Abstract
Background
Hookahs (e.g., water pipes) are increasingly being used in the U.S. and elsewhere. Despite the popularity of hookah bars, there is a paucity of research assessing the health effects of hookah smoke, and although New York City (NYC) bans indoor tobacco smoking, hookah lounges claim that they only use herbal products without tobacco and are exempt. This study investigated levels of multiple indices of air pollution in the indoor air of hookah bars in NYC.
Methods
Air samples were collected in 8 hookah bars in NYC during the summer and fall of 2013. Along with venue characteristics, real-time measurements of fine particulate matter (PM2.5), black carbon (BC), and carbon monoxide (CO), and integrated samples of total gravimetric PM, elemental carbon (EC), organic carbon (OC), and nicotine were collected in 1–2 hour sessions.
Results
Overall, levels of indoor air pollution increased with increasing numbers of active hookahs smoked. The mean (SD) real time PM2.5 level was 1179.9 (939.4) µg/m3, whereas the filter-based total PM mean was 691.3 (592.6) µg/m3. The mean real time BC level was 4.1 (2.3) µg/m3, OC was 237.9 (112.3) µg/m3, and CO was 32 (16) ppm. Airborne nicotine was present in all studied hookah bars (4.2 (1.5) µg/m3).
Conclusions
These results demonstrate that despite the ban on smoking tobacco products, at the very least, some NYC hookah bars are serving tobacco-based hookahs, and have elevated concentrations of indoor air pollutants and toxicants that may present significant health threat to visitors and employees. Therefore, there is an urgent need for better air quality monitoring in such establishments and policies to combat this emerging public health threat.
Keywords: hookahs (water pipes), secondhand smoke, air quality, exposure assessment, nicotine
INTRODUCTION
Tobacco use remains the leading preventable cause of death in the US and globally.1 Between 2000 and 2011, the consumption of cigarettes in the U.S. decreased 33%. In contrast, the use of alternative tobacco products (ATPs), such as hookahs (aka water pipes, nargiles, argiles or hubble bubble), cigarillos, cigars, bidis, kreteks, and various forms of smokeless tobacco, increased a remarkable 123% over the same time period.2 Approximately 3% of U.S. adolescents reported they were currently using and ~8% reported having ever used hookahs.3 The Centers for Disease Control and Prevention (CDC) warns that the decrease in cigarette use is being “offset by increases in other forms of tobacco”.4
Public health concern stems from the common misconception that hookah smoke is a safer alternative to cigarettes because it is “filtered” through water, despite research showing that hookah water pipes deliver tar, nicotine, and carbon monoxide in even higher doses than cigarettes.5–7 Recent meta-analyses link hookah use to lung cancer, respiratory illness, periodontal diseases and low birth-weight outcomes8 and some studies have linked its use to esophageal cancer,9,10 chromosomal abnormalities,11 decreased pulmonary and cardiovascular function,12,13 infertility,14 dental problems,15 and infectious diseases.16
According to the Surgeon General's Report, secondhand cigarette smoke includes more than 7,000 toxic chemicals and about 70 have been identified as causing cancer.17 It is well known that secondhand cigarette smoke is responsible for causing ear infections, asthma attacks, respiratory symptoms and infection, and a greater risk of sudden infant death syndrome and thus there should be a health concern for children exposed to secondhand hookah smoke in the home.18 In adults who have never smoked, SHS can cause heart disease and/or lung cancer.18 Most importantly, the report warns that there is no risk-free level of contact with SHS and that even brief exposure can be harmful to health.18
Because of the harmful and even lethal effects of secondhand smoke (SHS) from tobacco products, many states have implemented smoke-free laws that protect patrons and staff from exposure to SHS. Thirty five U.S. states, including New York, have passed laws that require 100% smoke-free workplaces including restaurants and bars.19,20 However, legislation is often limited to cigarette smoking or smoking of other nicotine containing products, thereby exempting indoor smoking of claimed “tobacco free” or “herbal” hookah products.20–24 Among 73 of the 100 largest US cities that have banned cigarette smoking in bars, 69 have exemptions that allow hookah shisha (the plant material used in hookah water pipes that contains a number of components which may or may not include tobacco, non-tobacco plant material, flavoring, odorants, and/or molasses) smoking.24 In New York City (NYC), hookah use is permitted in hookah bars if the shisha does not contain tobacco. Of note, indoor hookah use in public spaces has recently been banned even in countries where hookah use is widespread and culturally rooted such as Lebanon, Kazakhstan, Turkey, parts of India, and Saudi Arabia.21
One of the critical challenges faced by policy makers and public health officials is the scarcity of data on the quality of ambient air to which hookah bar patrons and workers are exposed and the health effects of both mainstream and secondhand hookah smoking. To our knowledge, this is the first study performed in NYC hookah bars to assess indoor air quality for toxins and pollutants, such as particulate matter (PM2.5), black carbon (BC), carbon monoxide (CO), and nicotine.
METHODS
Location Selection
Hookah bars in NYC were identified through online search engines “Yelp” and “Google Map” using key search terms “hookah/water pipe cafe”, “hookah/water pipe bar”, “hookah/water pipe lounge”. Most hookah bars are concentrated in the Lower East Side of Manhattan and a convenience sample of 8 different venues, including 1 that was visited twice, were studied.
