Abstract
Biochemical tests to detect B-type natriuretic peptide (BNP) or N-terminal pro-brain BNP (NT-proBNP) are useful diagnostic methods for patients with possible HF. These tests are valuable prognostic predictors for the entire spectrum of HF disease severity. Therefore, the measurements of BNP or NT-proBNP taken along with conventional clinical assessments may assist clinicians in deciding treatment. The following review briefly summarizes the available information regarding the clinical significance of BNP and NT-proBNP.
Keywords: Natriuretic peptide, Heart failure
INTRODUCTION
Heart failure is a progressive disease that is currently the most common cause of death among all cardiovascular diseases. The prevalence of heart failure continues to rise due to an increase in the proportion of elderly people as well as an increase in the number of patients with chronic heart failure who have survived acute heart failure because of new therapies [1,2]. Therefore, heart failure is a very important disease from both a medical and socioeconomic standpoint [3]. However, the clinical application of the Framingham diagnostic criteria for heart failure has low sensitivity and specificity and can lead to a variety of diagnoses.
Echocardiography is the gold standard for diagnosing heart failure; it is the most useful method and the basis for diagnostic and therapeutic decision-making. Its disadvantages include high cost and ineffectiveness in patients who are obese or have concomitant chronic lung diseases with respiratory distress. Therefore, biochemical markers have become useful and essential clinical tools for the easy and accurate diagnosis and prognosis of heart failure by clearly determining its incidence and stage [4]. B-type natriuretic peptide (BNP) and N-terminal pro-BNP (NT-proBNP) have been used as routine laboratory tests; a large number of studies have proven their clinical usefulness in the differential diagnosis of serious acute respiratory distress syndrome and the diagnosis and prognostic rating of heart failure [5,6]. However, both the biochemical markers that have been used in the past and those that have been recently reported on have limited application as diagnostic and prognostic tools and thus have limited general applicability. To address this problem, this paper focuses on the significance of BNP in patients with heart failure.
MAIN FEATURES
1. Physiology of BNP and NT-proBNP
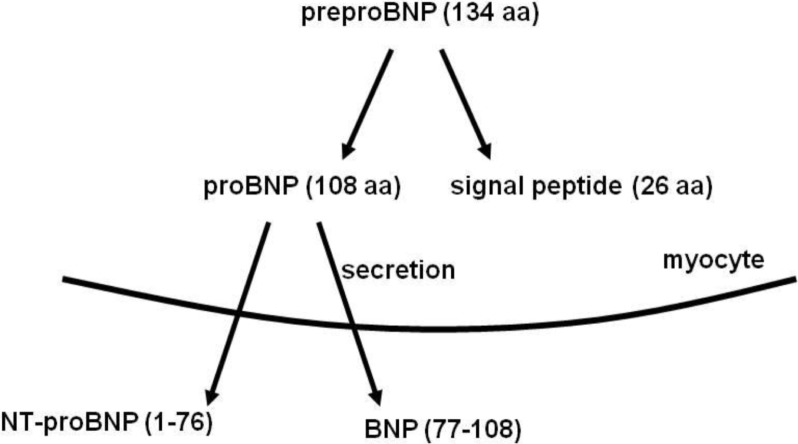
BNP was first discovered in the porcine brain and hence, it was named brain natriuretic peptide. Later, it was found to be secreted from the left ventricular myocardium in response to hemodynamic stimuli such as ventricular volume expansion and pressure overload [7]. The released proBNP enters the circulatory system after it is cleaved into the biologically active C-terminal of BNP and the biologically inactive, NT-proBNP (Fig. 1). proBNP is primarily synthesized and released in the ventricle in response to ventricular hemodynamic changes; therefore, it can reflect ventricular dysfunction better than other natriuretic peptides (NPs) [8]. Moreover, it is also known to cause strong vascular relaxation and to stimulate natriuresis. Unlike atrial natriuretic peptide (ANP), BNP does not usually cause immediate changes in normal hearts because its synthesis and secretion increases in response to hemodynamic stimuli over a considerable length of time [9]. The neurohormonal theory explains the major mechanism of heart failure; according to this theory, the level of BNP in the blood increases through activation of the natriuretic peptide system, which acts as a counter-regulatory system, to counteract the impaired neurohormonal balance in response to activation of the systems that induce vascular spasms (renin-angiotensin system, sympathetic nervous system, endothelin system). Therefore, BNP is primarily synthesized and released from the ventricle in response to ventricular hemodynamic changes and stress, and has been reported to indicate ventricular dysfunctions more efficiently than other NPs [10].
