Abstract
Although falls are a serious health risk for community dwelling older adults, their ascertainment has been complicated by issues such as recall and reporting biases. We examined a novel method, individualized tailored calendars, to accurately ascertain falls in older adults. A convenience sample of 125 cognitively normal participants enrolled in longitudinal studies of healthy aging at xxxxxx center was followed prospectively for 12 months. Tailored calendar journal pages were used to document falls daily and returned by mail monthly. Participants received a $5 gift card incentive for each month returned. Participants returned 1,487 of 1,500 calendar months over the 12 month follow up for 99.1 % compliance rate. There were 154 falls reported. Tailored calendar journals and incentives may be effective in ascertaining falls among community dwelling older adults. This tool could improve the accuracy of outcome measures for occupational therapy interventions.
Keywords: tailored interventions, calendar journals, fall reporting
Introduction
Falls pose a significant health risk to older adults as about 30% of community-dwelling older adults, age 65 or older fall annually (Tromp, Pluijm, Smith et al. 2001). Reliably ascertaining falls and accurately calculating days to a fall among community older adults are important to assess the effectiveness of occupational therapy fall prevention interventions. While the risk of fall related injuries increases with age (Etman, Wijlhuizen, van Heuvelen, Chorus, & Hopman-Rock, 2012), the ability to reliably self-report a fall event accurately becomes more difficult (Ganz, Higashi, & Rubenstein, 2005). Retrospective self-reported fall rates likely under-report falls (Mackenzie, Byles, & D'Este, 2006). Long term tracking methods that exceed 3 months result in inaccurate fall reports (Cummings, Nevitt, & Kidd, 1988; Ganz et al., 2005). Weekly or monthly intervals yield more accurate fall data and optimize participant engagement (Ganz et al., 2005; Lamb et al., 2005). The current gold standard for reporting falls is prospective recording of falls using various techniques including calendars (Tinetti & Williams, 1998), diaries (Davison, Bond, Dawson, Steen, & Kenny, 2005; Latham et al., 2003) or post cards (Hale, Delaney, & Cable, 1993). However, even prospective fall event reporting is subjective and lacks precision (Hale et al., 1993). Potential bias in subjective reports of falls makes interpreting the outcome of fall interventions difficult. For example, older adults who have limitations with memory or executive function are unreliable in reporting falls (Ganz et al., 2005; Perry et al., 2012). Participants who experienced multiple falls may also be less likely to comply with fall reporting methods. Possible reasons for lack of compliance may be related to: the characteristics of these fallers that make completing the fall diaries difficult (e.g. poor memory); shame; or even denial (Perry et al., 2012). The lack of a reliable, precise report of the primary endpoint of fall studies (particularly those with time to fall event as outcome) is a major barrier to conducting studies of fall prevention. Developing a more reliable system of ascertaining falls is vital for evaluating and comparing occupational therapy fall prevention intervention studies.
There are four strategies used in other fields that may inform the development of more reliable fall ascertainment system to assess the outcome of occupational therapy fall interventions. First, the use of landmark dates as an anchor to life events can assist in more accurate recall of health events such as illness and hospital admissions (van der Vaart & Glasner, 2010). In retrospective reports, recall of events was enhanced by using landmark life events such as births, deaths, or holidays compared to interview alone (Belli, Shay, & Stafford, 2001), although recall is not enhanced when the landmarks are not personal (van der Vaart & Glasner, 2010). Using personal landmark dates could improve accuracy of reporting the date when a fall occurred. Another strategy commonly used by occupational therapy practitioners that has the potential to enhance compliance with reporting is tailoring or using personalized strategies targeted to an individual based on their unique preferences. Tailored print media are created especially for an individual based on knowledge of that person. Tailoring has been an effective method to improve participation in other behavioral studies (Kreuter, Caburnay, Chen, & Donlin, 2004;,and could be useful to develop a fall reporting system. Creating fall calendar journals that are developed with individual choices in mind may improve the use of the document. Another useful strategy to improve compliance is telephonic coaching. Coaching via telephone is both cost-effective and successful in eliciting desired behavior in interventions involving diabetes maintenance, diet and physical activity change (Goode, Morrison, & Malone, 2012; Sacco, Morrison, & Malone, 2004). Using a telephonic coaching session to incorporate reporting falls on a daily basis may increase compliance. Finally, providing financial incentives (e.g., $5 coupons) to participants, has been shown to enhance participant compliance and retention better than use of alternative incentives or no incentive at all (Giuffrida & Torgerson, 1997; Rudy, Estick, Kerr, & Menzel, 1994). An incentive to return calendar pages monthly may improve compliance in returning calendar journal pages.