Air Sampling and Monitoring
Sample Collection
Air quality data were collected between July and November of 2013. Air sampling occurred between 9 pm and 1 am on Wednesday, Thursday, Friday or Saturday nights, when hookah bars have the most patrons. The research team entered each venue unannounced for a 1 to 2 hr sampling session with handbags or backpacks containing air monitoring equipment. All equipment was concealed in the bag, except for a small portion of the tubing that protruded from one corner. Venue characteristics such as the number of hookahs being used at the time of sampling, active smokers, and the general ventilation status of the bars were recorded in the field.
Styrene, 2-piece cassettes (SKC, Inc; Eighty Four, PA) were used to collect total PM samples on PTFE (low trace element background; Pall Corp, Port Washington, NY) for gravimetric and trace element analyses. Using pre-baked (650°C overnight) quartz (Pall) filters, organic/elemental carbon (OC/EC) levels were analyzed. The quartz fiber filters were undenuded and thus our samples likely collected a fraction of semi-volatile organic vapors. After sampling, the quartz filters were sealed and transferred to a −20°C freezer shortly after collection. Sample flow rates were calibrated before each run using a dry gas meter (BIOS Dry Cal DC-Lite., Brandt Instruments, Prairieville, LA). Nicotine was sampled with an XAD-4 sampling tube (SKC, Inc) at a flow rate of 1.5 L/min and PTFE and quartz filters at 4 L/min. Filters and nicotine were sampled with personal sampling pumps with battery packs (BGI 400, BGI, Inc, Waltham, MA). The handbags/backpacks also contained a micro-aethalometer (Model AE51, AethLabs, San Francisco, CA), a gas monitor (GrayWolf, Shelton, CT), and a pressure and humidity compensated aerosol monitor (pDR-1500, Thermo Fisher Scientific) to measure real time BC2.5 (1 min intervals), CO, and PM2.5 (1 minute intervals) concentrations, respectively. A particle size selection device was attached to the inlet of the aethalometer and pDR-1500 to monitor PM2.5 and BC2.5.
Chemical Speciation
Gravimetric analysis of PTFE filters was performed in an environmentally-controlled weighing facility procedures (22° ± 1 ° C room temperature and 40% ± 2% relative humidity) using standard operating procedures. Filters were equilibrated to ambient conditions in the weighing facility for a minimum of 24 hours before weighing. Samples collected on PTFE filters were analyzed for 35 elements via energy dispersive X–ray fluorescence, ED–XRF (ARL QUANT’X X-Ray Fluorescence Spectrometer, Thermo Scientific) and the EPA compendium methods for metal speciation as described previously.25 Concentrations of elements were defined as above the detection limit if they were a minimum of 3 times the uncertainty of the measurements (3σ) and corrected for the mean of blank filters (n = 6). Quartz filters were analyzed for EC/OC with a Sunset Instruments carbon analyzer calibrated with a sucrose solution (4.2 µg carbon/µL). Nicotine was measured by gas chromatography using NIOSH method 2551.26 Approximately 10% of all filters were field or laboratory blanks.
RESULTS
During the peak hours, a number of variations were observed in the 8 studied hookah bars, all of which could influence air quality measurements. The number of active hookah water pipes ranged from 4 to as many as 18 with an average of 9 per bar (Table 1). The ventilation status also varied among venues, with some having multiple open windows and doors and others having none (Table 1).
Table 1.
Hookah bar characteristics.
| Hookah Bar ID |
Day of Week |
# of Active Hookahs |
Patrons | Ventilation | Temp (°F) |
|---|---|---|---|---|---|
| 1 | Wed | 4 | ND | Closed windows and open door; air condition operating |
74 |
| 2 | Fri | 18 | 36 | Closed windows and doors | 76 |
| 3 | Fri | 6 | 15 | Closed windows and doors | 73 |
| 4 | Wed | 6 | 11 | Overhead fans operating; open door | 73 |
| 5 | Fri | 10 | 30 | Closed windows and open door; fans operating |
78 |
| 5a | Wed | 4 | 20 | Closed windows and open door; fans operating |
ND |
| 6 | Fri | 4(back)+ 3 (front) |
20 | Front: closed windows and doors Back: air conditioning units operating |
76 |
| 7 | Sat | 7 | 12 | Open doors | ND |
| 8 | Th | 13 | 30 | Closed windows and doors | 70 |
Hookah bars 5 and 5a are the same bar assessed on 2 nights. ND = not determined.
