Abstract
An intracranial tumor is a rare cause of secondary parkinsonism. Our patient presented to our clinic for recently-developed asymmetric parkinsonism without pyramidal signs. However, a meningioma located in the sphenoidal ridge was identified upon imaging studies. This case suggests that additional causes should be considered when approaching patients with parkinsonism and that imaging studies can provide useful information to make accurate diagnoses.
Keywords: Parkinsonism, Meningioma, PET
INTRODUCTION
Parkinsonism is a neurological syndrome that presents with tremor, rigidity, bradykinesia and postural instability. Parkinsonism is largely divided into primary and secondary parkinsonism. Primary parkinsonism is caused by neurodegerative disease, whereas secondary parkinsonism is due to many causes such as intoxication, metabolic disorders, cerebrovascular disorders, head injury, intracranial infection or intracranial tumor. Among these causes, an intracranial tumor is a rare cause of secondary parkinsonism [1–5]. Here, we report a patient who visited our hospital for parkinsonism and an intracranial meningioma was found in brain imaging.
CASE REPORT
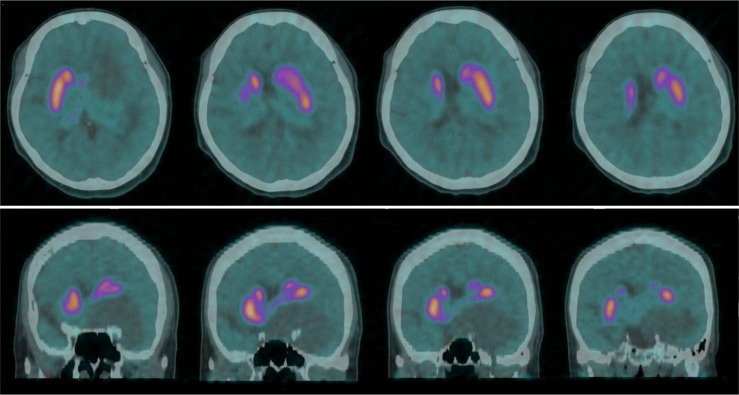
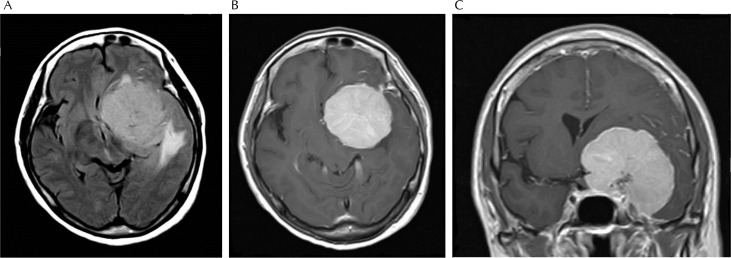
A 58-year-old female visited our hospital for 2 months of resting tremor. She had been treated for hypercholesterolemia, and did not report any familial history. Both of her hands showed 6–7 Hz of frequency and less than 1 cm of amplitude, and the tremor was more prominent in the right hand. When she stretched her arm forward, a similar degree of postural tremor was observed in both hands. Finger and foot tapping showed mild bradykinesia in the right hand and right foot. Physical examination revealed cogwheel rigidity in both arms, but with a prominence in the right. Her standing posture and postural stability appeared normal, and her walking pattern was also fair except reduced arm swing on the right side. Her eyeballs showed no saccadic slowing or eye movement limitation. The Unified Parkinson’s Disease Rating Scale part III was 17 points. Muscle strength and sensation were normal in all four limbs, and deep tendon reflexes of both knees and biceps tendons were also normoactive. The results of complete blood cell count, serum chemistry tests, and thyroid function tests were within the normal range. A 18F-FP-CIT PET scan showed a normal strength of radioisotope uptake in both striatum, but the left caudate nucleus and putamen were displaced dorsally (Fig. 1). A brain magnetic resonance imaging (MRI) revealed a lobulated and well-defined mass (5.67 × 5.01 cm) in the left sphenoid ridge (Fig. 2). The mass had iso-signal intensity on T1-weighted imaging and high signal intensity on T2 FLAIR imaging, and the central region showed low signal intensity on both T1 and T2 weighted imaging, which was consistent with calcification. The mass compressed the left cavernous sinus, and the cerebral midline was shifted toward the right side. Edema around the mass was also noted.
