Abstract
In 1978, when the Task Panel report to the US President’s Commission on Mental Health emphasized the importance of improving health care and easing the pain of those suffering from emotional distress syndromes including loneliness, few anticipated that this issue would still need to be addressed 40 years later. A meta-analysis (Masi et al., 2011) on the efficacy of treatments to reduce loneliness identified a need for well-controlled randomized clinical trials focusing on the rehabilitation of maladaptive social cognition. We review assessments of loneliness and build on this meta-analysis to discuss the efficacy of various treatments for loneliness. With the advances made over the past 5 years in the identification of the psychobiological and pharmaceutical mechanisms associated with loneliness and maladaptive social cognition, there is increasing evidence for the potential efficacy of integrated interventions that combine (social) cognitive behavioral therapy with short-term adjunctive pharmacological treatments.
Life in America in the 21st century is unlike any period in human history. People are living longer than ever before, and the rise in the Internet has transformed how Americans work, play, search, shop, study, communicate, and relate to one another. People are increasingly connected digitally, but the prevalence of loneliness (perceived social isolation) also appears to be rising. From a prevalence estimated to be 11–17% in the 1970s (Peplau, Russell, & Heim, 1979), loneliness has increased to over 40% in middle aged and older adults1 (Edmondson, 2010; Perissinotto, Cenzer, & Covinsky, 2012). Over the past 40 years, loneliness has also become more widespread overseas (e.g., Victor, Scambler, Bowling, & Bond, 2005; Randall, 2012; Victor & Yang, 2012; Stickley et al., 2013). For instance, a 2010 survey from Statistics New Zealand shows that 33% of individuals aged 15 and above experienced loneliness in the four weeks preceding the survey. In the U.K., prevalence of loneliness is estimated between 5%–6% (for individuals reporting feeling “often” lonely), 21%–31% (for individuals reporting feeling “sometimes” lonely; Victor et al., 2005; Victor & Yang, 2012), and prevalence rates as high as 45% have been reported throughout the U.K. according to an online survey that took place in March 2010 (Griffin, 2010). As the prevalence of loneliness rises, evidence accrues that loneliness is a major risk factor for poor physical and mental health outcomes.
Definition of Loneliness
Psychiatrist Fromm-Reichmann (1959) raised awareness of loneliness and noted the need for a rigorous, scientific definition of loneliness. In the decades that followed, loneliness as a psychological condition was characterized, and measures for quantifying individual differences were introduced (e.g., Lynch & Convey, 1979; Peplau, Russell, & Heim, 1979; Russell, Peplau, & Cutrona, 1980; Weiss, 1973). Loneliness corresponds to a discrepancy between an individual’s preferred and actual social relations (Peplau & Perlman, 1982). This discrepancy then leads to the negative experience of feeling alone and/or the distress and dysphoria of feeling socially isolated even when among family or friends (Weiss, 1973). This definition underscores the fact that feeling alone or lonely does not necessarily mean being alone nor does being alone necessarily mean feeling alone (see J. T. Cacioppo et al., this issue). One can feel lonely in the crowd or in a marriage. Reciprocally, one may enjoy being alone (a pleasant state defined as solitude; Tillich, 1959) at times in order to reach personal growth experiences (such as those achieved through solitary meditation or mindfulness exercises) or to simply take a temporary break from dealing with the demands of modern life.
Loneliness emphasizes the fact that social species require not simply the presence of others but also the presence of significant others whom they can trust, who give them a goal in life, with whom they can plan, interact, and work together to survive and prosper (J. T. Cacioppo & Patrick, 2008). Moreover, the physical presence of significant others in one’s social environment is not a sufficient condition. One needs to feel connected to significant others to not feel lonely. Accordingly, one can be temporarily alone and not feel lonely as they feel highly connected with their spouse, family, and/or friends – even at a distance. Subjectivity and perception of the friendly or hostile nature of one’s social environment is, thus, a characteristic of loneliness. As comedian Robin Williams said: “I used to think the worst thing in life was to end up all alone. It’s not. The worst thing in life is to end up with people who make you feel all alone” (2009). Although this crucial component of loneliness helps better differentiate subjective social isolation (loneliness) from objective social isolation, it has led occasionally to a conflation of loneliness and other dysphoric states (e.g., social anxiety, depression) in which a person’s subjective experiencing of their social environment plays also a crucial role.
A main challenge for physicians and mental health clinicians has been, therefore, to become sufficiently informed about the scientific definition of loneliness so that other mental disorders were not mistakenly diagnosed and treated when loneliness was either the primary presenting problem or the cause of the depression for which treatment was sought (Booth, 2000). For instance, because loneliness and depression share some characteristics and a correlation ranging from .38 to .71 (cf., Booth, 2000; J. T. Cacioppo et al., 2006), many clinicians believed, for decades, that loneliness was simply an aspect of depression with no distinct concept worthy of study (cf. Young, 1982). There is now considerable evidence showing that loneliness and depression are separable and that loneliness increases the risk for depression (J. T. Cacioppo et al., 2006; Heinrich & Gullone, 2006). In 1980, for instance, Weeks et al. administered loneliness and depression scales to undergraduate college students. Using data from 333 subjects, they concluded that loneliness and depression, though correlated with each other, were “clearly different constructs.” These results have been replicated and extended in recent longitudinal research (J. T. Cacioppo et al., 2010; VanderWeele et al., 2011), and reinforced Ostrov and Offer’s (1978) clinical observation that a potential difference between loneliness and depression was that while both are filled with helplessness and pain, loneliness is characterized by the hope that all would be perfect if only the lonely person could be united with another longed for person.
Who Can Feel Lonely?
Loneliness does not discriminate. Although loneliness is more likely in populations who are at risk for social alienation, isolation, and separation (such as older individuals who live alone and are isolated from friends and families; patients with psychiatric disorders; patients with long-term health conditions that limit their communicative capacities or mobility; and/or stigmatized groups; for reviews see Andersson, 1998, J. T. Cacioppo in this special issue), anyone can feel lonely at any time. For instance, the same objective social relationship can be perceived as caring and protective or as exploitive and isolating based on a host of factors including an individual’s prior experiences, current attributions, and overall preference for social contact (J. T. Cacioppo, Cacioppo, Capitanio, & Cole, 2015). Accordingly, loneliness is not limited to older adults who are infirmed and live alone but is evident across the lifespan and is even evident in people surrounded by large numbers of other young adults or with numerous contacts/followers/friends on social media (e.g., Qualter et al., this issue).
Dimensions of Loneliness
Loneliness is a complex construct that includes three related facets or dimensions: 1) Intimate loneliness; 2) Relational loneliness; and 3) Collective loneliness (Hawkley et al., 2005; Hawkley, Gu, Luo, & Cacioppo, 2012). These three dimensions match the three dimensions surrounding one’s attentional space (Hall, 1963, 1966; Figure 1): intimate space (the closest space surrounding a person), social space (the space in which people feel comfortable interacting with family and acquaintances), and the public space (a more anonymous space). These three dimensions of loneliness also appear to share some correspondence with the structure of human personal social networks identified by Weiss (1973) and Dunbar (2014; Figure 1). The translation of these three dimensions into a structured attentional personal space (Ortigue, Megevand, Perren, Landis, & Blanke, 2006; Ortigue et al., 2003; Rizzolatti et al., 1983, 1987) are interesting in light of analyses of the mental organization for people’s loneliness/social connection (Figure 1). In loneliness, these three dimensions have been found in various populations, such as college students (Hawkley et al., 2005; McWhirter, 1990b) and older adults in the U.S. (Hawkley et al., 2005; Peplau & Perlman, 1982), and in young and older adults in China. (Hawkley et al., 2012)2. Each dimension also corresponds to different types of loneliness.
