Abstract
Background
Although it is thought that inner-city areas have a high burden of asthma, the prevalence of asthma in inner-cities across the U.S. is not known.
Objective
To estimate the prevalence of current asthma in U.S. children living in inner-city and non-inner city areas, and to examine whether urban residence, poverty or race/ethnicity are the main drivers of asthma disparities.
Methods
The National Health Interview Survey 2009–2011 was linked by census tract to data from the U.S. Census and the National Center for Health Statistics. Multivariate logistic regression models adjusted for sex, age, race/ethnicity, residence in an urban, suburban, medium metro or small metro/rural area, poverty, and birth outside the U.S. with current asthma and asthma morbidity as outcome variables. Inner-city areas were defined as urban areas with ≥20% of households below the poverty line.
Results
23,065 children living in 5,853 census tracts were included. The prevalence of current asthma was 12.9% in inner-city and 10.6% in non-inner-city areas, but this difference was not significant after adjusting for race/ethnicity, region, age and sex. In fully adjusted models, Black race, Puerto Rican ethnicity and lower household income, but not residence in poor or urban areas, were independent risk factors for current asthma. Household poverty increased the risk of asthma among non-Hispanics and Puerto Ricans but not among other Hispanics. Associations with asthma morbidity were very similar to prevalent asthma.
Conclusions
Although the prevalence of asthma is high in some inner-city areas, this is largely explained by demographic factors and not by living in an urban neighborhood.
Keywords: inner-city asthma, childhood asthma, urban/rural, neighborhood, race/ethnicity
INTRODUCTION
The idea that certain features of life in poor urban areas promote asthma dates back to more than a half century ago, when researchers began to describe an “inner-city asthma epidemic” of high asthma prevalence and morbidity in poor areas of large cities.(1–8) Research focusing on the inner-city, typically defined as census tracts in large metro center areas with at least 20% of households below the poverty line(9), has led to significant advances in our understanding of what causes asthma and how to treat it(10), but the prevalence of asthma in inner-city areas across the U.S. is not known, nor how it compares to the prevalence in other types of communities. Studies of prevalence of asthma in the inner-city have generally focused on individual urban communities and have not separated demographic features of inner-city areas from their metropolitan status.(5, 11–19) Nationally representative studies have also suffered from several limitations, including the fact that much of the work on the relative contribution of metropolitan status to asthma disparities overall was done decades ago, used measures of metropolitan status that are not consistent with NIH definitions of the “inner-city”, and rarely looked at the independent contributions of poverty, metropolitan status and race/ethnicity.(3, 6, 20) Despite our significant and ongoing national commitment to combatting inner-city asthma, we do not actually know the prevalence of asthma in inner-cities across the U.S., whether it is in fact higher than that found in other areas, and, if there are differences, whether race/ethnicity, poverty or residence in an urban area explain them.
Thus, our primary objectives were to (1) estimate childhood asthma prevalence for inner108 city and non-inner city areas in the US and (2) disentangle the effects of urban residence, neighborhood poverty, race/ethnicity, and household poverty on asthma prevalence. Understanding whether asthma disparities seen in various geographic areas are primarily a result of environmental exposures concentrated in the inner-city, or are instead related to socio-demographic features of the inhabitants of these neighborhoods is key to advancing an efficient and effective national research and public health agenda.
METHODS
Data was drawn from the National Health Interview Survey (NHIS), survey years 2009–2011. The NHIS is a survey conducted annually by the National Center for Health Statistics (NCHS), part of the Centers for Disease Control and Prevention (CDC). It has a multistate probability design that covers all 50 states and the District of Columbia, and it is intended to be representative of the civilian non-institutionalized population living in the United States. In order to increase precision of estimates in certain subgroups, Black, Asian and Hispanic populations are oversampled. Data collection is in-person using a computer assisted personal interviewing mode. The overall response rate for the child section of these surveys ranged from 71–75%.(21–23) Because asthma is not reliably diagnosed in young children, the sample population was limited to children aged 6–17.
In order to evaluate the effect of geographic variables on asthma outcomes, we linked participants’ census tracts, as classified by the 2000 census, to two additional datasets: the 2006 NCHS Urban-Rural Classification Scheme for Counties and the 2000 U.S. Census. The 2006 NCHS Urban-Rural Classification scheme divides counties into six categories: (1) large metro, central, (2) large metro, fringe, (3) medium metro, (4) small metro, (5) micropolitan and (6) non-core based on population density and other measures of urbanization. Generally large metro central is considered the urban core while large metro fringe is thought to be equivalent to “suburban”.(24) Because there were relatively few people residing in small metro, micropolitan and non-core areas, these categories were combined and classified as small metro/rural areas. The 2000 Census provided the percent of households living below the federally defined poverty level in each census tract. This was generally treated as a continuous variable in our analyses, although in some analyses we defined inner-city neighborhoods as census tracts located in large metro central areas with ≥20% of households below the poverty line.(9) Household income was defined as household income divided by the federally defined poverty level.
Ever asthma was defined by a yes answer to “Has a doctor or other health professional EVER told you that [name] had asthma?”. Other questions that defined asthma were: “Does [name] still have asthma?” (Current Asthma), “During the past 12 months, has [name] had an episode of asthma or an asthma attack?” (Asthma Episode) and “during the past 12 months, did [name] have to visit an emergency room or urgent care center because of [his/her] asthma?” (Asthma Emergency Room Visit).
Race/ethnicity was by self-report and recoded in the NHIS data in the following categories: Hispanic, Non-Hispanic White (called “White” here), Non-Hispanic Black (“Black”), Non-Hispanic Asian (“Asian”) and all other race/ethnicities, a group comprising less than 1% of the total population. Because it has been previously reported that Puerto Rican Hispanics have different asthma risk than other Hispanics,(25) we created a separate race/ethnicity category for those of Puerto Rican heritage. Hereafter “Hispanic” refers to non-Puerto Rican Hispanics.
