Abstract
Introduction
Erectile dysfunction (ED) is a risk factor for cardiovascular disease (CVD). We examine the costs of screening men with ED for CVD risk factors and the cost savings of treating these at risk men.
Aim
To evaluate the effect of screening men presenting with ED for CVD risk factors and to determine the cost effectiveness of this screening protocol.
Methods
The known incidence and prevalence of ED and CVD, the rate of undiagnosed CVD, and the effects of CVD treatment were used to model the change in prevalence of acute CVD events and ED as a function of the number of men with ED and CVD. The cost savings associated with reduction in acute CV events and ED prevalence was estimated over 20 years.
Main Outcome Measures
Acute CVD event rate reduction and associated cost savings were modeled over 20 years.
Results
The relative risk (RR) of ED in men with CVD is 1.47 and the co-prevalence of both ED and CVD was estimated at 1,991,520 men. Approximately 44% of men with CVD risk factors are unaware of their risk. If all men presenting with ED were screened for CVD, 5.8 million men with previously unknown CVD risk factors would be identified over 20 years, costing $2.7 billion to screen. Assuming a 20% decrease in CV events as a result of screening and treatment, 1.1 million cardiovascular events would be avoided, saving $21.3 billion over 20 years. Similarly, 1.1 million cases of ED would be treated, saving $9.7 billion. Together, the reduction in acute CVD and ED treatment cost would save $28.5 billion over 20 years.
Conclusions
Screening for CVD in men presenting with ED can be a cost-effective intervention for secondary prevention of both CVD and, over the longer term, ED.
Keywords: erectile dysfunction, cardiovascular disease, cardiovascular risk factors, cost analysis, erectile dysfunction treatment, cardiovascular disease treatment
INTRODUCTION
Erectile dysfunction is the persistent inability to achieve or maintain penile erection sufficient for satisfactory sexual performance, and affects more than 18 million men in the United States alone1–2. It has significant societal cost; over $1 billion a year worldwide is spent on pharmacological treatment of ED3. A growing body of evidence links cardiovascular disease (CVD) and erectile dysfunction, with both conditions having similar risk factors including hypertension, hyperlipidemia, diabetes, obesity and smoking. Because penile arteries have a smaller diameter than coronary arteries, the earliest manifestation of CVD may be ED4. In fact, a growing body of literature has identified ED to be an independent risk factor for coronary heart disease (CHD) and stroke, on par with smoking and a family history of CHD1,3–6. Data from the Prostate Cancer Prevention Trial linked the onset of ED with angina, myocardial infarction (MI), and stroke5, whereas the Massachusetts Male Aging Study (MMAS) demonstrated that the relative risk (RR) for ED in the setting of CVD is 1.41 (95% CI 1.05–1.90) even when controlling for age and traditional CV risk factors2. A meta-analysis by Dong et al. supports an increased risk of CVD, stroke and all-cause mortality in men with ED6, and a meta-analysis by Vlachopoulos et al. demonstrated an independent association between ED, CVD, and all cause mortality, showing a greater effect of ED on CVD and mortality in younger men7. In men less than 75 years old, ED is predictive of future atherosclerotic cardiovascular events2,8. The higher rate of CVD events in men with ED is present even in diabetic men with ED when compared to those without9. A recent meta-analysis demonstrated that the RR of CVD in men presenting with ED is 1.47, demonstrating a clear cardiac risk in these men10.
While ED has been regarded as a disease of older age, over 20% of men less than 40 years old may suffer from ED11. A study of men 18–45 years old presenting with ED demonstrated that more than 50% showed signs of insulin resistance, suggesting vascular dysfunction may occur at a younger age than previously appreciated12. Flaccid penile acceleration can predict adverse metabolic profiles in younger men13. In fact, a near 50-fold increase in CHD incidence was observed in men 40–49 years old with ED versus men without, indicating potential prognostic utility of screening for CVD risk in younger men with ED14. Importantly, CVD screening at presentation for ED may be most valuable in younger men, as the relative risk of CVD associated with ED is inversely correlated with age15.
ED shares an underlying pathophysiology with CVD, specifically endothelial cell dysfunction and impaired nitrous oxide (NO) production16,17. Accordingly, it is possible that improving overall vascular health may improve ED symptoms. Lifestyle changes resulting in weight loss, lower blood pressure and higher HDL cholesterol also reduce ED symptoms16. Moreover, it is hypothesized that phosphodiesterase 5 inhibitor (PDE5i) treatment may improve endothelial function with resultant improvement in CVD outcomes, as PDE5i treatment decreases pulmonary and coronary vascular tone18. PDE5i's are commonly used for the treatment of ED in men with CVD, although the effects of PDE5i’s have not been clearly studied for CVD endpoints16,17,19.
Given the clear value of ED as a risk factor for CVD, attempts have been made to incorporate ED screening and treatment into risk stratification for CVD. However, analysis of the MMAS data showed that inclusion of ED screening in the Framingham risk score failed to significantly increase its ability to predict myocardial infarction (MI) or coronary death2. Nevertheless, patients presenting with ED provide an opportunity to diagnose and treat underlying CVD. In fact, the third Princeton Consensus Conference recommends cardiac risk stratification in men presenting with ED20. This point of intervention may be particularly valuable in men who are not aware of underlying CVD and CVD risk factors (CVDRFs) and who may not otherwise seek regular healthcare21.