Through improved ascertainment of fall data, we can more precisely estimate the effectiveness of fall prevention intervention. We propose that an easy to use, tailored calendar journal will aid in recall of falls. To our knowledge, this strategy has not been previously employed in fall prevention intervention trials. The purpose of this study is to determine if providing an individually tailored calendar journal to record falls daily, supported with one telephonic coaching session and monthly financial incentives to return the calendar pages will result in a high rate of compliance among cognitively normal, healthy, community dwelling older adults with a low risk of falls.
Methods
Overview and setting
A twelve-month prospective study examined the effectiveness of using tailored calendar journals with pages returned monthly to track participant falls among cognitively normal older adults who participate in longitudinal studies of memory and aging at xxxxxx center. In this single group, prospective observational study, participants were assessed for covariates known to be related to falls. They received training to use the calendar journal for daily recording of falls over the 12-month follow-up period. If participants experienced a fall, they were asked to immediately complete a form to provide details about the fall. After monthly calendar journal pages were returned, the fall report was followed-up with a telephone interview to verify details such as location and nature of the fall, and if medical care was needed.
Participants
Detailed information regarding recruitment, enrollment, and clinical assessment of the participants has been published (Johnson, Wilkins, & Morris, 2006). Briefly, participants were community-dwelling individuals in longitudinal studies of memory and aging without health conditions that could adversely affect participation in the study (e.g., renal failure requiring dialysis). Each participant received an annual clinical assessment. We invited individuals to participate in the current study if they met the following criteria: (1) age 65 or older; (2) normal cognition as indicated by Clinical Dementia Rating (CDR) of 0 (Morris, 1993) at their most recent clinical and cognitive assessment. Of the 153 participants who met eligibility criteria, 142 were able to be contacted for enrollment in this study. Five of these participants did not respond to further telephone contact attempts. After a phone interview, 12 participants declined to consent. The final sample included 125 participants (Table 1). Two participants died during the follow up period. One participant was lost to follow up after the death of his spouse. Recruitment and follow up occurred from May of 2010 until November of 2011. Study protocols were approved by xxxxx Human Subjects Committee and written informed consent was obtained from all participants after thorough review of informed consent form.
Table 1.
Participant Demographics
| Total sample | |
|---|---|
| Age y (SD) | 74.4 (5.71) |
| Female (%) | 78.0(62.40) |
| Race | |
| African American (%) | 4 (3.20) |
| White (%) | 120 (96.0) |
| American Indian or Alaskan Native (%) | 2(0.08)a |
| Education in years (SD) | 15.5 (2.67) |
| Number of prescription medications (SD) | 3.72 (2.77) |
| ADL performanceb (SD) | 27.5 (0.82) |
| Alcohol problemc (SD) | 0.27 (0.71) |
Note: N=125
One participant noted race as both White and American Indian or Alaskan Native
Older Adult Resources Services Activity of Daily Living Scale score/28 with higher scores indicating more independence in ADL
Short Michigan Alcoholism Screening Test—Geriatric Version where score >2 indicates probable alcohol problem.
Materials
During the clinical examination, experienced clinicians interviewed the participant and a collateral source using a standardized protocol to generate a CDR (Morris, 1993). The CDR is determined based on performance in six domains: memory, orientation, judgment and problem solving, community affairs, home and hobbies, and personal care and has established reliability (Morris et al., 1997). CDR scores range from 0 (cognitive normality) to 3 (severe dementia). Participants in this study all were CDR 0 at their entry into the study.