Although multi-level modeling is often used in analyses of the association between neighborhood factors and disease, multi-level modeling typically requires at least 25 individuals per group (in this case census tract)(26), and in this analysis, there were an average of only 4 subjects per census tract. Thus, for this analysis, standard survey methods were used with sample weights and strata provided in the survey. This accounts for the complex survey design, correctly adjusts the variances for clustering within sampling unit and does not require a minimum number of subjects per group. For analyses of individual level income, the CDC provides multiply imputed data for subjects missing income data. These data are generated by the CDC using sequential regression multivariate imputation, implemented by the module IMPUTE using IVEware (www.isr.umich.edu/src/smp/ive),(27) and were analyzed using the MI ESTIMATE commands in Stata, which accounts for the imputation uncertainty using the methods of Rubin.(28) Three logistic regression models for prediction of current asthma, asthma episode and emergency room visit in the past year were generated: crude bivariate analyses, multivariate models adjusted for age, sex, race/ethnicity, region of residence, neighborhood poverty and urban/rural status, and multivariate models additionally adjusted for household income. To determine whether race/ethnicity or metropolitan residence modified the relationship between poverty and asthma, we also investigated interactions between these factors and constructed stratified models. Model diagnostics included the Pearson goodness-of-fit test, visual examination of the data, and with sensitivity analyses excluding very large values. Individual and neighborhood level poverty were examined for collinearity, and because the collinearity was not strong (variance-inflation factor of 1.2), both variables were included in some models. Because we identified differences in the relationship between current asthma and both neighborhood and individual-level poverty between Hispanics and non-Hispanics, we stratified these analyses into (1) Hispanics and (2) all others, including Puerto Ricans. Our analyses confirmed that children of Puerto Rican heritage were more similar to non-Hispanic populations than Hispanics in the relationship between asthma and poverty (data not shown), supporting this method of stratification. Sensitivity analyses of the main model were done including the variables: (1) whether the child had a well-child visit in the past year, and (2) whether the child had at any point been uninsured in the past year. A significance level of 0.05 was used. All analyses were done using Stata 13/SE (College Station, TX). Because census tract information is not available in the public NHIS dataset, these analyses were conducted at the Research Data Center with approval from the NCHS Research Ethics Review Board (ERB). Data collection for the NHIS was approved by the NCHS Research ERB.
RESULTS
Population characteristics
Twenty-three thousand and sixty-five subjects aged 6–17 living in 5,853 different census tracts were included in this analysis. Because the sample was derived from a population-based survey and was weighted to reflect the non-institutionalized U.S. population, the demographics of the analytic population matched those of children 6–17 in the U.S. as a whole (Table 1). On average, subjects resided in census tracts in which 12% of households lived below the poverty line. Twenty-eight percent resided in urban census tracts, 16% resided in poor tracts (defined as ≥20% living below the poverty line), and 7% resided in poor, urban tracts (the “inner-city”) (Table 1). The lifetime asthma prevalence was 16.3%, current asthma prevalence was 10.7%, 5.9% reported an asthma episode, and 1.6% reported visiting the emergency room for asthma in the prior year.
Table 1.
Demographic Characteristics
| Overall | Poor* Urban (2411) |
Non-Poor Urban (5383) |
Poor Non- Urban (2337) |
Non-Poor Non- Urban (12,934) |
||
|---|---|---|---|---|---|---|
| Characteristic | N | % (95% CI) | ||||
| Race/ethnicity | ||||||
| White | 10425 | 57.6 (56.5–58.7) | 7.2 (5.0–10.3) | 45.3 (42.3–47.8) | 32.3 (28.3–36.6) | 71.3 (70.0–72.6) |
| Black | 4067 | 15.2 (14.5–16.0) | 36.7 (32.9–40.7) | 16.7 (15.0–18.6) | 28.5 (24.9–32.3) | 10.4 (9.6–11.2) |
| Hispanic (Non-Puerto Rican) | 6301 | 19.5 (18.7–20.4) | 48 (44.2–52.0) | 27 (25.0–29.2) | 31 (27.3–35.1) | 12.1 (11.1–13.2) |
| Puerto Rican | 600 | 2.1 (1.8–2.3) | 3.9 (2.9–5.2) | 2.2 (1.7–2.8) | 3.6 (2.6–4.9) | 1.6 (1.3–1.9) |
| Asian | 1464 | 4.5 (4.1–4.9) | 3.7 (2.6–5.3) | 8.4 (7.4–9.6) | 1.6 (1.1–2.4) | 3.7 (3.3–4.2) |
| Region | ||||||
| Northeast | 3475 | 16.5 (15.6–17.4) | 24.2 (20.7–28.1) | 11.2 (9.5–13.1) | 9.5 (7.1–12.5) | 18.5 (17.2–19.8) |
| Midwest | 4564 | 24.2 (23.0–25.3) | 13.8 (11.2–16.7) | 18.5 (15.8–21.5) | 13.2 (9.7–17.6) | 28.9 (27.2–30.5) |
| South | 7871 | 35.3 (34.0–36.6) | 24.6 (20.7–29.0) | 30.6 (27.6–33.7) | 51.3 (46.1–56.5) | 35.7 (34.0–37.5) |
| West | 6047 | 24.0 (22.8–25.2) | 37.5 (32.7–42.5) | 39.8 (36.8–42.8) | 26.1 (22.0–30.7) | 17.0 (15.4–18.7) |
| Born in US | ||||||
| Yes | 21320 | 94.3 (93.9–94.7) | 89.1 (87.4–90.7) | 92 (91.0–92.9) | 92.9 (90.8–94.5) | 95.9 (95.4–96.3) |
| No | 1735 | 5.7 (5.3–6.1) | 10.9 (9.4–12.6) | 8 (7.2–9.0) | 7.1 (5.5–9.2) | 4.1 (3.7–4.6) |
| Asthma prevalence | ||||||
| Asthma, lifetime | 3933 | 16.3 (15.7–17.0) | 18.7 (16.5–21.2) | 15.3 (14.0–16.6) | 19.2 (17.1–21.5) | 16 (15.3–16.8) |
| Asthma, current | 2574 | 10.7 (10.2–11.3) | 12.9 (11.1–14.9) | 10 (9.0–11.2) | 12.4 (10.8–14.2) | 10.5 (9.9–11.2) |
| Asthma episode, past 12 months | 1378 | 5.9 (5.5–6.3) | 6.5 (5.5–7.7) | 5.6 (4.8–6.5) | 6.1 (4.9–7.6) | 5.9 (5.4–6.4) |
| ER visit for asthma, past 12 months | 408 | 1.6 (1.4–1.8) | 3.0 (2.2–4.0) | 1.8 (1.3–2.5) | 2.3 (1.6–3.1) | 1.3 (1.4–1.8) |
Poor defined as ≥20% of households living below the poverty line.