We perform a cost analysis for screening men over 20 years of age presenting with ED for CVD, assessing the cost and impact of screening and treatment of these men on incidence and prevalence of CVD.
METHODS
Pertinent Data Identification and Extraction
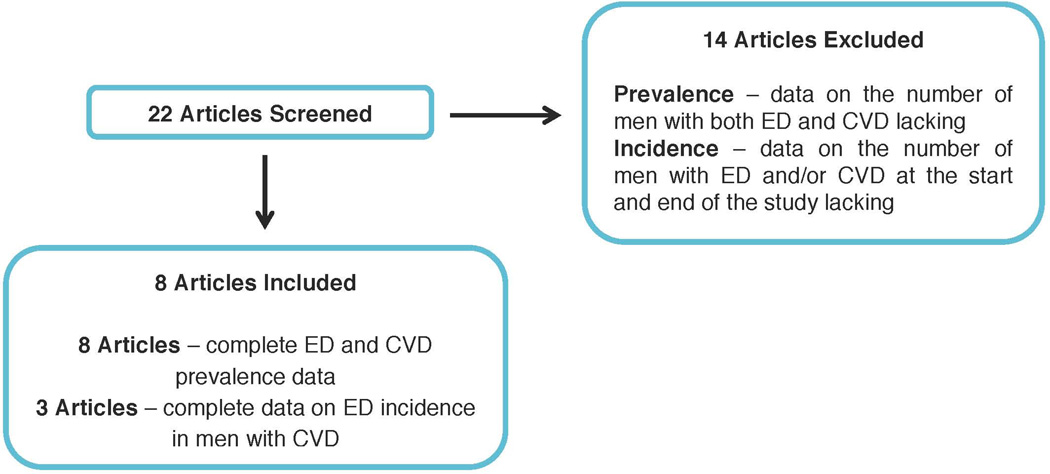
A PubMed literature search was performed for the terms “erectile dysfunction”, “coronary vascular disease”, “coronary artery disease,” “incidence”, and “prevalence” and articles containing information about the prevalence and incidence of ED within a population of men with CVD were identified. Twenty-two articles were identified with data relevant to the incidence and prevalence of CVD and ED. Of the 22 articles, 8 clearly defined the prevalence of ED in CVD patients2,5,9,14,22–25; these articles provided estimates for the number of men with CVD, as well as estimates for the number of ED cases among these men. For incidence data, 3 articles contained data sufficient to estimate ED incidence in men with CVD9,24,26. Incidence and prevalence rates were then extracted and averaged (Figure 1).
Figure 1. Selection of Relevant Articles for Identification of ED and CVD Incidence and Prevalence.
Flow chart depicting selection process of published articles containing ED and CVD prevalence and incidence data.
Costs Associated with CVD
The cost of CVDRF screening, including blood pressure measurement, lipid panel, and Hemoglobin A1c was determined from Medicare reimbursement rates from the Urologic Diseases in America Online Compendium (UDAOC) 2012 data (Table 2). The average cost per acute CV event was determined from aggregated Medicare data for discharge costs for the Major Diagnostic Classification (MDC) of Disease of the Circulatory System (MDC 7) for 2012, the last year available (Table 3). Medicare costs frequently represent the benchmark against which insurance companies base their pricing. This cost for CVD was $11,602 for an average hospital stay of 4.7 days and was used to calculate the total cost of acute CV events avoided27.
Table 2.
CVD Screening Costs44
| Test | Cost | |
|---|---|---|
| HbA1c | $ | 65.60 |
| Lipid Panel | $ | 72.60 |
| Blood Pressure | $ | - |
| Total: | $ | 138.20 |
HbA1c – hemoglobin A1c, Lipid Panel – consists of total cholesterol, high density lipoprotein (HDL) cholesterol, low density lipoprotein (LDL) cholesterol, triglycerides
Table 3.
Annual Medicare Spending for Acute CVD (2009)21
| Discharges | Total Days of Care | Program Payments | ||||
|---|---|---|---|---|---|---|
| Principal ICD-9-CM Diagnosis Within MDC |
ICD-9-CM Code |
Number | Number | Per Discharge |
Amount in Thousands |
Per Discharge |
| Diseases of the Circulatory System (MDC 7) | 390–459 | 2,773,075 | 13,257,725 | 4.8 | $30,644,608 | $11,112 |
| Heart Disease | 391–392.0, 393–398,402,404, 410–416,420–429 | 1,874,405 | 9,068,280 | 4.8 | 21,917,570 | 11,755 |
| Acute Myocardial Infarction | 410 | 274,970 | 1,491,355 | 5.4 | 3,963,122 | 14,462 |
| Coronary Atherosclerosis | 414.0 | 344,155 | 1,332,890 | 3.9 | 4,790,363 | 14,055 |
| Other Ischemic Heart Disease | 411–413, 414.1–414.9 | 30,845 | 84,405 | 2.7 | 353,239 | 11,578 |
| Cardiac Dysrhythmias | 427 | 408,990 | 1,572,995 | 3.8 | 3,399,280 | 8,345 |
| Congestive Heart Failure | 428.0 | 233,205 | 1,139,875 | 4.9 | 1,998,717 | 8,615 |
| Cerebrovascular Disease | 430–438 | 467,890 | 2,089,015 | 4.5 | 3,956,941 | 8,504 |
Lists aggregated Medicare data for discharge costs for the Major Diagnostic Classification (MDC) of Disease of the Circulatory System (MDC 7) for 2012
Costs Associated with ED
The cost per patient for ED diagnosis and annual treatment was estimated using Medicare reimbursement rates from the UDAOC to be $6,220, reflecting common diagnostic tests, medications, and other treatments used in men with ED (Table 4)28. Although the emergency room (ER), imaging, surgical, and inpatient costs of treating ED in a single man appear low, it is important to note that all men will not receive these interventions and that these costs represent the average across all men with ED. Medication costs for men with ED were calculated assuming a daily regimen of PDE5i, as well as on-demand PDE5i. Additional average costs are included in Table 4.
