Abstract
Objective
To identify population subgroups under-vaccinated for influenza through classification tree analysis to inform interventions aimed at improving future vaccine uptake.
Method
A cross-sectional community health needs assessment was conducted from 09/2012 through 11/2012 among randomly selected households in six low-income neighborhoods in New Haven, CT (N=1300 adults, aged 18-65). Known correlates of influenza vaccine uptake plus experience of medical mistreatment were used to develop a classification tree to identify under-vaccinated population subgroups
Results
Forty-five percent of respondents reported receiving the influenza vaccine. The classification tree identified healthy adults and uninsured adults at increased risk of influenzacomplications as subgroups with low vaccine uptake (40% and 30%, respectively). The subgroup representing insured, high-risk adults who reported experience of medical mistreatment had moderate vaccine uptake (45%). Sensitivity of the classification tree was high (83%, 95% CI= 80% to 86%), indicating a strong true positive rate using these subgroups.
Conclusion
Results highlight the need for renewed attention to promoting the influenza vaccination recommendation for all adults, particularly among healthy adults, uninsured, high-risk adults and insured, high-risk adults who have experienced medical mistreatment. Further research is needed to better understand how to reach these population subgroups.
Introduction
In the wake of the 2009-H1N1 pandemic, the Centers for Disease Control and Prevention (CDC) recommended that everyone older than 6 months receive the seasonal influenza vaccine annually.1 During the 2012-2013 moderately severe influenza season, the CDC estimated that the influenza vaccine prevented 6.6 million illnesses and 79,260 hospitalizations.2 Despite burden of illness, hospitalization and mortality associated with seasonal influenza and preventive benefits of the influenza vaccine,2,3 only 42% of U.S. adults (≥18 years) reported getting vaccinated during the 2012-2013 season.4 Understanding factors associated with vaccine uptake, and how they interact with each other, can inform interventions to increase vaccine coverage.
Several studies conducted during the 2009-2010 influenza season among adults documented that influenza vaccine uptake increased with age,5–7 and White Americans were more likely than Latino and Black Americans to be vaccinated.5,8 Being female,5,7 U.S. nativity,6 and having higher income5 and health insurance5 were also associated with uptake. Beyond sociodemographics, one study found that negative health behaviors (consuming fewer than 5 servings of fruits and vegetables daily, no physical activity, and smoking) and obesity were associated with lower vaccine uptake, and people reporting poor health status and prior diagnoses of chronic disease were more likely to be vaccinated compared to healthy adults.5 Although not directly related to vaccine uptake, other research suggests that when individuals feel they have been discriminated against or treated unfairly by a medical professional, they are less likely to utilize healthcare services.9–12
CDC reports since the universal recommendation show that age, racial/ethnic and gender disparities persist in vaccine uptake.4 During the 2012/2013 season, 58% of adults were unvaccinated against seasonal influenza, with rates even higher among 18-64 year-olds (64%), Black (64%) and Latino adults (66%), and men (62%).4 Since the universal recommendation, no studies have explored how factors associated with lack of vaccine uptake interact with each other to identify more specific under-vaccinated population subgroups, nor have they examined the impact of medical mistreatment, which may contribute to limited vaccine uptake.
This study addresses these gaps by using classification tree analysis, a decision tree methodology with useful applications to and increasingly used in public health studies to test complex interactions between factors known or hypothesized to be associated with health and health behaviors.13–16 This study's objective is to develop a classification tree to identify under-vaccinated subgroups among a sample of predominantly Black and/or Latino adults, aged 18-65, from low-income neighborhoods in New Haven, CT, representing an underserved population with increased health risk and low influenza vaccine coverage. Results may inform future intervention efforts to reduce disparities in and increase vaccine uptake.
Methods
A randomized, cross-sectional health needs assessment was conducted from 09/2012 through 11/2012 among adults aged 18-65 in six low-income neighborhoods (i.e., 35% of general population living below federal poverty level and median family income 41% and 38% of the metropolitan area and state median, respectively17). Households were randomly selected from a complete list of residential addresses provided by the City of New Haven. Each was approached a maximum of three times or until an eligible resident answered the door and agreed or refused to participate. Of 3,983 households randomized, 16% of addresses were ineligible (e.g., businesses), 35% did not answer or were not accessible, 12% refused participation, and 4% were ineligible due to age or language. An eligible resident was reached within three attempts for 1,788 households, and 73% of these (N=1300) agreed to participate. Surveys were administered in English or Spanish by trained interviewers who resided in the neighborhoods under study. Responses were entered into hand-held computers. Participants received a $10 grocery store voucher and were entered into a $500 raffle. Participants provided informed consent, and all procedures were approved by Yale University's Institutional Review Board.