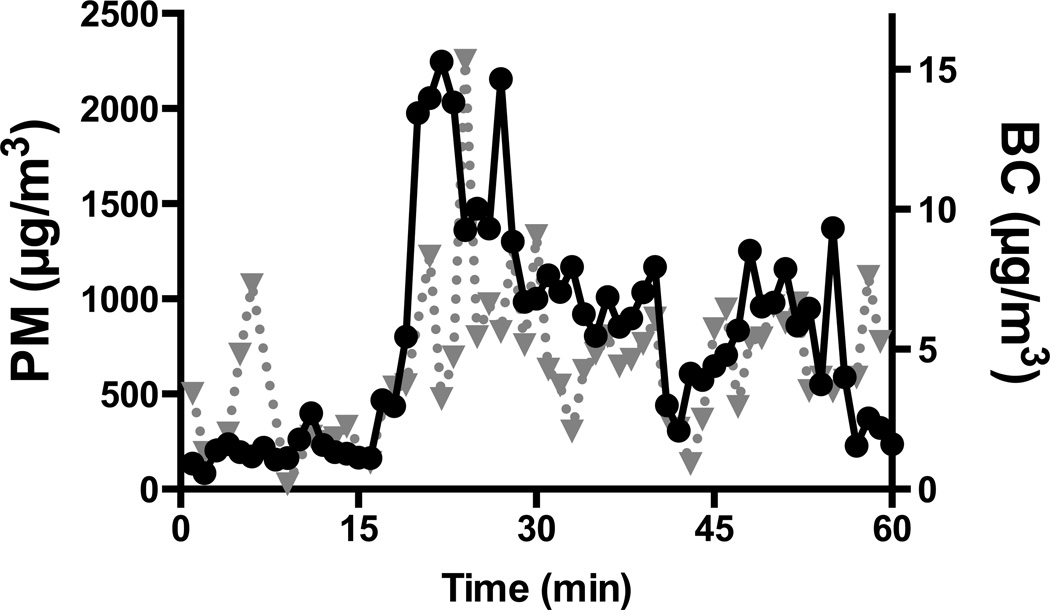
During the 1–2 hour sampling periods, the mean real time PM2.5 concentration was 1,180 µg/m3 with a range of 481– 2,986 µg/m3 (Table 2). The gravimetric filter-based total PM mean of 691 µg/m3 (range of 109 to 1,270) was lower than the real time PM2.5 concentration. Both PM2.5 and BC concentrations varied nearly an order of magnitude during the sampling period (Figure 1). BC and EC, however, made up only a small fraction of the particle mass. Mean BC level was 4.1 µg/m3 with a range of 1.2 to 7.6 µg/m3. Although the filter-based EC measurements should generally be equivalent to the real time BC values, EC was below the detection limit for all but one hookah bar. OC accounted for a larger mass fraction of indoor particles with a mean concentration of 238 µg/m3 and a range of 59 µg/m3 to 404 µg/m3. Mean CO was 32 ppm with a range of 10–50 ppm.
Table 2.
Hookah bar air pollution concentrations.
| Hookah Bar ID |
Real Time PM2.5 (µg/m3) |
Gravimetric PM (µg/m3) |
BC (µg/m3) |
EC (µg/m3) |
OC (µg/m3) |
CO ppm |
Nicotine (µg/m3) |
|---|---|---|---|---|---|---|---|
| 1 | 1,279.4 | 833.0 | 3.5 | BDL | 321.6 | 28 | 4.9 |
| 2 | 481.3 | 321.3 | 6.6 | BDL | 59.3 | 49 | 3.4 |
| 3 | 694.3 | ND | 5.8 | ND | ND | 10 | 4.4 |
| 4 | ND | 109.4 | 1.4 | BDL | 189.0 | 50 | 4.0 |
| 5 | 2,986.4 | 1,270.2 | 7.6 | 5.3 | 225.2 | ND | ND |
| 5a | 540.9 | 141.2 | ND | 5.3 | 291.5 | ND | 2.7 |
| 6 | ND | 1,112.5 | 3.0 | BDL | 403.6 | 34 | 2.7 |
| 7 | 135.6 | ND | 1.2 | BDL | 175.3 | ND | ND |
| 8 | 1,607.1 | 1,091.1 | 4.2 | ND | ND | 21 | 7.1 |
| Regulatory Standard | NA | 35 µg/m3 | NA | 3.5 mg/m3 | NA | 35 | 500 µg/m3 |
Hookah bars 5 and 5a are the same bar assessed on 2 nights. ND = not determined; BDL = below the detection limit; NA = none available. The regulatory standard for PM and CO are EPA's 24 hr and 1 hr, respectively, National Ambient Air Quality Standards, whereas elemental carbon and nicotine are OSHA's 8 hr Permissible Exposure Limits.
Figure 1.
Real time levels of PM2.5 (solid black line and circles) and black carbon (BC; dotted gray line and triangles) in hookah bar #3 (1 minute intervals).
Additionally, airborne nicotine was found in all establishments (Table 2), despite the ban on the use of tobacco-based shisha in water pipes in NYC hookah bars. As shown in Table 3, the elemental composition of the secondhand hookah smoke particulate matter was dominated by Na, S, Cl, K, and Ca. In general, the airborne elemental concentrations were less than 1 µg/m3 with a maximum value of 6 µg/m3 for Cl.
Table 3.
Trace element concentrations (ng/m3) in NYC hookah bars as measured by x-ray fluorescence.
| Hookah Bar ID |
Na | Mg | Al | S | Cl | K | Ca | Fe | Zn |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 511 | 94 | BDL | 128 | 986 | 192 | 242 | 84 | 23 |
| 2 | 1,152 | 61 | BDL | 1,126 | 6,098 | 5,494 | 226 | 116 | 129 |
| 3 | 193 | 91 | 15 | 364 | 627 | 955 | 768 | 259 | 37 |
| 4 | 208 | 68 | 20 | 165 | 142 | 393 | 108 | 74 | 12 |
| 5 | 135 | 53 | 31 | 199 | 176 | 130 | 312 | 95 | 16 |
| 5a | BDL | 1 | BDL | 151 | 110 | 92 | 119 | 68 | 21 |
| 6 | ND | ND | ND | ND | ND | ND | ND | ND | ND |
| 7 | 71 | 22 | 20 | 80 | 200 | 485 | 146 | 83 | 12 |
| 8 | 384 | 302 | 68 | 396 | 1,153 | 2,237 | 2,681 | 196 | 40 |
ND = not determined and BDL = below the detection limit.