Upon enrolling, each participant received a 10-15 minute telephone interview to ascertain fall risk factors shown in previous studies to be related to falls. Alcohol abuse is a risk factor for falls (Rubenstein, 2006; Mukamal, Mittleman et al. 2004) and was measured using the Short Michigan Alcoholism Screening Test—Geriatric Version, (Blow, 1991) a 10-item interview validated for the older adult population. Scores of 2 or more are indicative of a probable alcohol problem (Blow, 1991). Limitations in the ability to perform activities of daily living (ADL) and instrumental ADL (IADL) have been associated with an increased risk of falls (Mahoney, Sager et al. 1994; Davis, Ross et al. 1999). The Older American Resources and Services (OARS) ADL scale was used to determine individuals’ level of ADL/IADL impairment (Fillenbaum, 1988). The OARS is brief and easy to administer over the telephone. Respondents are asked about their ability to perform 14 activities, and responses are scored on a 0-2 scale, with higher scores indicating greater independence. Prescription medications are a risk factor for falls (Hartikainen, Lonnroos, & Louhivuori, 2007); medication names and dosages were reported by participant; total number of medications used on a monthly basis was summed.
To gather information necessary to tailor the calendars, participants were asked to identify dates of personal importance such as birthdays and anniversaries of family and friends. Participants were also given the option to include religious and non-secular holidays in the calendar. Additionally, color scheme preferences and a choice of cover photo were options given to each individual. Once necessary information was obtained, the calendars were created using Calendar Maker software.
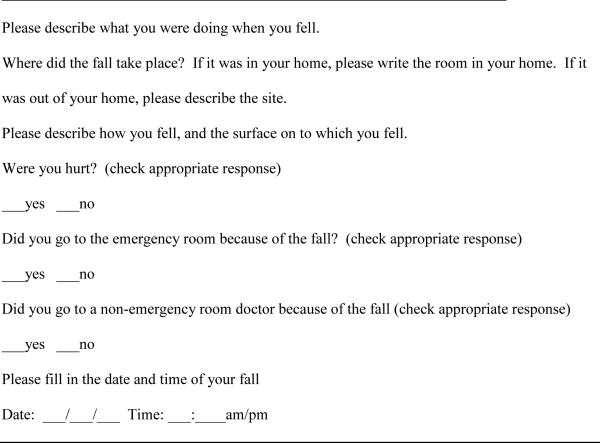
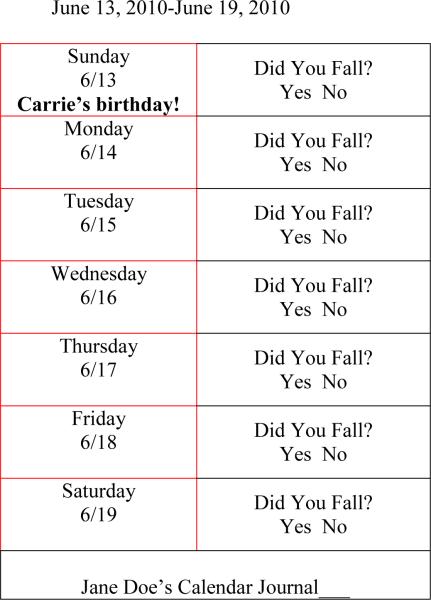
A 12-month calendar journal, tailored with birthdays and other important personal dates, was produced for each participant to record whether or not a fall occurred daily using calendar software. Personal dates were provided as a cue to help accurately recall when a fall event occurred. Each page of the 10.8cm × 14.0 cm large print calendar journal had space to record one week's fall outcome on each page. The journal was spiral bound and contained 16 point Arial font. The calendar journal included fall survey pages to record details of a fall (Figure 1) and was customized with a name and personalized color scheme (Figure 2).
Figure 1.
Fall Form: The above form was filled out by participants if they fell. Participants were advised to complete the fall form as soon as possible following a fall.