Table 4.
Cost of ED Treatment44
| Intervention | Cost |
|---|---|
| Medication Total | $4,800.00 |
| Daily PDE5 inhibitor | $2,880.00 |
| On demand PDE5 inhibitor | $1,920.00 |
| Office Visit (average 2 times per man) | $129.89 |
| Duplex Penile U/S | $377.00 |
| Ambulatory Surgery | $82.05 |
| ER | $2.35 |
| Inpatient costs | $141.31 |
| Labs | $687.40 |
| Total: | $6,220.00 |
PDE – phosphodiesterase 5, U/S – ultrasound, ER – emergency room
Calculation of Relevant Parameters
Extracted incidence and prevalence data were used to calculate relevant parameters using the equations in Appendix 1, adjusted for inflation, and extrapolated over a 20-year period in consideration of the lead-time associated with preventive intervention. The number of incident cases of ED in men with CVD was calculated by multiplying the CVD incidence by the incidence of ED in the CVD population. The number of men potentially identified with CVDRFs at presentation for ED was calculated by multiplying the rate of undiagnosed hypertension in the general population as a surrogate for the rate of undiagnosed CVDRFs. To determine the reduction in the number of CV events, we modeled the acute event risk reduction attributable to standard of care pharmacotherapy in managing CVD risk multiplied by the number of men with CVDRFs without prior diagnosis. Costs were calculated by multiplying the average cost per hospitalization for an acute CVD event by the number of events potentially avoided. Costs for the screening protocol were determined by multiplying the sum of the costs of the screening components by the number of men to be screened.
MAIN OUTCOME MEASURES
The primary outcome is a model of the impact of screening men with ED for CVDRFs, as well as an estimate of the effect of treating men with CVDRFs on both the savings associated with such a screening program as well as disease prevalence.
RESULTS
We aimed to determine the cost savings associated with screening men over the age of 20 presenting with ED for cardiovascular risk factors, and treating men in whom risk factors were diagnosed as a result of screening. We identified available data for the costs, prevalence and incidence associated with ED and CVD from the literature. The incidence of CVD was calculated to be 4.83 cases / 1000 men / year29, and the incidence of ED in patients with CVD to be 47.1 cases / 1000 men / year2,9,14,22–26. The relative risk (RR) of CVD in men with ED is estimated at 1.47, as determined in a recent meta-analysis10. CVD affects approximately 8.8 million men in the United States, and approximately 2 million men have both CVD and ED (Table 1).
Table 1.
Factors Determining Annual and 20-Year Projected Costs of ED and CVD
| Variable | Value |
|---|---|
| Total prevalence of CVD | 81.1/1000 |
| Population of men in US (age 20+)29 | 108,384,730 |
| Number of Men with CVD in US | 8,790,002 |
| Number of Men with ED in US2 | 18,000,000 |
| RR of ED with CVD compared to normal population10 | 1.47 |
| Number of men with CVD and ED | 1,991,520 |
CVD – cardiovascular disease, RR – relative risk, ED – erectile dysfunction
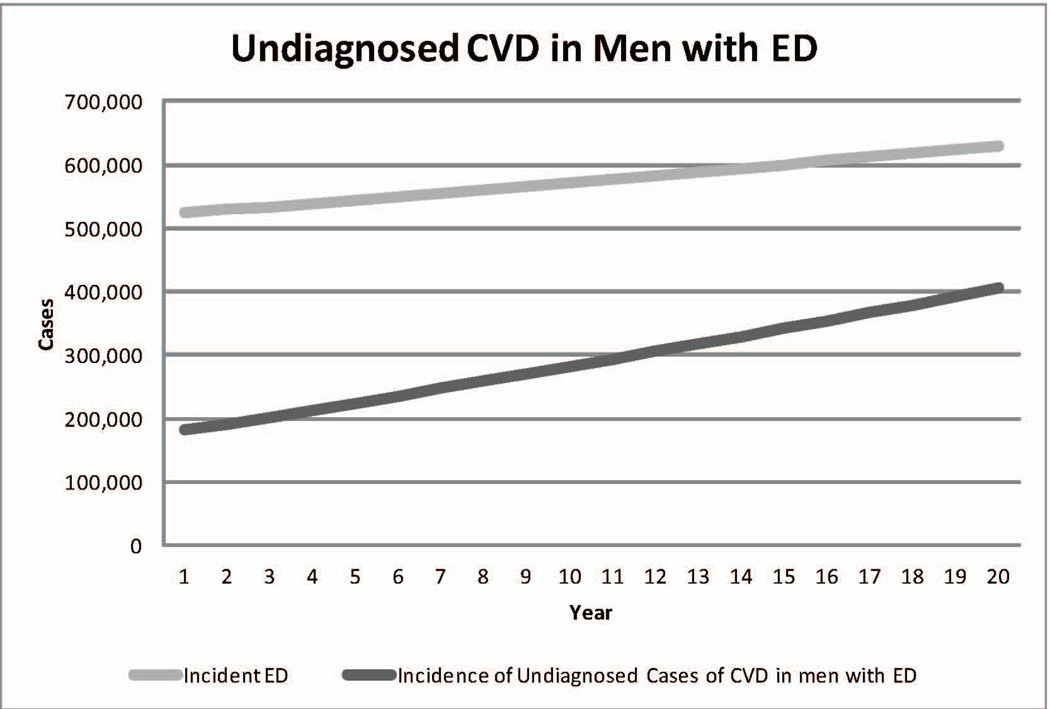