Fig. 1.
The release of BNP or NT-proBNP from the ventricular myocardium [16].
2. Test methods
BNP testing can be divided into point-of-care tests (POCTs), manually performed methods, and automated methods. The Triage® kit (Biosite Diagnostics, San Diego, CA, USA) was designed as an instant POCT, and is currently used. This tool enables a diagnosis using whole blood samples and thus, can bypass time-consuming processes, such as centrifugation, in emergencies [10]. Its main drawbacks are that it is expensive and requires manual examination of specimens. The main advantage and disadvantage of automated testing is its accuracy and long processing time, respectively. However, as a general chemical examination, systematic automation has the advantages of easy quality control and personnel cost reduction. These characteristic features of each method should be taken into account when choosing the test equipment; POCT can be more useful in situations that require rapid test results of patients in the emergency room or with acute symptoms such as acute respiratory distress, whereas automated equipment may be more useful for follow-up testing of outpatients, stable chronic patients, or for differential diagnostic purposes [10].
Recent research trends involve integral methods, such as the development of automated equipment including POCT kits and one-stop equipment for simultaneous measurements of other cardiac markers (troponin I, creatine kinase-MB) as well as simplified methods for repeated measurements at the bedside, which is similar to blood glucose testing. Various companies have developed different methods for measuring both BNP and NT-proBNP, the two substances simultaneously cleaved from proBNP. Either one may be used as a diagnostic or prognostic factor because they yield the same results. However, they have their respective advantages and disadvantages due to their different biological and chemical characteristics, and these differences must be taken into consideration during testing. It must be kept in mind that their standard values and ranges are not exchangeable; therefore, they should be used independently when interpreting the results [10].
3. Diagnosis using BNP or NT-proBNP
1). Patients in the emergency room or ones who are complaining of acute symptoms:
An accurate and rapid diagnosis is crucial for the diagnosis of patients who present to the emergency room or outpatient examination room with acute respiratory distress. The usability of a test greatly depends on its negative predictive value, which has vital significance as a differential diagnostic tool for serious acute respiratory distress syndrome, and can be very effective in the differential diagnosis of emergency room patients with heart failure. In general, the diagnostic accuracy is approximately 90% at the cut-off value of BNP (100 pg/mL) or NT-proBNP (162 pmol/L). Due to its high accuracy, the negative predictive value is useful not only in diagnosing heart failure but also in differentiating it from respiratory disorders that lead to respiratory distress [11–13]. In clinical reality, there are obvious differences in the cut-off values of cases of heart failure with acute symptoms and in those with stable chronic heart failure. The negative predictive value can greatly help in determining the cause of the patients’ respiratory distress.
2). Patients with stable chronic heart failure:
Most patients with chronic heart failure can maintain their condition unless they develop acute compensated or unresponsive heart failure. According to a study by Cowie et al. on patients with heart failure who presented to a heart failure clinic, BNP demonstrated 97% sensitivity and 84% specificity in the group with BNP values ≥76.4 pg/mL, which was more accurate in the diagnosis of heart failure than chest radiographs [14]. However, Tang et al. recently showed that among outpatients with stable chronic heart failure, approximately 21% showed normal BNP values, and this was mostly in young women with normal renal function and lower ventricular fibrillation frequencies [15]. Therefore, particular care should be taken to interpret the test values when examining outpatients with relatively stable chronic heart failure.
