Abstract
Background
Modular metal-backed tibia components allow surgeons intraoperative flexibility. Although it is known that modular tibia components introduce the possibility for backside wear resulting from relative motion between the polyethylene insert and the tibial baseplate, it is not known to what degree variability in the conformity of the tibial polyethylene liner itself might contribute to backside wear.
Questions/purposes
The purpose of this study was to determine whether a flat, cruciate-retaining tibial polyethylene bearing generates less backside wear than a more conforming (curved) tibial polyethylene bearing in an analysis of specimens explanted during revision surgery.
Methods
The study included 70 total knee inserts explanted at revision surgery, all implanted and explanted by the same surgeon. Two different cruciate-retaining insert options in an otherwise similar knee system were used: one with a curved-on-flat (17) articular geometry and one with a highly conforming curved-on-curved design (53); both groups were sequential cohorts. The composite backside wear depth for the insert as well as the volume of backside wear was measured and compared between groups.
Results
The median linear backside-normalized wear for the posterior lipped inserts was 0.0063 mm/year (range, 0–0.085 mm/year), which was lower than for the curved inserts at 0.05 mm/year (range, 0.00003–0.14 mm/year) (p < 0.001). The median calculated volumetric backside-normalized wear for the posterior lipped inserts was 14.2 mm3/year (range, 0–282.8 mm3/year) compared with 117 mm3/year (range, 2.1–312 mm3/year) for the curved inserts (p < 0.001).
Conclusions
In this retrieval study, more conforming tibial inserts demonstrated more backside-normalized wear than the flatter designs. This suggests that in this modular total knee arthroplasty design, higher articular conformity to address the issues of high bearing contact stress comes at a price: increased torque transmitted to the backside insert-to-tray interface. We suggest further work be undertaken to examine newer insert designs to evaluate if our conclusions hold true with the newer generation locking mechanism, tibial tray finish and polyethylene designs, as more highly conforming tibial inserts are introduced into the market.
Level of Evidence
Level III, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
Modular metal-backed tibial components are used by most orthopaedic surgeons today. Modular tibial components allow intraoperative flexibility during the primary surgery and the possibility of isolated insert exchange during revision surgery, decreasing the complexity of the procedure and potentially avoiding bone loss associated with explantation of the entire tibial component. Modular implants, however, introduce a second bearing surface that is a potential site for particle generation. Relative motion between the polyethylene insert and the tibial base plate has been shown to be a source of wear and fine polyethylene particle generation that can lead to clinically significant osteolysis and implant loosening [2, 4, 9, 12, 13]. Retrieval studies have confirmed the presence of tibial insert polyethylene backside wear and shown a relationship to the tibial insert locking mechanism and implantation time [2, 4, 9, 12, 13].
In fixed-bearing knee designs, a certain amount of multidirectional motion can occur at the topside femoral implant/polyethylene insert articulation. During the past three decades we have observed that tibial insert topside topography evolved from “flat” to “curved” to increase articular conformity and try to address issues of polyethylene topside wear [4]. Backside wear and subsequent osteolysis were relatively rare beneath the original flat inserts but became an issue and a possible source of polyethylene wear and debris after the more rotationally conforming inserts were introduced. Although it is known that modular tibial components introduce the possibility for backside wear resulting from relative motion between the polyethylene insert and the tibial baseplate [2, 4, 9, 12, 13], it is not known to what degree that variability in the conformity of the tibial polyethylene insert itself might have on the tibial insert backside wear.
We had a unique opportunity to evaluate this by studying the amount of backside volumetric wear and the rate of wear that occurred in retrieved inserts from one knee system where the main implant variable in the study was the degree of topside conformity between the two insert designs.
We sought to determine whether a flat, cruciate-retaining tibial polyethylene bearing generates less backside wear than a more conforming (curved) tibial polyethylene bearing in an analysis of specimens explanted at revision TKA.
Patients and Methods
This study is based on 70 explanted PFC® total knee arthroplasty implants (DePuy/J&J, Warsaw, IN, USA) sent for evaluation to an established orthopaedic implant retrieval laboratory. The study was conducted under institutional review board approval.
