Abstract
Objective
The aim of this study was to estimate the prevalence and correlates of mental disorders in Korean adults.
Methods
Door to door household surveys were conducted with community residents aged 18-74 years from July 19, 2011, to November 16, 2011 (n=6,022, response rate 78.7%). The sample was drawn from 12 catchment areas using a multistage cluster method. Each subject was assessed using the Korean version of the World Health Organization Composite International Diagnostic Interview (CIDI) based on the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV).
Results
Lifetime and 12-month prevalence estimates were as follows: alcohol use disorders, 13.4% and 4.4%, respectively; nicotine use disorders, 7.2% and 4.0%, respectively; anxiety disorders, 8.7% and 6.8%, respectively; and mood disorders, 7.5% and 3.6%, respectively. The prevalence rates of all types of DSM-IV mental disorders were 27.6% and 16.0%, respectively. Being female; young; divorced, separated, or widowed; and in a low-income group were associated with mood and anxiety disorders after adjustment for various demographic variables, whereas being male and young were associated with alcohol use disorders. Higher income was not correlated with alcohol use disorder as it had been in the 2001 survey.
Conclusion
The rate of depressive disorders has increased since 2001 (the first national survey), whereas that of anxiety disorders has been relatively stable. The prevalence of nicotine and alcohol use disorders has decreased, and the male-to-female ratio of those with this diagnosis has also decreased.
Keywords: Korean adults, Mental disorders, CIDI, Prevalence
INTRODUCTION
Epidemiological surveys can provide basic information on the progress, treatment, and long-term prognosis of disorders.1 Data from community-based epidemiological studies are especially important in psychiatry because information obtained from national insurance claim forms is not sufficient to evaluate the prevalence and distribution of mental disorders given that the lifetime treatment rate of mental disorders is as low as 15.7%1 in Korea. Thus, data from national insurance forms represent only a small portion of the entire target population.
The most recent nationwide epidemiological studies on mental disorders in Korea were the 2006 Korean Epidemiologic Catchment Area study Replication (KECA-R)1 and the 2001 Korean Epidemiologic Catchment Area study (KECA).2 The KECA and KECA-R used the Korean version of the Composite International Diagnostic Interview 2.1 (K-CIDI 2.1)3 to evaluate mental disorders based on the Diagnostic and Statistical Manual of Mental Disorders-fourth edition (DSM-IV).4 Comparisons of the results of these two studies revealed that the prevalence of mental disorders changed considerably during the 5 years between 2001 and 2006. The lifetime prevalence of nicotine and alcohol use disorders markedly decreased, from 23.5% in 2001 to 16.4% in 2006. In contrast, the lifetime prevalence of major depressive disorder (MDD) increased, from 4.3% in 2001 to 5.6% in 2006.1,2
Korean society has experienced rapid change during past a few decades, and mental health problems such as suicide have emerged as social issues. Consequently, we need a new national survey to evaluate changes in mental illnesses since 2006. This study, conducted with the support of the Korea Ministry of Health and Welfare, estimated the prevalence and correlates of mental disorders in Korean adults and compared these results with those from previous studies.
METHODS
Subjects
The 2011 Korean Epidemiologic Catchment Area study (KECA-2011) is a nationally representative survey on mental illness conducted between July 19, 2011, and November 16, 2011. The target population included all non-institutionalized eligible Koreans aged 18-74. This is the first national survey on mental disorders to include individuals older than 65 years.
We used a multistage, cluster sampling method based on 2010 Population Census data obtained from the Korea National Statistical Office.5 We initially divided South Korea into six large divisions according to administrative districts. We then selected 12 catchment areas (Si/Gun/Gu in Korean) in these divisions based on population size and accessibility to research centers. Next, between three and eight subdivisions (Eup/Myeon/Dong) per catchment area were selected based on population size. We adopted the census blocks used in the 2010 national population census5 ("enumeration districts") as sampling units. A total of 246 sampling units were selected from within the total of 61 subdivisions. Every household in each unit was included in the survey (14,204 households), and one individual per household was randomly chosen as the respondent. Trained field workers conducted preliminary surveys by visiting every household to compile a list of eligible subjects. Household visits were repeated at least five times to contact individuals who were temporarily unavailable. We excluded individuals who were not within the age range, whose eligibility could not be ascertained, and who were impossible to contact. Houses that were not households and empty houses were also excluded.
