SUMMARY
Systemic inflammation causes learning and memory deficits through mechanisms that remain poorly understood. Here, we studied the pathogenesis of memory loss associated with inflammation and found that we could reverse memory deficits by pharmacologically inhibiting α5-subunit-containing γ-aminobutyric acid type A (α5GABAA) receptors and deleting the gene associated with the α5 subunit. Acute inflammation reduces long-term potentiation, a synaptic correlate of memory, in hippocampal slices from wild-type mice, and this reduction was reversed by inhibition of α5GABAA receptor function. A tonic inhibitory current generated by α5GABAA receptors in hippocampal neurons was increased by the key proinflammatory cytokine interleukin-1β through a p38 mitogen-activated protein kinase signaling pathway. Interleukin-1β also increased the surface expression of α5GABAA receptors in the hippocampus. Collectively, these results show that α5GABAA receptor activity increases during inflammation and that this increase is critical for inflammation-induced memory deficits.
INTRODUCTION
Acute systemic inflammation caused by a variety of disorders, including autoimmune diseases, infection, traumatic brain injury, and stroke, can lead to memory loss (Dantzer et al., 2008; Di-Filippo et al., 2008; Kipnis et al., 2008; Yirmiya and Goshen, 2011). Such memory loss manifests as impaired explicit recall in humans, and deficiencies of fear-associated memory and reduced performance for object-recognition tasks in laboratory animals (Yirmiya and Goshen, 2011). Inflammation also contributes to chronic neurodegenerative diseases that are characterized by memory loss, including Alzheimer disease, Parkinson disease, multiple sclerosis, and even AIDS-related dementia (Di Filippo et al., 2008; Kipnis et al., 2008; Yirmiya and Goshen, 2011).
Systemic inflammation increases the production of multiple cytokines in the brain, including interleukin-1β (IL-1β), tumor necrosis factor-α (TNF-α), and IL-6 (Dantzer et al., 2008; Yirmiya and Goshen, 2011). In particular, elevated levels of IL-1β are known to contribute to inflammation-induced memory deficits. For example, in patients with sepsis-associated encephalopathy, increased plasma levels of IL-1β were correlated with cognitive deficits (Serantes et al., 2006). In another study, elderly people with a genetic variant of the IL-1β-converting enzyme that produces lower levels of IL-1β exhibited better cognitive performance than the general aged population (Trompet et al., 2008). In laboratory animals that underwent orthopedic surgery, elevated levels of IL-1β in the hippocampus were strongly correlated with memory deficits (Cibelli et al., 2010). Furthermore, it was shown that memory deficits associated with elevated levels of IL-1b were typically hippocampus dependent, whereas hippo-campus-independent memory was spared (Yirmiya and Goshen, 2011).
The mechanisms underlying inflammation-induced memory deficits are not well understood. Changes involving multiple neurotransmitter receptors have been demonstrated, including a reduction in N-methyl-D-aspartate (NMDA) receptor activity, alterations in the trafficking and phosphorylation of 2-amino-3-(5-methyl-3-oxo-1,2-oxazol-4-yl)propanoic acid receptors, and activation of the α7 subtype of nicotinic acetylcholine receptors (Stellwagen et al., 2005; Terrando et al., 2011; Viviani et al., 2003). However, despite a long history of investigation, no treatments that effectively reverse or prevent the memory deficits associated with inflammation are available. General inhibition of the inflammatory response and specific blocking of IL-1β activity by inhibiting the membrane-bound type 1 IL-1 receptors are impractical approaches because of the risks of infection and delayed wound healing (Fleischmann et al., 2006). Moreover, low basal levels of IL-1β in the hippocampus play a physiological role in maintaining normal memory performance (Yirmiya and Goshen, 2011). Thus, identification of additional down-stream mediators of inflammation that induce memory loss is necessary for the development of effective treatments.
The inhibitory neurotransmitter γ-aminobutyric acid (GABA) is a powerful regulator of learning, memory, and synaptic plasticity (Collinson et al., 2002). GABA type A (GABAA) receptors generate two distinct forms of inhibition: phasic, fast inhibitory postsynaptic currents and a tonic form of inhibition that is primarily mediated by extrasynaptic GABAA receptors (Brickley and Mody, 2012; Glykys and Mody, 2007; Luscher et al., 2011). In the CA1 subfield of the hippocampus, a tonic inhibitory conductance is generated mainly by the α5-subunit-containing subtype of GABAA (α5GABAA) receptors (Caraiscos et al., 2004), which are likely composed of α5b3γ2 subunits (Burgard et al., 1996; Glykys and Mody, 2007; Ju et al., 2009). Drugs that increase α5GABAA receptor activity cause profound memory blockade (Cheng et al., 2006; Martin et al., 2009). Conversely, a reduction in the expression or function of this receptor improves performance for certain memory tasks (Collinson et al., 2002; Martin et al., 2010). Here, using a combination of behavioral studies, electro-physiological recordings, and biochemical methods together with genetic and pharmacological tools, we sought to determine whether increased α5GABAA receptor activity contributes to inflammation-induced memory deficits. The results of these studies show that α5GABAA receptors are critical downstream mediators of inflammation-induced memory deficits.