The rates of treatable CVDRFs including hypertension, hyperlipidemia, and diabetes in the general population are well established. However, 43.7% of Americans with hypertension are unaware of the diagnosis30, as are approximately 50% with hyperlipidemia31. We used the fraction of undiagnosed American men with hypertension as a surrogate for the total number of men with treatable, undiagnosed CVDRFs to provide a conservative estimate (Figure 2). We then applied a 5 year risk reduction in acute CV events of 0.19, as derived from studies evaluating statin therapy in men with known CVDRFs32. While combination therapy with aspirin, statin and one or more antihypertensive medications shows greater benefit than statin alone (hazard ratio (HR) 0.66 (95% CI 0.49–0.88)), not all patients are treated with multiple agents, and thus our model reflects a more conservative approach using monotherapy to avoid overestimation of effect size33.
Figure 2. Undiagnosed CVD in Men with ED.
Chart depicting the rise in incidences of ED alone and CVD in men with ED projected over 20 years.
The cost of CVDRF screening in men presenting with ED was estimated to be $138.20 per man, the annual cost per man for the diagnosis and treatment of ED to be $6,220 and the average cost per acute CV event at $11,602, as described in Methods (Table 2). These cost estimates were then used to calculate screening and treatment costs.
Up to 5.8 million men presenting with ED over the next 20 years may have undiagnosed CVDRFs (Table 5). The number of acute CV events that could be avoided by applying the 5-year risk reduction in CV events using statin therapy is approximately 1.1 million over 20 years, averaging 55,000 a year32. Reasoning that improved CV health could result in fewer ED cases requiring treatment, we estimated the number of men in this cohort by applying the same risk reduction resulting from statin therapy to all men with both ED and CVD, resulting in a potential reduction in 1.1 million cases of ED over 20 years. Based on these estimates, only 12 men presenting with ED of any etiology require CV risk factor screening to prevent a single CV event.
Table 5.
Effects of Screening and Treatment on ED and CVD Incidence Over 20 Years
| Variable | Number of Patients |
|---|---|
| Incidence of ED in CVD Population (Number of Men to be Screened) | 13,251,356 |
| Proportion of Men with Silent CVD Risk Factors30 | 0.437 |
| Number of Men Identified with Silent CVD Risk Factors at ED screening | 5,790,843 |
| Number of Acute CVD Events Avoided with Proper Preventative care | 1,100,260 |
| Potential Reduction in Number of Chronic ED Cases | 1,100,260 |
| Number Needed to Screen to Avoid one Acute CVD event | 12.04 |
ED – erectile dysfunction, CVD – cardiovascular disease
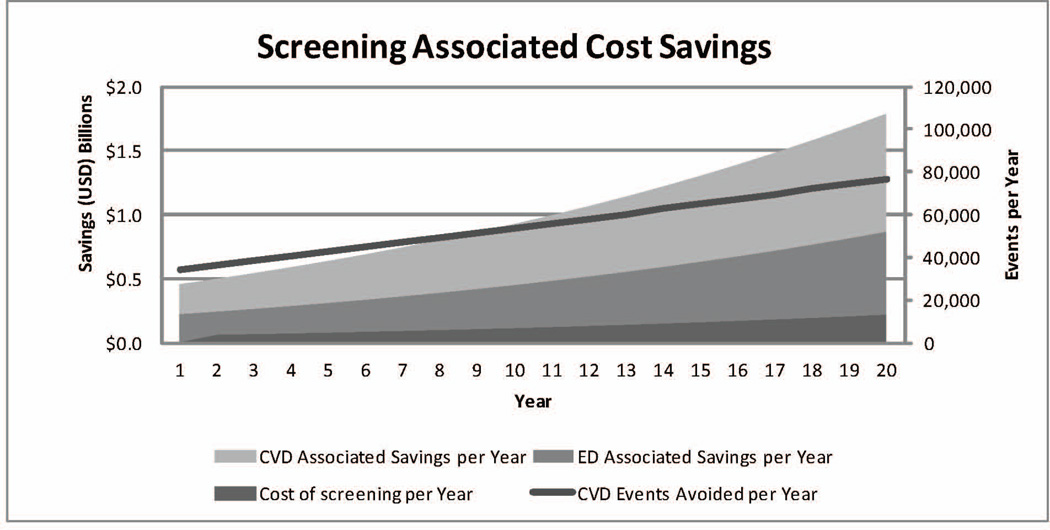
Costs associated with CV risk factor screening and treatment were estimated as described in Methods and are presented in Table 6. Briefly, using a CVDRF screening cost of $138.20 per man, screening over 20 years costs $2.6 billion and can identify 5.8 million men at risk for CVD. If these men were treated with pharmacological preventative care including statin and anti-hypertensive medications, 1.1 million acute CV events could be avoided, saving $20.4 billion in acute CVD treatment expenditures. Less the cost of screening, an estimated net savings of $21.3 billion (Figure 3), with over an eight-fold return on investment on the cost of screening can be realized for acute CV treatment costs alone.
