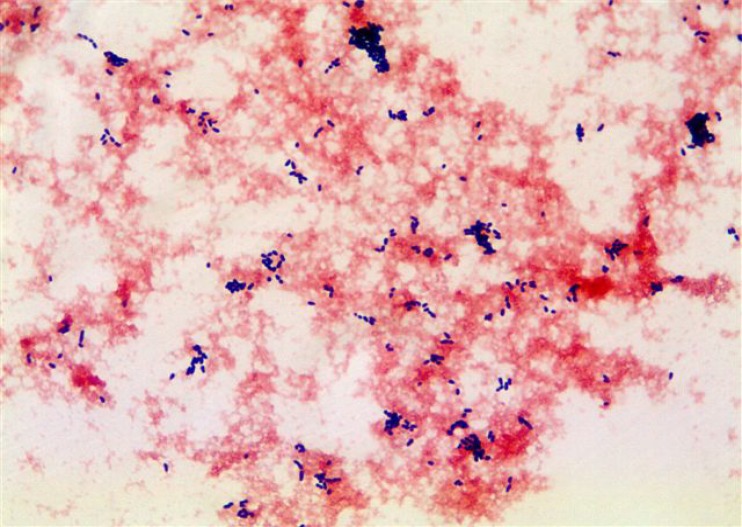
A 63-year-old Caucasian female with a history of Crohn's disease and recurrent gastrointestinal strictures requiring multiple surgeries, including end ileostomy, presented to our medical center in June 2012 with a 1-week history of fevers up to 104°F and rigors. She had also experienced acute worsening of her chronic high-volume stool output, for which she was taking a probiotic. She had had a peripherally inserted central catheter (PICC) in place for 3 months for total parenteral nutrition (TPN). Intravenous vancomycin had been started at her nursing home in the week prior to admission, with no improvement in symptoms. On examination, she appeared diaphoretic, with a fever of 102.7°F as determined orally. She was tachycardic (118 beats/minute), with normal blood pressure and respiratory rate. The PICC insertion site in her left arm showed no erythema or drainage. Her peripheral white blood cell count was 12,500 cells/μl (76.7% neutrophils, 14.3% lymphocytes, 8.6% monocytes, and 0.3% eosinophils). The chest X-ray was clear. Two sets of blood cultures were drawn from the periphery and one was drawn from the PICC prior to removal. She was started on empirical daptomycin and piperacillin-tazobactam. The three sets of blood cultures grew a Gram-positive coccobacillus in both Bactec Plus aerobic F and Bactec anaerobic lytic bottles (Bactec 9240 blood culture system; Becton Dickinson Diagnostic, Sparks, MD) (Fig. 1). Based on the Gram stain and this patient's underlying medical conditions and clinical presentation, what is the most likely organism?
FIG 1.
Gram stain from blood culture bottle (magnification, ×1,000).
(For answer and discussion, see page 1052 in this issue [doi:10.1128/JCM.00956-13].)