RESULTS
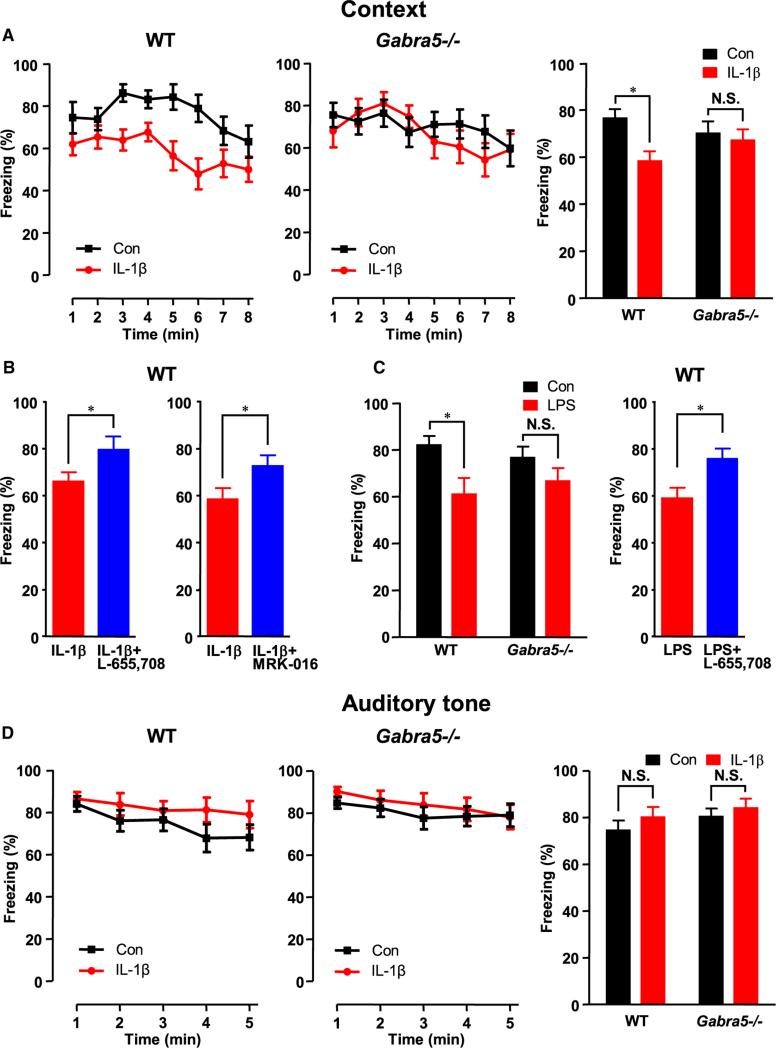
α5GABAA Receptors Regulate Inflammation-Induced Impairment of Contextual Fear Memory
We first investigated the role of α5GABAA receptors in inflammation-induced deficits using a fear-associated memory paradigm (Fanselow and Poulos, 2005). Wild-type (WT) and α5-subunit null mutant (Gabra5−/−) mice were treated with IL-1β (1 μg kg−1, i.p.) to mimic acute systemic inflammation (Yirmiya and Goshen, 2011). Three hours after treatment, the mice were trained to associate an electric foot shock (unconditioned stimulus) with an environmental context and a tone (conditioned stimuli). To study contextual fear memory, which is hippocampus dependent (Fanselow and Poulos, 2005), we reexposed the mice to the same environmental context 24 hr after training. To study cued fear memory in response to tone, which is hippocampus independent (Fanselow and Poulos, 2005), we reexposed the mice to the tone after training. The percentage of time that each mouse spent freezing in the same context or in response to the tone was used to assess memory. IL-1β-treated WT mice showed impairment of contextual fear memory, as evidenced by lower freezing scores compared with vehicle-treated controls (Figure 1A; n = 14–16; two-way analysis of variance [ANOVA], effect of IL-1β, F(1,56) = 5.60, p = 0.02; effect of geno-type, F(1,56) = 0.07, p = 0.79; effect of interaction, F(1,56) = 2.86, p = 0.10; Bonferroni post hoc test, p < 0.05), as shown previously (Yirmiya and Goshen, 2011). In contrast, Gabra5−/− mice treated with IL-1β exhibited no memory deficits (Figure 1A; n = 14–16; Bonferroni post hoc test, p > 0.05).
Figure 1. Inflammation-Induced Impairment of Contextual Fear Memory Is Absent in Gabra5−/− Mice and Can Be Prevented by Pharmacological Inhibition of α5GABAA Receptor in WT Mice.
(A) IL-1β reduced the freezing scores for contextual fear memory only in WT mice. The bar graph shows the summarized results.
(B) L-655,708 or MRK-016 restored the freezing scores for contextual fear memory to control values in WT mice.
(C) LPS reduced the freezing scores for contextual fear memory only in WT mice, and L-655,708 restored the freezing scores to control values in WT mice.
(D) IL-1β did not affect the freezing scores for cued fear memory in response to tone in both WT and Gabra5−/− mice. Data are represented as mean ± SEM. Here and in subsequent figures, Con stands for control. *p < 0.05, **p < 0.01, ***p < 0.001, N.S.: nonsignificant result. See also Figure S1.