All devices were implanted and retrieved by the same surgeon (RDS) between February 1988 and April 1996. During that time period, 895 consecutive primary posterior cruciate-retaining TKAs were implanted. The posterior lipped insert was used in 316 cases (35%) and the curved insert in the remaining 579 cases (65%). These two groups were generally sequential with the posterior lipped insert generally being used in the first 5 years (1988–1992) and the curved insert generally being used in the latter 5 years (1992–1996). The PFC® modular cruciate-retaining knee arthroplasty provided the option of a sagittally flat (posterior lipped insert) or a more conforming sagittally curved tibial insert. Both were prepared from identical polyethylene bar stock, gamma radiation sterilized in air, packaged in the same way, and, when implanted, articulated with the same femoral component.
When comparing both groups, no statistically significant difference was noted in relation to demographic characteristics such as age, sex, and body mass index (BMI) as well as physician-evaluated activity level with a mean age for the posterior lipped and curved inserts of 75.1 years (SD 12.7) and 68.2 years (SD 9.7), respectively. Mean BMI was 22.3 kg/m2 (SD 11.1) for the posterior lipped insert cohort and 25.3 kg/m2 (SD 7) for the curved insert cohort.
Through 2012, 29 of the 316 posterior lipped inserts (9%) and 77 of the 579 curved inserts (13%) (p = 0.13) were removed for reasons that included radiographic wear, synovitis, synovitis and lysis, instability, incidental exchanges for late infection, secondary patellar resurfacing, or revision of a loose prosthetic component. Three percent of the posterior lipped inserts and 11% of the curved inserts were removed for wear-related complications. Osteolysis was the reason for revision in 1.6% of the posterior lipped insert and 8% of the curved insert cases. We analyzed a total of 70 of the 106 explanted bearing surfaces (66%), 17 of the posterior lipped inserts and 53 of the curved liners. We selected these implants for analysis while excluding all explanted TKA implants that had a newer geometry (Sigma®, DePuy/J&J) and analyzing only explanted TKA implants with the original PFC® design so as not to introduce another uncontrolled variable.
The mean in situ duration for the series was 142 months (range, 15–289 months). The retrievals in the study were distributed as follows: 17 posterior lipped inserts (mean in situ duration 187 months [range, 15–289 months]) and 53 curved inserts (mean in situ duration 127 months [range, 45–204 months]) (Table 1).
Table 1.
Summary data on the study series
| Variable | Flat (posterior lipped insert) | Curved | Total |
|---|---|---|---|
| Number | 17 | 53 | 70 |
| Mean duration (months) | 187 | 127 | 142 |
| Range (months) | 15–289 | 45–204 |
A measurement of backside wear was possible because the components’ design incorporates topside datum surfaces that normally remain undamaged and unworn in vivo [1]. The thickness of the polyethylene inserts was measured from several topside reference points to the bottom surface using dial calipers and a dial indicator following a previously published method (Fig. 1) [1]. Design drawings were used to obtain the nominal initial thickness at the corresponding measurement points and backside wear depth was estimated by subtracting measured thickness from design thickness (Fig. 2). The composite backside wear depth for an insert was calculated by linear interpolation of the wear depth at each measurement point to the center point of the backside area. To estimate the volume of backside wear, the composite backside wear depth was multiplied by the backside surface area.
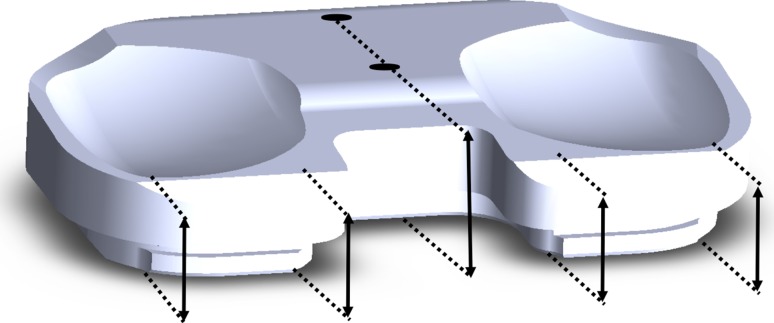
Fig. 1.