DISCUSSION
To the best of our knowledge, this is the first study to assess indoor air quality in hookah bars in NYC, a city with the largest number of hookah bars in the U.S. based on Internet searches. Although there are no indoor regulatory standards for air quality indices, the indoor hookah bar concentrations of ambient air pollutant and toxicants, such as PM2.5 and CO, were found to exceed the 24 hr and 1 hr U.S. federal standards for outdoor PM2.5 and CO, respectively.27 The levels of elemental carbon and nicotine were below the occupational standards promulgated by the Occupational Safety and Health Administration, although these standards are intended for healthy workers and may not be applicable to the general population or susceptible individuals. Perhaps most importantly, measurable airborne concentrations of nicotine were found in all hookah bars studied, suggesting that tobacco-based shisha is, in fact, commonly used in NYC hookah bars, in violation of NYC laws. This suggests that there is an urgent need for official assessment to see if lounges are non-compliant with NYC law. The findings raise serious concerns about potential adverse health effects among patrons and employees of hookah bars. We believe the findings reported provide critical information to assist tobacco policy and public health officials in regulating hookah smoking in hookah bars in NYC.
An increasing number of studies have examined the presence of particulate air pollution in hookah bars. The first published study on indoor air quality of hookah bars measured PM2.5 in 10 hookah lounges in Oregon.28 Those authors suggested that by comparison of the hookah smoke PM2.5 to the U.S. EPA ambient air quality standard for PM2.5, the air quality in the hookah bars ranged from “unhealthy” to “hazardous”, although it might not be appropriate to compare the 24 hr PM2.5 standard to an acute indoor exposure. Subsequently, Cobb et al investigated the indoor air pollution, again measuring only PM2.5 , in 28 hookah cafes in Virginia and reached similar conclusions.20 A Canadian study by Zhang et al 21 extended these findings by examining not only airborne PM2.5, but also CO and nicotine levels. Their observed levels of CO and nicotine in Toronto hookah bars were 18 ppm and 3 µg/m3, respectively, similar to our findings in NYC. The results from these studies suggested a concern for adverse health effects due to exposure to secondhand hookah smoke in hookah hospitality venues.21 A more recent study of water pipe cafes in Baltimore, Maryland found that concentrations of CO and PM2.5 were substantially elevated in water pipe cafes and were higher than in bars where cigarettes were smoked. While air nicotine concentrations were not as high as in cafes where cigarettes were smoked, the nicotine levels were significantly higher than in smoke-free bars and restaurants.29 The findings from the present study complement and extend those of the previous studies by assessing not only airborne PM, nicotine, and CO, but also BC, EC, OC, and trace elements in NYC hookah bars.
Among the selected locations, the real time mean PM2.5 concentration was 1,179 µg/m3 with a peak mean value of 2,986 µg/m3 at one hookah venue. These values were higher than those reported for secondhand smoke levels in bars where and when cigarette smoking has been permitted in the U.S., Scotland,30 and Asia.31 In comparison, the gravimetric PM concentrations were, as expected, lower than the real time PM2.5 concentrations, likely due to measurement error possibly resulting from the presence of water, on the airborne secondhand hookah smoke particles, which may be removed (potentially along with volatile and semi-volatile compounds) during the PTFE filter equilibration period in the climate-controlled weighing facility. Regardless, the indoor particle concentrations were considerably higher than the ambient outdoor values, which were generally 5 to 15 µg/m3, as measured with the real time monitor just prior to entering and after exiting the NYC hookah bars (data not shown).
While ascertaining the indoor concentration of PM in hookah bars is critical in risk evaluations, particle composition is also important. The concentration ratio of combustion products of plant material used in shisha, including organic and elemental carbon compounds, depends upon combustion efficiency and the burning/charring temperature of the shisha. This is the first study to report that the indoor BC concentration in hookah bars (4.1 µg/m3) was greater than outdoor ambient BC levels previously measured in the boroughs of NYC.32–34 However, BC accounted for less than 1% of the airborne particle mass in the secondhand hookah smoke, suggesting that it may not significantly contribute to the adverse effects of secondhand hookah smoke. On the other hand, organic carbon (238 µg/m3) constituted a larger fraction of the secondhand hookah smoke and therefore, may play a more important role in adverse health effects. XRF analysis of trace elements was also performed and the results (Table 3) show that Ca, Na, Cl, K, S, and Mg are present in the greatest amounts in secondhand hookah smoke. As with BC, these elements accounted for a small fraction of the total PM mass concentration. Based upon our limited sampling, however, the large variability in trace element concentrations among the hookah bars suggests that the source of the particles, i.e., the charcoal and the shisha, differed from bar to bar.