To determine whether pharmacological inhibition of α5GABAA receptors would prevent the memory deficit, we studied the effects of two benzodiazepine inverse agonists that preferentially inhibit α5GABAA receptors (Atack et al., 2009; Quirk et al., 1996). At 30 min before fear conditioning, the mice were treated with either L-655,708 [ethyl (13aS)-7-methoxy-9-oxo-11,12,13,13a-tetrahydro-9H-imidazo[1,5-α]pyrrolo[2,1-c] [1,4]benzodiazepine-1-carboxylate] (0.35 or 0.5 mg kg−1, i.p.) or MRK-016 [3-tert-butyl-7-(5-methylisoxazol-3-yl)-2-(1-methyl-1H-1,2,4-triazol-5-ylmethoxy)-pyrazolo[1,5-d][1,2,4]triazine] (3 mg kg−1, i.p.). Of note, under baseline conditions, L-655,708 does not modify contextual fear memory in WT or Gabra5−/− mice (Martin et al., 2010). However, L-655,708 reversed the contextual fear memory deficits induced by IL-1β in WT mice (Figure 1B; n = 11; Student's t test, t = 2.0, p = 0.03). Similarly, another inverse agonist that is structurally distinct from L-655,708, MRK-016, attenuated the contextual fear memory deficits induced by IL-1β in WT mice (Figure 1B; n = 16; Student's t test, t = 2.1, p = 0.04).
We next used a widely employed model of systemic inflammation to probe whether elevated levels of endogenous cytokines also impair memory through activation of α5GABAA receptors. WT and Gabra5−/− mice were treated with the gram-negative bacterial endotoxin lipopolysaccharide (LPS; 125 μg kg−1, i.p.) 3 hr before behavioral training. WT mice, but not Gabra5−/− mice, exhibited a reduction in contextual fear memory after treatment with LPS (Figure 1C; n = 10–15; two-way ANOVA, effect of LPS, F(1,53) = 8.16, p = 0.006; effect of genotype, F(1,53) = 0.0005, p = 0.98; effect of interaction, F(1,53) = 1.02, p = 0.32; Bonferroni post hoc test, p < 0.05 for WT). The deficit exhibited by WT mice was reversed by inhibiting α5GABAA receptors with L-655,708 (Figure 1C; n = 10–11; Student's t test, t = 2.7, p = 0.01).
Of interest, treatment with either IL-1β or LPS did not affect cued fear memory in response to the conditioned tone (Figures 1D and S1; n = 14–16; two-way ANOVA, effect of IL-1β, F(1,54) = 1.28, p = 0.26; effect of genotype, F(1,54) = 1.45, p = 0.23; effect of interaction, F(1,54) = 0.06, p = 0.80). Collectively, these results suggest that the impairment of memory induced by inflammation did not result from a global disruption of cognitive processes, but rather from disruption of hippocampal function.
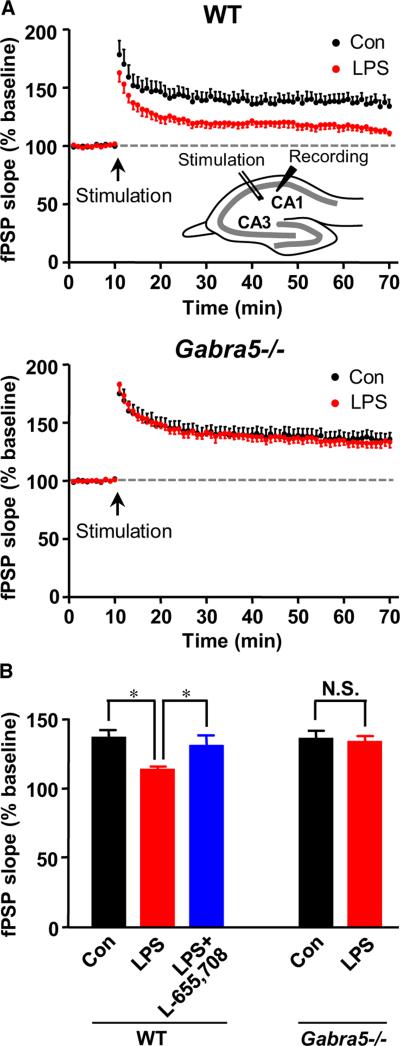
α5GABAA Receptors Regulate Inflammation-Induced Impairment of Long-Term Potentiation
Long-term potentiation (LTP), which refers to the prolonged enhancement of excitatory synaptic transmission, is a widely studied cellular model of learning and memory (Lynch, 2004). We next examined whether the activity of α5GABAA receptors regulates the impairment of LTP induced by acute inflammation. Brain slices were prepared from mice 3 hr after they were injected with the endotoxin LPS (125 μg kg−1, i.p.). Theta burst stimulation of the Schaffer collateral pathway was used to induce LTP in the CA1 subfield of the hippocampus, and field postsynaptic potentials (fPSPs) were recorded before and after stimulation (Figure 2A, inset). In slices from the vehicle-treated WT mice, after stimulation, the slope of the fPSPs increased to 136.1% ± 5.6% of baseline (n = 9). In contrast, in slices from the LPS-treated mice, the increase in LTP was only 113.1% ± 2.5% of baseline (n = 10; one-way ANOVA, F(2,26) = 4.38, p = 0.02; New-man-Keuls post hoc test, p < 0.05; Figures 2A and 2B). Pharmacological inhibition of α5GABAA receptors in hippo-campal slices by application of L-655,708 (20 nM) eliminated LPS-induced reduction of LTP (fPSP slope: 130.3% ± 7.7% of baseline, n = 10; one-way ANOVA followed by Newman-Keuls post hoc test, p < 0.05; Figure 2B). Furthermore, in slices from Gabra5−/− mice, LPS failed to impair LTP. The fPSP slope was 133.1% ± 4.3% of baseline for LPS treatment (n = 15) compared with 135.4% ± 5.9% of baseline for vehicle treatment (n = 13; Figures 2A and 2B), and there was no significant difference compared with the WT (two-way ANOVA, effect of LPS, F(1,43) = 6.33, p = 0.02; effect of genotype, F(1,43) = 3.71, p = 0.06; effect of interaction, F(1,43) = 4.28, p = 0.04; Bonferroni post hoc test, p > 0.05 for Gabra5−/−). Together, these results suggest that α5GABAA receptors are required for inflammation-induced impairment of LTP.