Measures
Vaccination Status
Influenza vaccine uptake was assessed using the question, “During the past 12 months, have you had either a seasonal flu shot or a seasonal flu vaccine that was sprayed in your nose?” Responses were grouped into four categories: Yes, No, Don't know/Not sure, and Refused.18 Participants who responded Don't know/Not sure (N=13) or Refused (N=102) were excluded from analyses. Seven more respondents were excluded because they skipped this question; therefore the analytic sample included 1,178 participants. Compared to the analytic sample, excluded respondents were more likely to be healthy weight (38% vs 26%) and uninsured (21% vs 11%), but no other differences were observed.
Socio-Demographics
Participants reported age, race/ethnicity, sex, income, and U.S. nativity.
Health Status
Participants were asked to rate their overall health as excellent, very good, good, fair or poor.19 Participants who reported one or more chronic disease that increases risk for flu-related complications (i.e. asthma, chronic obstructive pulmonary disease, heart disease or heart attack, cancer, diabetes, and/or morbid obesity) were classified as high-risk.20 Body Mass Index (BMI= kg/m2) was calculated from self-reported weight and height,21 and BMI risk category was determined using CDC guidelines.22
Health Behaviors
Participants reported fruit and vegetable intake by number of days/week and number of servings/day to calculate average daily intake.23 Participants reporting zero minutes of moderate and vigorous physical activity were coded as being sedentary.24 Smoking status was assessed by the question “Do you currently smoke cigarettes every day, some days, or not at all?”18 Smokers included participants who reported smoking every day or some days.
Health Care Measures
To measure insurance status, participants were asked, “Do you have health insurance?” Response choices included: Yes, I have health insurance, Medicare, or Medicaid (Title 19); No, I do not have it now, but I used to have health insurance; and I have never had health insurance. The last two items were coded as “No” to create a dichotomous yes/no variable. As further measures of access to and utilization of care, two questions asked: “Do you have one person or place you think of as your personal doctor or health care provider?” and “Have you seen a doctor or other health care provider in the past 12 months for health advice or treatment?” (no/yes).18 Experience of medical mistreatment was measured by the question, “How often have you felt that a doctor or medical staff that you saw judged you unfairly or treated you with disrespect?”25 Response choices included Never, Almost never, Sometimes, Fairly often, and Very often to capture a range of frequencies.
Statistical Analyses
Frequencies and percentages on outcome and independent variables were calculated for descriptive purposes. Bivariate associations of sample characteristics with seasonal influenza vaccination were tested using Pearson's χ2 statistic and t-tests. Descriptive and bivariate analyses were conducted using SAS v9.3 (Cary, NC). To test independent and interactive associations of independent variables with influenza vaccine uptake, a classification tree analysis was conducted.13,26,27,28
Classification tree analysis offers several benefits over logistic regression.13,26–28 It is a non-parametric method, so assumptions (such as linearity) do not have to be met. Second, classification tree analysis allows for testing complex interactions (e.g., 3-way and 4-way interactions) that are difficult to interpret and test in logistic regression, where small cell sizes often make estimates unreliable. Third, observations with missing data can be included in the analysis. Finally, results lead to a decision tree that is easy to interpret and clearly identifies population subgroups to be targeted for intervention.
Classification tree analysis involves an algorithm used to split the parent node, consisting of the entire sample. The algorithm examines a set of candidate splitting variables to find the variable and its optimal cut point that results in the most homogeneous descendent nodes with respect to the outcome variable. The process is recursively applied to all descendent nodes until no significant improvement in the homogeneity of the nodes can be gained or a minimum cell size is reached. Nodes that cannot be split are called terminal nodes and represent the population subgroups. This analysis was conducted in R29 using the R package, rpart30 which uses the CART algorithm and the Gini Index and altered priors for its splitting rule. Minimum node size was specified as 30 observations (2.5% of the total sample),13 and 0.001 was the lower limit for the complexity parameter, a measure of how much each node improves the relative error of the tree. To validate the resulting data-driven classification tree, a 10-fold cross-validation method was used.28 This method divides the sample into 10 equal subsamples. Nine of the subsamples are used to create a learning tree, and the resulting tree is tested with the remaining subsample and a misclassification rate is calculated. This procedure is repeated until all of the subsamples have been used to test a learning tree and an average of the 10 misclassification rates is calculated. A cross-validated misclassification rate similar to the misclassification rate of the tree based upon the entire sample indicates that the resulting classification tree is stable and generalizable. Resulting classification trees can be large and often over-fit the data so the pruned tree associated with the complexity parameter with the minimum cross-validated misclassification error was selected as the final tree.
