Abstract
Schwannomas (neurilemmomas) are benign tumors arising from the Schwann cells of the neural sheath. They are typically, well-encapsulated lesions which rarely adhere to the adjacent structures. In the chest, schwannomas are often seen within the posterior mediastinum and commonly originating along intercostal nerves. Several operative approaches have previously been described for the resection of these tumors, including thoracoscopic techniques and posterolateral thoracotomy. We report in this case a giant cystic mediastinal schwannoma of the left recurrent laryngeal nerve with cervical extension, unresectable by the usual described approaches, which was completely removed through a cervical approach.
Keywords: mediastinal tumor, schwannoma, thoracotomy, cervicotomy
Endothoracic neurogenic tumors are relatively uncommon. They account for 12–21% of all primary mediastinal tumors (1). Schwannoma and neurofibroma are the most common nerve sheath tumors. Usually, they arise from the sympathetic chain or the intercostal nerves. Treatment is based on surgery. Posterolateral thoracotomy represents the classic approach of these tumors.
We report in this case an exceptional giant Cervico-mediastinal schwannoma of the left recurrent laryngeal nerve which was completely resected by transversal cervicotomy.
Case report
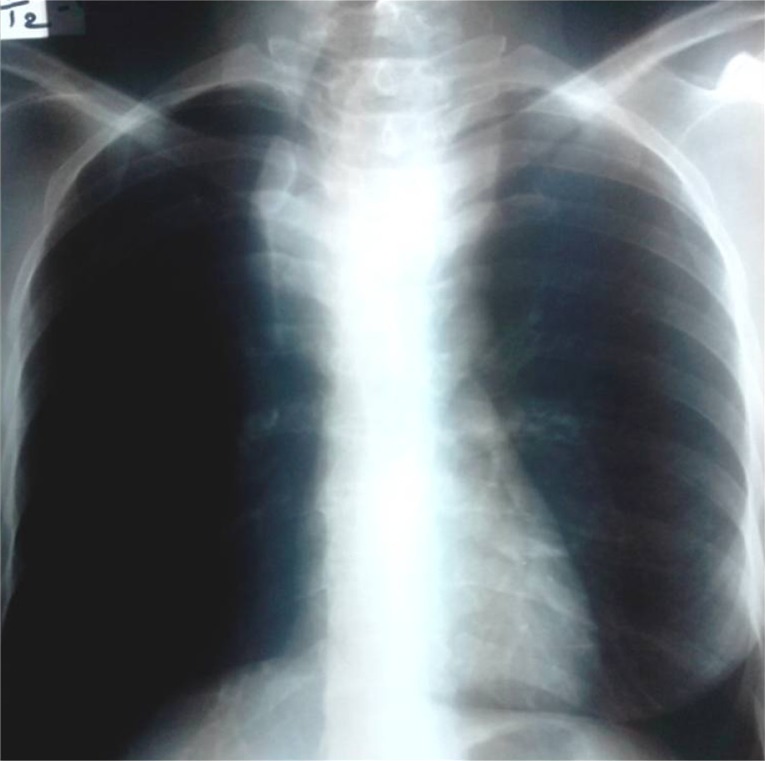
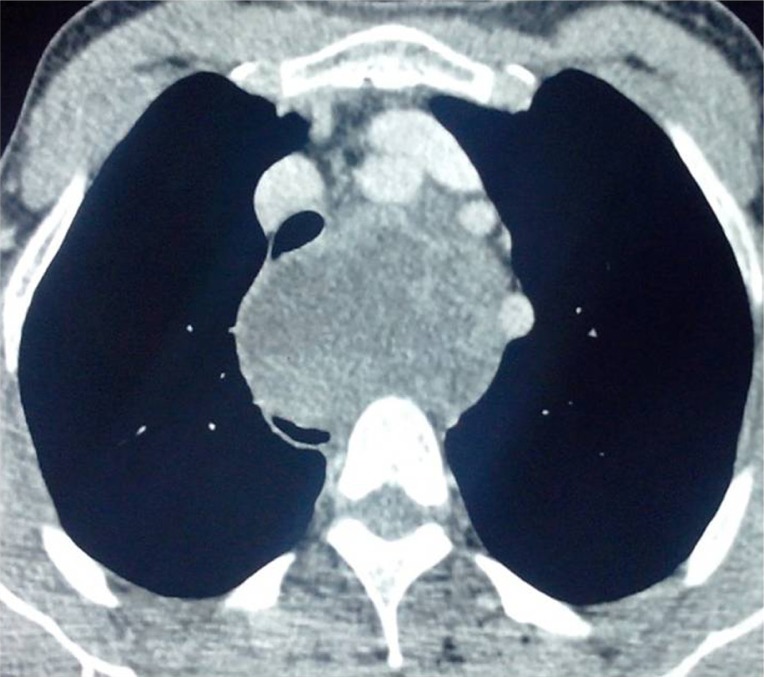
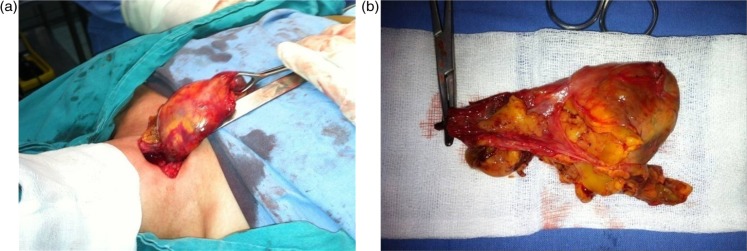
A 44-year-old patient followed 2 years ago for wheezing nocturnal dyspnea associated with a dry cough treated as allergic asthma without symptomatic improvement. Evolution was marked by worsening of dyspnea with paroxysmal breath blockages. Clinical exam revealed only lung bases wheezing. The chest radiography showed an enlargement of the superior mediastinum associated to a right tracheal deviation (Fig. 1). The computed tomography chest scan revealed a cervico-mediastinal multilocular mass extended from the left thyroid lobe to the tracheal bifurcation measuring 12 cm in height (Fig. 2). These structures were not invaded by tumor and edging security was well identified. The cystic nature of the mass was confirmed by MRI. In addition, MRI has shown an intracystic liquid–liquid level with low intensity T2 confirming the hemorrhagic nature of the fluid content. At the cervical and mediastinal regions, diameter of the mass was 4 and 8 cm, respectively. Esophagus and trachea were partially compressed by the tumor which represses the supra aortic trunks without invasion signs. Bronchoscopy showed an extrinsic compression of the trachea and paralysis of the left vocal cord. The patient had urgently been operated on because of the occurrence of an acute respiratory failure. Cystic mass was completely resected by a transversal cervicotomy after aspiration of the hemorrhagic content (Fig. 3a). The left recurrent laryngeal nerve seems to be carried away with the tumor (Fig. 3b). Histological findings confirm diagnosis of giant schwannoma developed at the expense of the left recurrent laryngeal nerve with necrosis areas. The postoperative course was marked by persistence of left vocal cord paralysis which has been well evolved after speech therapy rehabilitation. One year follow-up did not show any signs suggestive of a tumor recurrence.
Fig. 1.
Chest radiography: enlargement of the superior mediastinum with right tracheal deviation.