Table 6.
Projected Costs of Screening and Treatment Over 20 Years
| Cost Variable | Cost | |
|---|---|---|
| Cost of CVD Screening for One Man | $ | 138.20 |
| Avg. Cost of Acute CVD Treatment for One Man | $ | 11,602.00 |
| Avg. Cost of ED treatment per Man | $ | 6,220.00 |
| Total Cost of Screening | $ | 2,635,114,372.73 |
| Total Treatment Costs Avoided Through CV Event Reduction | $ | 21,293,421,419.28 |
| Total Treatment Costs Avoided by Reducing ED Incidence | $ | 9,847,292,752.60 |
| Net Savings | $ | 28,505,599,799.15 |
| Return on Screening Investment | 10.8 |
CVD – cardiovascular disease, ED – erectile dysfunction, CV – cardiovascular
Figure 3. Cost Savings Associated with Screening for CVD in Men with ED.
Chart depicting annual cost savings associated with screening for CVD in men with ED extrapolated over 20 years. The gray line estimates the number of CVD events avoided per year. The filled gray regions represent cost savings associated with screening men with ED for CVD and subsequent treatment, either as a function of ED or CVD. Cumulatively, over 1.1 million CV events are avoided with a cumulative savings of over $28.5 billion. Annual screening costs are also indicated and represent a small fraction of the total cost savings.
By screening men presenting with ED for CVD and treating these risk factors, we can model the effects on ED prevalence and associated cost savings. Our model predicts a reduction in 1.1 million cases of ED over 20 years, saving $9.7 billion that would have been spent on ED treatment. This additional savings may be added to $21.3 billion saved in acute CV care to arrive at the net effect of this intervention. The resulting total cost savings to the United States healthcare system over the next 20 years associated with screening for CVD at presentation for ED is estimated at $28.5 billion, a more than 10-fold return on the investment in screening costs.
DISCUSSION
Erectile dysfunction and CVD are considered a common endpoint of the same vascular pathology, and ED is an important predictor of vascular disease. ED can manifest 2–5 years before any coronary events34,35, and 1 in 5 men with new onset ED but without CVD symptoms have significant coronary artery stenosis on angiography7. Given this relatively short window between ED diagnosis and coronary events, it is important that men with undiagnosed CVDRFs are identified early, and men presenting with ED offer such an opportunity35. The proportion of men affected by silent, undiagnosed CVDRFs is significant; 49.6% of adults in the United States with hypercholesterolemia, 43.7% of men with hypertension30, and nearly 30% with type II diabetes36 are unaware of these diagnoses. Failure to identify silent markers of CVD early can have a significant human and financial cost, given that more than 60% of sudden cardiac deaths occur in people with no prior diagnosis of CHD37. Furthermore, given the higher prevalence, underlying pathophysiology, and early presentation of ED in men with CVD, the rates of silent, undiagnosed CVD may be even higher in men with ED.
Evaluation of men with ED for CVD is recommended by the Princeton Consensus Conference given the high risk of morbidity and mortality in this cohort of men20. We estimate that screening men with ED for CVDRFs and treatment of these risk factors could prevent 1.1 million acute CV events, and may reduce the ED burden by a comparable number of cases assuming equivalent treatment efficacy of standard pharmacotherapy. In addition, our cost estimates, already conservative due to the use of averaged ED treatment costs, likely understate the societal value of screening, given that we do not include benefits associated with improved quality of life and avoidance of lost wages due to illness.
Accordingly, screening for CVDRFs at presentation for ED appears to be an important and underutilized intervention point16,35. The financial burden of CVD in the United States is staggering; $127 billion was spent on direct medical costs in 2010 with costs expected to increase to $276 billion by 203038. Lost productivity due to CVD is expected to rise from $172 billion to $276 billion from 2010 to 203038. Hence, prevention of CVD progression is of great societal value. Screening just 12 men presenting with ED and subsequently treating these men can prevent an acute CVD event, and for every dollar spent on screening in this population, $10.80 in direct costs of acute CVD and ED care would be saved. By comparison, one dollar spent on a complete set of childhood vaccinations in the U.S. saves $5 in direct treatment costs39.