Figure 2. Inflammation Attenuates LTP in CA1 Region Only in WT Mice and This Can Be Prevented by Pharmacological Inhibition of α5GABAA Receptor.
(A) LPS impaired LTP induced by theta burst stimulation only in slices from WT mice. See also Figure S2.
(B) Summarized data showing the last 5 min of the recording. Note that pharmacological inhibition of α5GABAA receptors with L-655,708 prevented the impairment of LTP by LPS. Perfusion of the slices with L-655,708 (20 nM) was started 10 min before the stimulation and was present for LTP recording. Data are represented as mean ± SEM.
Next, to determine whether the LPS-induced reduction in LTP was mediated in part by IL-1β binding to the IL-1 receptor, as was suggested previously (Lynch et al., 2004), slices from LPS-treated mice were incubated with the specific IL-1 receptor antagonist (IL-1ra; 100 ng ml−1 for 1 hr before recording). IL-1ra restored LTP to 126.2% ± 3.9% of baseline (n = 10; p < 0.05 compared with LPS; Figure S2), which confirmed that the reduction in LTP was largely mediated by an increase in IL-1β activity.
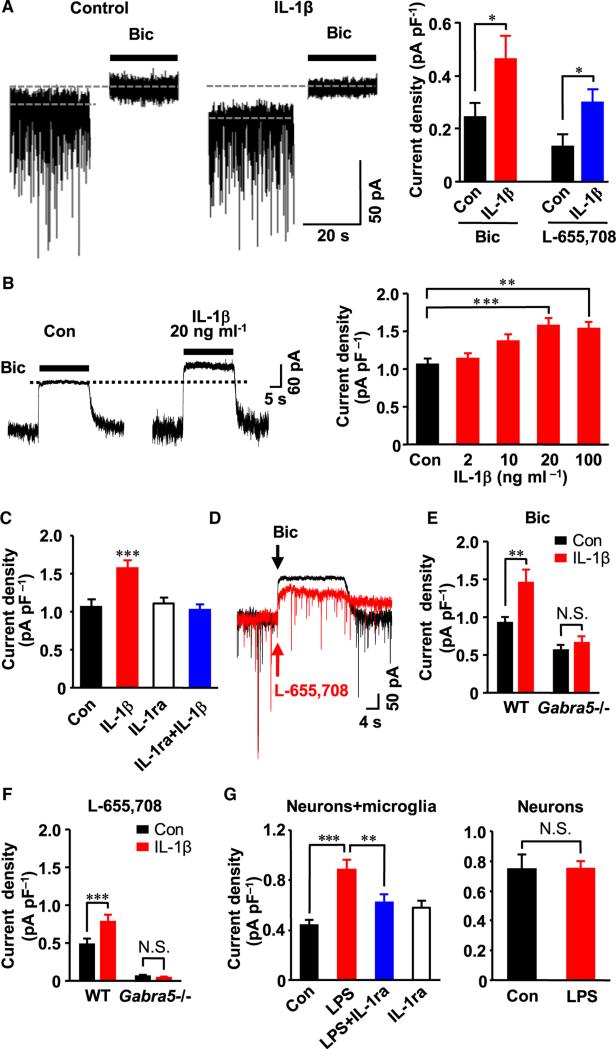
IL-1β Increases the Tonic Current in the CA1 region
In the CA1 region of the hippocampus, a tonic inhibitory conductance generated by α5GABAA receptors regulates synaptic plasticity and memory processes (Collinson et al., 2002; Martin et al., 2010), and an increase in the activity of these receptors causes memory deficits (Cheng et al., 2006; Martin et al., 2009). Therefore, we next determined whether IL-1β increases the amplitude of the tonic inhibitory current in CA1 pyramidal neurons by recording whole-cell currents in brain slices from WT mice injected with IL-1β (1 μg kg−1, i.p., 2–3 hr before sacrifice) or vehicle control (0.1% bovine serum albumin in phosphate-buffered saline). To investigate the changes in tonic current, the GABAA receptor antagonist bicuculline (Bic; 10 μM) or L-655,708 (20 nM) was applied, and the reduction in holding current was measured (Caraiscos et al., 2004; Glykys and Mody, 2007). In slices from IL-1β-treated mice, a 2-fold increase in tonic current density revealed by either Bic or L-655,708 was observed relative to vehicle-treated controls (Student's t test, n = 11–14, t = 2.2, p = 0.04 for Bic; n = 6–10, t = 2.3, p = 0.04 for L-655,708; Figure 3A).