Fig. 2.
Computed tomography chest scan (axial section) after iodinated contrast: a liquid mass of the middle mediastinum, well-limited, heterogeneous, repressing trachea and supra-aortic trunks without invasion signs.
Fig. 3.
(a) Tumor removal through the cervical approach. (b) Tumor’s aspect after a complete monoblock extirpation.
Discussion
Mediastinal neurogenic tumors are uncommon. Neurofibromas and schwannomas (neurilemmomas) are the most common nerve sheath tumor of the posterior mediastinum. Schwannomas usually arise in the base of the spinal nerves, but sometimes involve the thoracic nerves. They are often isolated lesions; however, multiple lesions along a nerve have been described (2). The usual site of origin is an intercostal nerve or the sympathetic chain. However, neurogenic tumors may arise from the vagus or the phrenic nerves in the middle mediastinum with tumors of the vagus being much more common than tumors of the phrenic nerve (3). Other atypical locations have also been reported such as trachea and lung (4, 5). In the present case, recurrent laryngeal nerve schwannoma without vagus nerve involvement is exceptional. Diagnosis is frequently evoked to the accidental discovery of abnormalities on chest radiography. Some giant forms may become symptomatic by compression of adjacent structures such as trachea or esophagus. Currently, MRI is the investigation of choice to better define the characteristics of the tumor and its limitations. Macroscopically, schwannomas appear as encapsulated tumor, well limited and taking aspect of spheroidal lobulated masses. Histologically, these tumors are composed of Schwann cells embedded in reticular tissue. They tend to be heterogeneous, especially in giant forms with a variable proportion of cystic areas, necrosis and small calcifications (6). Therapeutic management is based on surgery. Giant mediastinal cystic schwannomas with cervical extension pose problems of exposure because of the limited accessibility of conventional approaches, such as posterolateral thoracotomy, to the cervical region. Several approaches have been reported but none of these techniques have been widespread. Anterior trans cervical thoracic approach proposed by Macchiarini (7) seems to be an interesting alternative but does not justify esthetic and functional postoperative damages. Ladas (8) has described a cervical trans-sternal approach, which consists of a vertical cervicotomy along the anterior border of the sternocleidomastoid muscle pursued by a manubriotomy. This technique is useful and efficacious permitting a good exposure of the thoracic inlet. However, histological characteristics of schwannomas (well limited, encapsulated and liquid content) allow, in some cases like ours, only the cervical approach without absolute necessity of combined approaches. Transversal cervicotomy offers a good exposure of tumor proximal pole. Then, dissection will be progressively carried out until perception of the tumor distal pole. Tumor subsidence will be obtained by a simple puncture–aspiration of the hemorrhagic content. This allows extirpation of the tumor piece through transversal cervicotomy without necessity of approach enlargement. So, we think that some giant schwannomas with cervical extension can only be treated by cervical approach which avoids morbidities linked to cervicothoracic approaches.