Despite the potential impact of our conclusions, there are several limitations of this model that should be discussed. First, our model assumes that the proportion of men with undiagnosed CVDRFs relative to the total number of men with CVDRFs is the same in men with ED as it is in the general population, although there are no data to support this assumption. We feel that this is a reasonable assumption in that ED is often the first manifestation of CVD. Second, given the higher prevalence of CVD in the population of men with ED, with ED representing a later manifestation of uncontrolled CV risk, as well as the known aversion of men with respect to seeking medical and preventive care21, our model likely underestimates the rate of silent CVDRFs. Third, it is important to note that this study does not account for the cost of standard CVD secondary prevention, and these costs are excluded for two reasons: 1) the cost efficacy of the major classes of pharmaceutical prevention have been demonstrated independently40,41 and 2) men with CVDRFs should be treated appropriately regardless of whether they present with ED. Fourth, there are limitations of our calculations of ED rate reductions. Given the underlying pathophysiology of ED and CVD, our model assumes that improving underlying CV health medically can improve ED symptoms, though studies examining the effects of standard pharmacotherapy for CVDRFs have not definitively demonstrated this42,43. Thus, we assumed that the effect of medical therapy on CV events would result in a similar benefit in ED symptoms. Despite the above limitations, it is worth noting that CVD screening at ED presentation is cost-effective independent of whether medical therapy for CVD improves ED symptoms, and should future work demonstrate that medically improving CV health does not improve ED symptoms, the cost savings in acute CVD event reduction would still hold. Our model is also limited in that does not risk stratify by age, but relies on averages across the age range of our population. The choice not to age stratify was based on limited age-specific incidence data, especially for men less than 40 years old. Given rising rates of metabolic disorders in younger age groups, including men <40 years old in our calculations was particularly significant for early CVDRF identification. Finally, while ED may be a motivating factor for many men to see a physician, not every man with ED will seek medical attention. For that reason, the total number of avoided acute events and the total cost savings may be interpreted as a theoretical limit with all at-risk patients presenting for medical care. However, the CVD event risk reduction and cost efficacy for screening for any individual man presenting with ED is not affected by this limitation.
As the link between the etiologies of ED and CVD grows stronger, both the healthcare community and patients stand to benefit from screening for and treating CVD in men with ED. Such an approach could significantly decrease national healthcare costs and disease burden with significant societal implications. Based upon our model, we call for a paradigm shift that moves research and treatment of ED away from merely deriving symptomatic improvement in the disease to a proactive and comprehensive view that appreciates and attempts to reverse the underlying and concurrent vascular pathology.
CONCLUSIONS
Screening men presenting with ED for CVD represents a cost-effective intervention for secondary prevention of both CVD and ED, resulting in substantial cost savings relative to identification of CVD at the time of manifestation, which requires substantially more expensive treatment. As such, the medical practitioner intervening on behalf of a patient’s sexual function is placed in the role of global caretaker.
Supplementary Material
Acknowledgments
Funding: This study has been supported in part by NIH/NCI Career Development Award Grant to Guilherme Godoy (K23CA160664)
REFERENCES
- 1.Saigal CS, et al. Predictors and prevalence of erectile dysfunction in a racially diverse population. Arch. Intern. Med. 2006;166:207–212. doi: 10.1001/archinte.166.2.207. [DOI] [PubMed] [Google Scholar]
- 2.Araujo AB, et al. Does Erectile Dysfunction Contribute to Cardiovascular Disease Risk Prediction Beyond the Framingham Risk Score? J. Am. Coll. Cardiol. 2010;55:350–356. doi: 10.1016/j.jacc.2009.08.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Polinski JM, Kesselheim AS. Where Cost, Medical Necessity, and Morality Meet: Should US Government Insurance Programs Pay for Erectile Dysfunction Drugs? Clin Pharmacol Ther. 2011;89:17–19. doi: 10.1038/clpt.2010.179. [DOI] [PubMed] [Google Scholar]
- 4.Gandaglia G, et al. A systematic review of the association between erectile dysfunction and cardiovascular disease. Eur. Urol. 2014;65:968–978. doi: 10.1016/j.eururo.2013.08.023. [DOI] [PubMed] [Google Scholar]
- 5.Thompson IM, et al. ERectile dysfunction and subsequent cardiovascular disease. JAMA. 2005;294:2996–3002. doi: 10.1001/jama.294.23.2996. [DOI] [PubMed] [Google Scholar]
- 6.Dong J-Y, Zhang Y-H, Qin L-Q. Erectile dysfunction and risk of cardiovascular disease: meta-analysis of prospective cohort studies. J. Am. Coll. Cardiol. 2011;58:1378–1385. doi: 10.1016/j.jacc.2011.06.024. [DOI] [PubMed] [Google Scholar]
