Abstract
Introduction
Oxaliplatin remains the most widely used chemotherapeutic agent for treating advanced colorectal cancer but its efficacy is hampered by dose-limiting neurotoxicity manifested by a painful polyneuropathy. Oxaliplatin-induced peripheral neuropathy (OIPN) is characterised by acute and transient cold hyperaesthesia in the hours and days following oxaliplatin infusion (>90% of patients), but also by retarded chronic neuropathy due to the repetition of chemotherapy cycles (30–50% of patients). OIPN impairs the health-related quality of life (HRQOL) of patients and no preventive or curative strategies have as yet proven effective. A polyamine-reduced diet (PRD) has recently demonstrated its efficacy to prevent OIPN in animals without adverse effects.
Methods and analysis
The NEUROXAPOL trial is a prospective, randomised, controlled, single-blind, monocentric and interventional study. This trial is aimed at evaluating the efficacy and feasibility of a PRD compared to a normal polyamine containing diet to prevent OIPN in patients treated by oxaliplatin-based chemotherapy. Patients (n=40 per group) will be randomly assigned to receive either a PRD or a normal diet before and during the chemotherapy regimen. The main objectives are to improve the cold pain thresholds, neuropathic pain symptoms, comorbidities (anxiety and depression) and HRQOL of patients. The primary end point is the assessment of cold pain thresholds 2 weeks after the third cycle of chemotherapy. The secondary end points are the evaluation of thermal pain thresholds, the grade of neuropathy, neuropathic pain, symptoms of anxiety and depression and HRQOL, until the 12th cycle of chemotherapy.
Ethics and dissemination
The study was approved by an independent medical ethics committee 1 (CPP Sud Est 1, Saint Etienne, France) and registered by the competent French authority (ANSM, Saint Denis, France). The results will be disseminated in a peer-reviewed journal and presented at international congresses.
Trial registration number
Introduction
Oxaliplatin remains one of the lead treatments for colorectal cancers.1 However, its anticancer efficacy is associated with adverse drug reactions and particularly chemotherapy-induced peripheral neuropathy (CIPN), which is the main dose-limiting toxicity2 of this treatment. Chronologically, oxaliplatin induces acute and transient nerve hyperexcitability followed by a chronic cumulative peripheral neuropathy.3 Oxaliplatin is certainly one of the most neurotoxic anticancer drugs, alongside Vinca alkaloids, taxanes, bortezomib and thalidomide.3 More than 90% of patients experience acute symptoms which are however resolved within a few days and 30–50% of patients suffer from chronic oxaliplatin-induced peripheral neuropathy (OIPN).2 4 OIPN grade and symptom duration can be variable between studies.2 However, although these symptoms seem to decrease with time, OIPN can last for several years after the end of the chemotherapy.2 5 The great majority of studies have demonstrated a link between a cumulative dose above 850 mg/m2 oxaliplatin and the onset of neuropathy.2 OIPN presents specific sensory disturbances, with cold and warm triggered pain and a decrease in vibratory perception in the hands and feet.6 In the longer term, OIPN has a deleterious impact on cancer survivors, often being associated with sleep disturbance, depressive symptoms and impaired health-related quality of life (HRQOL).7 8
Based on literature analysis, there are no pharmacological agents recommended for the prevention of OIPN and other CIPNs. Duloxetine is the only treatment that can be proposed for the treatment of CIPN, but with recommendations for moderation.9 Considering that colorectal cancer survivors represent the third largest group of cancer survivors,10 innovative strategies are needed to improve the prevention and/or treatment of OIPN. Among these innovative strategies, specific diets provide real opportunities for the management of neuropathy symptoms.11
A polyamine-reduced diet (PRD) containing less than 10 mg/kg of polyamines can relieve pain hypersensitivity (inflammatory and neuropathic pain) in animals.12 Polyamines (putrescine, spermidine and spermine) are polycations ubiquitously distributed in eukaryotic cells and mainly originating from dietary intake.13 Polyamines are known to be positive modulators of NR2B containing N-methyl-d-aspartate (NMDA) receptors which are involved in central sensitisation following peripheral nerve injury.14 As such, polyamines may play a facilitating role in nociceptive neurotransmission and pain chronicisation.12 One main hypothesis is that reducing polyamine intake may improve nociceptive symptoms by decreasing NMDA receptor activity.12 The same PRD has recently been assessed with success in a rat model of oxaliplatin-induced acute nerve hyperexcitability.15 A PRD initiated 7 days before the beginning of the experiments completely prevented acute cold hypersensitivity and mechanical allodynia induced by a single oxaliplatin injection in rats.15 More interestingly, an increase of glutamate concentration in the spinal cord was found in neuropathic animals, which was completely suppressed in PRD-fed animals.15 Finally, this PRD was well tolerated by animals with no significant adverse effect.12 15
This PRD has already been assessed in oncology for its antiproliferative properties16 and is well tolerated by patients.17–19 In clinical practice, this PRD is composed of a diet with low polyamine containing foods available in canned form (Polydol, Nutrialys Medical Nutrition, Saint-Grégoire, France).18 Consequently, these preliminary results in animals can be translated into a clinical trial to validate the preventive effect of a PRD on OIPN.