For backside wear estimates, thickness dimensions were taken at reference points indicated by the arrows on this schematic drawing. This typically does not show any proximal surface wear. All measurements were taken perpendicular to the surface planes.
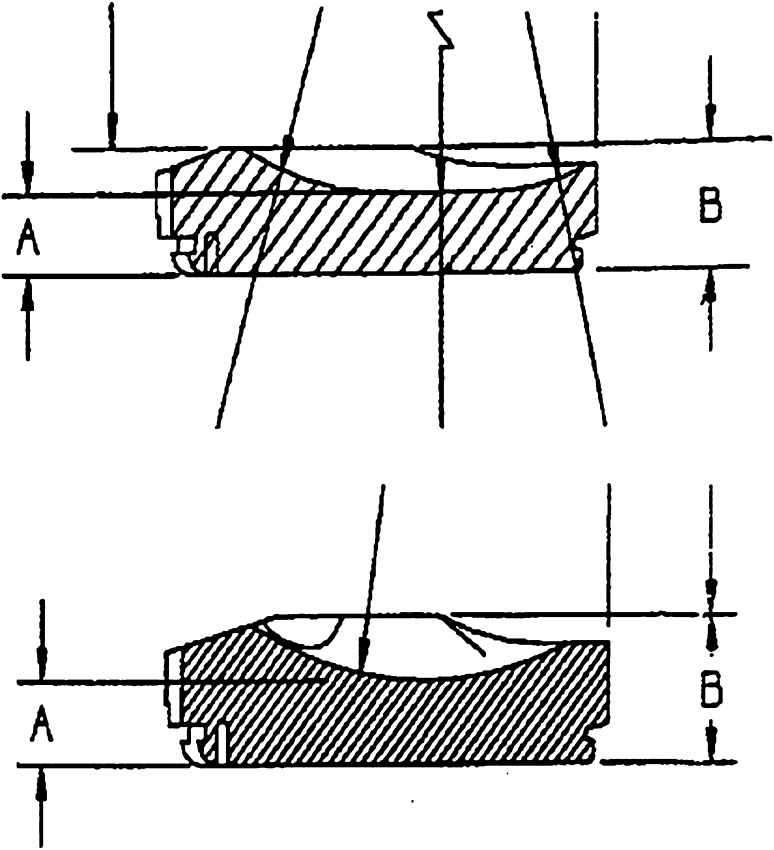
Fig. 2.
Composite backside wear depth of fixed-bearing inserts was determined by taking multiple measurements and interpolating to wear at the center of the insert (arrow). Inserts typically demonstrated a backside wear “wedge,” indicated here, with more wear posteriorly and medially. Backside wear volume was calculated by multiplying the composite wear depth by the backside area. (A) The topside datum surface serving as the topside reference point. (B) The articulating bottom surface that will exhibit thickness change resulting from wear.
To corroborate the backside-only wear that is the focus of this study, a measurement of total through-thickness wear of each insert was made (topside surface plus backside surface) by measuring the minimum thickness of both the medial and lateral condylar depressions using a dial indicator with 3-mm radius ball-end contacts (Fig. 3). Total wear penetration was calculated by subtracting the measured thickness dimension from the as-manufactured dimension. The backside wear data of each insert were considered valid only if the total through-thickness wear was equal to or exceeded the backside wear estimate. Five nonimplanted inserts were measured to confirm reference dimensions. A total of 30 measurements on nonimplanted inserts (six measurements on each one of the five sample inserts) showed a mean deviation from nominal thickness of −0.025 mm (SD = 0.056 mm; range, −0.152 mm to +0.076 mm). The manufacturing tolerance was 0.13 mm for all thickness measurements used for this study.
Fig. 3.