Figure 1.
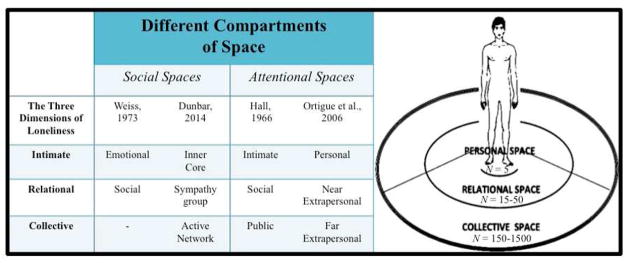
The three dimensions of loneliness and different compartments of space.
Intimate Loneliness
Intimate loneliness, or what Weiss (1973) termed emotional loneliness, refers to the perceived absence of a significant someone (e.g., a spouse), that is, a person one can rely on for emotional support during crises, who provides mutual assistance, and who affirms one’s value as a person. This form of intimate connection often has considerable self-other overlap (such as that observed between close friends e.g., husband-wife, best-friends; Hall, 1966; Ortigue et al., 2003, 2006). This dimension corresponds to what Dunbar described as the inner core, which can include up to 5 people (the “support clique”) and comprises the people we rely on for emotional support during crises (Dunbar, 2014).
A population-based study of middle-age and older adults showed that the best (negative) predictor of intimate loneliness was marital status, indicating that intimate partners tend to be a primary source of attachment, emotional connection, and emotional support for adults (Hawkley et al., 2005). These results are consistent with several studies indicating that having a significant partner/spouse is associated with lower levels of intimate loneliness and, reciprocally that losing a partner (through divorce or widowhood) is linked to greater intimate loneliness (e.g., J. T. Cacioppo & Patrick, 2008; Hughes et al., 2004; Lopata, Heinemann, & Baum, 1982; Russell, 1982; Waite & Gallagher, 2001; Weiss, 1973).
Relational Loneliness
The second dimension is relational loneliness, or what Weiss (1973) termed social loneliness. It refers to the perceived presence/absence of quality friendships or family connections, that is, connections from the “sympathy group” (Buys & Larson, 1979; Dunbar, 2014) within one’s relational space. According to Dunbar the “sympathy group” can include among 15 and 50 people and comprises core social partners whom we see regularly and from whom we can obtain high-cost instrumental support (e.g. loans, help with projects, child care; Dunbar, 2014).
The relational space is delimitated by the multi-modal (visual, auditory, and tactile) space that permits face-to-face communications and interactions. Like intimate loneliness, social loneliness is found in women as well as men, although there is some evidence that this dimension may tend to play a slightly greater role in influencing loneliness in women than in men (Hawkley et al., 2005). The best (negative) predictor of relational loneliness in middle-aged and older adults is the frequency of contact with significant friends and family, even after statistically controlling for the other two dimensions of loneliness (Hawkley et al., 2005). Nevertheless, it is not the quantity of friends, but the quality of significant friends/confidants that counts (Hawkley et al., 2008). This point is crucial when diagnosing loneliness.
Collective Loneliness
The third dimension is collective loneliness, an aspect that Weiss (1973) did not identify in his qualitative studies. Collective loneliness refers to a person’s valued social identities or “active network” (e.g., group, school, team, or national identity) wherein an individual can connect to similar others at a distance in the collective space. As such, this dimension may correspond to what Dunbar (2014) described as the outermost social layer, which can include among 150 and 1500 people (the “active network”) who can provide with information through weak ties (Granovetter, 1973), as well as low-cost support (Dunbar, 2014). The best (negative) predictor of collective loneliness found in middle-age and older adults was the number of voluntary groups to which individuals belonged: the more voluntary associations to which individuals belonged, the lower their collective loneliness, again even after statistically controlling for the two other dimensions. This dimension of loneliness is found in women as well as men but tends to be slightly more heavily weighted in men than in women (Hawkley et al., 2005). The emergence of a collective dimension of loneliness suggests that we may have evolved the capacity for and motivation to form relationships not only with other individuals but also with groups (e.g., villages or armies), with the consequence being the promotion of social identification and cooperation in adverse conditions (e.g., competition, hunting, or warfare; Brewer, 2004). The identification with and investments in the group, in turn, may increase the likelihood of the continuity of the group, its members, and their individual genetic legacy (J. T. Cacioppo, Cacioppo, & Boomsma, 2014).
Consequences of Loneliness
Loneliness can contribute to a constellation of physical and psychiatric dysfunctions and/or psychosocial risk factors, including depressive symptomatology (J. T. Cacioppo et al., 2006; J. T. Cacioppo, Hawkley, & Thisted, 2010; VanderWeele, Hawkley, Thisted, & Cacioppo, 2011), alcoholism (Akerlind & Hornquist, 1992), suicidal thoughts (Rudatsikira, Muula, Siziya, & Twa-Twa, 2007), aggressive behaviors, social anxiety, and impulsivity (e.g., S. Cacioppo, Capitanio, & Cacioppo, 2014; Ernst & Cacioppo, 1999; Kearns et al., 2014). In addition, loneliness is a risk factor for cognitive decline and the progression of Alzheimer’s Disease (Wilson et al., 2007), recurrent stroke (for review see S. Cacioppo, Capitanio, & Cacioppo, 2014), obesity (Lauder, Mummery, Jones, & Caperchione, 2006), increased vascular resistance (J. T. Cacioppo, Hawkley, Crawford et al., 2002), elevated blood pressure (J. T. Cacioppo, Hawkley, Crawford et al., 2002; Hawkley et al., 2006), increased hypothalamic pituitary adrenocortical activity (Adam, Hawkley, Kudielka, & Cacioppo, 2006; Steptoe, Owen, Kunz-Ebrecht, & Brydon, 2004), decreased sleep salubrity (J. T. Cacioppo, Hawkley, Berntson et al., 2002; Pressman et al., 2005), diminished immunity (Kiecolt-Glaser et al., 1984a b; Pressman et al., 2005), an under-expression of genes bearing anti-inflammatory glucocorticoid response elements and an upregulation of pro-inflammatory gene transcripts (Cole et al., 2007, 2011), abnormal ratios of circulating white blood cells (e.g., neutrophils, lymphocytes, and monocytes; Cole, 2008), and premature mortality (e.g., Luo et al., 2012).