Prevalence of asthma in urban poor (inner-city) and other poor areas
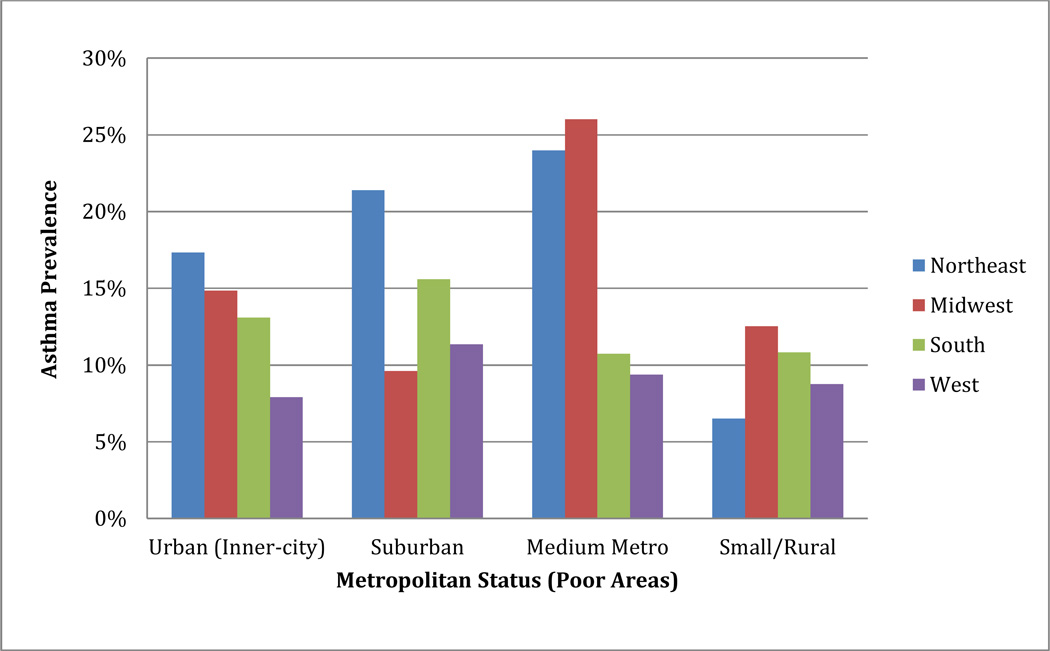
The overall prevalence of current asthma in “inner-city” neighborhoods in the U.S. was 12.9% (95% CI, 11.1–14.9%), compared to 10.6% (95% CI, 10.0–11.2) in non-inner city areas (p=0.01), but this difference was no longer significant after adjusting for race/ethnicity, region, sex, and age (OR: 1.01, 95% CI, 0.84–1.21, p=0.90). Approximately 8% of children with asthma are estimated to live in inner-city areas, compared to 7% of children overall (Supplementary Table 1). The prevalence of asthma in inner-city neighborhoods was not constant throughout the U.S., and ranged from 7.9% (95% CI, 5.9–10.5) in the West to 17.3% (95% CI, 13.2–22.4) in the Northeast (Figure 1). In addition, poor non-inner city areas in some regions had prevalence rates exceeding inner-city areas (Figure 1 and eTable 2). Although in crude stratified analyses, inner-city areas in the Northeast did have higher prevalence rates than non-inner-city areas, in stratified models adjusted for age, sex, place of birth and race/ethnicity, the prevalence of asthma in inner-city neighborhoods was not significantly higher than in non-inner-city areas in any region of the U.S. (data not shown). As shown below, differences in asthma prevalence were driven by racial/ethnic and socioeconomic factors, and not urban/rural status.
Figure 1. Asthma Prevalence by Metropolitan Status in US Children.
Asthma prevalence according to metropolitan status and region among children living in poor areas (defined as neighborhoods with ≥20% of households below the poverty line)
Associations with current asthma prevalence
Race/ethnicity
In unadjusted models, current asthma prevalence was significantly higher among Blacks (17.1%, 95% CI, 15.6–18.8) and Puerto Ricans (19.8%, 95% CI, 16.6–23.5%), than among Whites (9.6%, 95% CI, 8.9–10.3%), Hispanics (8.8%, 95% CI, 7.8–10.0) and Asians (8.1%, 95% CI, 6.5–10.0). Black race and Puerto Rican ethnicity remained strong and independent predictors of current asthma even when neighborhood poverty, urban/rural status, region, sex, age and birth in the U.S. were included in the model, and, additionally, in analyses that further adjusted for household poverty (Table 2 and eTable 3). Birth outside the U.S. was a strong and independent protective factor for asthma (Table 2).
Table 2.
Predictors of current Asthma
| Crude | Adjusted* | |||||
|---|---|---|---|---|---|---|
| OR | 95% CI | P | OR | 95% CI | P | |
| Overall | ||||||
| Race/ethnicity | ||||||
| White | Reference | |||||
| Black | 1.95 | 1.70–2.23 | <0.001 | 1.87 | 1.59–2.19 | <0.001 |
| Hispanic | 0.91 | 0.78–1.07 | 0.26 | 1.02 | 0.85–1.23 | 0.81 |
| Puerto Rican | 2.33 | 1.83–2.95 | <0.001 | 2.38 | 1.82–3.11 | <0.001 |
| Asian | 0.83 | 0.65–1.06 | 0.13 | 1.01 | 0.79–1.30 | 0.93 |
| Urbanization | ||||||
| Urban | Reference | |||||
| Suburban | 1.03 | 0.90–1.19 | 0.66 | 1.14 | 0.97–1.33 | 0.11 |
| Medium Metro | 0.97 | 0.83–1.14 | 0.72 | 1.05 | 0.88–1.24 | 0.60 |
| Small Metro/Rural | 1.00 | 0.85–1.16 | 0.95 | 1.10 | 0.92–1.31 | 0.30 |
| Region | ||||||
| Northeast | Reference | |||||
| Midwest | 0.93 | 0.79–1.11 | 0.43 | 0.98 | 0.82–1.16 | 0.81 |
| South | 0.87 | 0.75–1.01 | 0.06 | 0.85 | 0.73–0.99 | 0.40 |
| West | 0.77 | 0.66–0.91 | 0.002 | 0.90 | 0.76–1.07 | 0.25 |
| Birth outside the US | 0.32 | 0.23–0.45 | <0.001 | 0.33 | 0.24–0.47 | <0.001 |
| Household Poverty† | 1.07 | 1.05–1.10 | <0.001 | |||
| Neighborhood poverty‡ | 1.10 | 1.05–1.14 | <0.001 | 1.04 | 0.99–1.10 | 0.09 |
| Hispanics | ||||||
| Urbanization | ||||||
| Urban | Reference | |||||
| Suburban | 1.21 | 0.88–1.66 | 0.24 | 1.13 | 0.81–1.57 | 0.48 |
| Medium Metro | 1.21 | 0.85–1.72 | 0.28 | 1.25 | 0.88–1.78 | 0.22 |
| Small Metro/Rural | 1.08 | 0.71–1.64 | 0.72 | 1.11 | 0.72–1.70 | 0.64 |
| Household Poverty† | 0.95 | 0.89–1.01 | 0.09 | |||
| Neighborhood poverty‡ | 0.90 | 0.83–0.98 | 0.02 | 0.90 | 0.83–0.98 | 0.02 |
| Non-Hispanics and Puerto Ricans | ||||||
| Urbanization | ||||||
| Urban | Reference | |||||
| Suburban | 0.93 | 0.79–1.09 | 0.37 | 1.13 | 0.95–1.36 | 0.17 |
| Medium Metro | 0.88 | 0.73–1.05 | 0.15 | 1.01 | 0.83–1.22 | 0.93 |
| Small Metro/Rural | 0.91 | 0.76–1.08 | 0.28 | 1.07 | 0.88–1.30 | 0.48 |
| Household Poverty† | 1.10 | 1.07–1.14 | <0.001 | |||
| Neighborhood poverty‡ | 1.20 | 1.14–1.26 | <0.001 | 1.09 | 1.02–1.16 | 0.008 |
Adjusted for age, sex, race/ethnicity, region, neighborhood poverty, urban/rural status and birth outside the US.