All subjects were fully informed about the aims and methods of the study before completing the interview, and informed consent was obtained prior to participation. This study was approved by the Institutional Review Board of Seoul National University Hospital (IRB No. C-1104-092-359).
Diagnostic assessment
The Korean version of the Composite International Diagnostic Interview 2.1 (K-CIDI 2.1) was administered to all subjects by trained interviewers. The CIDI6 is a fully structured interview designed to identify psychiatric diagnoses. Although the CIDI6 can identify both ICD-10 diagnoses and DSM-IV4 diagnoses, this paper discusses only the DSM-IV diagnoses. The K-CIDI was validated by Cho et al.3 according to the World Health Organization (WHO) guidelines.7 The K-CIDI 2.1 was also used in the 2001 KECA and the 2006 KECA-R, both of which were national psychiatric epidemiological surveys.
A total of 78 interviewers recruited from each catchment area received a 5-day training session according to the standard protocols and training materials developed by the WHO.
Statistical analysis
Weights were calculated for the respondents and used to adjust the data to approximate the national age and sex distributions according to the 2010 census.5 All statistical analyses were based on the weighted data. Multivariate logistic regression was performed to determine the demographic correlates of MDD and alcohol use disorders. Statistical significance was set at p<0.05, and all analyses were performed using SPSS 18.0 for Windows.