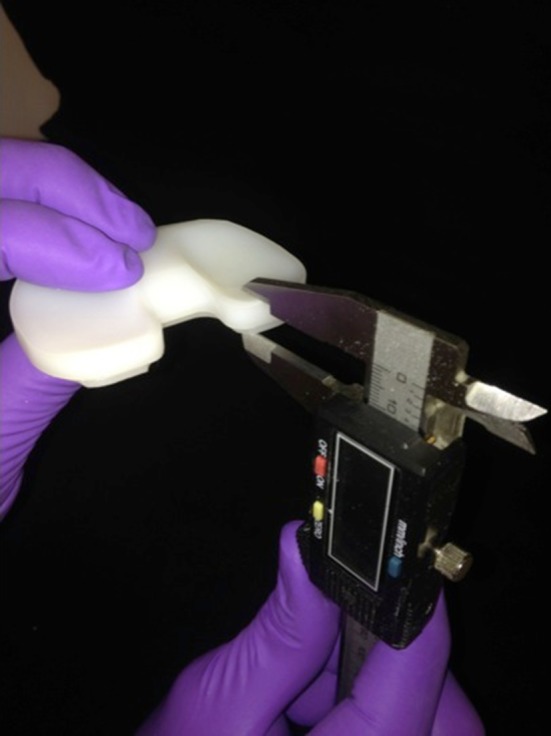
A dial indicator was used to measure retrieved insert thickness and thereby estimate total through-thickness wear in both the medial and lateral bearing areas, respectively.
Statistical Analysis
The dependence of normalized wear (wear/duration) on in vivo duration for each series was determined by calculating Spearman’s rho and significance assigned at p ≤ 0.05. Differences in normalized wear between groups were determined using the independent samples median test. The statistical package used was IBM® SPSS® Version 21 (IBM Corporation, Armonk, NY, USA).
Results
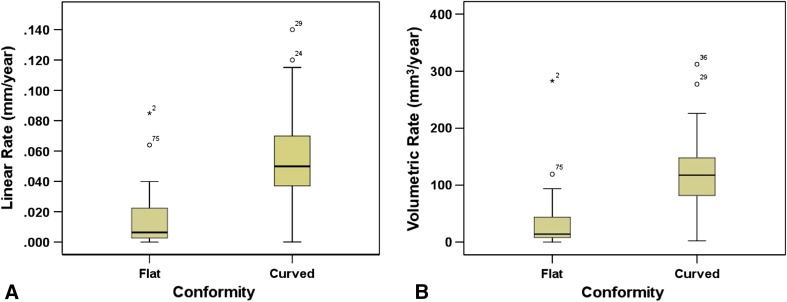
There was less linear and volumetric backside wear in the posterior lipped inserts than in the curved liners. The median linear backside-normalized wear for the posterior lipped inserts was 0.0063 mm/year (range, 0–0.085 mm/year), which was lower than for the curved inserts at 0.05 mm/year (range, 0.00003–0.14 mm/year) (p < 0.001). The median calculated volumetric backside-normalized wear for the PFC® posterior lipped inserts was 14.2 mm3/year (range, 0–282.8 mm3/year) compared with 117 mm3/year (range, 2.1–312 mm3/year) for the curved inserts (p < 0.001) (Table 2). The means of the linear backside-normalized wear and the volumetric backside-normalized wear for the two different insert geometries were compared showing a statistically significant difference (Fig. 4A–B).
Table 2.
Backside wear measurement results
| Measured variable | Flat (posterior lipped insert) | Curved | p value |
|---|---|---|---|
| Backside median linear wear rate (mm/year) | 0.0063 (range, 0–0.085) | 0.05 (range, 0.00003–0.14) | < 0.001 |
| Backside median volumetric rate (mm3/year) | 14.2 (range, 0–282.8) | 117 (range, 2.1–312) | < 0.001 |
Fig. 4A–B.
(A) Linear backside-normalized wear for the posterior lipped and curved inserts. (B) Volumetric backside-normalized wear for posterior lipped and curved inserts.
Discussion
Tibial insert backside wear is a known phenomenon in modular tibial TKAs and has been reported as a likely source of failure [2, 4, 9, 12, 13]. Many factors have been thought to affect tibial insert backside wear [2, 4, 9, 12, 13]; there are no reported studies that look specifically at topside tibial insert conformity in near isolation while eliminating most other variables.