Figure 2.
The above is a sample page (one week) from the personalized Calendar Journal. Participants were advised to complete the calendar journal daily by circling the appropriate answer.
Procedures
Participants received the calendar journal in the mail and underwent a telephonic training session to learn to accurately use the calendar journal. Verbal and written instruction was provided for where to place the journal, how to record details of falls using a fall form, and how to return calendar journal pages each month. Participants were given the definition of a fall (unintentional movement to the floor, the ground, or an object below knee level (Lamb et al., 2005) and provided with examples.
Each month participants were mailed a reminder to return their calendar pages monthly using a provided self-addressed stamped envelope. Pages not returned within 1 week of the due date or that were incomplete prompted a telephone call to the participant. Upon receipt of the pages, a $5 gift card was mailed to the participant. A report of a fall triggered a phone interview to verify that the reported fall met the definition and to ascertain details of the fall. Participants who did not want to record the fall using the calendar journal were given the option of answering the journal questions via phone with the study coordinator; although no participants chose this option
Results
Demographic characteristics are presented in table one. Of the 125 participants, the majority were female (78%) and white (96%). The mean age was 74 years. Participants were well educated (average 15 years). All participants were CDR 0 (cognitively normal) and all other covariates describing the healthy community dwelling sample are presented in Table 1. Participant's reported an average of 7.53 (SD 7.24) personal events (e.g. birthdays) recorded on the calendar journal. There were an average of 5.92 (SD 6.67) personal dates (birthdays, anniversaries) and 1.61(1.43) holidays selected by participants to include on their calendar. There were 1,500 possible months of data to be collected over the one year period. Of this 1,500, only 13 months of data were missing. This resulted in a 99.1% compliance rate.
The 125 participants had a total of 154 falls over the 365 day follow-up period. The number of falls reported by individuals ranged from 0-12 falls with 60 percent of individuals (n=75) reporting at least one fall. Thirty-six of the 75 fallers reported only one fall. Of the 73 participants who completed a phone interview (about their first fall), 14 reported seeking medical attention. No one reported hospitalization. The majority of the falls occurred in the community during walking.
Discussion
The main finding of this study is that a systematic approach to fall ascertainment using tailoring, anchor dates, telephonic coaching, monthly reminder with self-addressed stamped envelope, and monthly incentives is an effective strategy to obtain fall reports from healthy, cognitively intact community dwelling older adults. Older adults were compliant with each aspect of the study and highly engaged in reporting falls.
The effectiveness of fall prevention studies is dependent upon accurate self-reporting of the outcome of falls, yet falls are likely underreported (Hannan et al., 2010; Sattin, 1992). This study supports previous findings of underreporting of falls by demonstrating a higher than expected fall rate (60 percent) among this healthy, cognitively intact older adults with an expected 30 percent or lower risk of falls (Tinetti, Speechley, & Ginter, 1988).
This study identifies a set of strategies from the literature that can enhance fall ascertainment and provides preliminary efficacy that tailoring (Kreuter et al., 2004), use of personal landmark dates (van der Vaart & Glasner, 2010) on a fall reporting calendar, telephonic coaching (Sacco et al., 2004) and incentives (Rudy et al., 1994) may yield a high compliance rate and more accurate rate of falls. The telephonic coaching allowed each participant to ask questions and ensured that they understood the procedures. Monthly contact with participants via mail served as a cue and provided the resources (e.g., self-addressed stamped envelope) at the time it was needed to return the calendar pages. Gift card incentives were an interim reminder of participation in the fall study as well as remuneration for participation. Instructing participants to fill out calendars on a daily basis may also have contributed to the positive reporting outcome. In asking participants to recall information (like a fall) the unit of time should be small enough to maintain precision (Freedman, Thornton, Camburn, Alwin, & Young-DeMarco, 1988). For older adults, recall beyond one month has been shown to produce inaccurate results (Ganz et al., 2005). Calendars displayed one week of days, and participant reporting took place each month. This timeline may have allowed for optimal accuracy yet was not so burdensome to deter participants from completing the calendars.