RESULTS
Subjects characteristics
A total of 6,022 subjects completed the interview, and 1,628 refused (response rate: 78.7%). Table 1 presents the demographic profile of the sample.
Table 1. Demographic characteristics of the subjects: the KECA-2011 study.
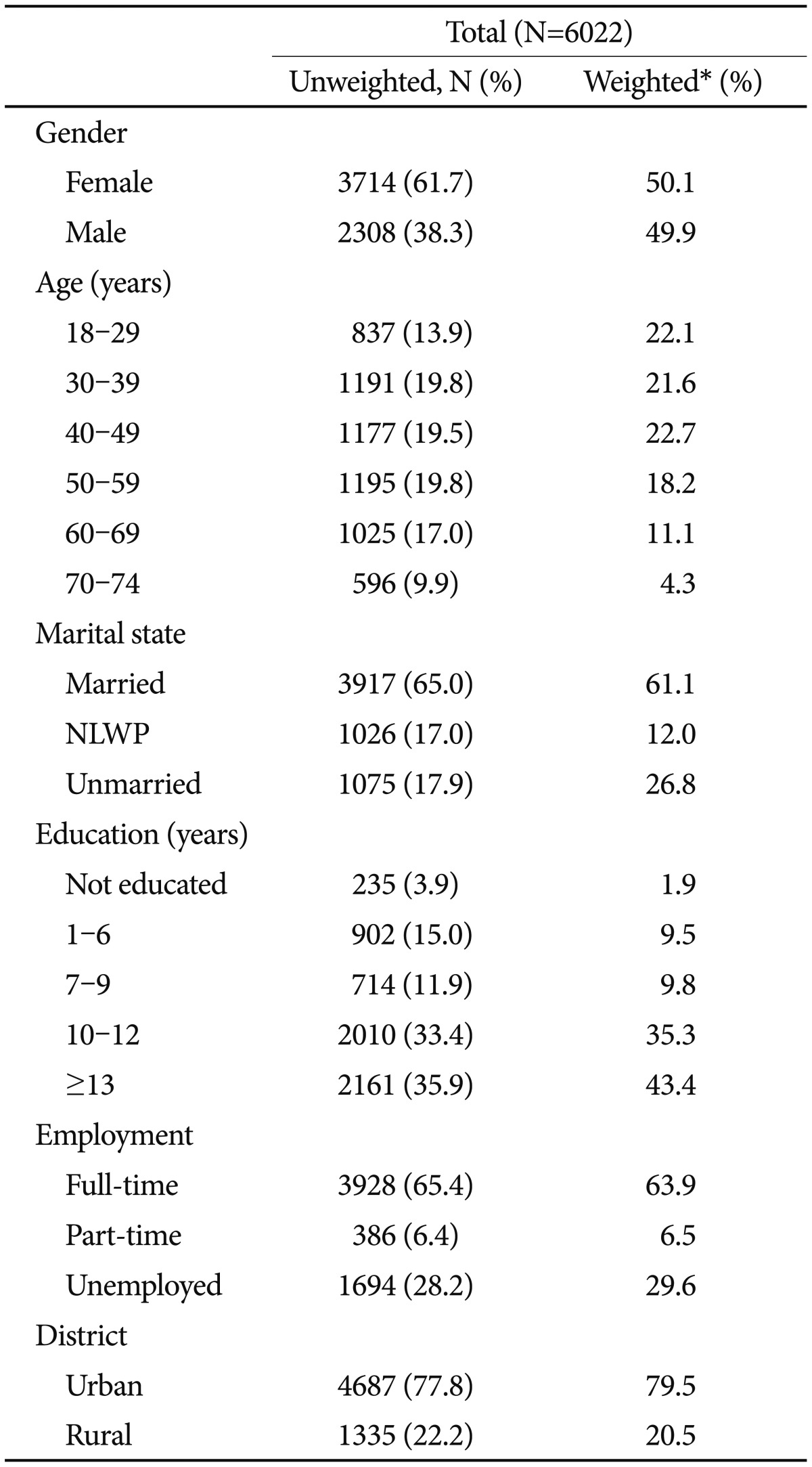
*weighted by age and sex to the general population of South Korea. KECA: Korean Edipemiologic Catchment Area, NLWP: not living with partner, or separated/divorced/widowed
Prevalence of mental disorders
Lifetime and 12-month prevalence rates of major DSM-IV mental disorders are shown in Table 2 along with their corresponding standard errors (SEs). More than one-quarter (27.6%) of respondents had experienced at least one DSM-IV mental disorder before being interviewed. Excluding nicotine use disorders, the lifetime prevalence of all DSM-IV mental disorders was 24.7%. When both nicotine and alcohol use disorders were excluded, the prevalence of all DSM-IV mental disorders decreased to 14.4%.
Table 2. Lifetime and 12-month prevalence* of DSM-IV major mental disorders in South Korea (weighted†).
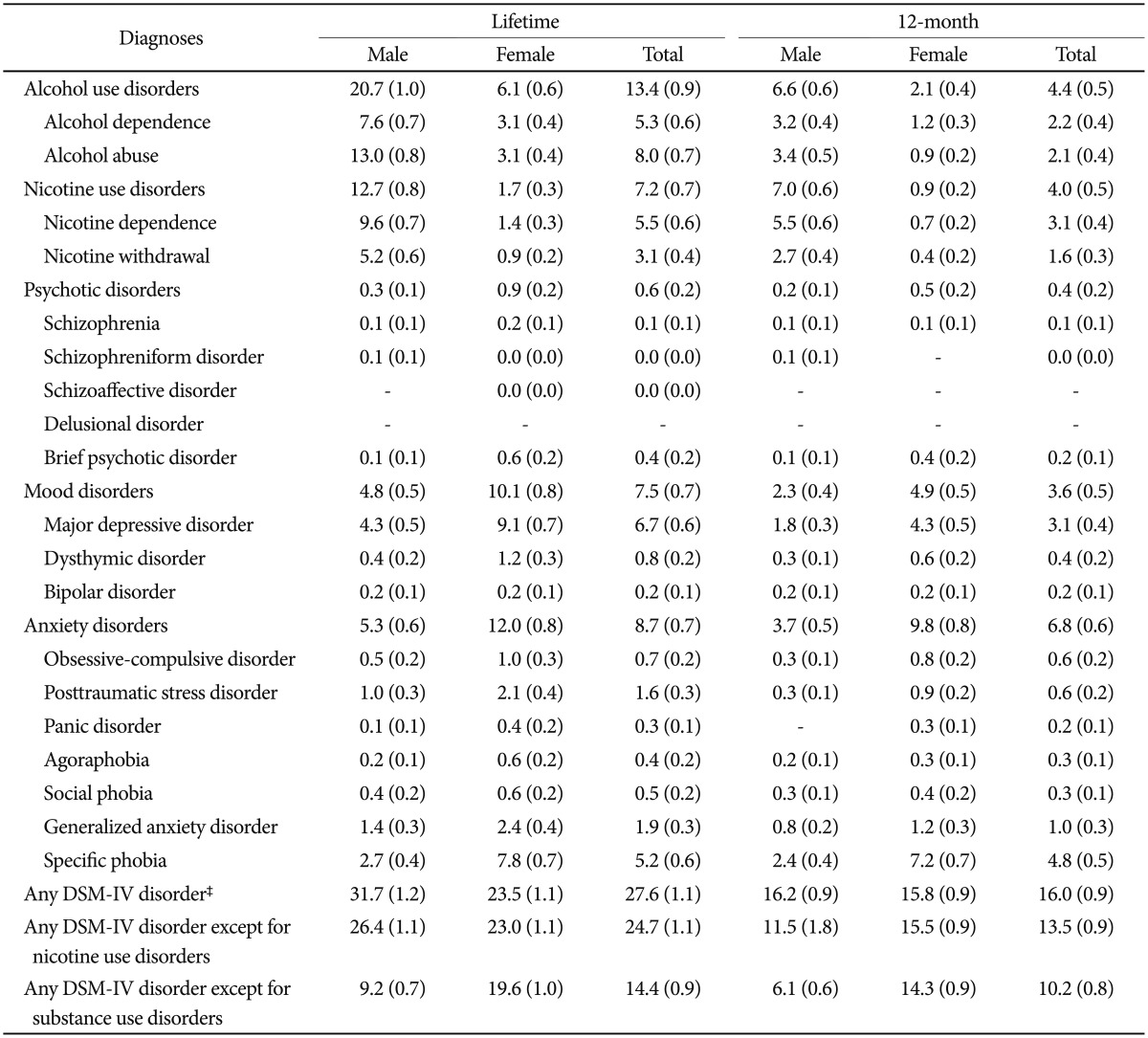
*values are given as % (SE), †weighted by age and sex to the general population of South Korea, ‡including alcohol use disorders, nicotine use disorders, psychotic disorders, mood disorders and anxiety disorders. DSM-IV: Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition
In terms of lifetime prevalence, alcohol use disorders were the most prevalent (13.4%), followed by anxiety disorders (8.7%), mood disorders (7.5%), and nicotine use disorders (7.2%). Alcohol use disorders were the most common lifetime diagnoses among men (20.7%), and anxiety disorders were the most common lifetime diagnoses (12.0%) among women.
During the 12 months before the survey, 16.0% of the subjects had suffered from more than one DSM-IV mental disorder. Anxiety disorders (6.8%) were most frequently reported, followed by alcohol use disorders (4.4%), nicotine use disorders (4.0%), and mood disorders (3.6%). Nicotine use disorders (7.0%) were the most common among men, and anxiety disorders (9.8%) were the most common among women.
Demographic correlates
Adjusted odds ratios of lifetime and 12-month prevalence rates of mood disorders, anxiety disorders, and alcohol use disorders were calculated by demographic characteristics (Table 3). Because these mental disorders were the most prevalent among Korean adults, they were included for further logistic regression analyses, which were adjusted for various demographic characteristics.
Table 3. Adjusted odds ratio (AOR)† and 95% confidence interval (CI) of lifetime and 12-month mood disorder, anxiety disorder, and alcohol use disorder by demographic characteristics (weighted‡).