To assess the utility of the final classification tree, sensitivity [true positives / (true positives + false negatives)] and specificity [true negatives / (true negatives + false positives)] of the classification tree were calculated, along with 95% confidence intervals using SAS v9.3 (Cary, NC). Sensitivity represents the ability of the tree to correctly classify those who were unvaccinated into subgroups needing intervention. Specificity measures its ability to correctly classify people who were vaccinated into subgroups not in need of intervention.
Results
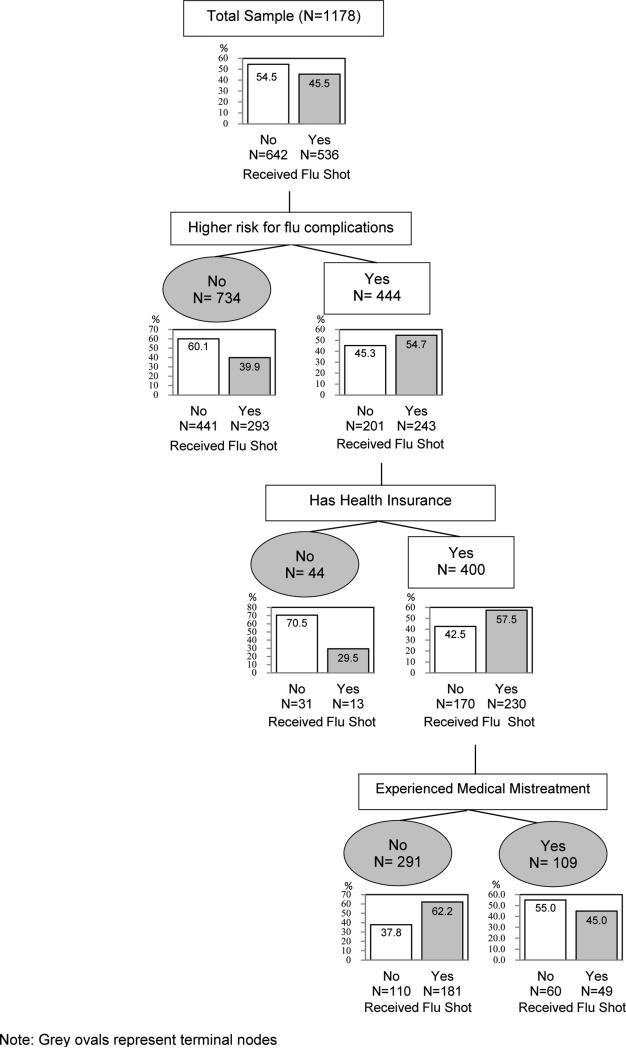
Sample characteristics and bivariate associations with vaccine uptake are in Table 1. Figure 1 shows results of the pruned classification tree analysis, which has 3 splits and 4 terminal nodes. The splitting variables are displayed above descendent nodes, and within each node, the total number of respondents classified into that node is shown. The bar graphs below each node show the proportion of people within nodes who were and were not vaccinated.
Table 1.
Sample Characteristics Overall and by Seasonal Influenza Vaccination Uptakea
| Received Vaccine | |||||
|---|---|---|---|---|---|
| Overallb n (column%) | No n (row %) | Yes n (row %) | χ2 p-value | ||
| Total Sample (N=1178) | 1178 (100%) | 642 (54.5) | 536 (45.5) | ||
| Socio-Demographics | Agec | 40.4 (13.4) | 39.7 (12.9) | 41.2 (13.9) | 0.060 |
| Race/Ethnicity | 0.041 | ||||
| Black | 727 (62.1) | 406 (55.9) | 321 (44.2) | ||
| Hispanic | 239 (20.4) | 114 (47.7) | 125 (52.3) | ||
| White | 114 (9.7) | 60 (52.6) | 54 (47.4) | ||
| Other | 91 (7.8) | 58 (63.7) | 33 (36.3) | ||
| Sex | <0.001 | ||||
| Male | 420 (35.7) | 257 (61.2) | 163 (38.8) | ||
| Female | 756 (64.3) | 384 (50.8) | 372 (49.2) | ||
| Income | 0.305 | ||||
| <$15,000 | 380 (34.7) | 211 (55.5) | 169 (44.5) | ||
| $15,000-$30,000 | 304 (27.8) | 176 (57.9) | 128 (42.1) | ||
| $30,000-$50,000 | 217 (19.8) | 108 (49.8) | 109 (50.2) | ||
| >$50,000 | 193 (17.6) | 103 (53.4) | 90 (46.6) | ||
| U.S. Nativity | 0.104 | ||||
| Yes | 1073 (91.2) | 577 (53.8) | 496 (46.2) | ||
| No | 103 (8.8) | 64 (62.1) | 39 (37.9) | ||
| Health Status | Self-Rated Health | 0.692 | |||
| Excellent | 177 (15.1) | 99 (55.9) | 78 (44.1) | ||
| Very Good | 292 (24.8) | 163 (55.8) | 129 (44.2) | ||
| Good | 393 (33.4) | 214 (54.5) | 179 (45.6) | ||
| Fair | 259 (22.0) | 139 (53.7) | 120 (46.3) | ||
| Poor | 55 (4.7) | 25 (45.5) | 30 (54.6) | ||
| High-risk for flu-related complicationsd | <0.001 | ||||
| Yes | 443 (37.6) | 201 (45.4) | 242 (54.2) | ||
| No | 734 (62.4) | 441 (60.1) | 293 (39.9) | ||
| BMI Risk | 0.081 | ||||
| Underweight (BMI<18.5) | 48 (4.6) | 31 (64.6) | 17 (35.4) | ||
| Healthy Weight (18.5≤BMI<25) | 264 (25.5) | 153 (58.0) | 111 (42.1) | ||
| Overweight (25.≤BMI<30) | 267 (25.8) | 152 (56.9) | 115 (43.1) | ||
| Obese (BMI≥30) | 457 (44.1) | 231 (50.6) | 226 (49.5) | ||
| Health Behaviors | Eats 5 fruits & vegetables/day | 0.170 | |||
| Yes | 217 (18.5) | 109 (50.2) | 108 (49.8) | ||
| No | 959 (81.6) | 531 (55.4) | 428 (44.6) | ||