Interventions to Reduce Loneliness
Increased recognition of loneliness as a risk factor for adverse psychological and physical health outcomes has elevated interest in interventions to reduce chronic loneliness. For instance, the British government is developing several initiatives aiming to improve the life quality and satisfaction of people suffering from the (real or perceived) absence of social relationships (Victor, Scambler, Bowling, & Bond, 2005). Campaigns designed to raise awareness about the growing problem of loneliness and isolation have also been launched in the United Kingdom by five partner organizations (http://www.campaigntoendloneliness.org/about-the-campaign/), in Denmark by the Crown Princess and her Mary Foundation (http://www.maryfonden.dk/en/loneliness) and the DaneAge Association (Ældre Sagen; http://www.aeldresagen.dk/presse/nyheder/Sider/Folkebevaegelse-skal-bryde-tabu-om-ensomhed.aspx), in Canada by the Canadian Seniors Council (http://www.seniorscouncil.gc.ca/eng/home.shtml), and in the United States by Oprah Winfrey, Sanjay Gupta, and Gayle King and supported by Skype (http://www.oprah.com/health/Just-Say-Hello-Fight-Loneliness), the AARP Foundation Initiative on Social Isolation (http://www.aarp.org/aarp-foundation/our-work/isolation/), and the Do-It Campaign to end isolation (http://women.oshkoshareacf.org/endisolation). These campaigns are essential to raise awareness about and to reduce the stigma surrounding loneliness, but these represent only a first step. Effective treatments are also needed.
Different types of treatments
To date, there have been a number of attempts to mitigate loneliness. Such interventions include one-on-one interventions (e.g., befriending, Mead et al., 2010; or mentoring, Dickens et al., 2011), group therapy (e.g., groups of lonely people), and wider community interventions (e.g., community events reaching out to a lonely person/s; Cattan et al., 2005; Findlay, 2003; Masi et al., 2011 for reviews). Most of them have been based on the intuitive understanding of loneliness. For instance, a first model has been to provide social support to lonely individuals. That said, as described above, loneliness is not only about getting support, it is also about giving support back and mutual aid.
A second model has been to increase opportunities for social interaction. But, as noted above, a large number of contacts is not equivalent to high quality relationships (Masi et al., 2011). Effects of our own mentation (what we think, what we perceive) involves both conscious and nonconscious mechanisms. Even if lonely individuals want to connect, their non-conscious hypervigilance for social threat can lead them to be negative with or withdraw from others.
A third model to reduce loneliness is based on teaching lonely people to master social skills. For unfortunate individuals who lack of social skills, this may be effective but people are lonely for many reasons other than poor social skills. Experimental research in which loneliness was manipulated shows that most adults have at least minimal social skills, but these adults are more likely to call upon these social skills when they feel low rather than high in loneliness (Cacioppo et al., 2006).
Which type of behavioral intervention is most effective to reduce loneliness?
We addressed this question in a quantitative meta-analysis on the efficacy of the various treatments tested to reduce loneliness between 1970 and 2009 (Masi et al., 2011), and we investigated various moderator variables, such as the experimental design (single group pretest-posttest; nonrandomized comparison group; randomized comparison group) and intervention format (individual or group). Results showed that the mean effect size was much lower when appropriate experimental and statistical controls were implemented, with the effect size for nonrandomized group comparison studies being −.459, and single-group pretest-posttest designs being −.367, whereas the effect size for randomized controlled studies being −.198. This finding implies that if a program or intervention to reduce loneliness is to be evaluated for efficacy – including large-scale programs such as those being introduced in the United States, Canada, Denmark, and the United Kingdom – it is important to control for potential confounding variables (time, expectancy effects, Hawthorne effects, confounding individual differences) to avoid biases that are likely to lead to an overestimate of treatment efficacy.
Contrary to the conclusion of previous narrative reviews carried out since the 1980s, Masi et al.’s (2011) quantitative literature review revealed little evidence for better efficacy of one-to-one individual therapies compared to group therapies. Type of intervention program was a significant moderator, however. Twenty studies met the criteria for randomized group comparison design, and all four primary types of interventions known to reduce loneliness were present in this group. These four primary types of intervention programs were (a) those that increased opportunities for social contact (e.g., social recreation intervention), (b) those that enhanced social support (e.g., through mentoring programs, Buddy-care program, conference calls), (c) those that focused on social skills (e.g., speaking on the phone, giving and receiving compliments, enhancing nonverbal communication skills), and (d) those that addressed maladaptive social cognition (e.g., cognitive behavioral therapy). Among these four types, interventions designed to address maladaptive social cognition were associated with the largest effect size (mean effect size = −.598).
These studies ranged from one with elderly adults from a nursing home in Tapei who participated in eight weekly sessions designed to increase awareness and expression of their feelings, to identify positive relationships from their past, and to apply these prior experiences to their current relationships (Chiang et al., 2009) to one with high-risk Naval recruits at basic training who met for 45 minutes per week for 9 weeks to learn, discuss, and practice strategies for increasing one’s sense of belonging, decreasing thought distortion, and improving one’s coping and stress management (Williams et al., 2004). Interventions designed to enhance social support produced a significant but small reduction in loneliness (mean effect size = −.162), while interventions to increase opportunities for social interaction (mean effect size = −.062, n.s.) and interventions to improve social skills (mean effect size = −.017, n.s.) were not found to be effective in lowering loneliness. These findings reinforce the notion that interpersonal contact or communication per se is not sufficient to address chronic loneliness in the general population.
One key to (social) cognitive behavioral therapy (CBT) in the framework of reducing loneliness is to educate individuals to identify the automatic negative thoughts that they have about others and about social interactions more generally, and to regard these negative thoughts as possibly faulty hypotheses that need to be verified rather than as facts on which to act (Anderson, Horowitz, & French, 1983; McWhirter, 1990a; Young, 1982). By aiming to change maladaptive social perception and cognition (e.g., dysfunctional and irrational beliefs, false attributions, and self-defeating thoughts and interpersonal interactions; Young, 1982; for reviews: Cacioppo & Patrick, 2008; Masi et al., 2011; McWhirter, 1990a), CBT approach implies that loneliness can be decreased (Masi et al., 2011, McWhirter, 1990a, for reviews).
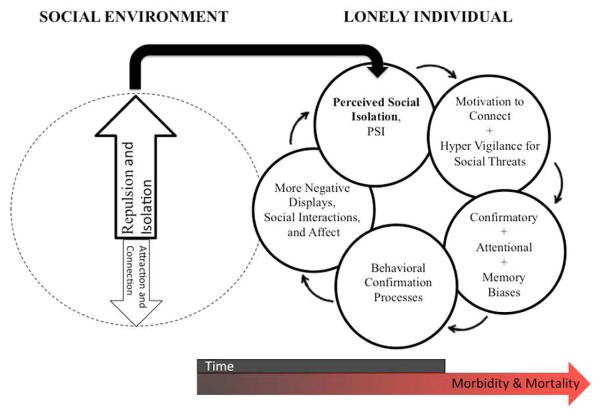
Research on social cognition as a function of loneliness has resulted in the model depicted in Figure 2. According to this model, lonely individuals typically do not voluntarily become lonely; rather, they “find themselves” on one edge of the continuum of social connections (S. Cacioppo & Cacioppo, 2012) and feeling desperately isolated (Booth, 2000). The perception that one is socially on the edge and isolated from others increases the motive for self-preservation. This, then, increases the motivation to connect with others but also increases an implicit hyper-vigilance for social threats, which then can introduce attentional, confirmatory, and memory biases. Given the effects of attention and expectation on anticipated social interactions, behavioral confirmation processes then can incline an individual who feels isolated to have or to place more import on negative social interactions, which if unchecked can reinforce withdrawal, negativity, and feelings of loneliness (e.g., see J. T. Cacioppo & Cacioppo, 2014; J. T. Cacioppo & Hawkley, 2009). This model points to a number of sources of dysfunctional and irrational beliefs, false expectations and attributions, and self-defeating thoughts and interpersonal interactions on which interventions might be designed to operate. For instance, the attentional, confirmatory, and memory biases could be targeted by training in perspective taking, empathy, and identifying automatic negative thoughts about others and about social interactions and in regarding these negative thoughts as possibly faulty hypotheses that need to be verified, whereas faulty behavioral confirmation processes could be targeted by training in mindfulness (Baer, 2003; Creswell et al., 2012) and capitalization (sharing good times; Gable & Reis, 2010; Woods et al., 2014).