Despite advances in wearable technology capable of recording falls, there is no currently available method to objectively ascertain falls in the community. While compliance in reporting efforts was high, this remains a subjective report of falls and there is currently no gold standard to know if these reports were more or less accurate than other methods. In addition, there was no comparison group for this single group observational study. Future studies comparing methods are warranted. This is a particularly motivated, and well-educated group. It is possible that not all populations would respond with such high levels of compliance.
While this study was focused on gathering fall data on a relatively small population, it stands to reason that these methods are generalizable to many other situations requiring data collection from study participants and/or patients. Tailoring interventions as well as tracking methods can be beneficial to both patients and occupational therapy providers. By individualizing methods, retention and engagement rates improve (Beutler, Zetzer, & Yost, 1997).
In conclusion, falls in older adults remain a significant public health concern and significantly impact the participation of older adults. This study adds to the body of literature demonstrating the efficacy of tailored tracking methods in ascertaining fall data from community dwelling older adults with normal cognition. The tailored approach used in this study returned a higher than expected result. It is possible that a fall ascertainment technique that uses tailoring, daily reporting intervals, coaching and incentives contributes to more reliable reporting of falls. Two advantages to using tailored calendars to anchor memory of events are: improvement of the quality of retrospective data being collected by helping the client to relate timing of events visually and mentally, and simplicity of recording events using a calendar rather than a questionnaire (Freedman et al., 1988). In this study, the tailored calendars had high compliance. This study provides a framework with which fall data can be ascertained from additional populations. We recommend further studies, to further strengthen the body of literature on ascertaining fall data in community dwelling older adults.
Acknowledgments
Funding
This work was supported by the National Institutes of Health Alzheimer's Disease Research Center, [grant number P50AG005681]; Healthy Aging Senile Dementia, [grant number P01AG003991]; and Antecedent Biomarkers for AD: The Adult Children Study, [grant number P01AG026276].
Dr. Stark reports funding by National Institutes of Health grant NIA P50AG05681-27; Housing and Urban Development grant MOLHH0196-09 and Centers for Disease Control grant 1K01DD00033301. Dr. Stark has received research support from The Retirement Research Foundation and the Barnes Jewish Hospital Foundation.
He receives research support from Eli Lilly/Avid Radiopharmaceuticals and is funded by National Institutes of Health grants P50AG005681; P01AG003991; P01AG026276 and U19AG032438.
Footnotes
Disclosures:
Mrs. Silianoff reports no disclosures.
Ms. Byan reports no disclosures.
Mrs. Conte reports no disclosures.
Dr. John C. Morris discloses neither he nor his family owns stock or has equity interest (outside of mutual funds or other externally directed accounts) in any pharmaceutical or biotechnology company. Dr. Morris has participated or is currently participating in clinical trials of antidementia drugs sponsored by the following companies: Janssen Immunotherapy, and Pfizer. Dr. Morris has served as a consultant for Lilly USA.
Conflicts of interest
None declared.