The objective of the current study was to test the hypothesis that higher articular conformity of tibial inserts allows more tibiofemoral torque to be transmitted to the backside surface of the modular tibial inserts, driving increased polyethylene backside wear. The test series provided an opportunity for a direct comparison of less and more conforming insert geometries in the same total knee device with a single insert-to-tray locking geometry in the hands of one surgeon with extensive experience in implantation of this total knee system. It should be noted that this study focuses on backside wear driven by relative motion at the insert-to-tray interface as distinct from topside wear on the articular surface.
Limitations of the study include its retrospective design and the fact that the in situ implantation durations of the groups were not equal (although it is interesting to note that the curved inserts failed earlier than the posterior lipped inserts). The effect of creep on the wear rate measurements was not estimated and was not taken into consideration. This study reflects the experience of one surgeon working with one TKA system and therefore the study results may not reflect the experience of all surgeons or the outcome of all TKA devices. Furthermore, we do not know if any other TKAs have failed and have not returned to us for care and thus have been lost to followup and not included in the study cohort. We have also not included information regarding stability, ROM, and patient satisfaction, although age, sex, and BMI were not different between the two study cohorts. Other demographic characteristics that were not examined may have introduced certain bias.
Our study results demonstrated that more topside conforming tibial inserts experienced higher backside-normalized wear than the flatter less conforming tibial insert designs. The results of this study support the conclusion that, at least in modular total knee designs, higher articular conformity used to address the issues of high bearing contact stress comes at a price: a possible increase in torque transmitted to the backside insert-to-tray interface resulting in an increased backside wear rate that may lead to increased osteolysis and possible aseptic failure of the TKA.
Accurate measurement of actual material loss from retrieved knee bearings presents difficult challenges because gravimetric methods are not useful with retrievals and unworn reference dimensions are often unavailable. Therefore, clinical performance of knee bearings is often based on visual assessment of bearing surfaces rather than actual material lost [7, 8, 10]. Rather than surface deformation features, it is the polyethylene debris from both the abrasive and adhesive wear on the backside surface of the tibial inserts that is implicated as a cause for wear debris osteolysis [11, 13].
In a study by Fehring et al. [6], five variables were identified as possible attributers to polyethylene wear: (1) shelf life; (2) polyethylene finishing method (wood tumbling or not); (3) polyethylene sheet vendor; (4) patient sex; and (5) patient age. All the inserts in this study were gamma-in-air sterilized, a known gateway to oxidation and fatigue failure [3]. The study by Fehring et al. [6] did not consider the advent of the more conforming polyethylene inserts.
The measured wear on the inserts in the current study is comparable to wear measurements reported in other studies of modular fixed-bearing knees [3, 6]. A relevant quantitative wear comparison to the current study is offered by Li et al. [9] in a study of modular fixed-bearing knee retrievals. In their study, they documented 87 mg/year (93 mm3/year) of backside wear, which falls well within the range of 44 mm3/year to 115 mm3/year measured in the current study. A study by Engh et al. [5] reported a backside linear normalized wear of 0.02 mm/year and a backside volumetric rate of 44 mm3/year, also comparable to the current study.
In this study that evaluated retrieved tibial inserts, more conforming tibial inserts demonstrated more backside-normalized wear than the flatter designs. This suggests that in this modular TKA design, higher articular conformity may cause increased torque transition to the backside insert-to-tray interface. We suggest further work be undertaken to examine newer insert designs to evaluate if our conclusions hold true with the newer generation locking mechanism, tibial tray finish and polyethylene designs, as more highly conforming tibial inserts are introduced into the market.
Acknowledgments
We thank Lee Joseph for her continued support and assistance.
Footnotes
One of the authors (RS) has received consulting fees from Smith & Nephew (Memphis, TN, USA) (less than USD 10,000). One of the authors (RDS) has received consulting fees from DePuy (Warsaw, IN, USA) (less than USD 10,000) and royalties from DePuy (greater than USD 1,000,000). One or more of the authors (EMC, JHS) has received institutional funding from DePuy, ConforMIS (Bedford, MA, USA), and Biomet (Warsaw, IN, USA).
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research ® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was conducted at the New England Baptist Hospital, Boston, MA USA. The biomechanical material analysis was conducted at the Thayer School of Engineering, Dartmouth College, Hanover, NH, USA.