Figure 2.
The effects of loneliness on social cognition. Modified from J. T. Cacioppo and Hawkley (2009).
In sum, a primary criterion for empirically supported therapies is that they demonstrate efficacy in randomized controlled studies. Although more research is needed, the meta-analysis suggests that interventions designed to modify maladaptive social cognition may be especially worth pursuing. Such interventions can be expensive and time-consuming, and the client’s lack of openness to changing their thoughts about and interactions with others can be an obstacle to effective treatment. It is possible that these interventions may be more effective (or effective for a greater proportion of individuals) if augmented initially by an appropriate pharmacologic treatment.
Potential Adjunctive Pharmacological Treatments
To date, there is no adjunctive pharmacological treatment for loneliness, but animal research sheds promising light on this issue. For instance, research in which a social animal (e.g., prairie voles, titi monkeys) is chronically housed either with a preferred partner or alone has shown that isolation has deleterious neurological (see review by S. Cacioppo, Capitanio, & Cacioppo, 2014) and neuroendocrinological effects (see review by J. T. Cacioppo, Cacioppo, Capitanio, & Cole, 2015). Interestingly, animal research showed that the behavioral effects of social isolation could be improved with pharmacological help. For instance, pharmacological help includes administration of: 1) antidepressants of the selective serotonin reuptake inhibitors (SSRIs) class that have a broad range of effects including (but not restricted to) improving anxiety-like behavior and fear responses (fluoxetine; Pinna, 2010); 2) neurosteroids (such as allopregnanolone, ALLO) that activate the hypothalamic pituitary adrenocortical (HPA) axis, thereby facilitate the recovery of physiological homeostasis following stressful stimuli (e.g., Evans, Sun, McGregor, & Connor, 2012; cf. S. Cacioppo, Capitanio, & Cacioppo, 2014); or 3) oxytocin, a neuropeptide.
For instance, fluoxetine, an antidepressant of the selective serotonin reuptake inhibitors (SSRIs) class, has a broad range of effects including (but not restricted to) improving the behavioral effects of social isolation, anxiety-like behavior and fear responses (Pinna, 2010; Mayo-Wilson et al., 2014). For patients who decline psychological interventions (such as CBT), SSRIs show consistent evidence of improvement. Interestingly, this improvement does not occur through the inhibition of selective serotonin reuptake (as in depression), but rather through elevated cortico-limbic levels of allopregnanolone (ALLO) and BDNF mRNA expression (Pinna, 2010).
Research supporting the hypothesis of a crucial role of ALLO in social isolation demonstrates that: i) the exaggerated contextual fear response expressed by socially-isolated mice can be normalized with a single injection of ALLO (Pibiri, Nelson, Guidotti, Costa, & Pinna, 2008); ii) HPA dysfunction and impairment of hippocampal neurogenesis respectively can be normalized or prevented with the administration of exogenous ALLO either during or following a period of chronic stress; iii) the establishment of depressive/anxiety-like behaviors in rats can be precluded also with administration of exogenous ALLO (Evans et al., 2012; S. Cacioppo, Capitanio, & Cacioppo, 2014; Nelson & Pinna, 2011; Pinna, 2010); and iv) contextual fear conditioning and aggression can be regulated with ALLO (Nelson & Pinna, 2011). Although further investigations of the effects of ALLO on social isolation are needed in humans, ALLO may provide an adjunctive therapeutic target early in cognitive behavioral interventions to alleviate chronic loneliness.
A third potential adjunctive pharmacological treatment for loneliness is oxytocin, a hypothalamic neuropeptide known to have a high sensitivity to social affiliation (Carter et al., 2008; Goossens et al., in this issue; Grippo, 2009; Young et al., 2014). Recent work with prairie voles raises the possibility that oxytocin may help buffer the deleterious neural, behavioral, immune and autonomic effects of social isolation from a pair-bonded partner (Grippo et al., 2009). The prairie vole is a monogamous rodent whose social structure has similarities to that of humans. In prairie voles, long-term social isolation from a mate or partner produces several negative behavioral and physiological alterations, including depressive and anxiety-relevant behaviors, and autonomic and cardiac dysfunction (Grippo et al., 2007a–c, 2008, 2011, 2012; McNeal et al., 2014). The exogenous peripheral administration of oxytocin eliminates the adverse behavioral and autonomic changes associated with social isolation in the prairie vole (Grippo et al., 2009, 2012).
Oxytocin administration in humans has been shown to promote pro-social behaviors, affiliation, and trust (Kosfeld et al., 2005), cooperation with others (Declerck, Boone, & Kiyonari, 2014), social synchrony (Arueti et al., 2013), autonomic cardiac control (Norman, Cacioppo et al., 2011a), and to decrease the emotional arousal in response to threatening human stimuli (Norman, Cacioppo et al., 2011b), but negative and inconsistent social effects have also been observed (see Bethlehem et al., 2014, and Bali & Jaggi, 2014, for reviews). For instance, some research studies suggest that oxytocin may make neurologically healthy individuals evaluate participants as more trusting and more pro-social in relaxed social situations and more aggressive in tense social situations (for review see: Bartz, Zaki, Bolger, & Ochsner, 2011), whereas others indicate that oxytocin administration increases outgroup aggression (e.g., De Dreu et al., 2010; Taylor et al., 2006). The fact that oxytocin has some prosocial effects, at least for some individuals or situations, is intriguing but how precisely oxytocin might prove helpful in the treatment of chronic loneliness requires additional research.
Conclusion
The etiology of loneliness and its consequences are complex. When the 1978 Task Panel report to the US President’s Commission on Mental Health emphasized the importance of improving health care and easing the pain of those suffering from loneliness, few would have thought that their recommendation would be even more relevant and important today. With increasing evidence that loneliness is a risk factor for mental and physical health problems, attention has begun to turn to interventions for addressing chronic loneliness.
As a first step, there is a need for increased public awareness – and awareness among healthcare providers – that loneliness is a condition that, like chronic pain, can become an affliction for almost anyone. Even popular and high status individuals can find themselves feeling lonely, and the stigma of loneliness further complicates assessment and treatment. Despite the fact that loneliness is a common emotional distress syndrome with a high risk factor for early mortality and a broad variety of physical health and psychiatric issues, it still gets little attention in medical training or in healthcare more generally.