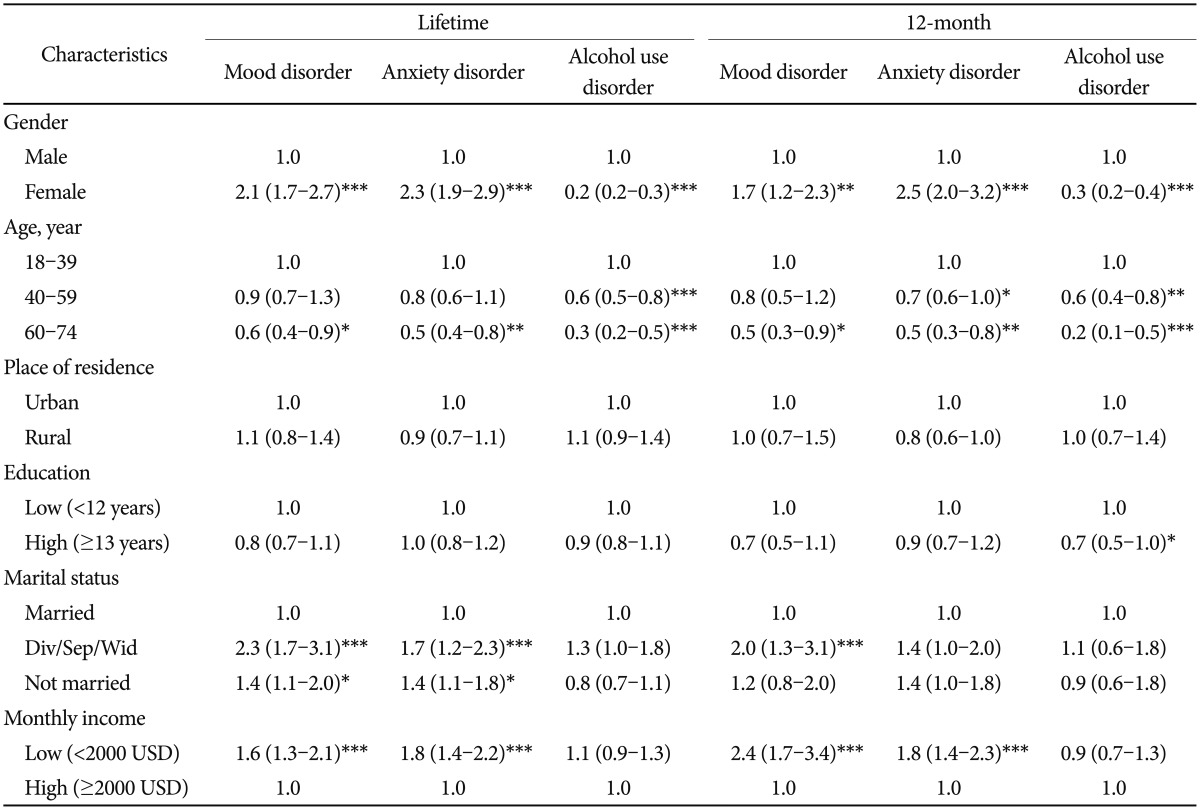
*p<0.05, **p<0.01, ***p<0.001, †adjusted for all of the variables above, ‡weighted by age and sex to the general population of South Korea
According to the bivariate analyses, being female; young; divorced, separated, or widowed (div/sep/wid); and in a low-income group (<2000 USD) were associated with an increased risk for both lifetime and 12-month prevalence rates of mood disorders, and also for the lifetime prevalence of anxiety disorders. In contrast, the lifetime and 12-month prevalence rates of alcohol use disorders decreased as a function of age, and being male was associated with the prevalence of alcohol use disorders. Marital status and monthly income were not related to the prevalence of alcohol use disorders, whereas having less education (<12 years) was significantly correlated with the 12-month prevalence of alcohol use disorders.
DISCUSSION
The prevalence of major mental disorders was as high in Korea as in other developed countries. More than one-quarter (27.6%) of the subjects had experienced at least one DSM-IV mental disorder in their lifetime.
We compared the results of this study with those of a previous national epidemiologic study conducted in 2006.1 The 12-month prevalence of any mental disorder, excluding those involving nicotine and alcohol use, increased from 9.1% in 2006 to 10.2% in 2011. However, the prevalence of nicotine and alcohol use disorders declined substantially. Thus, the overall prevalence of all DSM-IV mental disorders, including nicotine and alcohol use disorders, decreased among community residents aged 18-64 years from 19.0% in 20012 and 16.9% in 20061 to 16.2% in 2011.