Methods and analysis
Study design
The present study is a prospective, randomised, controlled, single-blind and monocentric, phase II/III trial that compares a PRD versus a diet with medium polyamine content to prevent OIPN.
Study objectives
The main objective is to demonstrate a decrease of the cold triggered pain threshold 2 weeks after the third cycle of chemotherapy in a group of patients receiving a PRD compared to a control group receiving a diet with medium polyamine content. Cold thermal sensitivity is a characteristic symptom of OIPN after the third cycle of chemotherapy.6 The other objectives of the study are to demonstrate an improvement of: hot triggered pain thresholds, vibration detection threshold, neuropathy grades and neuropathic pain. Besides the reduction of neuropathy symptoms, the trial aims at demonstrating an improvement of anxiety and depressive disorders as well as HRQOL in the PRD group compared to the control group. All these objectives will be assessed during the period of diet control (PRD or diet with medium polyamine content) from day 7 until day 100, after the beginning of oxaliplatin-based chemotherapy and after the return to a normal diet, for all the patients from day 100 until day 154 (end of the study). Under these conditions, a potential persisting effect of the PRD will be monitored from day 100 to day 154.
Inclusion and exclusion criteria
Participants are patients expected to receive adjuvant, neo-adjuvant or palliative oxaliplatin-based chemotherapy. The cycle length of the chemotherapy must be 15 days (eg, FOLFOX). The expected duration of treatment must be at least of eight cycles (4 months; for details see box 1).
Box 1. Inclusion and exclusion criteria of the study.
Inclusion criteria
Oxaliplatin-based chemotherapy (adjuvant, neoadjuvant or palliative) with a cycle length of 15 days and an expected duration of eight cycles (4 months)
Patients who provided written, informed consent
Patients affiliated with the French National Health Insurance
Patients who have not participated in another clinical trial within 15 days before inclusion (possibility of participating in an observational trial)
Effective contraception for patients, male or female of childbearing age
WHO performance index ≤2
Polynuclear neutrophils >2×109/L and/or platelets >100×109/L before the first treatment cycle
Exclusion criteria
Patient not able to receive oxaliplatin whatever the reason
Patient <18 years
Patient in under-nutrition (defined as: weight loss ≥5% after 1 month/≥10% after 6 months, body mass index <21, albuminemia <35 g/L)
Amputation of all or part of the upper limb
Patients with diabetes
Patients with previous neuropathy
Oral food intake impossible
Painful acts scheduled after inclusion (eg, surgical resection)
Neurological pathologies (eg, Parkinsonism, stroke, etc.)
Alcohol consumption over 3 units/day for man and 2 units/day for woman
Patients who have received previous neurotoxic cytotoxic chemotherapy (taxanes, platinum salts or vinca alkaloids)
Patients treated for other cancer within 5 years, with the exception of basal cell skin carcinoma or in situ cervix carcinoma
Any unbalanced progressive disease (hepatic, renal, respiratory, congestive heart failure, myocardial infarction within the past 6 months, etc)
Patients requiring infusions of Ca2+ or Mg2+
Known hypersensitivity or allergy to any component of the study products
Pregnant or breastfeeding women
Legal incapacity (person deprived of liberty or guardianship)
Patients who for psychological, social, family or geographical reasons cannot be monitored regularly and/or be compliant with the requirements of the study
Patients already included in another clinical trial
No treatment contraindication is imposed by the study. The oncologist will have a free choice of prescription for the therapeutic management of patients.
Each patient can be withdrawn of the study according to the following reasons: chemotherapy modification without oxaliplatin, intolerance to Polydol, withdrawal of consent, significant medical event.