| Physical Activity | 0.725 | ||||
| No physical activity | 291 (25.1) | 162 (55.7) | 129 (44.3) | ||
| >0 minutes/day | 870 (74.9) | 474 (54.5) | 396 (45.5) | ||
| Smoking Status | 0.187 | ||||
| Smoker | 346 (29.4) | 199 (57.5) | 147 (42.5) | ||
| Non-smoker | 831 (70.6) | 443 (53.3) | 388 (46.7) | ||
| Health Care | Insurance Status | <0.001 | |||
| Has Health Insurance | 1041 (88.9) | 543 (52.2) | 498 (47.8) | ||
| Uninsured | 130 (11.1) | 94 (72.3) | 36 (27.7) | ||
| Has a Usual Source of Care | <0.001 | ||||
| Yes | 1075 (91.6) | 563 (52.4) | 512 (47.6) | ||
| No | 99 (8.4) | 76 (76.8) | 23 (23.2) | ||
| Has seen a doctor in past year | <0.001 | ||||
| Yes | 907 (77.1) | 459 (50.6) | 448 (49.4) | ||
| No | 270 (22.9) | 182 (67.4) | 88 (32.6) | ||
| Freq. of Medical Mistreatment | 0.337 | ||||
| Never | 924 (78.8) | 488 (52.8) | 436 (47.2) | ||
| Almost never | 103 (8.8) | 64 (62.1) | 39 (37.9) | ||
| Sometimes | 102 (8.7) | 59 (57.8) | 43 (42.2) | ||
| Fairly often | 25 (2.1) | 15(60.0) | 10 (40.0) | ||
| Very often | 18 (1.5) | 11 (61.1) | 7 (38.9) | ||
Study conducted in New Haven, CT, Fall 2012
Numbers may not sum to total (N=1178) due to missing data
Age is a continuous variable so numbers represent means and standard deviations and p-value is from t-test
Self-report of asthma, chronic obstructive pulmonary disease, heart disease or heart attack, cancer, diabetes, and/or morbid obesity
Figure 1.
Classification tree identifying population subgroups and their influenza vaccine uptake, Fall 2012, New Haven, CT
Overall, 45.5% of respondents (95% CI, 42 to 49%) reported uptake of the seasonal influenza vaccine. Vaccine uptakes within each terminal node that were below, within and above the confidence interval were classified as low, moderate and high, respectively.14 Based upon the Gini Index, the CART algorithm identified each of our access to care measures (health insurance, usual source of care, and visit to a medical practitioner in the past year) as strong candidates for primary splitting variables, but the high/low health risk variable yielded the most homogeneous descendent nodes and was the first splitting variable. The terminal node representing respondents reporting no high-risk conditions was classified as having low vaccine uptake, with only 39.9% of respondents reporting uptake. High-risk respondents who were uninsured were classified into a terminal node with low vaccine uptake, in which 29.5% of respondents were vaccinated. The final split was among the node representing high-risk respondents with health insurance, which was further split according to report of never versus ever being medically mistreated. Vaccination uptake was high (59.0%) among the high-risk and insured patients reporting never experiencing medical mistreatment, compared to the moderate uptake (43.2%) among those who had experienced medical mistreatment. The misclassification rate for the entire sample was similar to the cross-validated misclassification rate (39.5% vs 41.4%, respectively), suggesting the resulting tree is stable and generalizable.