This study also found that levels of CO, a gaseous component with a mean of 32 ppm and a peak value of 50 ppm observed in one hookah bar, were considerably higher than EPA’s National Ambient Air Quality Standard (NAAQS) for 8 hrs and approached the 1 hr standard of 35 ppm.27 Recent studies have examined exhaled CO in patrons of hookah bars and demonstrated that exposure to CO via inhalation of mainstream and secondhand hookah smoke can result in exhaled CO concentrations that are similar to those observed with cigarette smoke.35 Although symptoms from acute CO poisoning are nonspecific, including dizziness, irritability, nausea, vomiting, syncope, and chest pain, prolonged exposure can have dire consequences such as myocardial infarction, cerebral edema, coma and even death.36 Acute CO poisoning in hookah users has been documented in several case reports, with patients presenting to the emergency department with syncope, confusion, slurred speech, and a serum carboxyhemoglobin level as high as 30% after hookah use.37–41 Although these studies have not partitioned out the contribution from mainstream vs. secondhand hookah smoke, it has been determined that the majority of CO produced by a hookah water pipe stems from the inefficient burning of charcoal, rather than the heating of shisha itself,42 suggesting an inherent danger of hookah smoking, regardless of the composition of shisha.
Although hookah bars in NYC are not allowed to use tobacco-based shisha in hookah water pipes, nicotine was found in each venue with a mean concentration of 4.2 µg/m3. We can think of no alternative explanation for the ambient levels of nicotine found, other than that the nicotine emanated from the smoke generated by the hookah use. Potentially, cigarette smoking by patrons and employees in back rooms may occur, but no cigarette smoking was observed in the main room of the hookah bars surveyed in this study. In addition to its potential for addiction and as a gateway to the use of other tobacco products, nicotine is known to have myriad harmful health consequences, such as teratogenic effects on neurodevelopment,43,44 “altering the formation, survival, and differentiation of brain cells, eliciting deficits in structure, synaptic function and behavioral performance”,45 and alteration in neurotransmitters,46 as well as being associated with fatal arrhythmias,47 low birth weight from prenatal exposure,48 hearing loss,49 tooth decay,50 and hyperactivity.51,52
In a typical hookah smoking session, a user inhales as much as 100 L of mainstream smoke53 containing numerous toxicants and carcinogens.5,54,55 In addition to the large amount of mainstream hookah smoke inhaled during a typical session, the effects of SHS are of particular concern. Although it must be noted that the composition of mainstream and secondhand hookah smoke differs from that produced at the higher temperatures occurring in cigarette smoking, these data strongly suggest that both active and passive hookah smokers, including individuals working in such settings, may be at as great or greater risk for tobacco-related adverse health effects than those using or exposed to smoke from cigarettes.
Limitations in the present study must be considered in applying the results broadly to other hookah venues and cities. The selection of the 8 NYC hookah bars was not random as we assessed ones that were popular among young urbanites based upon ratings on 2 internet sites. Moreover, the measurements were performed on nights with the greatest occupancy. Although the sample size of this study was sufficient to demonstrate that air quality in the selected hookah bars was hazardous to health, one should use caution in generalizing this finding to all the hookah venues in NYC, where over 100 such venues exist, or other cities. Additional potential factors that may have affected the observed variability among hookah bars’ indoor air quality include the number of open windows and doors, the size of the venues, air handling, and the number of active hookah water pipes and smokers. Interestingly, so-called ‘smoke-eaters’, which are commonly used to remove smoke, were not observed at any of the hookah bars. Although the present study extended basic measurements of PM and CO to elemental/organic carbon, nicotine, and trace elements, it was limited in the amount of sampling equipment that could be carried unannounced into hookah bars. Important toxic and carcinogenic components of tobacco smoking, such as polynuclear aromatic hydrocarbons (PAHs) and 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanol (NNALs), should be assessed in future studies.
The findings of this study provide evidence that hookah bars in NYC serve tobacco-based shisha in hookahs and generate levels of SHS potentially hazardous to the health of patrons and employees. This information is critical to informing tobacco control policies and regulations for SHS generated from hookahs—perhaps the most rapidly adopted alternative tobacco product in the U.S. These findings raise profoundly important and difficult public health policy questions, such as how one would obtain a random sample of sufficient size in NYC and elsewhere to make generic decisions about regulating hookah bars locally or nationally. That is, what public policies could be created and put into place to monitor hookah lounges in an ongoing fashion? In addition, there is a clear need to extend research to focus not only on the indoor air quality of public hookah bars, but also the toxicant exposure and health effects of home hookah users and those who reside with them. Moreover, there is a need to investigate whether non-tobacco based shishas, similar to tobacco based product, present a major public health hazard, which would then lead to policy debates about how municipalities, states, and the federal government would regulate the use of these forms of shisha.
What this paper adds.
This is the first study to show that many hookah bars in NYC serve tobacco-based shisha.
NYC hookah bars contain concentrations of indoor air pollutants and toxicants that may present significant health threat to visitors and employees.
There is an urgent need for better air quality monitoring and tobacco control policies in hookah bars.
Acknowledgements
The authors would like to thank Dr. George Thurston for the use of sampling equipment.
Funding Statement: This work was supported by NIEHS Center of Excellence grant number ES000260, and NCI grant number 3 P30 CA016087-33S1.
Footnotes
Competing Interests Statement: None of the authors have any conflict of interest to declare.