In Masi et al.’s meta-analysis (2011), we identified a need for well-controlled randomized studies focusing on the rehabilitation of the underlying maladaptive social cognition. With the advances made over the past 5 years in the identification of the psychobiological and pharmaceutical mechanisms associated with loneliness and maladaptive social cognition, it may soon be possible to combine (social) cognitive behavioral interventions with short-term adjunctive pharmacological treatments in order to reduce the prevalence of loneliness and its harmful consequences.
Acknowledgments
Preparation of this article was supported by the Department of the Army, Defense Medical Research and Development Program Grant No. W81XWH-11-2-0114.
Footnotes
Although significant overlaps exist between loneliness in adults and loneliness in children and adolescents (Qualter et al., in the present issue), we focus in the present article on reports involving adults.
To evaluate the three dimensions of loneliness, one typically uses the R-UCLA Loneliness scale (either the 20-item, 9-item or 3-item version; Russell et al., 1980; Hughes et al., 2004; Hawkley, Browne, & Cacioppo, 2005; Masi et al., 2011).
References
- Adam EK, Hawkley LC, Kudielka BM, Cacioppo JT. Day-to-day dynamics of experience--cortisol associations in a population-based sample of older adults. Proceedings of the National Academy of Sciences. 2006;103:17058–63. doi: 10.1073/pnas.0605053103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Akerlind I, Hörnquist JO. Loneliness and alcohol abuse: a review of evidences of an interplay. Social Science & Medicine. 1992;34:405–414. doi: 10.1016/0277-9536(92)90300-F. [DOI] [PubMed] [Google Scholar]
- Anderson CA, Horowitz LM, French R. Attributional style of lonely and depressed people. Journal of Personality and Social Psychology. 1983;45:127–136. doi: 10.1037//0022-3514.45.1.127. [DOI] [PubMed] [Google Scholar]
- Andersson L. Loneliness research and interventions: A review of the literature. Aging & Mental Health. 1998;2(4):264–274. doi: 10.1080/13607869856506. [DOI] [Google Scholar]
- Arueti M, Perach-Barzilay N, Tsoory MM, Berger B, Getter N, Shamay-Tsoory SG. When two become one: The role of oxytocin in interpersonal coordination and cooperation. Journal of Cognitive Neuroscience. 2013;25:1418–1427. doi: 10.1162/jocn_a_00400. [DOI] [PubMed] [Google Scholar]
- Baer RA. Mindfulness training as a clinical intervention: A conceptual and empirical review. Clinical Psychology: Science and Practice. 2003;10:125–143. doi: 10.1093/clipsy.bpg015. [DOI] [Google Scholar]
- Bali A, Jaggi AS. Multifunctional aspects of allopregnanolone in stress and related disorders. Progress in Neuro-Psychopharmacology & Biological Psychiatry. 2014;48:64–78. doi: 10.1016/j.pnpbp.2013.09.005. [DOI] [PubMed] [Google Scholar]
- Bartz JA, Zaki J, Bolger N, Ochsner KN. Social effects of oxytocin in humans: Context and person matter. Trends in Cognitive Sciences. 2011;15:301–309. doi: 10.1016/j.tics.2011.05.002. [DOI] [PubMed] [Google Scholar]
- Bethlehem RA, Baron-Cohen S, van Honk J, Auyeung B, Bos PA. The oxytocin paradox. Frontiers in Behavioral Neuroscience. 2014;8:48. doi: 10.3389/fnbeh.2014.00048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Booth R. Loneliness as a component of psychiatric disorders. Medscape General Medicine. 2000;2:1–7. [Google Scholar]
- Brewer MB. Taking the social origins of human nature seriously: Toward a more imperialist social psychology. Personality & Social Psychology Review. 2004;8:107–113. doi: 10.1207/s15327957pspr0802_3. [DOI] [PubMed] [Google Scholar]
- Buys CJ, Larson KL. Human sympathy groups. Psychology Reports. 1979;45:547–553. doi: 10.2466/pr0.1979.45.2.547. [DOI] [Google Scholar]
- Cacioppo JT, Cacioppo S. Social relationships and health: The toxic effects of perceived social isolation. Social and Personality Psychology Compass. 2014;8:58–72. doi: 10.1111/spc3.12087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacioppo JT, Cacioppo S, Boomsma DI. Evolutionary mechanisms for loneliness. Cognition and Emotion. 2014;28:3–21. doi: 10.1080/02699931.2013.837379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacioppo JT, Cacioppo S, Capitanio JP, Cole SW. The neuroendocrinology of social isolation. Annual Review of Psychology. 2015;66 doi: 10.1146/annurev-psych-010814-015240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacioppo JT, Cacioppo S, Cole SW, Capitanio JP, Goossens L, Boomsma DI. Loneliness across phylogeny and a call for animal models. Perspectives on Psychological Science. doi: 10.1177/1745691614564876. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacioppo JT, Ernst JM, Burleson MH, McClintock MK, Malarkey WB, Berntson GG. Lonely traits and concomitant physiological processes: The MacArthur Social Neuroscience Studies. International Journal of Psychophysiology. 2000;35:143–154. doi: 10.1016/S0167-8760(99)00049-5. [DOI] [PubMed] [Google Scholar]
- Cacioppo JT, Fowler JH, Christakis NA. Alone in the crowd: The structure and spread of loneliness in a large social network. Journal of Personality and Social Psychology. 2009;97:977–991. doi: 10.1037/a0016076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacioppo JT, Hawkley LC. Perceived social isolation and cognition. Trends in Cognitive Sciences. 2009;13:447–454. doi: 10.1016/j.tics.2009.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacioppo JT, Hawkley LC, Berntson GG, Ernst JM, Gibbs AC, Stickgold R, Hobson JA. Do lonely days invade the nights? Potential social modulation of sleep efficiency. Psychological Science. 2002;13:384–387. doi: 10.1111/1467-9280.00469. [DOI] [PubMed] [Google Scholar]
- Cacioppo JT, Hawkley LC, Crawford LE, Ernst JM, Burleson MH, Kowalewski RB, Berntson GG. Loneliness and health: potential mechanisms. Psychosomatic Medicine. 2002;64:407–417. doi: 10.1097/00006842-200205000-00005. [DOI] [PubMed] [Google Scholar]
- Cacioppo JT, Hawkley LC, Thisted RA. Perceived social isolation makes me sad: Five year cross-lagged analyses of loneliness and depressive symptomatology in the Chicago Health, Aging, and Social Relations Study. Psychology and Aging. 2010;25:453–463. doi: 10.1037/a0017216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacioppo JT, Hughes ME, Waite LJ, Hawkley LC, Thisted RA. Loneliness as a specific risk factor for depressive symptoms: Cross sectional and longitudinal analyses. Psychology and Aging. 2006;21:140–151. doi: 10.1037/0882-7974.21.1.140. [DOI] [PubMed] [Google Scholar]
- Cacioppo JT, Patrick W. Loneliness: Human nature and the need for social connection. New York: Norton; 2008. [Google Scholar]