For the sensitivity and specificity analysis, we assumed that we would target the subgroups with low and moderate but not high influenza vaccine uptake. . Table 2 compares the low/moderate versus high uptake subgroups to whether or not respondents actually reported receiving the vaccine. Sensitivity was calculated to be 83% (95% CI= 80% to 86%), meaning 83% of respondents who reported being unvaccinated were correctly identified as in need of a targeted intervention by the classification tree. Specificity was calculated to be 34% (95% CI = 30% to 38%), indicating only 34% who reported vaccine uptake were correctly identified as not in need of intervention.
Table 2.
Sensitivity and specificity of the classification tree (N=1173a)
| Classified Condition | In subgroup with low or moderate vs. high uptake? | True Condition | ||
| Received Influenza Vaccine? | ||||
| Did not report influenza vaccination | Reported influenza vaccination | |||
| Low/moderate uptake | 532 (true positives) | 354 (false positives) | ||
| High uptake | 108 (false negatives) | 179 (true negatives) | ||
| Sensitivity = 532 / (532 +108) = 83% | Specificity = 354 / (354 + 179) = 34% | |||
Five subjects with missing data on health-risk, insurance status, or medical mistreatment are not included in this analysis; Study conducted in New Haven, CT, Fall 2012
Discussion
The classification tree identified two subgroups with low vaccine uptake; healthy adults and uninsured individuals with high-risk health conditions. Insured individuals reporting high-risk conditions and experience of medical mistreatment were classified into a subgroup with moderate vaccine uptake. High vaccine uptake was observed among the subgroup representing insured, high-risk individuals who never experienced medical mistreatment.
Vaccine uptake was lower among people reporting no high-risk conditions (39.9%) compared to those at risk (45.3%), consistent with other research.5,31,32 Although barriers to vaccination were not assessed, results from classification tree and bivariate analyses suggest that lack of access to health care is an important barrier to vaccination uptake since being uninsured, not having a usual source of care and not seeing a medical practitioner in the past year were significantly associated with lower vaccine uptake. Aside from access, lack of awareness about the recently expanded recommendation for influenza vaccination could be a factor in low vaccine uptake among healthy adults. A study measuring awareness of the CDC's near universal vaccination recommendation showed that only one-half of U.S. adults were aware that they were recommended for influenza vaccination, and awareness was especially low among newly recommended healthy adults.33 Moreover, healthy individuals may perceive the risk associated with influenza to be low, a perception that health behavior theories and empirical studies suggest is a barrier to influenza vaccination uptake.34,35 More research is needed to further classify this subgroup into more useful subgroups and to understand barriers to vaccination uptake among individuals with no risk conditions.
Among the high-risk group, being uninsured was associated with lower likelihood of vaccination, with only 29.5% of high-risk, uninsured respondents reporting vaccination compared to 57.5% of their insured peers. Previous research has demonstrated similar independent associations of chronic disease diagnosis5,31,32 and health insurance coverage5,36,37 with influenza vaccination. This study demonstrates how these factors interact with each other, with lack of insurance being an important barrier to influenza vaccine uptake among high-risk adults. These findings also suggest that increasing access is not sufficient to substantially increase vaccine coverage because many (42.5%) insured, high-risk adults were not vaccinated.
Perceived medical mistreatment further limited influenza vaccine uptake among this group of high-risk, insured individuals, with vaccination coverage at 45.0% among those reporting experience of medical mistreatment versus 62.2% among those reporting no such experience. Like previous research, this finding suggests that being discriminated or mistreated by a medical professional reduces the likelihood of utilizing healthcare.9–11 The impact of individuals’ experiences with medical mistreatment on healthcare utilization may be heightened in communities that have experienced a long history of mistreatment by the medical system,12 such as low-income communities and communities of color, that are represented in this study. Interestingly, the best split for the medical mistreatment variable was determined to be between never and any frequency of mistreatment, suggesting that, as with other health outcomes,38 even infrequent experiences of mistreatment matter for influenza vaccination uptake.