References
- Belli RF, Shay WL, Stafford FP. Event History Calendars and Question List Surveys: A direct comparison of interviewing methods. Public Opinion Quarterly. 2001;65(1):45–74. doi: 10.1086/320037. [DOI] [PubMed] [Google Scholar]
- Beutler LE, Zetzer H, Yost E. onken LS, Blaine JD, Boren JJ, editors. Tailoring interventions to clients: effects on engagement and retention Beyond the Therapeutic Alliance: Keeping the Drug Dependent Individual in Treatment. 1997:85–109. [PubMed] [Google Scholar]
- Blow F. Michigan alcoholism screening test - Geriatric Version (MAST-G) University of Michigan Alcohol Research Center; Ann Arbor: 1991. [Google Scholar]
- Cummings SR, Nevitt MC, Kidd S. Forgetting Falls. The limited recall of falls in the elderly. Journal of American Geriatric Society. 1988;36(7):613–616. doi: 10.1111/j.1532-5415.1988.tb06155.x. [DOI] [PubMed] [Google Scholar]
- Davison J, Bond J, Dawson P, Steen IN, Kenny RA. Patients with recurrent falls attending Accident & Emergency benefit from multifactorial intervention— a randomised controlled trial. Age and Ageing. 2005;34(2):162–168. doi: 10.1093/ageing/afi053. [DOI] [PubMed] [Google Scholar]
- Etman A, Wijlhuizen GJ, van Heuvelen MJG, Chorus A, Hopman-Rock M. Falls incidence underestimates the risk of fall-related injuries in older age groups: a comparison with the FARE (Falls risk by Exposure). Age & Ageing. 2012;41(2):190–195. doi: 10.1093/ageing/afr178. [DOI] [PubMed] [Google Scholar]
- Fillenbaum GG. Multidimensional functional assessment of older adults: The Duke Older Americans Resources and Services procedures. Lawrence Erlbaum Associates, Inc.; 1988. [Google Scholar]
- Freedman D, Thornton A, Camburn D, Alwin D, Young-DeMarco L. The Life History Calendar: A Technique for Collecting Retrospective Data. Sociological Methodology. 1988;18:37–68. [PubMed] [Google Scholar]
- Ganz DA, Higashi T, Rubenstein LZ. Monitoring Falls in Cohort Studies of Community-Dwelling Older People: Effect of the Recall Interval. Journal of the American Geriatrics Society. 2005;53(12):2190–2194. doi: 10.1111/j.1532-5415.2005.00509.x. doi: 10.1111/j.1532-5415.2005.00509.x. [DOI] [PubMed] [Google Scholar]
- Giuffrida A, Torgerson D. Should we pay the patient? Review of financial incentives to enhance patient compliance. BMJ. 1997;315:703–707. doi: 10.1136/bmj.315.7110.703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goode A, Morrison A, Malone J. Telephone delivered interventions for physical activity and dietary behavior change: An updated systematic review. American Journal of Preventative Medicine. 2012;42(1):81–88. doi: 10.1016/j.amepre.2011.08.025. [DOI] [PubMed] [Google Scholar]
- Hale WA, Delaney MJ, Cable T. Accuracy of patient recall and chart documentation of falls. The Journal of the American Board of Family Practice/American Board of Family Practice. 1993;6(3):239. [PubMed] [Google Scholar]
- Hannan MT, Gagnon MM, Aneja J, Jones RN, Cupples LA, Lipsitz LA, Kiel DP. Optimizing the Tracking of Falls in Studies of Older Participants: Comparison of Quarterly Telephone Recall With Monthly Falls Calendars in the MOBILIZE Boston Study. American Journal of Epidemiology. 2010;171(9):1031–1036. doi: 10.1093/aje/kwq024. doi: 10.1093/aje/kwq024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartikainen S, Lonnroos E, Louhivuori K. Medication as a risk factor for falls: critical systematic review. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences. 2007;62(10):1172–1181. doi: 10.1093/gerona/62.10.1172. [DOI] [PubMed] [Google Scholar]
- Johnson DK, Wilkins CH, Morris JC. Accelerated weight loss may precede diagnosis in Alzheimer disease. Arch Neurol. 2006;63(9):1312–1317. doi: 10.1001/archneur.63.9.1312. [DOI] [PubMed] [Google Scholar]