Nutritional interventions
Before the beginning of the chemotherapy cycles until day 100, each patient will receive a specific diet according to group randomisation, that is, a PRD or a diet with medium polyamine content. Whatever the diet received, the daily intake for each patient will be about 2000 kcal. At day 100, patients will stop the imposed diet (PRD or diet with medium polyamine content) and return to normal feeding. All patients have to report in a notebook their daily intakes and any adverse effects in order to assess compliance with the diet and its safety.
Polyamine-reduced diet
Depending on the chemotherapy course, the PRD will associate 2 to 4 cans/day of Polydol (Nutrialys Medical Nutrition, Saint-Grégoire, France; tables 1 and 2) and meals with low polyamine content18 (examples of PRD are presented in the tables 3–5). Polydol is a nutritional drink containing all the requisite nutrients but with low polyamine content (357 nmol/L of polyamines and 300 kcal per can of Polydol, data from Nutrialys Medical Nutrition). The number of cans of Polydol per day is adjusted as a function of the time course of the chemotherapy in order to optimise the patient's compliance with the diet while maximising the depletion of polyamine at the time of oxaliplatin administration (figure 1). Before the first chemotherapy cycle, patients will take 4 cans/day of Polydol for 7 days and 3 cans/day after the first chemotherapy infusion. For the other chemotherapy cycles, patients will take 3 cans/day of Polydol, 2 days before and 2 days after the chemotherapy infusions. Finally, between each chemotherapy infusion, the patients will receive 2 cans/day of Polydol (figure 1).
Table 1.
Nutritional values and composition of Polydol can (200 mL)
| Nutritional value | |
|---|---|
| Energy | 300 kcal/1254 kJ |
| Proteins | 15 g |
| Carbohydrates | 36 g |
| Lipids | 12 g |
| Saturated | 3 g |
| Monoinsaturated | 5 g |
| Polyinsaturated | 4 g |
| Omega-3 | 2.6 g |
| Fibres | 0.4 g |
Table 2.
Vitamins and minerals composition of Polydol can (200 mL)
| Vitamins (200 mL) |
Minerals (200 mL) |
||
|---|---|---|---|
| C | 30 mg | K | 360 mg |
| B3 | 5.7 mg (niacin equivalent) | Na | 142 mg |
| E | 2.2 mg (total α-tocopherol) | Ca | 130 mg |
| B5 | 580 µg | P | 104 mg |
| B2 | 300 µg | Cl | 100 mg |
| B1 | 220 mg | Mg | 40 mg |
| A | 132 µg (retinol equivalent) | Fe | 1.4 mg |
| B9 | 40 µg | Zn | 1.4 mg |
| K1 | 13.2 µg | Mn | 360 µg |
| B8 | 2.8 µg | Cu | 224 µg |
| D3 | 2 µg | F | <30 µg |
| B12 | 0.5 µg | I | 20 µg |
| B6 | 0.38 µg | Mo | 10.6 µg |
| Se | 8 µg | ||
| Cr | 6 µg | ||
Table 3.
Examples of PRD with four cans of Polydol per day
| Lunch |
Diner |
|||||
|---|---|---|---|---|---|---|
| Breakfast | Starter | Main course | Dessert | Starter | Main course | Dessert |
| Grilled bread wheat + butter and honey + Polydol coffee taste |
Avocado + lamb's lettuce + olive oil and balsamic vinegar |
Polydol legume taste | French butter cookie + Polydol chocolate flavour |
Leek vinaigrette | Quiche Lorraine with tuna (puff pastry, egg, cream, canned tuna, onion) |
Breton cake + Polydol caramel flavour |
| Tea (Ceylon or green) or coffee + Polydol caramel taste |
Cheese soufflé + lamb's lettuce + seasoning |
Wok salmon onion ginger soy sauce + mashed sweet potato with lemon | Polydol vanilla flavour | Polydol legume flavour | Polydol caramel flavour | Fresh fruit salad (kiwi + apple + pear + pineapple) |
The amount of polyamines is estimated at 29 µmol/day.
PRD, polyamine-reduced diet.
Table 4.
Examples of PRD with three cans of Polydol per day
| Lunch |
Diner |
|||||
|---|---|---|---|---|---|---|
| Breakfast | Starter | Main course | Dessert | Starter | Main course | Dessert |
| Grilled bread wheat + butter and honey + Polydol coffee taste |
Avocado + lamb's lettuce + olive oil and balsamic vinegar |
Halibut fillet and melted leeks with parmesan cream | Polydol caramel taste | Beetroots | Polydol biscuit flavour | Floating island |
|
Polydol coffee taste +wheat toast + strawberry jam + grape juice |
Lamb's lettuce + feta cheese |
Plain omelette, green beans and butter | Polydol chocolate flavour | Polydol vegetable flavour | Sautéed Veal and pumpkin puree | Cottage cheese with apricot jam |
PRD, polyamine-reduced diet.