The observed 45.5% vaccination coverage in this study is higher than national and state rates of 33% and 36%, respectively among adults aged 18-64 during the 2011-2012 influenza season.31 This may be due to over-representation of women, older adults and people at high risk compared to the general population, groups that are all associated with higher rates of vaccination.5–7,31 Another possibility is that those who were excluded because of refusing to respond or not knowing actually did not get vaccinated, which would have decreased the percentage of the sample that got vaccinated. Black adults, but not Latino adults, were less likely to be to be vaccinated compared to White adults. This differs from national trends but is more consistent with trends in Connecticut where influenza vaccine coverage is similar among White (48%) and Latino (46%) adults, and comparatively lower among Black adults (37%).31
This study has limitations. As with all cross-sectional studies, our results suggest associations and not causal relationships. Our study sample was drawn from a predominantly low-income, Black and Latino urban population and was over-represented by females, older adults and those with high-risk conditions compared to the wider population, so generalizability of these results has yet to be determined. The low response rate to our survey further limits the generalizability of our results. Also, our measures were based upon self-report which could introduce respondent bias. Self-report of influenza vaccination has been shown to have high sensitivity, but low specificity due to the annual administration of the vaccine,39 and our measure of chronic disease captures only diagnosed cases. To reduce participant burden, survey items were relatively short (e.g., medical mistreatment was measured with a single item); nonetheless, we did use established measures. Future research should include more detailed assessments and include medical record reviews for objective health indicators and outcomes. Our classification tree had high sensitivity though low specificity, resulting in a high misclassification rate. However, for purposes of targeting effective interventions to increase influenza vaccine uptake, sensitivity is more important than specificity because it would be worse to miss those in need of intervention (i.e. people who do not get an influenza vaccine) than to accidentally target people who already get an influenza vaccine. The low specificity of our classification tree might lower the overall accuracy of our model, but given the greater importance of specificity, it doesn't adversely affect the utility of our model.
Conclusion
Results highlight the need for renewed attention to promoting and implementing CDC's influenza vaccination recommendation for all adults. Access to care remains an important factor for vaccination uptake so ways to provide free or low-cost influenza vaccinations are needed for individuals without health insurance, particularly for those at high-risk, until barriers to access are fully removed. Training to enhance sensitivity and eliminate bias among healthcare practitioners may result in better uptake of influenza vaccine among high-risk insured individuals, and further research is needed to understand which attributes are the basis for perceived medical mistreatment associated with lack of influenza vaccine uptake. The importance of provider recommendations, one of the strongest predictors for influenza vaccination,40 should be emphasized among healthcare practitioners and reinforced with provider incentives, such as higher reimbursement rates for the cost of administering the vaccine.41 Approaches to increasing influenza vaccine uptake must be multi-pronged since provider recommendations will not reach people without access to care and are less likely to be followed by people who are mistrustful of their provider.
Highlights.
A classification tree identified subgroups under-vaccinated for influenza
Healthy adults and uninsured, high-risk adults had low vaccine uptake
Among insured, high-risk adults, medical mistreatment was a factor that limited uptake
Renewed attention to promoting the influenza vaccination is needed
Acknowledgments
Funding for this study came from the Patrick and Catherine Weldon Donaghue Medical Research Foundation, the Kresge Foundation, Emerging and Promising Practices, Yale-New Haven Hospital System, and National Institute of Mental Health (T32MH020031). Research was conducted in affiliation with Community Interventions for Health, Oxford Health Alliance, Oxford, England.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest Statement
The authors declare that there are no conflicts of interest.
References
- 1.Center's for Disease Control and Prevention OW [2014 Jun 30];CDC Newsroom Press Release February 24, 2010 [Internet] Available from: http://www.cdc.gov/media/pressrel/2010/r100224.htm.
- 2.Centers for Disease Control and Prevention (CDC) Estimated influenza illnesses and hospitalizations averted by influenza vaccination - United States, 2012-13 influenza season. MMWR Morb Mortal Wkly Rep. 2013 Dec 13;62(49):997–1000. [PMC free article] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention (CDC) Estimates of deaths associated with seasonal influenza --- United States, 1976-2007. MMWR Morb Mortal Wkly Rep. 2010 Aug 27;59(33):1057–62. [PubMed] [Google Scholar]
- 4. [2014 Jul 1];CDC - Flu Vaccination Coverage, United States, 2012-13 Influenza Season | FluVaxView | Seasonal Influenza (Flu) [Internet] Available from: http://www.cdc.gov/flu/fluvaxview/coverage-1213estimates.htm#vaccine.