1 Unit decrease in ratio of household income to the poverty line
10 percentage point increase in households living below the poverty line
Neighborhood Poverty
A 10 percentage point increase in the number of households living below the poverty line (neighborhood poverty) was associated with a 10% increase in the odds of prevalent asthma in crude analyses (OR: 1.10, 95% CI, 1.05–1.14, p<0.001), although this was no longer significant in adjusted analyses (OR 1.04, 95% CI, 0.99–1.10, p=0.09). Race/ethnicity was found to significantly modify the relationship between neighborhood poverty and prevalent asthma (p=0.004 for the interaction between Hispanic ethnicity and neighborhood poverty), with neighborhood poverty as a significant risk factor among non-Hispanics and Puerto Ricans in adjusted analyses but protective among Hispanics (Table 2). Sensitivity analyses including whether the child received well child care in the past year or was uninsured at any point did not materially change the results of these analyses or those of residence in an urban neighborhood (data not shown).
Individual Level Household Poverty
In unadjusted analyses, a one unit decrease in the household income to poverty ratio was associated with a 7% increase in odds of prevalent asthma (95% CI, 1.05–1.10, p<0.001), with similar results in the model that adjusted for race/ethnicity, urban/rural status, region, age, sex and birth in the U.S. (OR: 1.06, 95% CI, 1.03–1.09, p<0.001). As was the case for neighborhood poverty, Hispanic ethnicity significantly modified the relationship between household poverty and prevalent asthma (p=0.002), and household poverty was a risk factor for asthma among non-Hispanics and Puerto Ricans (OR: 1.07, 95% CI, 1.03–1.10, p<0.001) but not Hispanics (OR: 1.00, 95% CI, 0.94–1.07, p=0.94) in adjusted analyses.
When both neighborhood and individual level poverty were included in the model, neighborhood level poverty was no longer a significant predictor of prevalent asthma in the overall or stratified models, but individual level poverty remained an independent predictor overall and among non-Hispanics and Puerto Ricans (eTable 3).
Residence in an Urban Neighborhood
There were no differences in asthma prevalence in suburban, small town, and rural neighborhoods compared to urban neighborhoods in either crude or adjusted analyses overall, or in analyses stratified by Hispanic ethnicity (Table 2) and residence in an urban area did not increase the association between race/ethnicity and asthma prevalence (data not shown). Moreover, living in an urban environment did not increase the association between neighborhood poverty and asthma prevalence (p=0.62).
Asthma Morbidity
Black race, Puerto Rican ethnicity and lower household income were strong independent risk factors for asthma exacerbation and emergency room visits for asthma (Tables 3 and 4 and eTable 3). Neighborhood poverty and urban/rural status were not risk factors in adjusted analyses with the exception of a protective effect of residence in small metro/rural areas compared to urban areas for emergency room visits in fully adjusted models of the overall population and among Non-Hispanics and Puerto Ricans (eTable 3).
Table 3.
Predictors of Asthma Episode
| Crude | Adjusted* | |||||
|---|---|---|---|---|---|---|
| OR | 95% CI | P | OR | 95% CI | P | |
| Overall | ||||||
| Race/ethnicity | ||||||
| White | Reference | |||||
| Black | 1.71 | 1.45–2.01 | <0.001 | 1.64 | 1.36–1.97 | <0.001 |
| Hispanic | 0.78 | 0.65–0.95 | 0.01 | 0.84 | 0.68–1.05 | 0.13 |
| Puerto Rican | 2.32 | 1.67–3.22 | <0.001 | 2.40 | 1.66–3.47 | <0.001 |
| Asian | 0.74 | 0.51–1.08 | 0.11 | 0.93 | 0.63–1.36 | 0.70 |
| Urbanization | ||||||
| Urban | Reference | |||||
| Suburban | 1.02 | 0.85–1.22 | 0.83 | 1.09 | 0.88–1.34 | 0.43 |
| Medium Metro | 1.02 | 0.84–1.26 | 0.78 | 1.09 | 0.87–1.35 | 0.46 |
| Small Metro/Rural | 0.99 | 0.82–1.19 | 0.89 | 1.03 | 0.83–1.29 | 0.77 |
| Region | ||||||
| Northeast | Reference | |||||
| Midwest | 1.01 | 0.80–1.28 | 0.93 | 1.07 | 0.84–1.37 | 0.58 |
| South | 0.99 | 0.80–1.21 | 0.89 | 1.01 | 0.82–1.24 | 0.94 |
| West | 0.82 | 0.66–1.02 | 0.07 | 1.00 | 0.79–1.26 | 0.98 |
| Birth outside the US | 0.31 | 0.20–0.47 | <0.001 | 0.34 | 0.22–0.53 | <0.001 |
| Household Poverty† | 1.06 | 1.02–1.10 | 0.003 | |||
| Neighborhood poverty‡ | 1.06 | 1.00–1.11 | 0.04 | 1.02 | 0.96–1.09 | 0.50 |
| Hispanics | ||||||
| Urbanization | ||||||
| Urban | Reference | |||||
| Suburban | 0.95 | 0.63–1.45 | 0.82 | 0.89 | 0.57–1.39 | 0.61 |
| Medium Metro | 1.26 | 0.87–1.84 | 0.21 | 1.08 | 0.93–1.95 | 0.12 |
| Small Metro/Rural | 0.88 | 0.51–1.54 | 0.66 | 0.87 | 0.50–1.52 | 0.63 |
| Household Poverty† | 0.98 | 0.92–1.03 | 0.4 | |||
| Neighborhood poverty‡ | 0.9 | 0.79–1.02 | 0.09 | 0.91 | 0.80–1.03 | 0.13 |
| Non-Hispanics and Puerto Ricans | ||||||
| Urbanization | ||||||
| Urban | Reference | |||||
| Suburban | 0.94 | 0.76–1.15 | 0.53 | 1.12 | 0.88–1.42 | 0.36 |
| Medium Metro | 0.93 | 0.74–1.17 | 0.53 | 1.05 | 0.81–1.36 | 0.70 |
| Small Metro/Rural | 0.91 | 0.74–1.13 | 0.39 | 1.05 | 0.82–1.35 | 0.70 |
| Household Poverty† | 1.09 | 1.05–1.14 | <0.001 | |||
| Neighborhood poverty‡ | 1.15 | 1.08–1.23 | <0.001 | 1.05 | 0.97–1.13 | 0.20 |
Adjusted for age, sex, race/ethnicity, region, neighborhood poverty, urban/rural status and birth outside the US.