Table 5.
Examples of PRD with two cans of Polydol per day
| Lunch |
Diner |
|||||
|---|---|---|---|---|---|---|
| Breakfast | Starter | Main course | Dessert | Starter | Main course | Dessert |
| Wheat bread + butter + honey + Polydol coffee taste |
Celery remoulade | Shelley White gratin ham and cream cheese | Applesauce and butter biscuit | Lamb's lettuce | Onion tart (puff pastry + onion + butter) | Polydol chocolate flavour |
| Tea (Ceylon or green) or coffee + Polydol caramel taste |
Rice salad + pepper + Emmental cheese |
Gratin of asparagus (Asparagus + Parmesan) and tuna steak | Raw pear and melted dark chocolate | Puff pastry with anchovy fillets | Wok fried rice with onions and diced grilled chipolata | Polydol caramel flavour |
PRD, polyamine-reduced diet.
Figure 1.
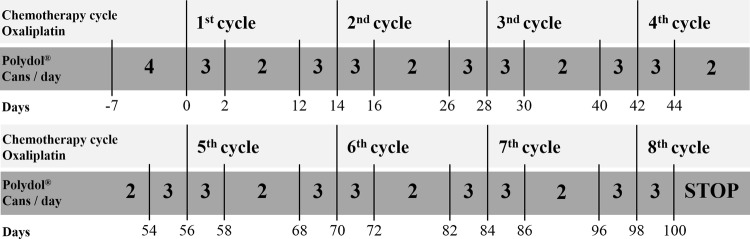
Administration scheme of polyamine-reduced diet according to the time course of chemotherapy cycle.
According to the diets defined above, polyamine intake will be about 29, 39 and 50 µmol per day with 4, 3 and 2 cans/day of Polydol, respectively (data from Nutrialys Medical Nutrition).
Diet with medium polyamine content
The diet with medium polyamine content will associate 1 can of Polydol with a defined diet of medium polyamine content18 (examples of diets with medium polyamine content are presented in table 6). This diet will be maintained throughout the study until day 100. A placebo of Polydol with normal polyamine content is not technically feasible, but the association of only 1 can of Polydol with medium polyamine content is expected to provide an amount of polyamines equivalent to a normal diet (425 µmol/day; data from Nutrialys Medical Nutrition).
Table 6.
Examples of diet with medium polyamine content with one can of Polydol per day
| Lunch |
Diner |
|||||
|---|---|---|---|---|---|---|
| Breakfast | Starter | Main course | Dessert | Starter | Main course | Dessert |
| Green or Ceylon tea + Wholemeal bread + Butter and honey + Orange Juice |
Tomato salad dressing with olive oil and balsamic vinegar | Roast chicken with porcini mushrooms + Farfalle with butter |
Natural yoghurt with honey | Carpaccio raw zucchini with lemon and parmesan | Quiche Lorraine with tuna (puff pastry + egg + cream + canned tuna + broccoli) | Breton cake + Polydol caramel flavour |
| Coffee + Milk with cocoa and chocolate granola cereal + Grapefruit juice |
Cucumber with seasoning (cream and wine vinegar) | Stuffed eggplant (with minced beef) + Semolina |
Apricot tart | Polydol vegetable flavour | Cauliflower gratin with bacon, cream and Comté cheese | Cottage cheese + Raspberries |
Study end points
The primary end point is the cold pain threshold (°C) in the hands (right and left thenar eminence) 42 days after the beginning of the oxaliplatin-based chemotherapy (2 weeks after the third cycle of chemotherapy; MEDOC TSA-II, Abioz Technologies, Ramat Yishai, Israel). The main secondary end points are presented hereafter and will be assessed throughout the study from 7 days before the beginning of chemotherapy until the end of chemotherapy on day 154 (12th cycle of chemotherapy; table 7).