Figure 3. IL-1β Increases the Tonic Current.
(A) The tonic current density revealed by Bic (10 mM) and L-655,708 (20 nM) was increased 2-fold in slices from mice treated with IL-1β (1.0 μg kg−1) compared with vehicle-treated controls.
(B–G) IL-1β increased the tonic current generated by α5GABAA receptors in cultured hippocampal neurons.
(B) Exogenous IL-1β (20 min) increased the tonic current, as revealed by the application of Bic (100 μM, left). The concentration-dependent effects of IL-1β on tonic current density are shown on the right (n = 13–22).
(C) IL-1β enhancement of tonic current was blocked by coapplication of IL-1ra (250 ng ml−1, 30 min).
(D) A representative recording showing the tonic currents revealed by Bic (100 μM) or by the inverse agonist for α5GABAA receptors, L-655,708 (20 nM).
(E and F) α5GABAA receptors are necessary for the enhancing effects of IL-1β on the tonic current revealed by (E) Bic (100 μM) and (F) L-655,708 (20 nM); n = 7–13; two-way ANOVA. (E) Effect of IL-1β: F(1,37) = 9.19, p = 0.004; effect of genotype: F(1,37) = 31.14, p < 0.0001; effect of interaction: F(1,37) = 4.35, p = 0.04. (F) Effect of IL-1β: F(1,36) = 8.17, p = 0.007; effect of genotype: F(1,36) = 138.92, p < 0.0001; effect of interaction: F(1,36) = 10.43, p = 0.03. Bonferroni post hoc test, **p < 0.01, ***p < 0.001 compared with control.
(G) The tonic current was increased by treating neuron and microglia cocultures, but not neurons cultured alone, with LPS (100 ng ml−1, overnight). The LPS-enhancing effects on the tonic current were blocked by treating the cocultures with IL-1ra (250 ng ml−1, overnight). Data are represented as mean ± SEM.
See also Figure S3 and Table S1.
IL-1β Increases α5GABAA Receptor Activity in Cultured Neurons
To investigate whether IL-1β directly enhances the tonic inhibitory conductance, whole-cell currents were recorded from cultured hippocampal neurons. The cell culture preparation offers the advantage of a high-throughput assay that can be used to study the effects of proinflammatory cytokines on the tonic and synaptic inhibitory currents. Treatment of the neurons with IL-1β (20 ng ml−1 for 20 min) increased the amplitude of the tonic current by 45% (IL-1β 1.6 ± 0.1 pA pF−1, n = 22, versus control 1.1 ± 0.1 pA pF−1, n = 21; one-way ANOVA, F(4,80) = 7.13, p < 0.0001; Dunnett's post hoc test, p < 0.001 compared with control; Figure 3B). Increasing the concentration and duration of IL-1β treatment (60 ng ml−1 for 3 h) further increased the current amplitude (IL-1β 2.0 ± 0.3 pA pF−1, n = 6, versus control 1.2 ± 0.2 pA pF−1, n = 6; Student's t test, t = 2.21, p = 0.03). No further increase in current amplitude was observed when neurons were treated for 12–15 hr (IL-1β 20 ng ml−1 1.3 ± 0.6 pA pF−1, n = 21, versus control 0.8 ± 0.08 pA pF−1, n = 12; Student's t test, t = 4.05, p = 0.0003). This concentration-dependent increase in tonic current by IL-1β was completely blocked by IL-1ra (250 ng ml−1 for 30 min, n = 11–22; one-way ANOVA, F(3161) = 7.92, p = 0.0002; Dunnett's post hoc test, p < 0.001 compared with control; Figure 3C).
Because acute inflammation is associated with increased levels of other key cytokines, including TNF-α and IL-6 (Dantzer et al., 2008; Yirmiya and Goshen, 2011), we examined the effects of these cytokines on the tonic current. No changes in the tonic current were observed when neurons were treated for 20 min with TNF-α (100 ng ml−1 0.9 ± 0.08 pA pF−1, 500 ng ml−1 1.0 ± 0.1 pA pF−1, versus control 1.0 ± 0.06 pA pF−1, n = 10–14; one-way ANOVA, F(2,34) = 0.05, p = 0.95) or IL-6 (10 ng ml−1 0.9 ± 0.05 pA pF−1, versus control 1.0 ± 0.06 pA pF−1, n = 5; Student's t test, t = 0.50, p = 0.63).
Neurons in the hippocampus express a variety of GABAA receptor subtypes (Glykys and Mody, 2007; Luscher et al., 2011). To further examine whether the IL-1β-enhanced tonic current was indeed mediated by α5GABAA receptors, we used a combination of pharmacological and genetic approaches. We first studied the effects of L-655,708 (20 nM), which inhibited the tonic current in WT neurons by 56.6% ± 9.2% (n = 7; Figure 3D). This effect size is consistent with the efficacy of L-655,708 for inhibition of α5GABAA receptors (Quirk et al., 1996). Next, we found that IL-1β increased the tonic current revealed by both Bic and L-655,708 recorded in WT neurons, but did not increase the tonic current recorded in Gabra5−/− neurons (Figures 3E and 3F). These results suggest that the α5GABAA receptors are necessary for IL-1β enhancement of the tonic current.