3). Treatment monitoring:
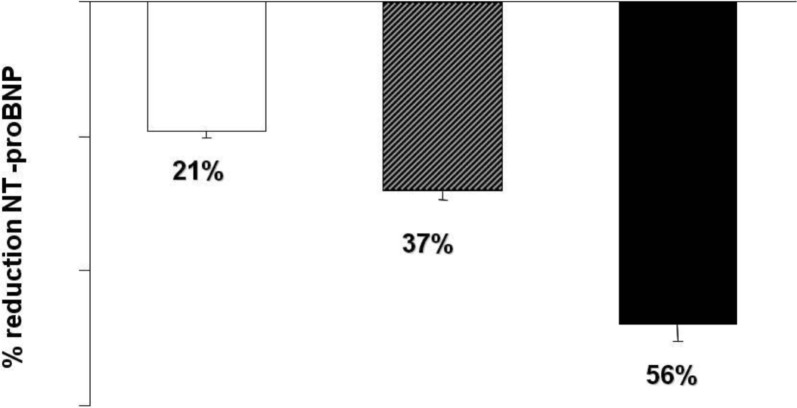
BNP is assumed to have a mechanism similar to a biochemical Swan-Ganz catheter and is thought to play a role similar to that of hemoglobin A1c in patients with diabetes mellitus or α-fetoprotein in patients with hepatoma. The development of various drugs that mitigate the course or symptoms of heart failure have prompted many discussions about the monitoring of therapeutic reactions or the possibility of drug titration. In a study on NT-proBNP, Lopez et al. reported that its concentration decreased by 21% in patients who maintained continuously decompensated heart failure, decreased by 37% in patients who maintained stable chronic heart failure, and decreased by approximately 56% in patients who fully recovered (Fig. 2) [12]. Further large-scale randomized clinical trials are required to determine whether this kind of monitoring can serve as a standard for therapeutic decision-making and drug dosage. However, the extent of NT-proBNP reduction is obviously associated with clinical improvement.
Fig. 2.
Percent reduction in N-terminal pro-brain BNP (NT-proBNP) levels according to the clinical course during hospitalization [12].
Because of the well-documented correlations between plasma BNP, NT-proBNP, concurrent haemodynamic measurements and indicators of left ventricular systolic function, it is possible that an adjustment of anti-heart failure therapy according to serial measurements of BNP (in addition to standard clinical assessment) may offer improved outcomes [16,17]. It has been well documented that converting enzyme inhibitors and diuretics lower BNP quite rapidly during the course of increased therapy in heart failure. Neurohormonal sub-studies from landmark randomized controlled trials of converting enzyme inhibitors in heart failure have suggested that the plasma neurohormonal status can predict the outcome of such therapy. These findings taken together were the rationale for a treatment of heart failure guided by plasma NT-proBNP [18]. However, neither BNP nor NT-proBNP was measured in neuro-hormonal sub-studies of randomized controlled trials of therapy in heart failure until the beta blocker therapy trials were launched. Recently, a French multicenter randomized study evaluated the benefit of BNP-guided therapy in CHF patients in clinical practice. This study showed that in optimally-treated CHF patients, a BNP-guided strategy reduced the risk of CHF-related death or hospital stays for CHF. The result was mainly obtained through an increase in angiotensin converting enzyme inhibitor and beta-blocker dosages [19]. However, because a cut-off value of BNP or NT-pro BNP for adjusting the anti-heart failure therapy was not determined, further studies are needed to determine the value.
4). Inadequate test results:
Some patients show results that are inconsistent with their clinical manifestations. BNP values can also vary according to the age and sex, as well as the comorbidity and medications administered. This should always be kept in mind, and care should be taken not to commit diagnostic errors by relying on a single-marker test (Table 1). Therefore, it seems important to use the BNP test not as a stand-alone test but rather as an auxiliary diagnostic tool for heart failure, and to consider the patient’s clinical condition in the diagnostic decision-making process [10].
Table 1.