Cold and hot pain thresholds (°C) in the hands (right and left thenar eminence; MEDOC TSA-II, Abioz Technologies, Ramat Yishai, Israel);
Vibrational detection threshold (right and left middle finger; MEDOC VSA 3000, Abioz Technologies, Ramat Yishai, Israel);
Pain assessment (visual analogue scale—VAS);
Neuropathic pain diagnostic (DN4-interview questionnaire—4 questions on neuropathic pain);20
Neuropathic pain intensity (NPSI questionnaire—Neuropathic pain symptoms inventory);21
Neuropathy and adverse drug reaction grades (Common technical classification of adverse effect v4, National Cancer Institute, 2009);
Anxiety and depressive disorders (HADS questionnaire—Hospitalised anxiety and depression scale);22
HRQOL (QLQ-C30 questionnaire—Quality of life questionnaire-core 30, European Organisation for Research and Treatment of Cancer);
Chemotherapy response (Response evaluation criteria in solid tumours—RECIST) for neoadjuvant and palliative chemotherapy;
Single and cumulative oxaliplatin dose received
Polyamine levels in erythrocytes.23
Table 7.
Chronology of end point assessment
| Chemotherapy cycle | 1 | 3 |
4 |
6 |
8 |
12 | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Days | −7 | 0 | 28 | 30 | 42 | 44 | 70 | 72 | 98 | 100 | 154 |
| End points | |||||||||||
| Thermal (cold and hot) pain thresholds Vibrational detection thresholds |
X | X | X | X | X | X | X | X | X | X | X |
| Pain VAS | X | X | X | X | X | X | X | X | X | X | X |
| DN4-interview and NPSI questionnaires | X | X | X | X | X | X | X | X | X | X | X |
| HADS and QLQ-C30 questionnaires | X | X | X | X | X | X | X | ||||
| Polyamine level in erythrocytes | X | X | X | X | X | X | |||||
HADS, Hospitalised anxiety and depression scale; NPSI, Neuropathic pain symptoms inventory; QLQ-30, Quality of life questionnaire-core 30; VAS, visual analogue scale.
Methodology and study design
The trial is performed at a single site. All the patients are recruited, treated and followed-up at the digestive surgery and oncology unit of the University Hospital of Clermont-Ferrand, France.
After controlling the inclusion and exclusion criteria, the NEUROXAPOL trial will be proposed by oncologists (CP and DP) to patients suffering from digestive tract cancer and requiring oxaliplatin-based chemotherapy, admitted in the oncology unit of the University Hospital of Clermont-Ferrand. The patients will be informed of the trial protocol and, on acceptance, will be randomised in the PRD group or in the diet with medium polyamine content group. Randomisation is performed using a dedicated centralised telephone system, accessible round the clock, and using a computer-generated allocation sequence. The randomisation sequence is generated by biostatistician (BP) using random blocks and stratified according to the presence or not of a tumour. Tumours can release polyamines in the blood stream and may influence outcomes.24
The NEUROXAPOL trial is a single-blind protocol because it is impossible to use a placebo for the PRD and the Polydol cans. Under these conditions, the investigator and the clinical research technician will know the type of diet taken by the patients. However, the primary end point (cold pain threshold in hands) is an independent measure performed by the investigator and the clinical research technician, using a validated medical device (MEDOC TSA-II, Abioz Technologies, Ramat Yishai, Israel).
The follow-up visits of patients will be very similar to the standard therapeutic practice in the oncology unit, so the number of missing data should be limited. Moreover, the compliance of patients to the proposed diet will be registered in a patient notebook throughout the study and considered in the statistical analysis.
Statistical considerations
Estimation sample size
According to our previous works and literature,6 we calculated that a sample size of n=35 patients by randomised group would provide 90% statistical power to detect an absolute difference of 5°C in the primary outcome 2 weeks after the third cycle of oxaliplatin-based chemotherapy (baseline of cold pain threshold in the hands at 8°C and standard-deviation equal to 6.3°C), for a two-sided α level of 0.05. Finally, a total of 80 patients will be considered. An interim analysis is planned after enrolment of the first 36 patients using the Lan and DeMets method (East software, Cytel Inc, Cambridge, Massachusetts, USA).