- Kreuter MW, Caburnay CA, Chen JJ, Donlin MJ. Effectiveness of individually tailored calendars in promoting childhood immunization in urban public health centers. American Journal of Public Health. 2004;94(1):122–127. doi: 10.2105/ajph.94.1.122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lamb SE, Jørstad-Stein EC, Hauer K, Becker C, on behalf of the Prevention of Falls Network, E., & Outcomes Consensus, G. Development of a Common Outcome Data Set for Fall Injury Prevention Trials: The Prevention of Falls Network Europe Consensus. Journal of the American Geriatrics Society. 2005;53(9):1618–1622. doi: 10.1111/j.1532-5415.2005.53455.x. doi: 10.1111/j.1532-5415.2005.53455.x. [DOI] [PubMed] [Google Scholar]
- Latham NK, Anderson CS, Lee A, Bennett DA, Moseley A, Cameron ID. A randomized, controlled trial of quadriceps resistance exercise and vitamin D in frail older people: the Frailty Interventions Trial in Elderly Subjects (FITNESS). Journal of the American Geriatrics Society. 2003;51(3):291–299. doi: 10.1046/j.1532-5415.2003.51101.x. [DOI] [PubMed] [Google Scholar]
- Mackenzie L, Byles J, D'Este C. Validation of self-reported fall events in intervention studies. Clinical Rehabilitation. 2006;20(4):331–339. doi: 10.1191/0269215506cr947oa. doi: 10.1191/0269215506cr947oa. [DOI] [PubMed] [Google Scholar]
- Morris JC. The Clinical Dementia Rating (CDR. Current version and scoring rules. Neurology. 1993;43(11):2412–2414. doi: 10.1212/wnl.43.11.2412-a. [DOI] [PubMed] [Google Scholar]
- Morris JC, Ernesto C, Schafer K, Coats M, Leon S, Sano M, Woodbury P. Clinical Dementia Rating training and reliability in multicenter studies. Neurology. 1997;48(6):1508–1510. doi: 10.1212/wnl.48.6.1508. [DOI] [PubMed] [Google Scholar]
- Perry L, Kendrick D, Morris R, Dinan S, Masud T, Skelton D, Iliffe S. Completion and return of fall diaries varies with participants’ level of education, first language, and baseline fall risk. Journals of Gerontology Series A: Biological Sciences & Medical Sciences. 2012;67(2):210–214. doi: 10.1093/gerona/glr175. [DOI] [PubMed] [Google Scholar]
- Rubenstein LZ. Falls in older people: epidemiology, risk factors and strategies for prevention. Age and Ageing. 2006;35(suppl 2):ii37–ii41. doi: 10.1093/ageing/afl084. [DOI] [PubMed] [Google Scholar]
- Rudy E, Estick P, Kerr M, Menzel L. Research incentives: Money versers gifts. Nursing Research. 1994;44(4):252–255. doi: 10.1097/00006199-199407000-00012. [DOI] [PubMed] [Google Scholar]
- Sacco WP, Morrison AD, Malone JI. A brief, regular, proactive telephone “coaching” intervention for diabetes: Rationale, description, and preliminary results. Journal of Diabetes and its Complications. 2004;18(2):113–118. doi: 10.1016/S1056-8727(02)00254-4. doi: http://dx.doi.org/10.1016/S1056-8727(02)00254-4. [DOI] [PubMed] [Google Scholar]
- Sattin R. Falls among older adults: a public health perspective. annual Review of Public health. 1992;13:489–508. doi: 10.1146/annurev.pu.13.050192.002421. [DOI] [PubMed] [Google Scholar]
- Tinetti ME, Speechley M, Ginter SF. Risk Factors for Falls among Elderly Persons Living in the Community. New England Journal of Medicine. 1988;319(26):1701–1707. doi: 10.1056/NEJM198812293192604. doi: doi:10.1056/NEJM198812293192604. [DOI] [PubMed] [Google Scholar]
- Tinetti ME, Williams CS. The effect of falls and fall injuries on functioning in community-dwelling older persons. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences. 1998;53(2):M112–M119. doi: 10.1093/gerona/53a.2.m112. [DOI] [PubMed] [Google Scholar]
- Tromp AM, Pluijm SMF, Smit JH, et al. Fall-risk screening test: a prospective study on predictors for falls in community-dwelling elderly. Journal of Clinical Epidemiology. 2001;54(8):837–844. doi: 10.1016/s0895-4356(01)00349-3. [DOI] [PubMed] [Google Scholar]
- van der Vaart W, Glasner T. Personal landmarks as recall aids in survey interviews. Field Methods. 2010;23(1):37–56. doi: 10.1177/1525822X10384367. [Google Scholar]