Factors adversely affecting BNP outcomes in the diagnosis of CHF [16]
| Factors that can account for high BNP levels and no CHF |
| Age |
| Sex |
| Renal failure |
| Myocardial infarction |
| Lung disease with right-sided failure |
| Acute large pulmonary embolism |
| Factors that can account for low BNP levels with CHF |
| Obesity (BMI > 30 kg/m2) |
| Flash pulmonary edema (< 1−2 h) |
| CHF secondary to causes upstream from left ventricle |
| Acute mitral regurgitation |
| Mitral stenosis |
| Stable NYHA class I patients with low ejection fractions |
BNP: brain natriuretic peptide, CHF: chronic heart failure, BMI: body mass index, NYHA: New York Heart Association.
4. Prognosis
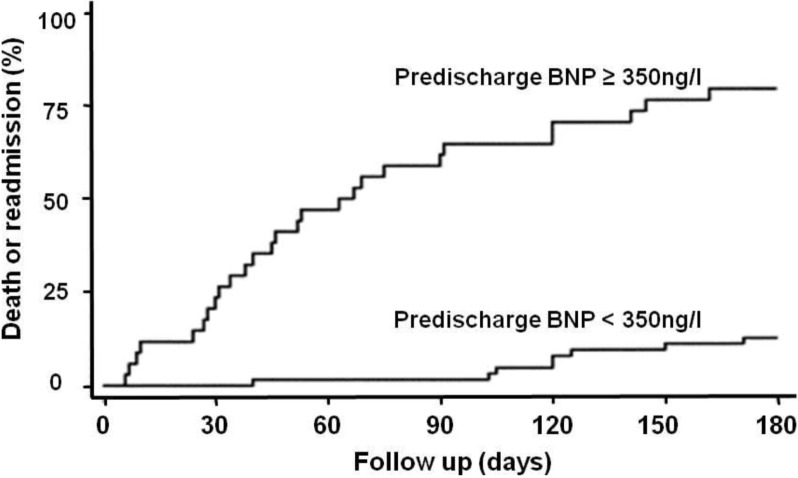
The BNP concentration is closely related to the incidence and severity of heart failure or absence thereof. In fact, its value increases with increasing severity, which has been categorized by the New York Heart Association functional classification. Therefore, it is very useful in predicting a patient’s status and establishing therapeutic strategies (Fig. 3) [17]. The criterion for the diagnostic value of a diagnostic test is its predictive power, which plays a crucial role in the process of therapeutic decision-making. From this point of view, BNP is an independent factor for the prediction of the incidence and mortality rates following myocardial infarction as well as heart failure [20]. Among all prognostic factors, such a clinical outcome is the most significant factor for predicting heart failure, and BNP is believed to be an essential prognostic factor that should be considered in future clinical trials [21].
Fig. 3.
Kaplan-Meier curves according to a predefined B-type natriuretic peptide (BNP) cut-off value (350 ng/l) [17].
CONCLUSION
The results of various studies have verified the high diagnostic significance of BNP and NT-proBNP for heart failure (Fig. 4). In clinical settings, they are considered objective “rule-out” tests in the emergency or outpatient departments. However, their use as stand-alone diagnostic tools is not recommended; rather, they should always be considered in conjunction with the patient’s clinical manifestations. Additionally, as important prognostic factors, they are expected to serve as an important basis for the diagnostic and therapeutic decision-making processes for heart failure.
Fig. 4.
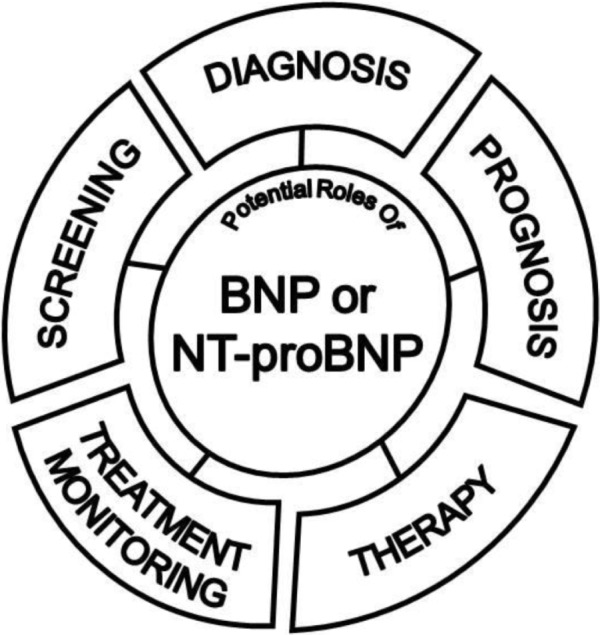
Diagram of the potential roles of B-type natriuretic peptide (BNP) [16].