References
- 1.Berry DJ, Currier JH, Mayor MB, Collier JP. Knee wear measured in retrievals: a polished tray reduces insert wear. Clin Orthop Relat Res. 2012;470:1860–1868. doi: 10.1007/s11999-012-2248-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Conditt MA, Stein JA, Noble PC. Factors affecting the severity of backside wear of modular tibial inserts. J Bone Joint Surg Am. 2004;86:305–311. doi: 10.2106/00004623-200402000-00013. [DOI] [PubMed] [Google Scholar]
- 3.Currier BH, Currier JH, Collier JP, Mayor MB, Scott RD. Shelf life and in vivo duration. Impacts on performance of tibial bearings. Clin Orthop Relat Res. 1997;342:111–122. doi: 10.1002/jor.1100150116. [DOI] [PubMed] [Google Scholar]
- 4.Engh GA, Dwyer KA, Hanes CK. Polyethylene wear of metal-backed tibial components in total and unicompartmental knee prostheses. J Bone Joint Surg Br. 1992;74:9–17. doi: 10.1302/0301-620X.74B1.1732274. [DOI] [PubMed] [Google Scholar]
- 5.Engh GA, Zimmerman RL, Parks NL, Engh CA. Analysis of wear in retrieved mobile and fixed bearing knee inserts. J Arthroplasty. 2009;24(Suppl):28–32. doi: 10.1016/j.arth.2009.03.010. [DOI] [PubMed] [Google Scholar]
- 6.Fehring TK, Murphy JA, Hayes TD, Roberts DW, Pomeroy DL, Griffin WL. Factors influencing wear and osteolysis in press-fit condylar modular total knee replacements. Clin Orthop Relat Res. 2004;428:40–50. [DOI] [PubMed]
- 7.Garcia RM, Kraay MJ, Messerschmitt PJ, Goldberg VM, Rimnac CM. Analysis of retrieved ultra-high-molecular-weight polyethylene tibial components from rotating-platform total knee arthroplasty. J Arthroplasty. 2009;24:131–138. doi: 10.1016/j.arth.2008.01.003. [DOI] [PubMed] [Google Scholar]
- 8.Kelly NH, Fu RH, Wright TM, Padgett DE. Wear damage in mobile-bearing TKA is as severe as that in fixed-bearing TKA. Clin Orthop Relat Res. 2011;469:123–130. doi: 10.1007/s11999-010-1557-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Li S, Scuderi G, Furman BD, Bhattacharyya S, Schmieg JJ, Insall JN. Assessment of backside wear from the analysis of 55 retrieved tibial inserts. Clin Orthop Relat Res. 2002;404:75–82. doi: 10.1097/00003086-200211000-00013. [DOI] [PubMed] [Google Scholar]
- 10.Lu YC, Huang CH, Chang TK, Ho FY, Cheng CK, Huang CH. Wear-pattern analysis in retrieved tibial inserts of mobile-bearing and fixed-bearing total knee prostheses. J Bone Joint Surg Br. 2010;92:500–507. doi: 10.1302/0301-620X.92B4.22560. [DOI] [PubMed] [Google Scholar]
- 11.Schmalzried TP, Jasty M, Rosenberg A, Harris WH. Polyethylene wear debris and tissue-reactions in knee as compared to hip-replacement prostheses. J Appl Biomater. 1994;5:185–190. doi: 10.1002/jab.770050302. [DOI] [PubMed] [Google Scholar]
- 12.Wasielewski RC, Galante JO, Leighty RM, Natarajan RN, Rosenberg AG. Wear patterns on retrieved polyethylene tibial inserts and their relationship to technical considerations during total knee arthroplasty. Clin Orthop Relat Res. 1994;299:31–43. [PubMed] [Google Scholar]
- 13.Wasielewski RC, Parks N, Williams I, Surprenant H, Collier JP, Engh G. Tibial insert undersurface as a contributing source of polyethylene wear debris. Clin Orthop Relat Res. 1997;345:53–59. doi: 10.1097/00003086-199712000-00009. [DOI] [PubMed] [Google Scholar]