Fig. 1.
The 18F-FP-CIT uptake was normal in both striata, but the location of the left striatum was displaced dorsally.
Fig. 2.
The MR FLAIR image revealed a large mass around the left basal ganglia with surrounding edema (A), and the T1 weighted image showed well-defined lobules and a discrete margin of the mass (B, C).
She underwent surgical removal of the tumor and histological study confirmed meningioma. Her symptoms improved gradually and disappeared 2 months after surgery without complications.
DISCUSSION
An intracranial tumor is a rare cause of parkinsonism, and parkinsonism is also rarely documented in patients with intracranial tumors. Krauss and colleagues reported that parkinsonism was observed in 0.3% of patients with a supratentorial tumor [1] and 0.4% of those with astrocytoma in the basal ganglia or thalamus [2].
Parkinsonism can be associated with any type of brain tumor located in the intracranial space. Meningioma is the most common tumor associated with parkinsonism, and when this tumor is located in the sphenoidal ridge, frontal or parietal area, it is more likely to induce parkinsonism symptoms [1,3].
The pathogenesis of tumor-induced parkinsonism can be explained as a disruption in neural circuits. First, the mass effect of the tumor can directly compress or distort the axon of the presynaptic dopaminergic neuron. If a tumor is near the midbrain, it could compress the cell body of the nigral dopaminergic neuron [4]. Next, the output pathway of the basal ganglia circuit from postsynaptic cells to cortex can be influenced by the tumor. This hypothesis is supported by a documented case of a parkinsonism patient with a tumor located in the supplementary motor area [5]. Finally, a supratentorium tumor might induce ipsilateral transtentorial herniation and compression of the contralateral midbrain by a margin of contralateral tentorium. This explanation is also applicable in cases of supratentorial subdural hemorrhage that causes parkinsonism [6].
This patient had recently developed parkinsonism and was asymmetric without any focal neurological symptoms, pyramidal signs, abnormal reflexes, or history of exposure to drugs or toxic substances. This finding could have been regarded as primary parkinsonism, however, the United Kingdom Parkinson’s Disease Society Brain Bank diagnostic criteria for idiopathic Parkinson’s disease (IPD) [7] states that a brain tumor should be excluded to make an IPD diagnosis. Therefore, all possible causes of parkinsonism should be considered to make accurate diagnoses, and imaging studies can be very useful to diagnose and treat parkinsonism in some cases.
REFERENCES
- 1.Krauss JK, Paduch T, Mundinger F, Seeger W. Parkinsonism and rest tremor secondary to supratentorial tumours sparing the basal ganglia. Acta neurochi. 1995;133:22–9. doi: 10.1007/BF01404943. [DOI] [PubMed] [Google Scholar]
- 2.Krauss JK, Nobbe F, Wakhloo AK, Mohadjer M, Vach W, Mundinger F. Movement disorders in astrocytomas of the basal ganglia and the thalamus. J Neurol Neurosurg Psychiatry. 1992;55:1162–7. doi: 10.1136/jnnp.55.12.1162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bostantjopoulou S, Katsarou Z, Petridis A. Relapsing hemiparkinsonism due to recurrent meningioma. Parkinsonism Relat Disord. 2007;13:372–4. doi: 10.1016/j.parkreldis.2006.07.017. [DOI] [PubMed] [Google Scholar]
- 4.Choi KH, Choi SM, Nam TS, Lee MC. Astrocytoma in the third ventricle and hypothalamus presenting with parkinsonism. J Korean Neurosurg Soc. 2012;51:144–6. doi: 10.3340/jkns.2012.51.3.144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Straube A, Sigel K. Parkinsonian syndrome caused by a tumour of the left supplementary motor area. J Neurol Neurosurg Psychiatry. 1988;51:730–1. doi: 10.1136/jnnp.51.5.730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Park B, Song SK, Hong JY, Lee PH. Parkinsonsim due to a chronic subdural hematoma. J Mov Disord. 2009;2:43–4. doi: 10.14802/jmd.09011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gibb WR, Lees AJ. The relevance of the Lewy body to the pathogenesis of idiopathic Parkinson’s disease. J Neurol Neurosurg Psychiatry. 1988;51:745–52. doi: 10.1136/jnnp.51.6.745. [DOI] [PMC free article] [PubMed] [Google Scholar]