1 Unit decrease in ratio of household income to the poverty line
10 percentage point increase in households living below the poverty line
Table 4.
Predictors of Asthma ER visit
| Crude | Adjusted* | |||||
|---|---|---|---|---|---|---|
| OR | 95% CI | P | OR | 95% CI | P | |
| Overall | ||||||
| Race/ethnicity | ||||||
| White | Reference | |||||
| Black | 4.07 | 3.03–5.46 | <0.001 | 3.45 | 2.45–4.87 | <0.001 |
| Hispanic | 1.41 | 0.98–2.01 | 0.06 | 1.24 | 0.81–1.90 | 0.31 |
| Puerto Rican | 5.41 | 3.23–9.04 | <0.001 | 4.48 | 2.64–7.58 | <0.001 |
| Asian | 0.89 | 0.46–1.73 | 0.74 | 0.96 | 0.48–1.92 | 0.90 |
| Urbanization | ||||||
| Urban | Reference | |||||
| Suburban | 0.61 | 0.41–0.89 | 0.01 | 0.75 | 0.47–1.18 | 0.21 |
| Medium Metro | 0.88 | 0.60–1.29 | 0.52 | 1.06 | 0.70–1.58 | 0.79 |
| Small Metro/Rural | 0.51 | 0.35–0.74 | <0.001 | 0.66 | 0.43–1.02 | 0.06 |
| Region | ||||||
| Northeast | Reference | |||||
| Midwest | 0.74 | 0.49–1.12 | 0.16 | 0.89 | 0.60–1.32 | 0.56 |
| South | 0.82 | 0.58–1.16 | 0.25 | 0.82 | 0.58–1.16 | 0.25 |
| West | 0.66 | 0.43–1.00 | 0.049 | 0.80 | 0.51–1.24 | 0.31 |
| Birth outside the US | 0.36 | 0.19–0.66 | 0.001 | 0.38 | 0.19–0.75 | 0.005 |
| Household Poverty† | 1.22 | 1.13–1.31 | <0.001 | |||
| Neighborhood poverty‡ | 1.24 | 1.14–1.36 | <0.001 | 1.04 | 0.93–1.16 | 0.49 |
| Hispanics | ||||||
| Urbanization | ||||||
| Urban | Reference | |||||
| Suburban | 0.67 | 0.30–1.48 | 0.32 | 0.70 | 0.291.68 | 0.42 |
| Medium Metro | 1.08 | 0.52–2.21 | 0.84 | 1.22 | 0.61–2.46 | 0.57 |
| Small Metro/Rural | 0.65 | 0.20–2.08 | 0.46 | 0.79 | 0.24–2.56 | 0.69 |
| Household Poverty† | 1.06 | 0.90–1.26 | 0.49 | |||
| Neighborhood poverty‡ | 1.04 | 0.83–1.32 | 0.71 | 1.07 | 0.86–1.33 | 0.50 |
| Non-Hispanics and Puerto Ricans | ||||||
| Urbanization | ||||||
| Urban | Reference | |||||
| Suburban | 0.55 | 0.35–0.86 | 0.008 | 0.75 | 0.44–1.26 | 0.28 |
| Medium Metro | 0.80 | 0.52–1.23 | 0.31 | 1.02 | 0.64–1.63 | 0.93 |
| Small Metro/Rural | 0.45 | 0.31–0.67 | <0.001 | 0.65 | 0.41–1.03 | 0.07 |
| Household Poverty† | 1.27 | 1.16–1.38 | <0.001 | |||
| Neighborhood poverty‡ | 1.34 | 1.22–1.48 | <0.001 | 1.03 | 0.90–1.18 | 0.65 |
Adjusted for age, sex, race/ethnicity, region, neighborhood poverty, urban/rural status and birth outside the US.
1 Unit decrease in ratio of household income to the poverty line
10 percentage point increase in households living below the poverty line
DISCUSSION
Although it has long been thought that the prevalence of asthma is high among children living in poor urban neighborhoods in the U.S., the prevalence of asthma in these neighborhoods throughout the U.S. has, surprisingly, not been described. Moreover, the relative contribution of race/ethnicity and household poverty versus other contextual neighborhood factors to asthma disparities related to the inner-city remains unclear. Here we show that although some inner-city areas have high rates of asthma, particularly in the Midwest and Northeast, other non-urban poor areas have equal or higher asthma prevalence. Overall, Black race, Puerto Rican ethnicity and poverty rather than residence in an urban area per se are the major risk factors for prevalent asthma. These findings suggest that the concept of “inner-city asthma” may need to be refined.
Original reports heralding the phenomenon of inner-city asthma were based on findings of very high asthma morbidity and mortality in several cities, including Baltimore, Chicago and New York City, and further research documented that poor neighborhoods in these cities were particularly affected.(1, 5, 7, 8, 19) These urban areas were also disproportionately home to ethnic minorities, particularly Non-Hispanic Blacks and Puerto Ricans, who were known to be at risk for asthma.(4) However, early research found conflicting results about whether racial/ethnic disparities were independent of socioeconomic factors.(3, 6, 20) Since that time, Black race and Puerto Rican ethnicity have become clear risk factors for asthma, although how much this is due to environmental exposures, including urban exposures, or to underlying susceptibility remains unknown. Race is a complex concept that is informed by genetic, cultural and historical factors, and thus it can be hard to parse genetic from environmental risk factors. Degree of African ancestry has been associated with asthma,(29, 30, 31) suggesting a genetic explanation, although it can be difficult to fully account for confounding by socioeconomic status even in genetic analyses,(32, 33) particularly because disparities in wealth, educational opportunities, family structure and employment by race/ethnicity are even higher than what is represented by income(34) and can correlate with ancestry. Here, in a very large, nationally representative dataset, we found that Black race and Puerto Rican ethnicity were strong risk factors for prevalent asthma and asthma morbidity, independent of income, neighborhood poverty and residence in an urban setting, but we cannot exclude residual confounding as an explanation for the association between race/ethnicity and asthma.