REFERENCES
- 1.Mozaffarian D, Anker SD, Anand I, Linker DT, Sullivan MD, Cleland JG, Carson PE, Maggioni AP, Mann DL, Pitt B, Poole-Wilson PA, Levy WC. Prediction of mode of death in heart failure: the Seattle Heart Failure Model. Circulation. 2007;116:392–8. doi: 10.1161/CIRCULATIONAHA.106.687103. [DOI] [PubMed] [Google Scholar]
- 2.Roger VL. Epidemiology of heart failure. Circ Res. 2013;113:646–59. doi: 10.1161/CIRCRESAHA.113.300268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McKee PA, Castelli WP, McNamara PM, Kannel WB. The natural history of congestive heart failure: the Framingham study. N Engl J Med. 1971;285:1441–6. doi: 10.1056/NEJM197112232852601. [DOI] [PubMed] [Google Scholar]
- 4.Chowdhury P, Kehl D, Choudhary R, Maisel A. The use of biomarkers in the patient with heart failure. Curr Cardiol Rep. 2013;15:372–86. doi: 10.1007/s11886-013-0372-4. [DOI] [PubMed] [Google Scholar]
- 5.Gopal DJ, Iqbal MN, Maisel A. Updating the role of natriuretic peptide levels in cardiovascular disease. Postgrad Med. 2011;123:102–13. doi: 10.3810/pgm.2011.11.2500. [DOI] [PubMed] [Google Scholar]
- 6.Yoo BS, Kim WJ, Jung HS, Kim JY, Lee SW, Hwang SO, Yoon J, Choe KH. The Clinical experience of B-type natriuretic peptide blood concentrations for diagnosis in congestive heart failure - The single hospital experience based on the large clinical database. Korean Circ J. 2004;34:684–90. [Google Scholar]
- 7.Baxter GF. The natriuretic peptides. Basic Res Cardiol. 2004;99:71–5. doi: 10.1007/s00395-004-0457-8. [DOI] [PubMed] [Google Scholar]
- 8.Lee CY, Burnett JC., Jr Natriuretic peptides and therapeutic applications. Heart Fail Rev. 2007;12:131–42. doi: 10.1007/s10741-007-9016-3. [DOI] [PubMed] [Google Scholar]
- 9.Suttner SW, Boldt J. Natriuretic peptide system: physiology and clinical utility. Curr Opin Crit Care. 2004;10:336–41. doi: 10.1097/01.ccx.0000135513.26376.4f. [DOI] [PubMed] [Google Scholar]
- 10.Silver MA, Maisel A, Yancy CW, McCullough PA, Burnett JC, Jr, Francis GS, Mehra MR, Peacock WFt, Fonarow G, Gibler WB, Morrow DA, Hollander J, BNP Consensus Panel BNP Consensus Panel 2004: A clinical approach for the diagnostic, prognostic, screening, treatment monitoring, and therapeutic roles of natriuretic peptides in cardiovascular diseases. Congest Heart Fail. 2004;10:1–30. doi: 10.1111/j.1527-5299.2004.03271.x. [DOI] [PubMed] [Google Scholar]
- 11.Maisel AS, Krishnaswamy P, Nowak RM, McCord J, Hollander JE, Duc P, Omland T, Storrow AB, Abraham WT, Wu AH, Clopton P, Steg PG, Westheim A, Knudsen CW, Perez A, et al. Rapid measurement of B-type natriuretic peptide in the emergency diagnosis of heart failure. N Engl J Med. 2002;347:161–7. doi: 10.1056/NEJMoa020233. [DOI] [PubMed] [Google Scholar]