Mood disorders
The 12-month prevalence of major depressive disorder increased from 1.8% in 20012 and 2.5% in 20061 to 3.1% in 2011. This increased prevalence of MDD may be associated with the high suicide rate in Korea, which increased dramatically between 1992 (8.3 per 100,000 individuals) and 2010 (31.2 per 100,000 individuals). However, the prevalence of dysthymic disorder and bipolar disorder remained relatively stable during this period.
In general, depressive disorder is less frequently reported in Asian countries than in countries with European ancestry: it was 2.2% in China,8 2.9% in Japan,9 9.6% in the US,10 and 5.2% in the Netherlands.11 Chang et al.12 suggested that the low prevalence of depression in Korea may be due to Koreans' use of a higher threshold for what constitutes a depressed mood. Although the prevalence of MDD in Korea remains lower than it is in Western countries, the prevalence of MDD has increased as industrialization and Westernization have progressed. Increased stress and rapid sociocultural change may affect vulnerability to mood disorders. Additionally, as public knowledge about MDD has advanced, Korean individuals may be more amenable to acknowledging depressive symptoms.
Whereas being female or separated/divorced was associated with the 12-month prevalence of MDD in the adjusted logistic regression model used in the 2001 survey,2 being younger and in a low-income group were added as correlates of MDD in this 2011 survey. This change suggests that more attention should be devoted to the mental health of members of the younger generation who are unemployed or have a low income.
Anxiety disorders
The 12-month prevalence of anxiety disorders also increased, from 5.0% in 20061 to 6.8% in 2011. This prevalence is higher than that in other East Asian countries (2.7% in metropolitan areas of China8 and 4.8% in Japan9), but it is much lower than it is in Western countries (12.0% in France,10 18.2% in the US,10 and 10.1% in the Netherlands). Obsessive-compulsive disorder, which had a prevalence of 0.6% in this study, was not treated as an anxiety disorder in the WHO-World Mental Health studies of Japan and China and in the Netherlands.10,11
Moreover, as some kinds of anxiety disorders are strongly influenced by the sociocultural environment, their prevalence in Korea and Western countries may differ substantially. For example, the prevalence of social phobia was 0.4% in this study, whereas it was 7.1% in the NCS-R,10 6.8% in the US,10 1.7% in France,10 and 3.8% in the Netherlands.11
Nicotine and alcohol use disorders
The prevalence of both nicotine and alcohol use disorders has been decreasing. The 12-month prevalence of nicotine dependence decreased from 6.0% in 20012 and 5.1% in 20061 to 3.2% in 2011. This dramatic change may be attributable to the government's anti-smoking policies and the negative social attitudes toward smokers.
Similarly, the 12-month prevalence of alcohol use disorders also dropped markedly, from 6.8% in 20012 and 5.6% in 20061 to 4.4% in 2011; however, it was still much higher than that in China (1.6%)8 and Japan (0.5%).9 Moreover, this prominent reduction in alcohol use disorders has been evident only in males (25.2% in 2001,2 25.5% in 2006,1 and 20.7% in 2011); in women, the prevalence has remained relatively stable (6.3% in 2001,2 6.9% in 2006,1 and 6.1% in 2011. As a result, the male to female ratio in the prevalence of alcohol use disorders declined from 4.4 in 20012 and 3.7 in 20061 to 3.4 in 2011.
This result may also be attributable to a change in the sociocultural environment. The traditionally permissive attitudes in Korea toward alcohol-related problems in males have shifted toward a disapproving view that treats these as "maladaptive patterns of alcohol use."13 In contrast, negative attitudes toward alcohol consumption by females have been reduced as more women have entered the workplace.
Being male and younger were associated with alcohol use disorders in the 2001 survey.2 However, although high income was an important correlate of alcohol use disorders in 2001 (AOR 1.7),2 economic status was no longer associated with these disorders in 2011. We can assume that the reduced prevalence of alcohol use disorders applies to those with high incomes and not to those with low incomes.
