stiffness [33]. It may be possible that after exposures to balance loss in the VR training, the CNS chose the most effective muscle synergy organization to achieve a common goal (i.e., recovery) with least energy expenditure during the Slip2 trial.
One of the primary contributions of this study is the application of VR environments in creating slip perturbation, which has only been suggested in the previous studies [4]. In addition, the study supported that healthy older adults were capable of walking in the VR environment with a stable gait after habituation, which is important while designing future locomotion research using virtual environments.
The study had several limitations. Participants adapted to the virtual slips within 2–3 trials, and subsequent visual tilts could not induce more perturbations. More importantly, future studies may explore the retention of the training effects over weeks or months on more diverse participant populations.
In summary, the study findings indicate that the VR training was able to generate a perturbation in older adults that evoked recovery reactions. The main effects of training were observed in reducing the reaction time to recovery such as reduced time to peak knee coactivity and reduced time to peak trunk extension.
Acknowledgments
This research was supported by the NSF (grant #CBET-0756058) and NIOSH (grant #CDC/NIOSH-R01-OH009222).
Contributor Information
Prakriti Parijat, Email: jiliu3@vt.edu, The School of Biomedical Engineering and Science, Virginia Tech, Blacksburg, VA 24060 USA.
Thurmon E. Lockhart, Email: thurmon.lockhart@asu.edu, The School of Biological and Health Systems Engineering, Arizona State University, Tempe, AZ 85287 USA.
Jian Liu, Email: liuji@marshall.edu, The Division of Applied Science and Technology, Marshall University, Huntington, WV 25755 USA.
References
- 1.Sterling DA, O’Connor JA, Bonadies J. Geriatric falls: injury severity is high and disproportionate to mechanism. J Trauma. 2001 Jan;50:116–9. doi: 10.1097/00005373-200101000-00021. [DOI] [PubMed] [Google Scholar]
- 2.Mansfield A, Peters AL, Liu BA, Maki BE. A perturbation-based balance training program for older adults: Study protocol for a randomised controlled trial. BMC Geriatr. 2007;7:12. doi: 10.1186/1471-2318-7-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hollman JH, Brey RH, Robb RA, Bang TJ, Kaufman KR. Spatiotemporal gait deviations in a virtual reality environment. Gait Posture. 2006 Jun;23:441–4. doi: 10.1016/j.gaitpost.2005.05.005. [DOI] [PubMed] [Google Scholar]
- 4.Nyberg L, Lundin-Olsson L, Sondell B, Backman A, Holmlund R, Eriksson S, et al. Using a virtual reality system to study balance and walking in a virtual outdoor environment: a pilot study. Cyberpsychol Behav. 2006 Aug;9:388–95. doi: 10.1089/cpb.2006.9.388. [DOI] [PubMed] [Google Scholar]
- 5.Sveistrup H. Motor rehabilitation using virtual reality. Journal of NeuroEngineering and Rehabilitation. 2004;1:10. doi: 10.1186/1743-0003-1-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jeka J, Oie KS, Kiemel T. Multisensory information for human postural control: integrating touch and vision. Exp Brain Res. 2000 Sep;134:107–25. doi: 10.1007/s002210000412. [DOI] [PubMed] [Google Scholar]
- 7.Sparto PJ, Whitney SL, Hodges LF, Furman JM, Redfern MS. Simulator sickness when performing gaze shifts within a wide field of view optic flow environment: preliminary evidence for using virtual reality in vestibular rehabilitation. J Neuroeng Rehabil. 2004 Dec 23;1:14. doi: 10.1186/1743-0003-1-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McComas J, MacKay M, Pivik J. Effectiveness of virtual reality for teaching pedestrian safety. Cyberpsychol Behav. 2002 Jun;5:185–90. doi: 10.1089/109493102760147150. [DOI] [PubMed] [Google Scholar]
- 9.Fung J, Richards CL, Malouin F, McFadyen BJ, Lamontagne A. A treadmill and motion coupled virtual reality system for gait training post-stroke. Cyberpsychol Behav. 2006 Apr;9:157–62. doi: 10.1089/cpb.2006.9.157. [DOI] [PubMed] [Google Scholar]
- 10.Haibach PS, Slobounov SM, Newell KM. The potential applications of a virtual moving environment for assessing falls in elderly adults. Gait Posture. 2008 Feb;27:303–8. doi: 10.1016/j.gaitpost.2007.04.004. [DOI] [PubMed] [Google Scholar]
- 11.Lockhart TE, Smith JL, Woldstad JC. Effects of aging on the biomechanics of slips and falls. Hum Factors. 2005 Winter;47:708–29. doi: 10.1518/001872005775571014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sekuler R, Sekuler AB. Oxford testbook of geriatric medicine. Oxford: Oxford University; 1992. Visual perception and cognition. [Google Scholar]