We next studied whether elevated levels of endogenous IL-1β also enhance the tonic current. Cocultures of microglia and neurons were prepared and treated with the endotoxin LPS (100 ng ml−1 for 12–15 h) to stimulate release of IL-1β, as previously described (Polazzi and Contestabile, 2006). LPS treatment increased the tonic current, an effect that was fully reversed by treating the cocultures with IL-1ra (250 ng ml−1, n = 13–19; one-way ANOVA, F(3,62) = 7.27, p = 0.0003; Newman-Keuls post hoc test, ** p < 0.01, *** p < 0.001 compared with LPS; Figure 3G). However, the tonic current studied in neurons that were cultured alone, in the absence of microglia, was unchanged by LPS (n = 10–14; Student's t test, t = 0.10, p = 0.92; Figure 3G), which suggests that IL-1β was released from activated microglia in the cocultures (Polazzi and Contestabile, 2006).
In the hippocampus, GABAA receptors also generate fast transient inhibitory postsynaptic currents that are predominantly mediated by GABAA receptors lacking the α5 subunit (Glykys and Mody, 2007). To determine whether IL-1β also enhances synaptic inhibition, we recorded miniature inhibitory postsynaptic currents (mIPSCs) from cultured hippocampal neurons. IL-1β caused a modest reduction in the mIPSCs (Figure S3; Table S1). Collectively, these results suggest that IL-1β preferentially increases the activity of GABAA receptors that generate tonic (but not synaptic) currents.
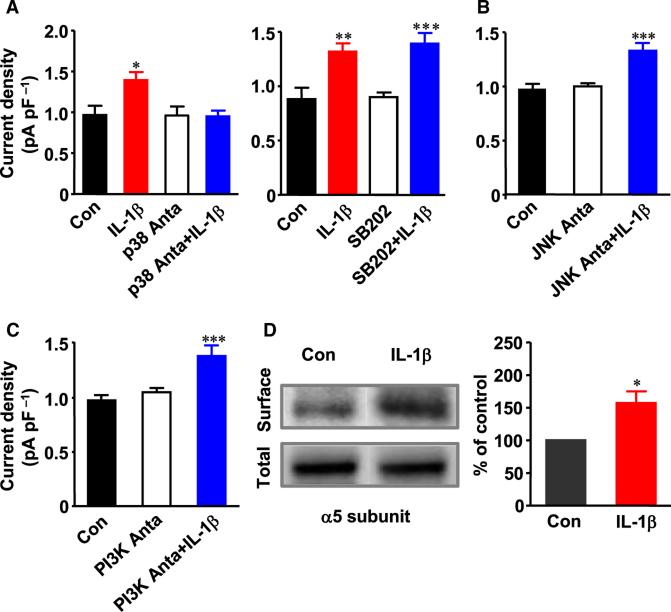
IL-1β Increases the Tonic Current via the p38 Mitogen-Activated Protein Kinase-Dependent Pathway
Next, to identify the predominant signaling pathways by which IL-1β increases the tonic currents, we treated hippocampal neurons with selective kinase inhibitors. SB203,580, an inhibitor of p38 mitogen-activated protein kinase (MAPK), completely blocked the IL-1β-induced increase in the tonic current (n = 10–14; one-way ANOVA, F(3,45) = 4.85, p = 0.005; Dunnett's post hoc test, p < 0.05 compared with control; Figure 4A), whereas its inactive analog, SB202,474 had no effect (n = 9–11; one-way ANOVA, F(3,35) = 11.10, p < 0.0001; Dunnett's post hoc test, ** p < 0.01 *** p < 0.001 compared with control; Figure 4A). This result suggested that p38 MAPK mediates the IL-1β-induced increase in tonic current. Inhibitors of c-Jun N-terminal kinases (JNKs; SP600,125) and phosphatidylinositol 3-kinases (PI3Ks; LY294,002) had no effect on IL-1β enhancement of the tonic current, showing that activation of these kinases was not required (Figures 4B and 4C).
Figure 4. Mechanisms for IL-1β-Induced Enhancement of the Tonic Current.
(A) Treatment with an inhibitor of p38 MAPK, SB203,580 (p38 Anta, 20 μM, 30 min) abolished the effect of IL-1β (20 ng ml−1, 20 min) on the tonic current (left). SB202,474 (SB202, 10 μM, 30 min), an inactive analog of the p38 MAPK inhibitor SB203,580, did not block the enhancing effects of IL-1β on the tonic current (right).
(B and C) IL-1β-induced enhancement of the tonic current was not blocked by the JNK antagonist SP600,125 (JNK Anta, 1 μM, 30 min) or the PI3K antagonist LY294,002 (PI3K Anta, 20 μM, 30 min). (B) n = 11–16; one-way ANOVA, F(2,37) = 14.42, p < 0.0001. (C) n = 10–12; one-way ANOVA, F(2,30) = 11.13, p = 0.0002. Dunnett's post hoc test, ***p < 0.001 compared with control.
(D) The surface expression of the α5 subunit in hippocampal slices treated with IL-1β (20 ng ml−1, 40 min) was increased compared with vehicle-treated control slices. Data are represented as mean ± SEM.