- Cacioppo S, Cacioppo JT. Decoding the invisible forces of social connections. Frontiers in Integrative Neuroscience. 2012;51:1–7. doi: 10.3389/fnint.2012.00051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacioppo S, Cacioppo JT. Do you feel lonely? You are not alone: Lessons from social neuroscience. Frontiers in Neuroscience for Young Minds. 2013 Nov 9; [Google Scholar]
- Cacioppo S, Capitanio JP, Cacioppo JT. Toward a neurology of loneliness. Psychological Bulletin. 2014 doi: 10.1037/a0037618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carter CS, Grippo AJ, Pournajafi-Nazarloo H, Ruscio MG, Porges SW. Oxytocin, vasopressin and sociality. Progress in Brain Research. 2008;170:331–336. doi: 10.1016/S0079-6123(08)00427-5. [DOI] [PubMed] [Google Scholar]
- Cattan M, White M, Bond J, Learmouth A. Preventing social isolation and loneliness among older people: A systematic review of health promotion interventions. Ageing and Society. 2005;25:41–67. doi: 10.1017/S0144686X04. [DOI] [PubMed] [Google Scholar]
- Chiang KJ, Chu H, Chang HJ, Chung MH, Chen CH, Chiou HY, Chou KR. The effects of reminiscence therapy on psychological well-being, depression, and loneliness among the institutionalized aged. International Journal of Geriatric Psychiatry. 2009;25:380–388. doi: 10.1002/gps.2350. [DOI] [PubMed] [Google Scholar]
- Cole SW. Social regulation of leukocyte homeostasis: the role of glucocorticoid sensitivity. Brain Behav Immun. 2008;22:1049–1055. doi: 10.1016/j.bbi.2008.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cole SW, Hawkley LC, Arevalo JM, Sung CY, Rose RM, Cacioppo JT. Social regulation of gene expression in human leukocytes. Genome biology. 2007;8:R189. doi: 10.1186/gb-2007-8-9-r189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Declerck CH, Boone C, Kiyonari T. The effect of oxytocin on cooperation in a prisoner’s dilemma depends on the social context and a person’s social value orientation. Social Cognitive and Affective Neuroscience. 2014;9:802–809. doi: 10.1093/scan/nst040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Dreu CK, Greer LL, Handgraaf MJ, Shalvi S, Van Kleef GA, Feith SWW. The neuropeptide oxytocin regulates parochial altruism in intergroup conflict among humans. Science. 2010;328:1408–1411. doi: 10.1126/science.1189047. [DOI] [PubMed] [Google Scholar]
- Dickens AP, Richards SH, Hawton A, Taylor RS, Greaves CJ, Campbell JL. An evaluation of the effectiveness of a community mentoring service for socially isolated older people: A controlled trial. BMC Public Health. 2011;11:218. doi: 10.1186/1471-2458-11-218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunbar RIM. The social brain: Psychological underpinnings and implications for the structure of organizations. Current Directions in Psychological Science. 2014;23:109–114. doi: 10.1177/0963721413517118. [DOI] [Google Scholar]
- Edmondson B. All the lonely people. AARP: The Magazine. 2010 Nov-Dec;(83) [Google Scholar]
- Ernst JM, Cacioppo JT. Lonely hearts: Psychological perspectives on loneliness. Applied and Preventive Psychology. 1999;8:1–22. [Google Scholar]
- Evans J, Sun Y, McGregor A, Connor B. Allopregnanolone regulates neurogenesis and depressive/anxiety-like behavior in a social isolation rodent model of chronic stress. Neuropharmacology. 2012;63:1315–1326. doi: 10.1016/j.neuropharm.2012.08.012. [DOI] [PubMed] [Google Scholar]
- Findlay RA. Interventions to reduce social isolation amongst older people: Where is the evidence? Ageing and Society. 2003;23:647–658. [Google Scholar]
- Gable SL, Reis HT. Good news! Capitalizing on positive events in an interpersonal context. In: Zanna MP, editor. Advances in Experimental Social Psychology. Vol. 42. San Diego, CA: Elsevier Academic Press; 2010. pp. 195–257. [Google Scholar]
- Goossens L, Verhagen M, van Roekel E, Cacioppo JT, Cacioppo S, Boomsma DI. The genetics of loneliness: The quest for underlying mechanisms and developmental processes. Perspectives on Psychological Science. doi: 10.1177/1745691614564878. in press. [DOI] [PubMed] [Google Scholar]
- Granovetter M. The strength of weak ties. American Journal of Sociology. 1973;78:1360–1380. doi: 10.1086/225469. [DOI] [Google Scholar]
- Griffin J. The lonely society? London: The Mental Health Foundation; 2010. [Google Scholar]
- Grippo AJ. Mechanisms underlying altered mood and cardiovascular dysfunction: The value of neurobiological and behavioral research with animal models. Neuroscience and Biobehavioral Reviews. 2009;33:171–180. doi: 10.1016/j.neubiorev.2008.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grippo AJ, Carter CS, McNeal N, Chandler DL, LaRocca MA, Bates SL, Porges SW. 24-Hour autonomic dysfunction and depressive behaviors in an animal model of social isolation: Implications for the study of depression and cardiovascular disease. Psychosomatic Medicine. 2011;73:59–66. doi: 10.1097/PSY.0b013e31820019e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grippo AJ, Lamb DG, Carter CS, Porges SW. Social isolation disrupts autonomic regulation of the heart and influences negative affective behaviors. Biological Psychiatry. 2007a;62:1162–1170. doi: 10.1016/j.biopsych.2007.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grippo AJ, Cushing BS, Carter CS. Depression-like behavior and stressor-induced neuroendocrine activation in female prairie voles exposed to chronic social isolation. Psychosomatic Medicine. 2007b;69:149–157. doi: 10.1097/PSY.0b013e31802f054b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grippo AJ, Gerena D, Huang J, Kumar N, Shah M, Ughreja R, Carter CS. Social isolation induces behavioral and neuroendocrine disturbances relevant to depression in female and male prairie voles. Psychoneuroendocrinology. 2007c;32:966–980. doi: 10.1016/j.psyneuen.2007.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grippo AJ, Wu KD, Hassan I, Carter CS. Social isolation in prairie voles induces behaviors relevant to negative affect: Toward the development of a rodent model focused on co-occurring depression and anxiety. Depression & Anxiety. 2008;25:E17–E26. doi: 10.1002/da.20375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grippo AJ, Trahanas DM, Zimmerman IIRR, Porges SW, Carter CS. Oxytocin protects against negative behavioral and autonomic consequences of long-term social isolation. Psychoneuroendocrinology. 2009;34:1542–1553. doi: 10.1016/j.psyneuen.2009.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grippo AJ, Pournajafi-Nazarloo H, Sanzenbacher L, Trahanas DM, McNeal N, Carter SC. Peripheral oxytocin administration buffers autonomic but not behavioral responses to environmental stressors in isolated prairie voles. Stress. 2012;15:149–161. doi: 10.3109/10253890.2011.605486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grippo A, Ihm E, Wardwell J, McNeal N, Scotti M, Preihs K. The effects of environmental enrichment on depressive and anxiety-relevant behaviors in socially isolated prairie voles. Psychosomatic Medicine. 2014;76:277–284. doi: 10.1097/PSY.0000000000000052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall ET. A System for the Notation of Proxemic Behavior. American Anthropologist. 1963;65:1003–1026. [Google Scholar]