- 5.Takayama M, Wetmore CM, Mokdad AH. Characteristics associated with the uptake of influenza vaccination among adults in the United States. Prev Med. 2012 May;54(5):358–62. doi: 10.1016/j.ypmed.2012.03.008. doi: 10.1016/j.ypmed.2012.03.008. [DOI] [PubMed] [Google Scholar]
- 6.Vlahov D, Bond KT, Jones KC, Ompad DC. Factors associated with differential uptake of seasonal influenza immunizations among underserved communities during the 2009-2010 influenza season. J Community Health. 2012 Apr;37(2):282–7. doi: 10.1007/s10900-011-9443-x. doi: 10.1007/s10900-011-9443-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Galarce EM, Minsky S, Viswanath K. Socioeconomic status, demographics, beliefs and A(H1N1) vaccine uptake in the United States. Vaccine. 2011 Jul 18;29(32):5284–9. doi: 10.1016/j.vaccine.2011.05.014. doi: 101016/j.vaccine.2011.05.014. [DOI] [PubMed] [Google Scholar]
- 8.Uscher-Pines L, Maurer J, Harris KM. Racial and Ethnic Disparities in Uptake and Location of Vaccination for 2009-H1N1 and Seasonal Influenza. Am J Public Health. 2011 Jul;101(7):1252–5. doi: 10.2105/AJPH.2011.300133. doi: 10.2105/AJPH.2011.300133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Earnshaw VA, Quinn DM. The impact of stigma in healthcare on people living with chronic illnesses. J Health Psychol. 2012 Mar;17(2):157–68. doi: 10.1177/1359105311414952. doi: 101177/1359105311414952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kinsler JJ, Wong MD, Sayles JN, Davis C, Cunningham WE. The effect of perceived stigma from a health care provider on access to care among a low-income HIV-positive population. AIDS Patient Care STDs. 2007 Aug;21(8):584–92. doi: 10.1089/apc.2006.0202. doi:10.1089/apc.2006.0202. [DOI] [PubMed] [Google Scholar]
- 11.Smedley BD, Stith AY, Nelson AR, Institute of Medicine (U.S.) Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care. Unequal treatment : confronting racial and ethnic disparities in health care. National Academy Press; Washington, D.C.: 2003. [PubMed] [Google Scholar]
- 12.Washington HA. Medical apartheid: the dark history of medical experimentation on Black Americans from colonial times to the present. 1st ed. Doubleday; New York: 2006. p. 501. [Google Scholar]
- 13.Lemon SC, Roy J, Clark MA, Friedmann PD, Rakowski W. Classification and regression tree analysis in public health: methodological review and comparison with logistic regression. Ann Behav Med Publ Soc Behav Med. 2003 Dec;26(3):172–81. doi: 10.1207/S15324796ABM2603_02. doi: 101207/S15324796ABM2603_02. [DOI] [PubMed] [Google Scholar]
- 14.Kershaw TS, Lewis J, Westdahl C, Wang YF, Rising SS, Massey Z, et al. Using clinical classification trees to identify individuals at risk of STDs during pregnancy. Perspect Sex Reprod Health. 2007 Sep;39(3):141–8. doi: 10.1363/3914107. doi: 10.1363/3914107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kajungu DK, Selemani M, Masanja I, Baraka A, Njozi M, Khatib R, et al. Using classification tree modelling to investigate drug prescription practices at health facilities in rural Tanzania. Malar J. 2012 Sep 5;11(1):311. doi: 10.1186/1475-2875-11-311. doi:10.1186/1475-2875-11-311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gass K, Klein M, Chang HH, Flanders WD, Strickland MJ. Classification and regression trees for epidemiologic research: an air pollution example. Environ Health. 2014 Mar 13;13(1):17. doi: 10.1186/1476-069X-13-17. doi:10.1186/1476-069X-13-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Social Explorer Tables . ACS 2008 to 2012 (5-Year Estimates) (SE) [Internet]. ACS 2008 to 2012 (5-Year Estemates) Social Explorer, U.S. Census Bureau; Available from. [Google Scholar]
- 18. [2014 Jul 1];CDC - BRFSS Questionnaires [Internet] Available from: http://www.cdc.gov/brfss/questionnaires.htm.
- 19.Idler EL, Benyamini Y. Self-rated health and mortality: a review of twenty-seven community studies. J Health Soc Behav. 1997 Mar;38(1):21–37. doi: 10.2307/2955359. [PubMed] [Google Scholar]
- 20. [2014 Jul 2];People at High Risk of Developing Flu–Related Complications | Seasonal Influenza (Flu) [Internet] Available from: http://www.cdc.gov/flu/about/disease/high_risk.htm.
- 21. [2014 Jul 2];NHANES - NHANES 2011-2012 - Questionnaires [Internet] Available from: http://www.cdc.gov/nchs/nhanes/nhanes2011-2012/questionnaires11_12.htm.
- 22.Healthy Weight [2014 Jul 2];Assessing Your Weight: BMI: About Adult BMI | DNPAO | CDC [Internet] Available from: http://www.cdc.gov/healthyweight/assessing/bmi/adult_bmi/index.html?s_cid=tw_ob064.