See also Figure S4.
MAPK signaling pathways are important regulators of GABAA receptor trafficking (Luscher et al., 2011). Thus, we studied whether IL-1β increased the expression of α5GABAA receptors on the surface of neurons. Hippocampal slices were treated with IL-1β (20 ng ml−1 for 40 min), and a quantitative western blot analysis of the biotinylated protein was performed (Abramian et al., 2010). The surface expression of the α5-subunit protein in IL-1β-treated slices was increased to 157.4% ± 17.6% of the surface protein measured in vehicle-treated control slices (n = 6, one-sample t test, t = 3.27, p = 0.02; Figure 4D). The surface expression of the α1 and α2 subunits was also studied, because these subunits are widely expressed and contribute primarily to synaptic GABAA receptors (Glykys and Mody, 2007; Luscher et al., 2011). IL-1β decreased the surface expression of the α1 subunit but did not modify the surface expression of the α2 subunit (Figure S4). These results are consistent with the observation that IL-1β caused a modest decrease in the amplitude of postsynaptic currents.
DISCUSSION
The results described here show that inflammation causes memory loss, at least in part, by increasing a tonic inhibitory conductance that is generated by α5GABAA receptors. We observed that genetic or pharmacological inhibition of α5GABAA receptors was sufficient to prevent impairment of contextual fear memory and synaptic plasticity induced by LPS and IL-1β. Further, IL-1β increased the tonic conductance generated by α5GABAA receptors in hippocampal neurons via activation of IL-1 receptors and p38 MAPK-dependent signaling. This increased tonic conductance by IL-1β was most likely due to an increase in the surface expression of α5GABAA receptors.
Multiple signaling pathways are activated by IL-1β binding to the IL-1 receptor, including pathways involving p38 MAPK, JNKs, and PI3Ks (O'Neill, 2002). Our results show that IL-1β enhances the tonic inhibitory conductance mediated by α5GABAA receptors primarily via activation of the p38 MAPK-dependent pathway. Activation of p38 MAPK by IL-1β has been shown in hippocampal neurons (Srinivasan et al., 2004) and cortical neurons (Li et al., 2003). Also, consistent with our results, others have shown that activation of p38 MAPK mediates the effects of IL-1β on hippocampal LTP (Coogan et al., 1999; Kelly et al., 2003).
The increase in tonic current was accompanied by an increase in the surface expression of α5GABAA receptors. Membrane clustering of α5GABAA receptors depends on the presence of radixin, an actin-binding protein that anchors the α5 subunit to cytoskeletal elements (Loebrich et al., 2006). Radixin is targeted by p38 MAPK (Koss et al., 2006), and phosphorylation of radixin could lead to enhanced membrane stability and clustering of α5GABAA receptors at extracellular sites. Alternatively, IL-1β-dependent activation of p38 MAPK could lead to increased activity of downstream mediators such as cAMP response element-binding protein (Srinivasan et al., 2004), which may also enhance the surface expression of α5GABAA receptors.
The available evidence indicates that IL-1β increases the tonic current primarily by increasing the expression of receptors on the surface rather than causing an increase in the concentration of agonist. Specifically, we studied the tonic current in cultured neurons and slices under “concentration-clamp” conditions, in which the extracellular concentration of GABA was fixed. Under these conditions, IL-1β increased the amplitude of the tonic current. Nevertheless, it is plausible that IL-1β also causes a concurrent increase in ambient levels of GABA in the brain in addition to increasing the surface expression of α5GABAA receptors. The concentration of GABA in the extracellular space increases in many proinflammatory states, such as stress (de Groote and Linthorst, 2007), stroke (Clarkson et al., 2010), and pain (Kupers et al., 2009). The increase in extracellular GABA could result from enhanced transmitter release and/or decreased reuptake of GABA. It is unlikely that such an increase in GABA induced by IL-1β is due to synaptic vesicular release, because the frequency of mIPSCs was not increased in the current study. Instead, reduced reuptake via GABA transporters (Wu et al., 2007), as well as increased release of GABA from activated glial cells (Lee et al., 2010), may increase GABA levels in the brain.
It is of interest that inflammation impairs memory performance in response to context but not to tone, because the former (but not the latter) behavior depends on the hippocampus (Fanselow and Poulos, 2005). This result is consistent with the relatively restricted expression of α5GABAA receptors to the hippo-campus (Pirker et al., 2000). In the hippocampus, d-subunit-containing GABAA (δGABAA) receptors are also located in extrasynaptic regions of the neurons, where they generate a tonic inhibitory conductance (Glykys and Mody, 2007). Our results do not rule out the possibility that inflammation modifies other GABAA receptor subtypes, including dGABAA receptors; however, these other subtypes are unlikely to play a role in memory loss. Gabra5−/− mice express dGABAA receptors, yet IL-1β failed to increase the tonic current in the hippocampal neurons of these mice. Also, inflammation did not induce memory deficits in Gabra5−/− mice. Of note, inflammation impairs synaptic plasticity in the dentate gyrus region, where the expression of α5GABAA receptors is low under baseline conditions (Glykys and Mody, 2007; Kelly et al., 2003). The levels of α5GABAA receptors in the dentate gyrus could be increased during inflammation. In support of this notion, the activity of α5GABAA receptors increases in the frontal cortex after ischemic stroke (Clarkson et al., 2010).