Residence in urban areas, a potential risk factor for asthma hypothesized to be mediated by exposure to indoor and outdoor pollution, pest allergens, and violence and other stressful life events,(20, 35) was not found to be a significant risk factor for prevalent asthma or asthma morbidity in this U.S. population-based analysis. The lack of a relationship between urban residence and asthma prevalence even in crude analyses may reflect shifting demographics since the inner-city asthma epidemic was first described. Although urban areas have historically tended to be poor, in recent years the fastest growth in high poverty areas has occurred in suburban and smaller metropolitan areas, with the slowest growth in the largest cities as shown by the U.S. Census’ Decennial and American Communities Surveys.(36, 37) The suburbanization of poverty means that, despite continued high rates of concentrated poverty in cities, there are now more poor people living in suburban than urban communities.(36, 37) The ethnic composition of poor and urban areas has also shifted, with a so-called “reverse migration” of Black populations from Northern cities to the South(38) and an influx of Hispanic populations to urban areas,(39) where they are now the most common ethnic group. These demographic changes challenge the use of “inner-city” as interchangeable with Black race, and mean that focusing on the inner-city may not fully capture the population most at risk for asthma. In this survey, we estimate that inner-city areas now house only 8% of all children with current asthma, compared to the 46% living in suburban or wealthier urban areas, following a similar distribution to children as a whole. The environmental factors contributing to asthma in non-inner city areas, especially poor suburban and medium metro areas, have been relatively less studied than those in the inner-city.
In contrast to residence in an urban area, neighborhood and individual level poverty were both associated with prevalent asthma, although neighborhood poverty was not independent of individual-level household poverty. Poverty may lead to increased risk of asthma through many pathways, as known risk factors for asthma are more common in poorer households, including smoking, shorter duration of breastfeeding, prematurity, higher levels of indoor allergens such as cockroach and mouse allergens, exposure to outdoor pollution such as diesel particles, poorer diet, and psychological stress.(40) Poverty (both neighborhood and household) was a not a risk factor for non-Puerto Rican Hispanics, and was in fact protective, a finding that has been reported in a smaller study in California.(41) Many of the risk factors for asthma that are found in poorer households in general may actually be less common among poorer, less acculturated, Hispanic households.(42) Increased acculturation has been linked to higher prevalence of asthma risk factors including shorter duration of breastfeeding,(43) smoking,(44) prematurity(45, 46) and poor diet,(47) and has been shown to be a risk factor for asthma among Mexican Hispanics.(48, 49) Although we adjusted for the subject child’s birth outside the U.S., our analyses did not adjust for the immigration status of the child’s parent, and thus acculturation is a potential explanation for the inverse relationship between poverty and asthma we found among Hispanics, although differences in diagnosis and gene-by-environment interactions may also play a role.
There are several important caveats to our findings. First, because the research questions addressed in this study could only be answered with a very large study population, the data, by necessity, were by self-report. Differences in likelihood of diagnosis of asthma by race, socio332 economic status or geography could potentially bias our results. However, assessment of asthma by the NHIS questions is a standard and well-accepted approach to identifying asthma(50), and self-report of race/ethnicity is considered the gold standard. Second, there is potential for misclassification of neighborhood characteristics, because subjects were surveyed in 2009–10, but were assigned to year 2000 census tracts in the NHIS survey. These tracts were linked to year 2000 census data for poverty and year 2005 urban/rural definitions. We expect that any changes in distribution of neighborhood poverty over the past decade, leading to misclassification of neighborhood poverty, are likely to lead to a bias towards the null in our analyses of the relationship between neighborhood poverty and asthma, while urban/rural status is unlikely to change substantially over 4–6 years. Finally, with regards to asthma morbidity, the outcome measures were fairly crude and there was less power than for analyses of asthma prevalence overall, and so we cannot exclude the possibility that residence in an urban area and poverty may have a stronger role in asthma morbidity than prevalent asthma. In addition, access to care, including emergency care, may explain some of our results, particularly the finding that those living in a rural area were less likely to have emergency room visits for asthma. More research is needed to understand how urban/rural status may affect other measures of asthma morbidity and asthma severity. These limitations, however, are countered by the study’s strengths, which are that it is representative of the US population and of sufficient size to disentangle the effects of race/ethnicity, neighborhood poverty and urban residence on asthma.
In conclusion, our work suggests that the concept of “inner-city asthma” may need to be revised. Focusing only on urban areas may miss communities that are also at high risk of asthma, particularly those with high concentrations of Black, Puerto Rican and poor children. This work highlights the need for a broad view of asthma disparities in order to develop the research and public health measures that are most likely to be effective in preventing and managing asthma.
Supplementary Material
Key Messages.
Although the prevalence of asthma is high in some U.S. inner-cities, it is equally high in some poor non-urban areas.
Taking the U.S. as a whole, living in an urban neighborhood is not associated with increased asthma prevalence.
Acknowledgements
This work was supported by the National Institute of Environmental Health Sciences (P50ES015903, P01ES018176, P01ES018181, R01ES019560), the Environmental Protection Agency (R832139, STAR Grant RD83451501, R21HL117772), the National Institute of Allergy and Infectious Diseases (R01AI070630, U01AI083238, T32AI007007, K23AI103187 and R21AI107085), and the National Cancer Institute (K07CA151910). No funder had any role in the design and conduct of the study; collection, management, analysis and interpretation of data, or preparation, review or approval of the manuscript. The findings and conclusions in this paper are those of the author(s) and do not necessarily represent the views of the Centers for Disease Control, the National Center for Health Statistics, or the Research Data Center.
ABBREVIATIONS
- CI
Confidence interval
- NHIS
National Health Interview Survey
- OR
Odds ratio
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Corinne A. Keet, Email: ckeet1@jhmi.edu, Johns Hopkins University School of Medicine, Division of Pediatric Allergy and Immunology.
Meredith C. McCormack, Email: mmccor16@jhmi.edu, Johns Hopkins University School of Medicine, Division of Pulmonary and Critical Care Medicine, Baltimore, MD.
Craig E. Pollack, Email: cpollac2@jhmi.edu, Johns Hopkins University School of Medicine, Division of General Internal Medicine, Baltimore, MD.
Roger D. Peng, Email: rpeng@jhsph.edu, Johns Hopkins Bloomberg School of Public Health, Department of Biostatistics, Baltimore, MD.
Emily McGowan, Email: emcgowa4@jhmi.edu, Johns Hopkins University School of Medicine, Division of Allergy and Clinical Immunology, and Graduate Student, Johns Hopkins Bloomberg School of Public Health, Baltimore, MD.