- 7.Vlachopoulos C, et al. Prevalence of Asymptomatic Coronary Artery Disease in Men with Vasculogenic Erectile Dysfunction: A Prospective Angiographic Study. Eur. Urol. 2005;48:996–1003. doi: 10.1016/j.eururo.2005.08.002. [DOI] [PubMed] [Google Scholar]
- 8.Chew K-K, et al. Erectile Dysfunction as a Predictor for Subsequent Atherosclerotic Cardiovascular Events: Findings from a Linked-Data Study. J. Sex. Med. 2010;7:192–202. doi: 10.1111/j.1743-6109.2009.01576.x. [DOI] [PubMed] [Google Scholar]
- 9.Batty GD, et al. Erectile Dysfunction and Later Cardiovascular Disease in Men With Type 2 Diabetes: Prospective Cohort Study Based on the ADVANCE (Action in Diabetes and Vascular Disease: Preterax and Diamicron Modified-Release Controlled Evaluation) Trial. J. Am. Coll. Cardiol. 2010;56:1908–1913. doi: 10.1016/j.jacc.2010.04.067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Guo W, et al. Erectile Dysfunction and Risk of Clinical Cardiovascular Events: A Meta-Analysis of Seven Cohort Studies. J. Sex. Med. 2010;7:2805–2816. doi: 10.1111/j.1743-6109.2010.01792.x. [DOI] [PubMed] [Google Scholar]
- 11.Heruti R, Shochat T, Tekes-Manova D, Ashkenazi I, Justo D. Prevalence of erectile dysfunction among young adults: results of a large-scale survey. J. Sex. Med. 2004;1:284–291. doi: 10.1111/j.1743-6109.04041.x. [DOI] [PubMed] [Google Scholar]
- 12.Chen S, et al. Insulin resistance is an independent determinate of ED in young adult men. PloS One. 2013;8:e83951. doi: 10.1371/journal.pone.0083951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rastrelli G, et al. Flaccid Penile Acceleration as a Marker of Cardiovascular Risk in Men without Classical Risk Factors. J. Sex. Med. 2014;11:173–186. doi: 10.1111/jsm.12342. [DOI] [PubMed] [Google Scholar]
- 14.Inman BA, et al. A Population-Based, Longitudinal Study of Erectile Dysfunction and Future Coronary Artery Disease. Mayo Clin. Proc. Mayo Clin. 2009;84:108–113. doi: 10.4065/84.2.108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vlachopoulos CV, Terentes-Printzios DG, Ioakeimidis NK, Aznaouridis KA, Stefanadis CI. Prediction of cardiovascular events and all-cause mortality with erectile dysfunction: a systematic review and meta-analysis of cohort studies. Circ. Cardiovasc. Qual. Outcomes. 2013;6:99–109. doi: 10.1161/CIRCOUTCOMES.112.966903. [DOI] [PubMed] [Google Scholar]
- 16.Nehra A, et al. Diagnosis and Treatment of Erectile Dysfunction for Reduction of Cardiovascular Risk. J. Urol. 2013;189:2031–2038. doi: 10.1016/j.juro.2012.12.107. [DOI] [PubMed] [Google Scholar]
- 17.Gazzaruso C, et al. Erectile Dysfunction as a Predictor of Cardiovascular Events and Death in Diabetic Patients With Angiographically Proven Asymptomatic Coronary Artery Disease: A Potential Protective Role for Statins and 5-Phosphodiesterase Inhibitors. J. Am. Coll. Cardiol. 2008;51:2040–2044. doi: 10.1016/j.jacc.2007.10.069. [DOI] [PubMed] [Google Scholar]
- 18.Corona G, Razzoli E, Forti G, Maggi M. The use of phosphodiesterase 5 inhibitors with concomitant medications. J. Endocrinol. Invest. 2008;31:799–808. doi: 10.1007/BF03349261. [DOI] [PubMed] [Google Scholar]
- 19.Corona G, et al. Phosphodiesterase Type 5 (PDE5) Inhibitors in Erectile Dysfunction: The Proper Drug for the Proper Patient. J. Sex. Med. 2011;8:3418–3432. doi: 10.1111/j.1743-6109.2011.02473.x. [DOI] [PubMed] [Google Scholar]
- 20.Nehra A, et al. The Princeton III Consensus Recommendations for the Management of Erectile Dysfunction and Cardiovascular Disease. Mayo Clin. Proc. Mayo Clin. 2012;87:766–778. doi: 10.1016/j.mayocp.2012.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.American Academy of Family Physicians. Executive Summary Report-Men’s Health Study. 2007 at < http://www.aafp.org/dam/AAFP/documents/media_center/men-prevention/final_executive_summary_061307.pdf>. [Google Scholar]
- 22.Schouten BWV, et al. Erectile dysfunction prospectively associated with cardiovascular disease in the Dutch general population: results from the Krimpen Study. Int J Impot Res. 2007;20:92–99. doi: 10.1038/sj.ijir.3901604. [DOI] [PubMed] [Google Scholar]
- 23.KLONER RA, et al. Erectile Dysfunction in the Cardiac Patient: How Common and Should We Treat? J. Urol. 2003;170:S46–S50. doi: 10.1097/01.ju.0000075055.34506.59. [DOI] [PubMed] [Google Scholar]
- 24.Hall SA, Shackelton R, Rosen RC, Araujo AB. Sexual Activity, Erectile Dysfunction, and Incident Cardiovascular Events. Am. J. Cardiol. 2010;105:192–197. doi: 10.1016/j.amjcard.2009.08.671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Selvin E, Burnett AL, Platz EA. Prevalence and Risk Factors for Erectile Dysfunction in the US. Am. J. Med. 2007;120:151–157. doi: 10.1016/j.amjmed.2006.06.010. [DOI] [PubMed] [Google Scholar]
- 26.Johannes CB, et al. Incidence Of Erectile Dysfunction In Men 40 To 69 Years Old: Longitudinal Results From The Massachusetts Male Aging Study. J. Urol. 2000;163:460–463. [PubMed] [Google Scholar]
- 27.Medicare & Medicaid Statistical Supplement. Table 5.5 (Centers for Medicare & Medicaid Services. 2013 at < https://www.cms.gov/Research-Statistics-Data-and-Systems/Research/MedicareMedicaidStatSupp/2013.html>.