- 13.Bugnariu N, Fung J. Aging and selective sensorimotor strategies in the regulation of upright balance. J Neuroeng Rehabil. 2007;4:19. doi: 10.1186/1743-0003-4-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Holden M, Todorov E, Callaban J, Bizzi E. Virtual environment training improves motor performance in two patients with stroke. Neurology Report. 1999;23:57–67. [Google Scholar]
- 15.Liu J, Lockhart TE. Age-related joint moment characteristics during normal gait and successful reactive-recovery from unexpected slip perturbations. Gait Posture. 2009 Oct;30:276–81. doi: 10.1016/j.gaitpost.2009.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lockhart TE, Woldstad JC, Smith JL. Effects of age-related gait changes on the biomechanics of slips and falls. Ergonomics. 2003 Oct 10;46:1136–1160. doi: 10.1080/0014013031000139491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Parijat P, Lockhart TE, Liu J. Effects of Perturbation-Based Slip Training Using a Virtual Reality Environment on Slip-induced Falls. Annals of Biomedical Engineering. 2014 Sep 23; doi: 10.1007/s10439-014-1128-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dick MB, Hsieh S, Dick-Muehlke C, Davis DS, Cotman CW. The variability of practice hypothesis in motor learning: does it apply to Alzheimer's disease? Brain Cogn. 2000 Dec;44:470–89. doi: 10.1006/brcg.2000.1206. [DOI] [PubMed] [Google Scholar]
- 19.Schmidt RA. A schema theory of discrete motor skill learning. Psychological Review. 1975;82:225–260. [Google Scholar]
- 20.Drowatzky KL, Drowatzky JN. Physical training programs for the elderly. Clinical Kinesiology. 1999;53:52–62. [Google Scholar]
- 21.Briggs J. Sports therapy: theoretical and practical thoughts and considerations. Chichester: Corpus Publishing; 2001. [Google Scholar]
- 22.Kottke FJ, Halpern D, Easton JK, Ozel AT, Burrill CA. The training of coordination. Arch Phys Med Rehabil. 1978 Dec;59:567–72. [PubMed] [Google Scholar]
- 23.Chambers AJ, Cham R. Slip-related muscle activation patterns in the stance leg during walking. Gait Posture. 2007 Apr;25:565–72. doi: 10.1016/j.gaitpost.2006.06.007. [DOI] [PubMed] [Google Scholar]
- 24.Lee SJ, Hidler J. Biomechanics of overground vs. treadmill walking in healthy individuals. J Appl Physiol (1985) 2008 Mar;104:747–55. doi: 10.1152/japplphysiol.01380.2006. [DOI] [PubMed] [Google Scholar]
- 25.Kadaba MP, Ramakrishnan HK, Wootten ME, Gainey J, Gorton G, Cochran GV. Repeatability of kinematic, kinetic, and electromyographic data in normal adult gait. J Orthop Res. 1989;7:849–60. doi: 10.1002/jor.1100070611. [DOI] [PubMed] [Google Scholar]
- 26.Lockhart TE. An integrated approach towards identifying age-related mechanisms of slip initiated falls. J Electromyogr Kinesiol. 2008 Apr;18:205–17. doi: 10.1016/j.jelekin.2007.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rudolph KS, Axe MJ, Buchanan TS, Scholz JP, Snyder-Mackler L. Dynamic stability in the anterior cruciate ligament deficient knee. Knee Surg Sports Traumatol Arthrosc. 2001;9:62–71. doi: 10.1007/s001670000166. [DOI] [PubMed] [Google Scholar]
- 28.Sheik-Nainar MA, Kaber DB. The utility of a virtual reality locomotion interface for studying gait behavior. Hum Factors. 2007;49:696–709. doi: 10.1518/001872007X215773. [DOI] [PubMed] [Google Scholar]
- 29.Parijat P, Lockhart TE. Effects of moveable platform training in preventing slip-induced falls in older adults. Annals of Biomedical Engineering. 2012 May;40:1111–21. doi: 10.1007/s10439-011-0477-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Troy KL, Grabiner MD. Recovery responses to surrogate slipping tasks differ from responses to actual slips. Gait Posture. 2006;24:441–447. doi: 10.1016/j.gaitpost.2005.09.009. [DOI] [PubMed] [Google Scholar]
- 31.Lockhart TE, Kim S. Relationship between hamstring activation rate and heel contact velocity: factors influencing age-related slip-induced falls. Gait Posture. 2006 Aug;24:23–34. doi: 10.1016/j.gaitpost.2005.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Winter DA. The biomechanics and motor control of human gait: normal, elderly and pathological. 2nd. Waterloo Biomechanics, Graphic Services; 1991. [Google Scholar]
- 33.Osternig LR, Hamill J, Lander JE, Robertson R. Co-activation of sprinter and distance runner muscles in isokinetic exercise. Med Sci Sports Exerc. 1986 Aug;18:431–5. [PubMed] [Google Scholar]