- 23.Duffany KO, Finegood DT, Matthews D, McKee M, Venkat Narayan KM, Puska P, et al. Community Interventions for Health (CIH): A novel approach to tackling the worldwide epidemic of chronic diseases. CVD Prev Control. 2011 Jun;6(2):47–56. doi:10.1016/j.cvdpc.2011.02.005. [Google Scholar]
- 24.Craig CL, Marshall AL, Sjöström M, Bauman AE, Booth ML, Ainsworth BE, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003 Aug;35(8):1381–95. doi: 10.1249/01.MSS.0000078924.61453.FB. doi: 10.1249/01.MSS.0000078924.61453.FB. [DOI] [PubMed] [Google Scholar]
- 25.Blanchard J, Nayar S, Lurie N. Patient–Provider and Patient–Staff Racial Concordance and Perceptions of Mistreatment in the Health Care Setting. J Gen Intern Med. 2007 Jul 5;22(8):1184–9. doi: 10.1007/s11606-007-0210-8. doi: 10.1007/s11606-007-0210-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zhang H. Recursive partitioning and applications. 2nd ed. Springer; New York: 2010. p. 259. [Google Scholar]
- 27.Breiman L. Classification and regression trees. Chapman & Hall; New York, N.Y.: 1993. [Google Scholar]
- 28.Therneau T, Atkinson E. An introduction to recursive partitioning using the RPART routines. Mayo Clinic; Report No.: 61. [Google Scholar]
- 29.R Core Team. R . A language and environment for statistical computing. R Foundation for Statistical Computing; Vienna, Austria: 2013. URL http://www.R-project.org/ [Google Scholar]
- 30.Therneau T, Atkinson B, Ripley B. rpart: Recursive Partitioning. R package version 4.1-3. 2013 http://CRAN.R-project.org/package=rpart;
- 31. [2014 Dec 8];2011-12 Report II | Health Professionals | Seasonal Influenza (Flu) [Internet] Available from: http://www.cdc.gov/flu/professionals/vaccination/reporti1112/reportii/index.htm.
- 32.Linn ST, Guralnik JM, Patel KV. Disparities in Influenza Vaccine Coverage in the United States, 2008. J Am Geriatr Soc. 2010 Jul;58(7):1333–40. doi: 10.1111/j.1532-5415.2010.02904.x. doi: 10.1111/j.1532-54152010.02904.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Maurer J, Harris KM, Parker AM. Who knew? Awareness of being recommended for influenza vaccination among US adults. Influenza Other Respir Viruses. 2012 Jul;6(4):284–90. doi: 10.1111/j.1750-2659.2011.00305.x. doi: 10.1111/j.1750-2659.2011.00305.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Brewer NT, Chapman GB, Gibbons FX, Gerrard M, McCaul KD, Weinstein ND. Meta- analysis of the relationship between risk perception and health behavior: The example of vaccination. Health Psychol. 2007;26(2):136–45. doi: 10.1037/0278-6133.26.2.136. doi: 10.1037/0278-6133.26.2.136. [DOI] [PubMed] [Google Scholar]
- 35.Seale H, Heywood AE, McLaws M-L, Ward KF, Lowbridge CP, Van D, et al. Why do I need it? I am not at risk! Public perceptions towards the pandemic (H1N1) 2009 vaccine. BMC Infect Dis. 2010;10(1):99. doi: 10.1186/1471-2334-10-99. doi:10.1186/1471-2334-10-99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Logan JL. Disparities in influenza immunization among US adults. J Natl Med Assoc. 2009 Feb;101(2):161–6. doi: 10.1016/s0027-9684(15)30830-0. [DOI] [PubMed] [Google Scholar]
- 37.Ayanian JZ. Unmet Health Needs of Uninsured Adults in the United States. JAMA. 2000 Oct 25;284(16):2061. doi: 10.1001/jama.284.16.2061. doi:10.1001/jama.284.16.2061. [DOI] [PubMed] [Google Scholar]
- 38.Williams DR, Neighbors HW, Jackson JS. Racial/Ethnic Discrimination and Health: Findings From Community Studies. Am J Public Health. 2003 Feb;93(2):200–8. doi: 10.2105/ajph.93.2.200. doi: 102105/AJPH.93.2.200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zimmerman RK, Raymund M, Janosky JE, Nowalk MP, Fine MJ. Sensitivity and specificity of patient self-report of influenza and pneumococcal polysaccharide vaccinations among elderly outpatients in diverse patient care strata. Vaccine. 2003 Mar 28;21(13-14):1486–91. doi: 10.1016/s0264-410x(02)00700-4. doi:10.1016/S0264-410X(02)00700-4. [DOI] [PubMed] [Google Scholar]
- 40.Fiore AE, Uyeki TM, Broder K, Finelli L, Euler GL, Singleton JA, et al. Prevention and control of influenza with vaccines: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Morb Mortal Wkly Rep. 2010;59(RR-8):1–62. [PubMed] [Google Scholar]
- 41.Yoo B-K. How to Improve Influenza Vaccination Rates in the U.S. J Prev Med Pub Health. 2011 Jul 31;44(4):141–8. doi: 10.3961/jpmph.2011.44.4.141. doi: 10.3961/jpmph.2011.44.4.141. [DOI] [PMC free article] [PubMed] [Google Scholar]