Psychotic disorders
The lifetime prevalence of schizophrenia in this study was 0.1%, which is same as in the previous studies in 20012 and 2006.1 However, the prevalence of schizophrenia in a community sample may be underestimated for several reasons. Psychotic disorders tend to be underreported in community samples as the social stigma and cognitive decline related to psychotic disorders can interfere with reports about psychotic symptoms or cause patients to refuse study participation. Additionally, the psychosis module of the CIDI has good specificity but poor sensitivity.14 As schizophrenia is very similar to schizophreniform and schizoaffective disorders, schizophrenia may have been misdiagnosed as one of the other two disorders. Even when the CIDI can make this differential diagnosis, it can be hard for lay interviewers to distinguish the disorders from one another. When the rates of schizophreniform and schizoaffective disorders was added to that of schizophrenia the prevalence increased to 0.2%.
Additionally, institutionalized individuals were not included in this study. If institutionalized patients with schizophrenia had been included, the prevalence may have increased to 0.3%, which is similar to the prevalence of this disorder according other national studies. The lifetime combined prevalence of schizophrenia, schizoaffective disorder, and schizophreniform disorder was 0.37% in the Netherlands,15,16 and the prevalence of schizophrenia was 0.4% in a Chinese rural area.17 In their systematic review Saha et al.18 reported that the median lifetime prevalence of schizophrenia was 0.4%.
Limitations
This study has several limitations, including its cross-sectional sectional design. Additionally, non-respondents may have affected the prevalence rates of mental disorders as it has been reported that non-respondents tend to have higher rates of mental disorders than do respondents.19,20 Indeed, individuals with severe mental disorders may have found it more difficult to complete the survey due to the symptoms of their specific disorder or related cognitive difficulties. Thus, more severe disorders may have been underreported compared with less severe disorders.
Moreover, recall bias may have influenced the results as respondents, especially elderly individuals with cognitive impairment, may forget or underestimate their symptoms.
Conclusion
This study examined the prevalence and correlates of major mental disorders in Korea and compared them with comparable data from previous surveys. We found that major mental disorders were highly prevalent in Korea. More than one-quarter of the subjects had experienced at least one DSM-IV mental disorder in their lifetime. Although the prevalence of nicotine and alcohol use disorders has decreased, they remained more prevalent in Korea than in Japan or China, and the decreasing trend was not observed in women. The prevalence of MDD has increased and is now similar to that in Japan, but it remains lower than that in Western countries. Conversely, anxiety disorders have become more prevalent in Korea than in other East Asian countries, but this rate was also much lower than that in Western countries.
Acknowledgments
This study was funded by the Korean Ministry of Health and Welfare, which had no role in study design; the collection, analysis, and interpretation of data; the writing of the report; or the decision to submit the paper for publication. The authors wish to express their gratitude to the 78 interviewers and to the subjects who completed the interview.
References
- 1.Cho MJ, Chang SM, Lee YM, Bae A, Ahn JH, Son J, et al. Prevalence of DSM-IV major mental disorders among Korean adults: a 2006 National Epidemiologic Survey (KECA-R) Asian J Psychiatr. 2010;3:26–30. doi: 10.1016/j.ajp.2010.01.009. [DOI] [PubMed] [Google Scholar]
- 2.Cho MJ, Kim JK, Jeon HJ, Suh T, Chung IW, Hong JP, et al. Lifetime and 12-month prevalence of DSM-IV psychiatric disorders among Korean adults. J Nerv Ment Dis. 2007;195:203–210. doi: 10.1097/01.nmd.0000243826.40732.45. [DOI] [PubMed] [Google Scholar]
- 3.Cho MJ, Suh DW, Hong JP, Bae JN, Kim JK, Lee DW, Cho SJ. Development of a Korean version of the Composite International Diagnostic Interview (K-CIDI) J Korean Neuropsychiatr Assoc. 2002;41:123–137. [Google Scholar]
- 4.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th Edition. Washington, DC: American Psychiatric Press; 1994. [Google Scholar]
- 5.Korea National Statistical Office. 2010 Population and Housing Census Report. Daejeon, Korea: Korea National Statistical Office; 2011. [Google Scholar]
- 6.World Health Organization. Composite International Diagnostic Interview (CIDI), Version 1.0. Geneva, Switzerland: World Health Organization; 1990. [Google Scholar]
- 7.World Health Organization. Procedures for the Development of New Language Versions of the WHO Composite International Diagnostic Interview (WHO-CIDI) Geneva, Switzerland: World Health Organization; 1997. [Google Scholar]
- 8.Shen YC, Zhang MY, Huang YQ, He YL, Liu ZR, Cheng H, et al. Twelve-month prevalence, severity, and unmet need for treatment of mental disorders in metropolitan China. Psychol Med. 2006;36:257–267. doi: 10.1017/S0033291705006367. [DOI] [PubMed] [Google Scholar]
- 9.World Mental Health Survey in Japan. [Accessed November 17, 2012]. Available at: http://www.ncnp.go.jp/nimh/keikaku/epi/result.html.