Elizabeth C. Matsui, Email: ematsui1@jhmi.edu, Johns Hopkins University 24 School of Medicine, Division of Pediatric Allergy and Immunology, Baltimore, MD.
References
- 1.Mak H, Johnston P, Abbey H, Talamo RC. Prevalence of asthma and health service utilization of asthmatic children in an inner city. J Allergy Clin Immunol. 1982;70(5):367–372. doi: 10.1016/0091-6749(82)90026-4. [DOI] [PubMed] [Google Scholar]
- 2.Booth S, Degroot I, Markush R, Horton RJ. Detection of Asthma Epidemics in Seven Cities. Arch Environ Health. 1965;10:152–155. doi: 10.1080/00039896.1965.10663974. [DOI] [PubMed] [Google Scholar]
- 3.Gergen PJ, Mullally DI, Evans R., 3rd National survey of prevalence of asthma among children in the United States, 1976 to 1980. Pediatrics. 1988;81(1):1–7. [PubMed] [Google Scholar]
- 4.Gergen PJ, Weiss KB. Changing patterns of asthma hospitalization among children: 1979 to 1987. JAMA. 1990;264(13):1688–1692. [PubMed] [Google Scholar]
- 5.Weiss KB, Wagener DK. Changing patterns of asthma mortality. Identifying target populations at high risk. JAMA. 1990;264(13):1683–1687. [PubMed] [Google Scholar]
- 6.Weitzman M, Gortmaker S, Sobol A. Racial, social, and environmental risks for childhood asthma. Am J Dis Child. 1990;144(11):1189–1194. doi: 10.1001/archpedi.1990.02150350021016. [DOI] [PubMed] [Google Scholar]
- 7.Carr W, Zeitel L, Weiss K. Variations in asthma hospitalizations and deaths in New York City. Am J Public Health. 1992;82(1):59–65. doi: 10.2105/ajph.82.1.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Marder D, Targonski P, Orris P, Persky V, Addington W. Effect of racial and socioeconomic factors on asthma mortality in Chicago. Chest. 1992;101(6 Suppl):426S–429S. doi: 10.1378/chest.101.6_supplement.426s. [DOI] [PubMed] [Google Scholar]
- 9.Busse WW. The National Institutes of Allergy and Infectious Diseases networks on asthma in inner-city children: an approach to improved care. The Journal of allergy and clinical immunology. 2010;125(3):529–537. doi: 10.1016/j.jaci.2010.01.036. quiz 38–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Togias A, Fenton MJ, Gergen PJ, Rotrosen D, Fauci AS. Asthma in the inner city: the perspective of the National Institute of Allergy and Infectious Diseases. J Allergy Clin Immunol. 2010;125(3):540–544. doi: 10.1016/j.jaci.2010.01.040. [DOI] [PubMed] [Google Scholar]
- 11.Bryant-Stephens T, West C, Dirl C, Banks T, Briggs V, Rosenthal M. Asthma prevalence in Philadelphia: description of two community-based methodologies to assess asthma prevalence in an inner-city population. J Asthma. 2012;49(6):581–585. doi: 10.3109/02770903.2012.690476. [DOI] [PubMed] [Google Scholar]
- 12.Gupta RS, Zhang X, Sharp LK, Shannon JJ, Weiss KB. Geographic variability in childhood asthma prevalence in Chicago. J Allergy Clin Immunol. 2008;121(3):639–645. e1. doi: 10.1016/j.jaci.2007.11.036. [DOI] [PubMed] [Google Scholar]
- 13.Claudio L, Stingone JA, Godbold J. Prevalence of childhood asthma in urban communities: the impact of ethnicity and income. Ann Epidemiol. 2006;16(5):332–340. doi: 10.1016/j.annepidem.2005.06.046. [DOI] [PubMed] [Google Scholar]
- 14.Mvula M, Larzelere M, Kraus M, Moisiewicz K, Morgan C, Pierce S, et al. Prevalence of asthma and asthma-like symptoms in inner-city schoolchildren. J Asthma. 2005;42(1):9–16. doi: 10.1081/jas-200044746. [DOI] [PubMed] [Google Scholar]
- 15.Gerbasi TR. Socioeconomic variation in asthma hospitalization: excess utilization or greater need? Pediatrics. 2000;105(5):1171. doi: 10.1542/peds.105.5.1171. [DOI] [PubMed] [Google Scholar]
- 16.Crain EF, Weiss KB, Bijur PE, Hersh M, Westbrook L, Stein RE. An estimate of the prevalence of asthma and wheezing among inner-city children. Pediatrics. 1994;94(3):356–362. [PubMed] [Google Scholar]
- 17.Buescher PA, Jones-Vessey K. Using Medicaid data to estimate state- and county-level prevalence of asthma among low-income children. Matern Child Health J. 1999;3(4):211–216. doi: 10.1023/a:1022377405914. [DOI] [PubMed] [Google Scholar]
- 18.Shalowitz MU, Sadowski LM, Kumar R, Weiss KB, Shannon JJ. Asthma burden in a citywide, diverse sample of elementary schoolchildren in Chicago. Ambul Pediatr. 2007;7(4):271–277. doi: 10.1016/j.ambp.2007.03.004. [DOI] [PubMed] [Google Scholar]
- 19.Weiss KB, Gergen PJ, Crain EF. Inner-city asthma. The epidemiology of an emerging US public health concern. Chest. 1992;101(6 Suppl):362S–367S. doi: 10.1378/chest.101.6.362s. [DOI] [PubMed] [Google Scholar]
- 20.Aligne CA, Auinger P, Byrd RS, Weitzman M. Risk factors for pediatric asthma. Contributions of poverty, race, and urban residence. American journal of respiratory and critical care medicine. 2000;162(3 Pt 1):873–877. doi: 10.1164/ajrccm.162.3.9908085. [DOI] [PubMed] [Google Scholar]
- 21.Centers for Disease Control and Prevention: 2009. Centers for Disease Control and Prevention, U.S. Department of Health and Human Services; 2010. [Google Scholar]
- 22.NHIS Survey Description: 2010. Centers for Disease Control and Prevention, U.S. Department of Health and Human Services; 2011. [Google Scholar]
- 23.NHIS Survey Description: 2011. Centers for Disease Control and Prevention, U.S. Department of Health and Human Services; 2012. [Google Scholar]
- 24.Ingram DD, Franco SJ. NCHS urban-rural classification scheme for counties. Vital Health Stat 2. 2012;(154):1–65. [PubMed] [Google Scholar]
- 25.Lara M, Akinbami L, Flores G, Morgenstern H. Heterogeneity of childhood asthma among Hispanic children: Puerto Rican children bear a disproportionate burden. Pediatrics. 2006;117(1):43–53. doi: 10.1542/peds.2004-1714. [DOI] [PubMed] [Google Scholar]