Statistical analysis
Statistical analysis will be conducted on intention to treat (ITT) using Stata software, V.13 (StataCorp, College Station, Texas, USA). A two-sided p value of less than 0.05 will be considered to indicate statistical significance (except interim analysis). Baseline characteristics will be presented for each randomised group as the mean±SD or the median (IQR) according to the statistical distribution for continuous data, and as the number of patients and associated percentages for categorical parameters. Comparisons between independent groups will be analysed using the χ2 or Fisher's exact test for categorical variables (chemotherapy response with RECIST criteria), and Student t test or Mann-Whitney's test for quantitative parameters (notably primary outcome, cold and hot pain thresholds in the hands, vibrational detection threshold, VAS, neuropathic pain diagnostic, polyamine levels in erythrocytes, etc), with normality verified by the Shapiro-Wilk test and homoscedasticity by the Fisher-Snedecor test. As suggested by Vickers and Altman,25 the primary analysis will be completed by an ANCOVA considering the cold pain threshold in the hands 2 weeks after the third cycle of oxaliplatin-based chemotherapy as a dependent variable, and the group and the baseline value of cold pain threshold in the hands as independent parameters. Regarding the analysis of repeated measures, a random-effect model (linear or generalied linear) will be considered, as usually proposed, to study the fixed effects group, time points and interaction ‘group x time’, taking into account between and within subject variability. According to clinical relevance, the multivariate analysis will consider oxaliplatin doses (single and cumulative) as adjustment covariate for each outcome assessed. To assess possible problems caused by missing data, the estimation methods developed by Verbeke and Molenberghs will be proposed.26
Dissemination
Approval
Any substantial change in the protocol and any change in the informed consent form will be presented to the independent medical ethics committee. The independent medical ethics committee and the competent French authority will be informed of the end of the study. In accordance with the independent medical ethics committee (Comité de Protection des Personnes Sud Est 1, Saint Etienne, France), no safety and data monitoring committee has been set up considering the low risk of the nutritional intervention.
The study is currently registered on the clinical trials website under the following number: NCT01775449. The protocol is currently in the V.8 since 14/1/2014.
Patient informed consent
According to the French law on clinical trials, written informed consent must be obtained from patients prior to participation in the study. Patients will voluntarily confirm their willingness to participate in the study, after having been informed (in writing and verbally) by oncologists of all aspects of the study that are relevant to their decision to participate. They will be informed about requirements concerning data protection and have to agree to direct access to their individual data. The patients will be informed that they are free to withdraw from the study at any time at their own discretion without necessarily giving reasons.
Data collection and quality management
A clinical research technician (BG) is dedicated to the data entry, coding, security and storage. Each included patient and study data are anonymisated. Study data are collected and managed using REDCap electronic data capture tools hosted at University Hospital of Clermont-Ferrand.27 REDCap (Research Electronic Data Capture) is a secure, web-based application designed to support data capture for research studies, providing: (1) an intuitive interface for validated data entry; (2) audit trails for tracking data manipulation and export procedures; (3) automated export procedures for seamless data downloads to common statistical packages; and (4) procedures for importing data from external sources.
A clinical research assistant will be commissioned by the sponsor (University Hospital of Clermont-Ferrand) in order to monitor the progress of the study in accordance with the Standard Operating Procedures implemented in the University Hospital of Clermont-Ferrand, in accordance with the Good Clinical Practice and the current French laws.
Access to data and dissemination of results
The data set will be propriety of the sponsor (CHU Clermont-Ferrand). However, the principal investigator (DP) and the project manager (DB) will have a full access to the final data set.
The results will be disseminated in a peer-reviewed journal, presented at international congresses and completed online on ClinicalTrials.gov.
Discussion
This translational research project aims to demonstrate the preventive effect of a PRD on OIPN on both the acute and chronic symptoms of thermal hyperaesthesia, notably cold hyperaesthesia. These cold-induced symptoms are very good biomarkers of OIPN and their precocity are predictive of a strong chronic neuropathy after the repetition of chemotherapy cycles.6 Therefore, the thermal threshold of cold triggered pain should be a reliable, sensitive and quantitative end point for assessing OIPN.
OIPN remains a problematic adverse drug reaction in digestive oncology, because up to 50% of patients can be affected and to this day, no preventive or curative strategy has proven indisputably effective.9 Neuropathy symptoms can last for months and even years after the end of chemotherapy (25 months,28 48 months29 and 8 years5) and the lack of support induces depression, sleep disorders7 and a decrease of HRQoL.7 8 Finally, CIPN has a strong economic and social impact, as patients with CIPN generate significant excess healthcare costs and resource use amounting to $17 344 per patient per year.30
Innovative therapeutic strategies are now more than necessary to control both OIPN and CIPN in oncology.
Footnotes
Contributors: DB and DP led the conceptualisation, design and implementation of this research protocol. JF contributed to the conceptualisation, design and implementation of this research protocol, and is a contributing author for this manuscript. BP led the development of the statistical analysis plan. BG, CP and AE participated in the design of the protocol for interventions and assessments. FL and JV participated in the implementation of the protocol and the setup for the laboratory analyses. All the authors have read and approved the final manuscript.