- 12.Bayes-Genis A, Santalo-Bel M, Zapico-Muniz E, Lopez L, Cotes C, Bellido J, Leta R, Casan P, Ordonez-Llanos J. N-terminal probrain natriuretic peptide (NT-proBNP) in the emergency diagnosis and in-hospital monitoring of patients with dyspnoea and ventricular dysfunction. Eur J Heart Fail. 2004;15:301–8. doi: 10.1016/j.ejheart.2003.12.013. [DOI] [PubMed] [Google Scholar]
- 13.Bettencourt P, Januzzi JL., Jr Amino-terminal pro-B-type natriuretic peptide testing for inpatient monitoring and treatment guidance of acute destabilized heart failure. Am J Cardiol. 2008;101:67–71. doi: 10.1016/j.amjcard.2007.11.026. [DOI] [PubMed] [Google Scholar]
- 14.Cowie MR, Struthers AD, Wood DA, Coats AJ, Thompson SG, Poole-Wilson PA, Sutton GC. Value of natriuretic peptides in assessment of patients with possible new heart failure in primary care. Lancet. 1997;350:1349–53. doi: 10.1016/S0140-6736(97)06031-5. [DOI] [PubMed] [Google Scholar]
- 15.Tang WH, Girod JP, Lee MJ, Starling RC, Young JB, Van Lente F, Francis GS. Plasma B-type natriuretic peptide levels in ambulatory patients with established chronic symptomatic systolic heart failure. Circulation. 2003;108:2964–6. doi: 10.1161/01.CIR.0000106903.98196.B6. [DOI] [PubMed] [Google Scholar]
- 16.Yoo BS. Biomarkers in heart failure: Focus on B-type natriuretic peptide. Korean J Intern Med. 2012;82:647–50. [Google Scholar]
- 17.Logeart D, Thabut G, Jourdain P, Chavelas C, Beyne P, Beauvais F, Bouvier E, Solal AC. Predischarge B-type natriuretic peptide assay for identifying patients at high risk of re-admission after decompensated heart failure. J Am Coll Cardiol. 2004;43:635–41. doi: 10.1016/j.jacc.2003.09.044. [DOI] [PubMed] [Google Scholar]
- 18.Troughton RW, Frampton CM, Yandle TG, Espiner EA, Nicholls MG, Richards AM. Treatment of heart failure guided by plasma aminoterminal brain natriuretic peptide (N-BNP) concentrations. Lancet. 2000;355:1126–30. doi: 10.1016/s0140-6736(00)02060-2. [DOI] [PubMed] [Google Scholar]
- 19.Jourdain P, Jondeau G, Funck F, Gueffet P, Le Helloco A, Donal E, Aupetit JF, Aumont MC, Galinier M, Eicher JC, Cohen-Solal A, Juilliere Y. Plasma brain natriuretic peptide-guided therapy to improve outcome in heart failure: the STARS-BNP Multicenter Study. J Am Coll Cardiol. 2007;49:1733–9. doi: 10.1016/j.jacc.2006.10.081. [DOI] [PubMed] [Google Scholar]
- 20.Choi HM, Yoo BS, Doh JH, JUNE NG, Kwak JJ, Lee SY, Ahn MS, Kim JY, Lee SH, Yoon JH. The optimal time of B-type natriuretic peptide sampling associated with post-myocardial infarction remodeling after primary percutaneous coronary intervention. Cardiovasc J Afr. 2013;24:165–70. doi: 10.5830/CVJA-2013-024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gopal DJ, Iqbal MN, Maisel A. Updating the role of natriuretic peptide levels in cardiovascular disease. Postgrad Med. 2011;123:102–13. doi: 10.3810/pgm.2011.11.2500. [DOI] [PubMed] [Google Scholar]