Contributorship Statement:
Sherry Zhou and Terry Gordon were integral from the conceptualization, design and execution of the study. Ms. Zhou drafted the initial manuscript and submitted the study.
Michael Weitzman, Ruzmyn Vilcassim, Jennifer Wilson, Nina Legrand, Eric Saunders, Mark Travers, Lung-Chi Chen, and Richard Peltier all had substantial contribution to all stages of this study, especially in collecting and analyzing data. They also helped draft the initial manuscript, interpreted results, critically reviewed and revised the manuscript, and approved the final manuscript as submitted.
REFERENCES
- 1.Samet JM. Tobacco smoking: the leading cause of preventable disease worldwide. Thorac Surg Clin. 2013 May;23(2):103–112. doi: 10.1016/j.thorsurg.2013.01.009. [DOI] [PubMed] [Google Scholar]
- 2.Consumption of cigarettes and combustible tobacco—United States, 2000–2011. Morbidity and Mortality Weekly Report. 61(30):565–569. [PubMed] [Google Scholar]
- 3.Amrock SM, Gordon T, Zelikoff JT, et al. Hookah Use Among Adolescents in the United States: Results of a National Survey. Nicotine & tobacco research : official journal of the Society for Research on Nicotine and Tobacco. 2013 Oct 23; doi: 10.1093/ntr/ntt160. [DOI] [PubMed] [Google Scholar]
- 4.Centers for Disease Control (CDC) Drop in cigarette consumption offset by increases in other forms of smoked tobacco. 2012 [Google Scholar]
- 5.Shihadeh A. Investigation of mainstream smoke aerosol of the argileh water pipe. Food and chemical toxicology : an international journal published for the British Industrial Biological Research Association. 2003 Jan;41(1):143–152. doi: 10.1016/s0278-6915(02)00220-x. [DOI] [PubMed] [Google Scholar]
- 6.Knishkowy B, Amitai Y. Water-pipe (narghile) smoking: an emerging health risk behavior. Pediatrics. 2005 Jul;116(1):e113–e119. doi: 10.1542/peds.2004-2173. [DOI] [PubMed] [Google Scholar]
- 7.Eissenberg T, Shihadeh A. Waterpipe tobacco and cigarette smoking: direct comparison of toxicant exposure. American journal of preventive medicine. 2009 Dec;37(6):518–523. doi: 10.1016/j.amepre.2009.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Akl EA, Gaddam S, Gunukula SK, et al. The effects of waterpipe tobacco smoking on health outcomes: a systematic review. International journal of epidemiology. 2010 Jun;39(3):834–857. doi: 10.1093/ije/dyq002. [DOI] [PubMed] [Google Scholar]
- 9.Gunaid AA, Sumairi AA, Shidrawi RG, et al. Oesophageal and gastric carcinoma in the Republic of Yemen. British journal of cancer. 1995 Feb;71(2):409–410. doi: 10.1038/bjc.1995.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nasrollahzadeh D, Kamangar F, Aghcheli K, et al. Opium, tobacco, and alcohol use in relation to oesophageal squamous cell carcinoma in a high-risk area of Iran. British journal of cancer. 2008 Jun 3;98(11):1857–1863. doi: 10.1038/sj.bjc.6604369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yadav JS, Thakur S. Genetic risk assessment in hookah smokers. Cytobios. 2000;101(397):101– 113. [PubMed] [Google Scholar]
- 12.Al Mutairi SS, Shihab-Eldeen AA, Mojiminiyi OA, et al. Comparative analysis of the effects of hubble-bubble (Sheesha) and cigarette smoking on respiratory and metabolic parameters in hubble-bubble and cigarette smokers. Respirology (Carlton, Vic.) 2006 Jul;11(4):449–455. doi: 10.1111/j.1440-1843.2006.00873.x. [DOI] [PubMed] [Google Scholar]
- 13.Kiter G, Ucan ES, Ceylan E, et al. Water-pipe smoking and pulmonary functions. Respiratory medicine. 2000 Sep;94(9):891–894. doi: 10.1053/rmed.2000.0859. [DOI] [PubMed] [Google Scholar]
- 14.Inhorn MC, Buss KA. Ethnography, epidemiology and infertility in Egypt. Social science & medicine (1982) 1994 Sep;39(5):671–686. doi: 10.1016/0277-9536(94)90023-x. [DOI] [PubMed] [Google Scholar]
- 15.Dar-Odeh NS, Abu-Hammad OA. Narghile smoking and its adverse health consequences: a literature review. British dental journal. 2009 Jun 13;206(11):571–573. doi: 10.1038/sj.bdj.2009.475. [DOI] [PubMed] [Google Scholar]
- 16.Steentoft J, Wittendorf J, Andersen JR. Tuberculosis and water pipes as source of infection. Ugeskrift for laeger. 2006 Feb 27;168(9):904–907. [PubMed] [Google Scholar]
- 17.A Report of the Surgeon General: How Tobacco Smoke Causes Disease: What It Means to You. Atlanta: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2010. [Google Scholar]
- 18.The Health Consequences of Involuntary Exposure to Tobacco Smoke: A Report of the Surgeon General. Atlanta: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, Office on Smoking and Health; 2006. [PubMed] [Google Scholar]
- 19.American Nonsmokers' Rights Foundation. Overview List - How Many Smoke Free Laws? http://www.no-smoke.org/pdf/mediaordlist.pdf.