Conclusion
Giant cystic schwannomas with cervical extension are uncommon benign tumors. Involvement of the recurrent laryngeal nerve as a site of origin is exceptional. Currently, therapeutic management is based on surgery. Neither posterolateral thoracotomy nor video-assisted thoracoscopy are effective because of exposure defaults. Supra sternal transversal cervicotomy is a suitable approach which permits tumor resection with less morbidity compared to combined cervicothoracic approach as described in our case.
Conflict of interest and funding
The authors have not received any funding or benefits from industry or elsewhere to conduct this study.
References
- 1.Cardillo G, Carleo F, Khalil MW, Carbone L, Treggiari S, Salvadori L, et al. Surgical treatment of benign neurogenic tumours of the mediastinum: a single institution report. Eur J Cardiothorac Surg. 2008;34:1210–14. doi: 10.1016/j.ejcts.2008.09.006. [DOI] [PubMed] [Google Scholar]
- 2.Eguchi T, Yoshida K, Kobayashi N, Saito G, Hamanaka K, Shiina T, et al. Multiple schwannomas of the bilateral mediastinal vagus nerves. Ann Thorac Surg. 2011;91:1280–1. doi: 10.1016/j.athoracsur.2010.09.063. [DOI] [PubMed] [Google Scholar]
- 3.Reza RD, William P, Kittle CF. Intrathoracic tumors of the vagus nerve. Ann Thorac Surg. 1990;50:494–7. doi: 10.1016/0003-4975(90)90509-5. [DOI] [PubMed] [Google Scholar]
- 4.Dorfman J, Jamison BM, Morin JE. Primary tracheal schwannoma. Ann Thorac Surg. 2000;69:280–1. doi: 10.1016/s0003-4975(99)01195-9. [DOI] [PubMed] [Google Scholar]
- 5.Uchiyama M, Shimoyama Y, Usami N, Ito S, Yasuda A, Kawaguchi K, et al. Primary pulmonary malignant schwannoma with extension to the tracheal carina. J Thorac Cardiovasc Surg. 2007;133:265–7. doi: 10.1016/j.jtcvs.2006.09.004. [DOI] [PubMed] [Google Scholar]
- 6.Kumar AJ, Kuhajda FP, Martinez CR, Fishman EK, Jezic DV, Siegelman SS. Computed tomography of the extracranial nerve sheath tumors with pathological correlation. J Comput Tomogr. 1983;7:857–65. doi: 10.1097/00004728-198310000-00020. [DOI] [PubMed] [Google Scholar]
- 7.Macchiarini P, Dartevelle P, Chapellier A, Lenot B, Cerrina J, Ladurie FL, et al. Technique for resecting primary and metastatic nonbronchogenic tumors of the thoracic outlet. Ann Thorac Surg. 1993;55:611–18. doi: 10.1016/0003-4975(93)90263-h. [DOI] [PubMed] [Google Scholar]
- 8.Ladas G, Rhys-Evans PH, Goldstraw P. Anterior cervical – transsternal approach for resection of benign tumors at the thoracic inlet. Ann Thorac Surg. 1999;67:785–9. doi: 10.1016/s0003-4975(98)01323-x. [DOI] [PubMed] [Google Scholar]