Funding: This work is supported by funding from the CHU Clermont-Ferrand (AOI 2011), the Ligue Contre le Cancer and the APICIL Foundation.
Competing interests: The authors (DB and JF) declare a patent on the concept of polyamine-reduced diet to prevent oxaliplatin-induced neuropathy (FR 2967868 (A1)—USE OF FOOD COMPOSITION IN THE TREATMENT AND/OR PREVENTION OF NEUROPATHIC PAIN INDUCED BY AN ANTICANCER AGENT). Polydol cans are generously provided by Nutrialys Medical Nutrition.
Patient consent: Obtained.
Ethics approval: CPP Sud Est 1, Saint Etienne, France. The approval of the medical ethics committee was obtained on 20 December 2012. The protocol was declared to the competent French authority (Agence Nationale de Sécurité du Médicament et des produits de santé, Saint Denis, France) and registered under the number 2011-A00911–40. Authorisation was obtained on 10 October 2012.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Nordlinger B, Sorbye H, Glimelius B et al. Perioperative FOLFOX4 chemotherapy and surgery versus surgery alone for resectable liver metastases from colorectal cancer (EORTC 40983): long-term results of a randomised, controlled, phase 3 trial. Lancet Oncol 2013;14:1208–15. 10.1016/S1470-2045(13)70447-9 [DOI] [PubMed] [Google Scholar]
- 2.Beijers AJM, Mols F, Vreugdenhil G. A systematic review on chronic oxaliplatin-induced peripheral neuropathy and the relation with oxaliplatin administration. Support Care Cancer 2014;22:1999–2007. 10.1007/s00520-014-2242-z [DOI] [PubMed] [Google Scholar]
- 3.Balayssac D, Ferrier J, Descoeur J et al. Chemotherapy-induced peripheral neuropathies: from clinical relevance to preclinical evidence. Expert Opin Drug Saf 2011;10:407–17. 10.1517/14740338.2011.543417 [DOI] [PubMed] [Google Scholar]
- 4.Tofthagen C. Surviving chemotherapy for colon cancer and living with the consequences. J Palliat Med 2010;13:1389–91. 10.1089/jpm.2010.0124 [DOI] [PubMed] [Google Scholar]
- 5.Yothers G, O'Connell MJ, Allegra CJ et al. Oxaliplatin as adjuvant therapy for colon cancer: updated results of NSABP C-07 trial, including survival and subset analyses. J Clin Oncol 2011;29:3768–74. 10.1200/JCO.2011.36.4539 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Attal N, Bouhassira D, Gautron M et al. Thermal hyperalgesia as a marker of oxaliplatin neurotoxicity: a prospective quantified sensory assessment study. Pain 2009;144:245–52. 10.1016/j.pain.2009.03.024 [DOI] [PubMed] [Google Scholar]
- 7.Tofthagen C, Donovan KA, Morgan MA et al. Oxaliplatin-induced peripheral neuropathy's effects on health-related quality of life of colorectal cancer survivors. Support Care Cancer 2013;21:3307–13. 10.1007/s00520-013-1905-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mols F, Beijers T, Lemmens V et al. Chemotherapy-induced neuropathy and its association with quality of life among 2- to 11-year colorectal cancer survivors: results from the population-based PROFILES registry. J Clin Oncol 2013;31:2699–707. 10.1200/JCO.2013.49.1514 [DOI] [PubMed] [Google Scholar]
- 9.Hershman DL, Lacchetti C, Dworkin RH et al. Prevention and management of chemotherapy-induced peripheral neuropathy in survivors of adult cancers: American Society of Clinical Oncology Clinical Practice Guideline. J Clin Oncol 32:1941–67. 10.1200/JCO.2013.54.0914 [DOI] [PubMed] [Google Scholar]
- 10.Ganz PA. Why and how to study the fate of cancer survivors: observations from the clinic and the research laboratory. Eur J Cancer 2003;39:2136–41. 10.1016/S0959-8049(03)00489-1 [DOI] [PubMed] [Google Scholar]
- 11.Bell RF, Borzan J, Kalso E et al. Food, pain, and drugs: does it matter what pain patients eat? Pain 2012;153:1993–6. 10.1016/j.pain.2012.05.018 [DOI] [PubMed] [Google Scholar]
- 12.Rivat C, Richebé P, Laboureyras E et al. Polyamine deficient diet to relieve pain hypersensitivity. Pain 2008;137:125–37. 10.1016/j.pain.2007.08.021 [DOI] [PubMed] [Google Scholar]