- Hall ET. The Hidden Dimension. Garden City, N.Y: Doubleday; 1966. [Google Scholar]
- Hawley LC, Browne MW, Cacioppo JT. How can I connect with thee? Let me count the ways. Psychological Science. 2005;16:798–804. doi: 10.1111/j.1467-9280.2005.01617.x. [DOI] [PubMed] [Google Scholar]
- Hawkley LC, Gu Y, Luo YJ, Cacioppo JT. The mental representation of social connections: Generalizability extended to Beijing adults. PLoS ONE. 2012;7(9):e44065. doi: 10.1371/journal.pone.0044065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkley LC, Hughes ME, Waite LJ, Masi CM, Thisted RA, Cacioppo JT. From social structure factors to perceptions of relationship quality and loneliness: The Chicago Health, Aging, and Social Relations Study. Journal of Gerontology: Social Sciences. 2008;63B:S375–S384. doi: 10.1093/geronb/63.6.s375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkley LC, Masi CM, Berry JD, Cacioppo JT. Loneliness is a unique predictor of age-related differences in systolic blood pressure. Psychology and Aging. 2006;21:152–164. doi: 10.1037/0882-7974.21.1.152. [DOI] [PubMed] [Google Scholar]
- Heinrich LM, Gullone E. The clinical significance of loneliness: a literature review. Clinical Psychology Review. 2006;26:695–718. doi: 10.1016/j.cpr.2006.04.002. [DOI] [PubMed] [Google Scholar]
- Holt-Lunstad J, Smith TB. Loneliness and Social Isolation as Risk Factors for Mortality: A Meta-Analytic Review. Perspectives on Psychological Science/ doi: 10.1177/1745691614568352. in press. [DOI] [PubMed] [Google Scholar]
- Hughes ME, Waite LJ, Hawkley LC, Cacioppo JT. A short scale for measuring loneliness in large surveys: Results from two population-based studies. Research on Aging. 2004;26:655–672. doi: 10.1177/0164027504268574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kearns A, Whitley E, Tannahill C, Ellaway A. Loneliness, social relations and health and well-being in deprived communities. Psychology, Health, & Medicine. 2014:1–13. doi: 10.1080/13548506.2014.940354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiecolt-Glaser JK, Garner W, Speicher CE, Penn GM, Holliday JE, Glaser R. Psychosocial modifiers of immunocompetence in medical students. Psychosomatic Medicine. 1984a;46:7–14. doi: 10.1097/00006842-198401000-00003. [DOI] [PubMed] [Google Scholar]
- Kiecolt-Glaser JK, Ricker D, George J, Messick G, Speicher CE, Garner W, Glaser R. Urinary cortisol levels, cellular immunocompetency, and loneliness in psychiatric inpatients. Psychosomatic Medicine. 1984b;46:15–23. doi: 10.1097/00006842-198401000-00004. [DOI] [PubMed] [Google Scholar]
- Kosfeld M, Heinrichs M, Zak PJ, Fischbacher U, Fehr E. Oxytocin increases trust in humans. Nature. 2005;435:673–676. doi: 10.1038/nature03701. [DOI] [PubMed] [Google Scholar]
- Lauder W, Mummery K, Jones M, Caperchione C. A comparison of health behaviours in lonely and non-lonely populations. Psychol Health Med. 2006;11:233–245. doi: 10.1080/13548500500266607. [DOI] [PubMed] [Google Scholar]
- Lopata HZ, Heinemann GD, Baum J. Loneliness: Antecedents and coping strategies in the lives of widows. In: Peplau LA, Perlman D, editors. Loneliness: A sourcebook of current theory, research and therapy. New York: Wiley-Interscience; 1982. pp. 310–326. [Google Scholar]
- Luo Y, Hawkley LC, Waite LJ, Cacioppo JT. Loneliness, health, and mortality in old age: A national longitudinal study. Social Science & Medicine. 2012;74:907–914. doi: 10.1016/j.socscimed.2011.11.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lynch JJ, Convey WH. Loneliness, disease, and death: Alternative approaches. Psychosomatics. 1979;20:702–708. doi: 10.1016/s0033-3182(79)73751-0. [DOI] [PubMed] [Google Scholar]
- Masi CM, Chen HY, Hawkley LC, Cacioppo JT. A meta-analysis of interventions to reduce loneliness. Personality and Social Psychology Review. 2011;15:219–266. doi: 10.1177/1088868310377394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mayo-Wilson E, Dias S, Mavranesouli I, Kew K, Clark DM, Ades AE, Pilling S. Psychological and pharmacological interventions for social anxiety disorder in adults: A systematic review and network meta-analysis. The Lancet Psychiatry. 2014;1:368–376. doi: 10.1016/S2215-0366(14)70329-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mead N, et al. Effects of befriending on depressive symptoms and distress: Systematic review and meta-analysis. British Journal of Psychiatry. 2010;196:96–100. doi: 10.1192/bjp.bp.109.064089. [DOI] [PubMed] [Google Scholar]
- McNeal N, Scotti MA, Wardwell J, Chandler DL, Bates SL, Grippo AJ. Disruption of social bonds induces behavioral and physiological dysregulation in male and female prairie voles. Autonomic Neuroscience: Basic and Clinical. 2014;180:9–16. doi: 10.1016/j.autneu.2013.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McWhirter BT. Loneliness: A review of current literature, with implications for counseling and research. Journal of Counseling & Development. 1990a;68:417–422. doi: 10.1002/j.1556-6676.1990.tb02521.x. [DOI] [Google Scholar]
- McWhirter BT. Factor analysis of the revised UCLA Loneliness Scale. Current Psychology: Research and Reviews. 1990b;9:56–68. doi: 10.1007/BF02686768. [DOI] [Google Scholar]
- Nelson M, Pinna G. S-norfluoxetine infused into the basolateral amygdala increases allopregnanolone levels and reduces aggression in socially isolated mice. Neuropharmacology. 2011;60:1154–1159. doi: 10.1016/j.neuropharm.2010.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norman GJ, Cacioppo JT, Morris JS, Malarkey WB, Berntson GG, De Vries CA. Oxytocin increases autonomic cardiac control: Moderation by loneliness. Biological Psychology. 2011a;86:174–180. doi: 10.1016/j.biopsycho.2010.11.006. [DOI] [PubMed] [Google Scholar]
- Norman GJ, Cacioppo JT, Morris JS, Karelina K, Malarkey WB, DeVries AC, Bernston GG. Selective influences of oxytocin on the evaluative processing of social stimuli. Psychopharmacology. 2011b;25:1313–1319. doi: 10.1177/0269881110367452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ortigue S, Megevand P, Perren F, Landis T, Blanke O. Double dissociation between representational personal and extrapersonal neglect. Neurology. 2006;66:1414–1417. doi: 10.1212/01.wnl.0000210440.49932.e7. [DOI] [PubMed] [Google Scholar]
- Ortigue S, Viaud-Delmon I, Michel CM, Blanke O, Annoni JM, Landis T. Pure imagery hemi-neglect of far space. Neurology. 2003;60:2000–2002. doi: 10.1212/01.WNL.0000068028.63291.B6. [DOI] [PubMed] [Google Scholar]
- Ostrov E, Offer D. Adolescent youth and society. Chicago: University of Chicago Press; 1978. [Google Scholar]