- 26.Duncan C, Jones K, Moon G. Context, composition and heterogeneity: using multilevel models in health research. Social science & medicine. 1998;46(1):97–117. doi: 10.1016/s0277-9536(97)00148-2. [DOI] [PubMed] [Google Scholar]
- 27.Multiple Imputation of Family Income and Personal Earnings in the National Health Interview Survey: Methods and Examples. Division of Health Interview Statistics, National Center for Health Statistics. 2011 [Google Scholar]
- 28.Rubin DB. Multiple imputation for nonresponse in surveys. New York: Wiley; 1987. p. xxix.p. 258. [Google Scholar]
- 29.Vergara C, Caraballo L, Mercado D, Jimenez S, Rojas W, Rafaels N, et al. African ancestry is associated with risk of asthma and high total serum IgE in a population from the Caribbean Coast of Colombia. Hum Genet. 2009;125(5–6):565–579. doi: 10.1007/s00439-009-0649-2. [DOI] [PubMed] [Google Scholar]
- 30.Flores C, Ma SF, Pino-Yanes M, Wade MS, Perez-Mendez L, Kittles RA, et al. African ancestry is associated with asthma risk in African Americans. PLoS One. 2012;7(1):e26807. doi: 10.1371/journal.pone.0026807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Choudhry S, Seibold MA, Borrell LN, Tang H, Serebrisky D, Chapela R, et al. Dissecting complex diseases in complex populations: asthma in latino americans. Proc Am Thorac Soc. 2007;4(3):226–233. doi: 10.1513/pats.200701-029AW. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Brehm JM, Acosta-Perez E, Klei L, Roeder K, Barmada MM, Boutaoui N, et al. African ancestry and lung function in Puerto Rican children. J Allergy Clin Immunol. 2012;129(6):1484–1490. e6. doi: 10.1016/j.jaci.2012.03.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kumar R, Nguyen EA, Roth LA, Oh SS, Gignoux CR, Huntsman S, et al. Factors associated with degree of atopy in Latino children in a nationwide pediatric sample: the Genes-environments and Admixture in Latino Asthmatics (GALA II) study. J Allergy Clin Immunol. 2013;132(4):896–905. e1. doi: 10.1016/j.jaci.2013.02.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sampson RJ, Sharkey P, Raudenbush SW. Durable effects of concentrated disadvantage on verbal ability among African-American children. Proc Natl Acad Sci U S A. 2008;105(3):845–852. doi: 10.1073/pnas.0710189104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Busse WW, Mitchell H. Addressing issues of asthma in inner-city children. J Allergy Clin Immunol. 2007;119(1):43–49. doi: 10.1016/j.jaci.2006.10.021. [DOI] [PubMed] [Google Scholar]
- 36.Howell AJ, Timberlake JM. Racial and Ethnic Trends in the Suburbanization of Poverty in Us Metropolitan Areas, 1980–2010. J Urban Aff. 2014;36(1):79–98. [Google Scholar]
- 37.Kneebone E. The Changing Geography of Metropolitan Poverty. The Atlantic Magazine. 2012 Sep 20; [Google Scholar]
- 38.Rastogi SJT, Hoeffel E, Drewery M. The Black Population: 2010. U.S. Department of Commerce. 2011 [Google Scholar]
- 39.Jargowsky PA. Concentration of Poverty in the New Millennium: Changes in the Prevalence, Composition, and Location of High-Poverty Neighborhoods. New York: The Century Foundation and Rutgers CURE; 2013. [Google Scholar]
- 40.Wright RJ, Subramanian SV. Advancing a multilevel framework for epidemiologic research on asthma disparities. Chest. 2007;132(5 Suppl):757S–769S. doi: 10.1378/chest.07-1904. [DOI] [PubMed] [Google Scholar]
- 41.Thakur N, Oh SS, Nguyen EA, Martin M, Roth LA, Galanter J, et al. Socioeconomic status and childhood asthma in urban minority youths. The GALA II and SAGE II studies. Am J Respir Crit Care Med. 2013;188(10):1202–1209. doi: 10.1164/rccm.201306-1016OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Negy C, Woods DJ. A Note on the Relationship between Acculturation and Socioeconomic-Status. Hispanic J Behav Sci. 1992;14(2):248–251. [Google Scholar]
- 43.Ahluwalia IB, D'Angelo D, Morrow B, McDonald JA. Association between acculturation and breastfeeding among Hispanic women: data from the Pregnancy Risk Assessment and Monitoring System. J Hum Lact. 2012;28(2):167–173. doi: 10.1177/0890334412438403. [DOI] [PubMed] [Google Scholar]
- 44.Kaplan RC, Bangdiwala SI, Barnhart JM, Castaneda SF, Gellman MD, Lee DJ, et al. Smoking among u.s. Hispanic/Latino adults: the Hispanic community health study/study of latinos. Am J Prev Med. 2014;46(5):496–506. doi: 10.1016/j.amepre.2014.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Crump C, Lipsky S, Mueller BA. Adverse birth outcomes among Mexican-Americans: are US-born women at greater risk than Mexico-born women? Ethn Health. 1999;4(1–2):29–34. doi: 10.1080/13557859998164. [DOI] [PubMed] [Google Scholar]
- 46.Shaw RJ, Pickett KE. The health benefits of Hispanic communities for non-Hispanic mothers and infants: another Hispanic paradox. Am J Public Health. 2013;103(6):1052–1057. doi: 10.2105/AJPH.2012.300985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wiley JF, Cloutier MM, Wakefield DB, Hernandez DB, Grant A, Beaulieu A, et al. Acculturation determines BMI percentile and noncore food intake in Hispanic children. J Nutr. 2014;144(3):305–310. doi: 10.3945/jn.113.182592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Mosnaim GS, Sadowski LS, Durazo-Arvizu RA, Sharp LK, Curtis LM, Shalowitz MU, et al. Parental language and asthma among urban Hispanic children. J Allergy Clin Immunol. 2007;120(5):1160–1165. doi: 10.1016/j.jaci.2007.08.040. [DOI] [PubMed] [Google Scholar]
- 49.Gold DR, Acevedo-Garcia D. Immigration to the United States and acculturation as risk factors for asthma and allergy. J Allergy Clin Immunol. 2005;116(1):38–41. doi: 10.1016/j.jaci.2005.04.033. [DOI] [PubMed] [Google Scholar]
- 50.Moorman JE, Person CJ, Zahran HS. Asthma attacks among persons with current asthma - United States, 2001–2010. MMWR Surveill Summ. 2013;62(Suppl 3):93–98. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.