- 28.Litwin M, Saigal C, editors. Urologic Diseases in America. Department of Health and Human Services, Public Health Service, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; 2012. pp. 490–496. [Google Scholar]
- 29.United States Census Bureau. American FactFinder. 2011 at < http://factfinder.census.gov/servlet/STTable?_bm=y&-geo_id=01000US&-qr_name=ACS_2009_1YR_G00_S0101&-ds_name=ACS_2009_1YR_G00_&-_lang=en&-redoLog=false&-state=st&-CONTEXT=st>.
- 30.Vital signs: awareness and treatment of uncontrolled hypertension among adults - United States, 2003–2010. MMWR Morb. Mortal. Wkly. Rep. 2012;61:703–709. [PubMed] [Google Scholar]
- 31.Ford ES, Li C, Pearson WS, Zhao G, Mokdad AH. Trends in hypercholesterolemia, treatment and control among United States adults. Int. J. Cardiol. 2010;140:226–235. doi: 10.1016/j.ijcard.2008.11.033. [DOI] [PubMed] [Google Scholar]
- 32.Cholesterol Treatment Trialists’ Collaborators. Efficacy and safety of cholesterol-lowering treatment: prospective meta-analysis of data from 90?056 participants in 14 randomised trials of statins. The Lancet. 2005;366:1267–1278. doi: 10.1016/S0140-6736(05)67394-1. [DOI] [PubMed] [Google Scholar]
- 33.Lafeber M, et al. The combined use of aspirin, a statin, and blood pressure–lowering agents (polypill components) and the risk of vascular morbidity and mortality in patients with coronary artery disease. Am. Heart J. 2013;166:282.e1–289.e1. doi: 10.1016/j.ahj.2013.04.011. [DOI] [PubMed] [Google Scholar]
- 34.Vlachopoulos C, Jackson G, Stefanadis C, Montorsi P. Erectile dysfunction in the cardiovascular patient. Eur. Heart J. 2013 doi: 10.1093/eurheartj/eht112. [DOI] [PubMed] [Google Scholar]
- 35.Scranton RE, Goldstein I, Stecher VJ. Erectile Dysfunction Diagnosis and Treatment as a Means to Improve Medication Adherence and Optimize Comorbidity Management. J. Sex. Med. 2013;10:551–561. doi: 10.1111/j.1743-6109.2012.02998.x. [DOI] [PubMed] [Google Scholar]
- 36.Centers for Disease Control and Prevention. National diabetes fact sheet: national estimates and general information on diabetes and prediabetes in the United States. US Dep. Health Hum. Serv. 2011 at < http://www.cdc.gov/diabetes/pubs/pdf/ndfs_2011.pdf>.
- 37.Ni H, et al. Trends from 1987 to 2004 in sudden death due to coronary heart disease: The Atherosclerosis Risk in Communities (ARIC) study. Am. Heart J. 2009;157:46–52. doi: 10.1016/j.ahj.2008.08.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Heidenreich PA, et al. Forecasting the Future of Cardiovascular Disease in the United States: A Policy Statement From the American Heart Association. Circulation. 2011;123:933–944. doi: 10.1161/CIR.0b013e31820a55f5. [DOI] [PubMed] [Google Scholar]
- 39.Zhou F, Santoli J, Messonnier ML, et al. EConomic evaluation of the 7-vaccine routine childhood immunization schedule in the united states, 2001. Arch. Pediatr. Adolesc. Med. 2005;159:1136–1144. doi: 10.1001/archpedi.159.12.1136. [DOI] [PubMed] [Google Scholar]
- 40.Pignone M, Earnshaw S, Tice JA, Pletcher MJ. Aspirin, Statins, or Both Drugs for the Primary Prevention of Coronary Heart Disease Events in Men: A Cost–Utility Analysis. Ann. Intern. Med. 2006;144:326–336. doi: 10.7326/0003-4819-144-5-200603070-00007. [DOI] [PubMed] [Google Scholar]
- 41.Choudhry NK, Avorn J, Antman EM, Schneeweiss S, Shrank WH. Should Patients Receive Secondary Prevention Medications For Free After A Myocardial Infarction? An Economic Analysis. Health Aff. (Millwood) 2007;26:186–194. doi: 10.1377/hlthaff.26.1.186. [DOI] [PubMed] [Google Scholar]
- 42.Miner M, et al. Prognostic utility of erectile dysfunction for cardiovascular disease in younger men and those with diabetes. Am. Heart J. 2012;164:21–28. doi: 10.1016/j.ahj.2012.04.006. [DOI] [PubMed] [Google Scholar]
- 43.Trivedi D, et al. Can simvastatin improve erectile function and health-related quality of life in men aged ≥40 years with erectile dysfunction? Results of the Erectile Dysfunction and Statins Trial [ISRCTN66772971] BJU Int. 2013;111:324–333. doi: 10.1111/j.1464-410X.2012.11241.x. [DOI] [PubMed] [Google Scholar]
- 44.Urologic Diseases in America Online Compendium. National Institute of Diabetes and Digestive and Kidney Diseases; 2012. at < http://udaonline.net/>. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.