- Peplau LA, Perlman D. Perspectives on loneliness. In: Peplau LA, Perlman D, editors. Loneliness: A sourcebook of current theory, research and therapy. New York: Wiley; 1982. pp. 1–8. [Google Scholar]
- Peplau LA, Russell D, Heim M. The experience of loneliness. In: Frieze IH, Bar-Tal D, Carroll JS, editors. New approaches to social problems: Applications of attribution theory. San Francisco, CA: Jossey-Bass; 1979. pp. 53–78. [Google Scholar]
- Perissinotto CM, Cenzer IS, Covinsky KE. Loneliness in older persons: A predictor of functional decline and death. Archives of Internal Medicine. 2012;172:1078–1083. doi: 10.1001/archinternmed.2012.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pibiri F, Nelson M, Guidotti A, Costa E, Pinna G. Decreased corticolimbic allopregnanolone expression during social isolation enhances contextual fear: A model relevant for posttraumatic stress disorder. Proceedings of the National Academy of Sciences. 2008;105:5567–5572. doi: 10.1073/pnas.0801853105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinna G. In a mouse model relevant for post-traumatic stress disorder, selective brain steoidogenic stimulants (SBSS) improve behavioral deficits by normalizing allopregnanolone biosynthesis. Behavioral Pharmacology. 2010;21:438–450. doi: 10.1097/FBP.0b013e32833d8ba0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pressman SD, Cohen S, Miller GE, Barkin A, Rabin BS, Treanor JJ. Loneliness, social network size, and immune response to influenza vaccination in college freshmen. Health Psychology. 2005;24:297–306. doi: 10.1037/0278-6133.24.3.297. [DOI] [PubMed] [Google Scholar]
- Qualter P, Vanhalst J, Harris R, Van Roekel E, Lodder G, Bangee M, Maes M, Verhagen M. Loneliness across ontogeny. Perspectives on Psychological Science. doi: 10.1177/1745691615568999. in press. [DOI] [PubMed] [Google Scholar]
- Randall C. Measuring national well-being – Our relationships, 2012. Office of National Statistics 2012 [Google Scholar]
- Rizzolatti G, Matelli M, Pavesi G. Deficits in attention and movement following the removal of postarcuate (area 6) and prearcuate (area 8) cortex in macaque monkeys. Brain. 1983;106:655–673. doi: 10.1093/brain/106.3.655. [DOI] [PubMed] [Google Scholar]
- Rizzolatti G, Riggio L, Dascola I, Umiltà C. Reorienting attention across the horizontal and vertical meridians: evidence in favor of a premotor theory of attention. Neuropsychologia. 1987;25:31–40. doi: 10.1016/0028-3932(87)90041-8. [DOI] [PubMed] [Google Scholar]
- Rudatsikira E, Muula AS, Siziya S, Twa-Twa J. Suicidal ideation and associated factors among school-going adolescents in rural Uganda. BMC Psychiatry. 2007;7:67. doi: 10.1186/1471-244X-7-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell D. The measurement of loneliness. In: Peplau LA, Perlman D, editors. Loneliness: A sourcebook of current theory, research and therapy. New York: Wiley; 1982. pp. 81–104. [Google Scholar]
- Russell D, Peplau LA, Cutrona CE. The revised UCLA loneliness scale: Concurrent and discriminant validity evidence. Journal of Personality and Social Psychology. 1980;39:472–480. doi: 10.1037//0022-3514.39.3.472. [DOI] [PubMed] [Google Scholar]
- Steptoe A, Owen N, Kunz-Ebrecht SR, Brydon L. Loneliness and neuroendocrine, cardiovascular, and inflammatory stress responses in middle-aged men and women. Psychoneuroendocrinology. 2004;29:593–611. doi: 10.1016/S0306-4530(03)00086-6. [DOI] [PubMed] [Google Scholar]
- Stickley A, Koyanagi A, Roberts B, Richardson E, Abbott P, Tumanov S, Mckee M. Loneliness: Its correlates and association with health behaviors and outcomes in nine countries of the former soviet union. Plos One. 2013;8:e67978. doi: 10.1371/journal.pone.0067978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor SE. Tend and befriend: Biobehavioral bases of affiliation under stress. Current Directions in Psychological Science. 2006;15:273–277. doi: 10.1111/j.1467-8721.2006.00451.x. [DOI] [Google Scholar]
- Tillich P. The external now. In: Feifel H, editor. The meaning of death. New York: McGraw-Hill; 1959. pp. 30–38. [Google Scholar]
- U.S. President’s Commission on Mental Health. Report to the President from the President’s Commission on Mental Health. Vol. 4. Washington, D.C: U.S. Government Printing Office; 1978. [Google Scholar]
- VanderWeele TJ, Hawkley LC, Thisted RA, Cacioppo JT. A marginal structural model analysis for loneliness: Implications for intervention trials and clinical practice. Journal of Clinical and Consulting Psychology. 2011;79:225–235. doi: 10.1037/a0022610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Victor CR, Scambler SJ, Bowling A, Bond J. The prevalence of, and risk factors for, loneliness in later life: a survey of older people in Great Britain. Aging and Society. 2005;25:357–375. doi: 10.1017/S0144686X04003332. [DOI] [Google Scholar]
- Victor CR, Yang K. The prevalence of loneliness among adults: A case study of the United Kingdom. Journal of Psychology. 2012;146:85–104. doi: 10.1080/00223980.2011.613875. [DOI] [PubMed] [Google Scholar]
- Waite LJ, Gallagher M. Case for marriage: Why married people are happier, healthier, and better off financially. New York: Doubleday; 2001. [Google Scholar]
- Weeks DG, Michela JL, Peplau LA, Bragg ME. The relation between loneliness and depression: A structural equation analysis. Journal of Personality and Social Psychology. 1980;39:1238–1244. doi: 10.1037/h0077709. [DOI] [PubMed] [Google Scholar]
- Weiss RS, editor. Loneliness: The experience of emotional and social isolation. Cambridge, MA: MIT Press; 1973. [Google Scholar]
- Williams RA, Hagerty BM, Yousha SM, Horrocks J, Hoyle KS, Liu D. Psychosocial effects of the boot strap intervention in Navy recruits. Military Medicine. 2004;169:814–820. doi: 10.7205/milmed.169.10.814. [DOI] [PubMed] [Google Scholar]
- Wilson RS, Krueger KR, Arnold SE, Schneider JA, Kelly JF, Bennett DA. Loneliness and risk of Alzheimer disease. Archives of General Psychiatry. 2007;64:234–240. doi: 10.1001/archpsyc.64.2.234. [DOI] [PubMed] [Google Scholar]
- Woods S, Lambert N, Brown P, Fincham F, May R. “I’m so excited for you!” How an enthusiastic responding intervention enhances close relationships. Journal of Social and Personal Relationships. 2014;4:1–17. doi: 10.1177/0265407514523545. [DOI] [Google Scholar]
- Young JE. Loneliness, depression and cognitive therapy: Theory and application. In: Peplau LA, Perlman D, editors. Loneliness: A sourcebook of current theory, research and therapy. New York: Wiley; 1982. pp. 379–406. [Google Scholar]
- Young KA, Liu Y, Gobrogge KL, Wang H, Wang Z. Oxytocin reverses amphetamine-induced deficits in social bonding: Evidence for an interaction with nucleus accumbens dopamine. The Journal of Neuroscience. 2014;34:8499–8506. doi: 10.1523/JNEUROSCI.4275-13.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]