- 20.Cobb CO, Vansickel AR, Blank MD, et al. Indoor air quality in Virginia waterpipe cafes. Tobacco control. 2013 Sep;22(5):338–343. doi: 10.1136/tobaccocontrol-2011-050350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhang B, Haji F, Kaufman P, et al. 'Enter at your own risk': a multimethod study of air quality and biological measures in Canadian waterpipe cafes. Tobacco control. 2013 Oct 25; doi: 10.1136/tobaccocontrol-2013-051180. [DOI] [PubMed] [Google Scholar]
- 22.Hammal F, Chappell A, Wild TC, et al. 'Herbal' but potentially hazardous: an analysis of the constituents and smoke emissions of tobacco-free waterpipe products and the air quality in the cafes where they are served. Tobacco control. 2013 Oct 15; doi: 10.1136/tobaccocontrol-2013-051169. [DOI] [PubMed] [Google Scholar]
- 23.Noonan D. Exemptions for hookah bars in clean indoor air legislation: a public health concern. Public Health Nurs. 2010 Jan-Feb;27(1):49–53. doi: 10.1111/j.1525-1446.2009.00826.x. [DOI] [PubMed] [Google Scholar]
- 24.Primack BA, Hopkins M, Hallett C, et al. US health policy related to hookah tobacco smoking. American journal of public health. 2012 Sep;102(9):e47–e51. doi: 10.2105/AJPH.2012.300838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Maciejczyk P, Zhong M, Li Q, et al. Effects of subchronic exposures to concentrated ambient particles (CAPs) in mice. II. The design of a CAPs exposure system for biometric telemetry monitoring. Inhalation toxicology. 2005 Apr;17(4–5):189–197. doi: 10.1080/08958370590912743. [DOI] [PubMed] [Google Scholar]
- 26.National Institute of Occupational Safety and Health. Nicotine. 2003. Method 2551. Issue 1. www.cdc.gov/niosh/docs/2003-154/pdfs/2551.pdf.
- 27.U.S. Environmental Protection Agency. National Ambient Air Quality Standards (NAAQS) http://www.epa.gov/air/criteria.html.
- 28.Fiala SC, Morris DS, Pawlak RL. Measuring indoor air quality of hookah lounges. American journal of public health. 2012 Nov;102(11):2043–2045. doi: 10.2105/AJPH.2012.300751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Torrey CM, Moon KA, Williams DA, et al. Waterpipe cafes in Baltimore, Maryland: Carbon monoxide, particulate matter, and nicotine exposure. Journal of exposure science & environmental epidemiology. 2014 doi: 10.1038/jes.2014.19. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Semple S, Creely KS, Naji A, et al. Secondhand smoke levels in Scottish pubs: the effect of smoke-free legislation. Tobacco control. 2007 Apr;16(2):127–132. doi: 10.1136/tc.2006.018119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lee J, Lim S, Lee K, et al. Secondhand smoke exposures in indoor public places in seven Asian countries. International journal of hygiene and environmental health. 2010 Sep;213(5):348–351. doi: 10.1016/j.ijheh.2010.05.007. [DOI] [PubMed] [Google Scholar]
- 32.Kheirbek I, Ito K, Neitzel R, et al. Spatial Variation in Environmental Noise and Air Pollution in New York City. Journal of urban health : bulletin of the New York Academy of Medicine. 2014 Feb 1; doi: 10.1007/s11524-013-9857-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Clougherty JE, Kheirbek I, Eisl HM, et al. Intra-urban spatial variability in wintertime street-level concentrations of multiple combustion-related air pollutants: the New York City Community Air Survey (NYCCAS) Journal of exposure science & environmental epidemiology. 2013 May-Jun;23(3):232–240. doi: 10.1038/jes.2012.125. [DOI] [PubMed] [Google Scholar]
- 34.Spira-Cohen A, Chen LC, Kendall M, et al. Personal exposures to traffic-related particle pollution among children with asthma in the South Bronx, NY. Journal of exposure science & environmental epidemiology. 2010 Jul;20(5):446–456. doi: 10.1038/jes.2009.34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Martinasek MP, Ward KD, Calvanese AV. Change in Carbon Monoxide Exposure Among Water Pipe Bar Patrons. Nicotine & tobacco research : official journal of the Society for Research on Nicotine and Tobacco. 2014 Mar 18; doi: 10.1093/ntr/ntu041. [DOI] [PubMed] [Google Scholar]
- 36.Prockop LD, Chichkova RI. Carbon monoxide intoxication: an updated review. J Neurol Sci. 2007 Nov 15;262(1–2):122–130. doi: 10.1016/j.jns.2007.06.037. [DOI] [PubMed] [Google Scholar]
- 37.Bens BW, ter Maaten JC, Ligtenberg JJ. Carbon monoxide poisoning after smoking from a water pipe. Ned Tijdschr Geneeskd. 2013;157(29):A6201. [PubMed] [Google Scholar]
- 38.Clarke SF, Stephens C, Farhan M, et al. Multiple patients with carbon monoxide toxicity from water-pipe smoking. Prehosp Disaster Med. 2012 Dec;27(6):612–614. doi: 10.1017/S1049023X12001227. [DOI] [PubMed] [Google Scholar]