- 13.Milovic V. Polyamines in the gut lumen: bioavailability and biodistribution. Eur J Gastroenterol Hepatol 2001;13:1021–5. 10.1097/00042737-200109000-00004 [DOI] [PubMed] [Google Scholar]
- 14.Ji R-R, Kohno T, Moore KA et al. Central sensitization and LTP: do pain and memory share similar mechanisms? Trends Neurosci 2003;26:696–705. 10.1016/j.tins.2003.09.017 [DOI] [PubMed] [Google Scholar]
- 15.Ferrier J, Bayet-Robert M, Pereira B et al. A polyamine-deficient diet prevents oxaliplatin-induced acute cold and mechanical hypersensitivity in rats. PloS ONE 2013;8:e77828 10.1371/journal.pone.0077828 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ramani D, De Bandt JP, Cynober L. Aliphatic polyamines in physiology and diseases. Clin Nutr 2014;33:14–22. 10.1016/j.clnu.2013.09.019 [DOI] [PubMed] [Google Scholar]
- 17.Cipolla B, Guillí F, Moulinoux J-P. Polyamine-reduced diet in metastatic hormone-refractory prostate cancer (HRPC) patients. Biochem Soc Trans 2003;31:384–7. 10.1042/BST0310384 [DOI] [PubMed] [Google Scholar]
- 18.Cipolla BG, Havouis R, Moulinoux JP. Polyamine contents in current foods: a basis for polyamine reduced diet and a study of its long term observance and tolerance in prostate carcinoma patients. Amino Acids 2007;33:203–12. 10.1007/s00726-007-0524-1 [DOI] [PubMed] [Google Scholar]
- 19.Cipolla BG, Havouis R, Moulinoux J-P. Polyamine reduced diet (PRD) nutrition therapy in hormone refractory prostate cancer patients. Biomed Pharmacother 2010;64:363–8. 10.1016/j.biopha.2009.09.022 [DOI] [PubMed] [Google Scholar]
- 20.Bouhassira D, Attal N, Alchaar H et al. Comparison of pain syndromes associated with nervous or somatic lesions and development of a new neuropathic pain diagnostic questionnaire (DN4). Pain 2005;114:29–36. 10.1016/j.pain.2004.12.010 [DOI] [PubMed] [Google Scholar]
- 21.Bouhassira D, Attal N, Fermanian J et al. Development and validation of the Neuropathic Pain Symptom Inventory. Pain 2004;108:248–57. 10.1016/j.pain.2003.12.024 [DOI] [PubMed] [Google Scholar]
- 22.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand 1983;67:361–70. 10.1111/j.1600-0447.1983.tb09716.x [DOI] [PubMed] [Google Scholar]
- 23.Moulinoux JP, Quemener V, Khan NA. Biological significance of circulating polyamines in oncology. Cell Mol Biol 1991;37:773–83. [PubMed] [Google Scholar]
- 24.Linsalata M, Russo F. Nutritional factors and polyamine metabolism in colorectal cancer. Nutrition 2008;24:382–9. [DOI] [PubMed] [Google Scholar]
- 25.Vickers AJ, Altman DG. Statistics notes: analysing controlled trials with baseline and follow up measurements. BMJ 2001;323:1123–4. 10.1136/bmj.323.7321.1123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Verbeke G. Linear mixed models for longitudinal data. New York: Springer, 2009. [Google Scholar]
- 27.Harris PA, Taylor R, Thielke R et al. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42:377–81. 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Park SB, Lin CSY, Krishnan AV et al. Long-term neuropathy after oxaliplatin treatment: challenging the dictum of reversibility. Oncologist 2011;16:708–16. 10.1634/theoncologist.2010-0248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.André T, Boni C, Navarro M et al. Improved overall survival with oxaliplatin, fluorouracil, and leucovorin as adjuvant treatment in stage II or III colon cancer in the MOSAIC trial. J Clin Oncol 2009;27:3109–16. 10.1200/JCO.2008.20.6771 [DOI] [PubMed] [Google Scholar]
- 30.Pike CT, Birnbaum HG, Muehlenbein CE et al. Healthcare costs and workloss burden of patients with chemotherapy-associated peripheral neuropathy in breast, ovarian, head and neck, and nonsmall cell lung cancer. Chemother Res Pr 2012;2012:913848. [DOI] [PMC free article] [PubMed] [Google Scholar]