- 10.Demyttenaere K, Bruffaerts R, Posada-Villa J, Gasquet I, Kovess V, Lepine JP, et al. Prevalence, severity, and unmet need for treatment of mental disorders in the World Health Organization World Mental Health Surveys. JAMA. 2004;291:2581–2590. doi: 10.1001/jama.291.21.2581. [DOI] [PubMed] [Google Scholar]
- 11.de Graaf R, Ten Have M, van Gool C, van Dorsselaer S. [Prevalence of mental disorders, and trends from 1996 to 2009. Results from NEMESIS-2] Tijdschr Psychiatr. 2012;54:27–38. [PubMed] [Google Scholar]
- 12.Chang SM, Hahm BJ, Lee JY, Shin MS, Jeon HJ, Hong JP, et al. Cross-national difference in the prevalence of depression caused by the diagnostic threshold. J Affect Disord. 2008;106:159–167. doi: 10.1016/j.jad.2007.07.023. [DOI] [PubMed] [Google Scholar]
- 13.Hahm BJ, Cho MJ. Prevalence of alcohol use disorder in a South Korean community--changes in the pattern of prevalence over the past 15 years. Soc Psychiatry Psychiatr Epidemiol. 2005;40:114–119. doi: 10.1007/s00127-005-0854-9. [DOI] [PubMed] [Google Scholar]
- 14.Cooper L, Peters L, Andrews G. Validity of the Composite International Diagnostic Interview (CIDI) psychosis module in a psychiatric setting. J Psychiatr Res. 1998;32:361–368. doi: 10.1016/s0022-3956(98)00021-1. [DOI] [PubMed] [Google Scholar]
- 15.Bijl RV, Ravelli A, van Zessen G. Prevalence of psychiatric disorder in the general population: results of The Netherlands Mental Health Survey and Incidence Study (NEMESIS) Soc Psychiatry Psychiatr Epidemiol. 1998;33:587–595. doi: 10.1007/s001270050098. [DOI] [PubMed] [Google Scholar]
- 16.van Os J, Hanssen M, Bijl RV, Vollebergh W. Prevalence of psychotic disorder and community level of psychotic symptoms: an urban-rural comparison. Arch Gen Psychiatry. 2001;58:663–668. doi: 10.1001/archpsyc.58.7.663. [DOI] [PubMed] [Google Scholar]
- 17.Ran MS, Xiang MZ, Li SX, Shan YH, Huang MS, Li SG, et al. Prevalence and course of schizophrenia in a Chinese rural area. Aust N Z J Psychiatry. 2003;37:452–457. doi: 10.1046/j.1440-1614.2003.01203.x. [DOI] [PubMed] [Google Scholar]
- 18.Saha S, Chant D, Welham J, McGrath J. A systematic review of the prevalence of schizophrenia. PLoS Med. 2005;2:e141. doi: 10.1371/journal.pmed.0020141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.de Graaf R, Bijl RV, Smit F, Ravelli A, Vollebergh WA. Psychiatric and sociodemographic predictors of attrition in a longitudinal study: The Netherlands Mental Health Survey and Incidence Study (NEMESIS) Am J Epidemiol. 2000;152:1039–1047. doi: 10.1093/aje/152.11.1039. [DOI] [PubMed] [Google Scholar]
- 20.Eaton WW, Anthony JC, Tepper S, Dryman A. Psychopathology and attrition in the epidemiologic catchment area surveys. Am J Epidemiol. 1992;135:1051–1059. doi: 10.1093/oxfordjournals.aje.a116399. [DOI] [PubMed] [Google Scholar]