- 39.La Fauci G, Weiser G, Steiner IP, et al. Carbon monoxide poisoning in narghile (water pipe) tobacco smokers. Cjem. 2012 Jan;14(1):57–59. doi: 10.2310/8000.2011.110431. [DOI] [PubMed] [Google Scholar]
- 40.Ozkan S, Ozturk T, Ozmen Y, et al. Syncope Associated with Carbon Monoxide Poisoning due to Narghile Smoking. Case Rep Emerg Med. 2013;2013:796857. doi: 10.1155/2013/796857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Turkmen S, Eryigit U, Sahin A, et al. Carbon monoxide poisoning associated with water pipe smoking. Clin Toxicol (Phila) 2011 Aug;49(7):697–698. doi: 10.3109/15563650.2011.598160. [DOI] [PubMed] [Google Scholar]
- 42.Monzer B, Sepetdjian E, Saliba N, et al. Charcoal emissions as a source of CO and carcinogenic PAH in mainstream narghile waterpipe smoke. Food and chemical toxicology : an international journal published for the British Industrial Biological Research Association. 2008 Sep;46(9):2991–2995. doi: 10.1016/j.fct.2008.05.031. [DOI] [PubMed] [Google Scholar]
- 43.Nicol CJ, Harrison ML, Laposa RR, et al. A teratologic suppressor role for p53 in benzo[a]pyrene-treated transgenic p53-deficient mice. Nature Genetics. 1995;10(2):181–187. doi: 10.1038/ng0695-181. [DOI] [PubMed] [Google Scholar]
- 44.Slotkin TA, Orband Miller L, Queen KL. Development of [3H]nicotine binding sites in brain regions of rats exposed to nicotine prenatally via maternal injections or infusions. The journal of pharmacology and experimental therapeutics. 1987;242(1):232–237. [PubMed] [Google Scholar]
- 45.Slotkin T, Pinkerton K, Seidler F. Perinatal environmental tobacco smoke exposure in rhesus monkeys: critical periods and regional selectivity for effects on brain cell development and lipid peroxidation. Environmental Health Perspectives. 2006;114(1):34–39. doi: 10.1289/ehp.8286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Slotkin T, Seidler F. Mimicking maternal smoking and pharmacotherapy of preterm labor: interactions of fetal nicotine and dexamethasone on serotonin and dopamine synaptic function in adolescence and adulthood. Brain Research Bulletin. 2010;82(1–2):124–134. doi: 10.1016/j.brainresbull.2010.02.015. [DOI] [PubMed] [Google Scholar]
- 47.Feng Y, Caiping M, Li C, et al. Fetal and offspring arrhythmia following exposure to nicotine during pregnancy. Journal of applied toxicology. 2010;30(1):53–58. doi: 10.1002/jat.1471. [DOI] [PubMed] [Google Scholar]
- 48.Langley. Effects of low birth weight, maternal smoking in pregnancy and social class on the phenotypic manifestation of Attention Deficit Hyperactivity Disorder and associated antisocial behaviour: investigation in a clinical sample. BMC Psychiatry. 2007;7:26. doi: 10.1186/1471-244X-7-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Fabry D, Davila E, Arheart K, et al. Secondhand smoke exposure and the risk of hearing loss. Tobacco control. 2011;20(1):82–85. doi: 10.1136/tc.2010.035832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Aligne CA, Moss M, Auinger P, et al. Association of pediatric dental caries with passive smoking. JAMA (Chicago, Ill.) 2003;289(10):1258–1264. doi: 10.1001/jama.289.10.1258. [DOI] [PubMed] [Google Scholar]
- 51.Peters MA, Ngan LL. The effects of totigestational exposure to nicotine on pre- and postnatal development in the rat. Archives internationales de pharmacodynamie. 1982;257(1):155–167. [PubMed] [Google Scholar]
- 52.Richardson SA, Tizabi Y. Hyperactivity in the offspring of nicotine-treated rats: role of the mesolimbic and nigrostriatal dopaminergic pathways. Pharmacology, biochemistry and behavior. 1994;47(2):331–337. doi: 10.1016/0091-3057(94)90018-3. [DOI] [PubMed] [Google Scholar]
- 53.Katurji M, Daher N, Sheheitli H, et al. Direct measurement of toxicants inhaled by water pipe users in the natural environment using a real-time in situ sampling technique. Inhalation toxicology. 2010 Nov;22(13):1101–1109. doi: 10.3109/08958378.2010.524265. [DOI] [PubMed] [Google Scholar]
- 54.Sepetdjian E, Abdul Halim R, Salman R, et al. Phenolic compounds in particles of mainstream waterpipe smoke. Nicotine & tobacco research : official journal of the Society for Research on Nicotine and Tobacco. 2013 Jun;15(6):1107–1112. doi: 10.1093/ntr/nts255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Shihadeh A, Saleh R. Polycyclic aromatic hydrocarbons, carbon monoxide, "tar", and nicotine in the mainstream smoke aerosol of the narghile water pipe. Food and chemical toxicology : an international journal published for the British Industrial Biological Research Association. 2005 May;43(5):655–661. doi: 10.1016/j.fct.2004.12.013. [DOI] [PubMed] [Google Scholar]