The current study has several limitations. The first of these relates to the widely used model that we employed to induce systemic inflammation via intraperitoneal injection of IL-1β and LPS. This experimental model mimics many of the features of acute systemic illness in humans (Yirmiya and Goshen, 2011); however, the method does not restrict the induction of inflammation to the hippocampus. Second, the Gabra5−/− mouse does not limit the reduction of expression either regionally or temporally. Also, global deletion of genes for GABAA receptor subunits can lead to compensatory changes in the expression of other subunits or proteins, although this has not been reported for Gabra5−/− mice (Collinson et al., 2002; Crestani et al., 2002). Behaviors elicited by pharmacological treatments with L-655,708 and MRK-016 faithfully mimicked behaviors exhibited by Gabra5−/− mice. Future studies employing conditional mutagenesis of the Gabra5 gene that is restricted to the CA1 subfield would advance our understanding of the specific role of α5GABAA receptors in the CA1 hippocampus. Finally, although the consequences of injecting various drugs directly into the hippocampus would be of interest, we did not perform such experiments, in part because of the requirement for carefully designed and performed control experiments, given that inflammation induced by surgery (Cibelli et al., 2010) and treatment with general anesthetics (Zurek et al., 2012) can cause long-term impairment of memory performance.
Currently, no treatments are available to reduce the memory deficits associated with inflammation. The results of this study indicate that the attenuation of memory loss by the administration of inverse agonists for α5GABAA receptors is a potential treatment strategy. Because of the restricted expression of α5GABAA receptors in the hippocampus (Pirker et al., 2000), the inverse agonists that inhibit these receptors are generally well tolerated and lack the proconvulsant and anxiogenic properties of nonselective GABAA receptor antagonists (Atack, 2010). Finally, this study may stimulate interest in the effects of inflammation on GABAA receptors that are expressed in tissues outside the nervous system (Watanabe et al., 2002), including the lung and liver. Upregulation of these GABAA receptors may also contribute to organ dysfunction associated with infection, trauma, and immune-related diseases (Dantzer et al., 2008).
EXPERIMENTAL PROCEDURES
All experimental procedures were approved by the Animal Care Committee of the University of Toronto (Toronto, ON, Canada). In all studies, the experimenter was blinded to the drug treatment and genotype of the mice. For behavioral analysis and studies of hippocampal plasticity, male 3- to 4-month-old WT and Gabra5−/− mice were used. Experiments were started 3 hr after injection of IL-1β (1 μg kg−1, i.p.) or LPS (125 μg kg−1, i.p.) because cytokine levels, and particularly IL-1β peak at this time point (Hansen et al., 2000; Yirmiya and Goshen, 2011). Pavlovian fear conditioning was used to study memory performance. Each mouse was trained to associate the context and a 3,600 Hz tone lasting 20 s with an electric foot shock (2 s, 0.5 mA). Each sequence was presented three times, separated by 60 s. LTP was induced in the hippocampal slices with a theta burst stimulation, which consisted of 10 stimulus trains at 5 Hz, with each train consisting of four pulses at 100 Hz. Whole-cell voltage-clamp recordings were obtained from hippocampal slices, cell culture, and neuron-microglia coculture. To record the tonic GABAergic current, 5 or 0.5 μM GABA was added to the slices or cultured neurons, respectively. All recordings were performed at a holding potential of −60 mV. A cell-surface biotinylation assay was used to determine the surface expression of GABAA receptor α1, α2, and α5 subunits. Data are represented as the mean ± SEM. A Student's paired or unpaired t test was used to compare pairs of data. To compare three or more groups, a one-way (drug treatment only) or two-way (drug treatment versus genotype) ANOVA followed by a Dunnett, Newman-Keuls, or Bonferroni post hoc test was used. A one-sample t test was used to compare the surface expression of GABAA receptor subunits. Statistical significance was set at p < 0.05.
Supplementary Material
ACKNOWLEDGMENTS
We thank Ella Czerwinska for her assistance with the cell cultures. This work was supported by Canadian Institutes of Health Research operating grants MOP-38028 and MOP-79428 to B.A.O. A.A.Z. is supported by a Natural Sciences and Engineering Research Council of Canada Graduate Scholarship. I.L. is supported by a Savoy Foundation Studentship. S.A. is supported by a Canadian Anesthesia Society/Vitaid Residents’ Research Grant from the Canadian Anesthesia Research Foundation. P.A.D. is supported by a grant from the National Institute of Alcoholism and Alcohol Abuse, National Institutes of Health (AA017938). B.A.O. holds a Canada Research Chair.
Footnotes
SUPPLEMENTAL INFORMATION
Supplemental Information includes Extended Experimental Procedures, four figures, and one table and can be found with this article online at http://dx.doi.org/10.1016/j.celrep.2012.08.022.
REFERENCES
- Abramian AM, Comenencia-Ortiz E, Vithlani M, Tretter EV, Sieghart W, Davies PA, Moss SJ. Protein kinase C phosphorylation regulates membrane insertion of GABAA receptor subtypes that mediate tonic inhibition. J. Biol. Chem. 2010;285:41795–41805. doi: 10.1074/jbc.M110.149229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Atack JR. Preclinical and clinical pharmacology of the GABAA receptor a5 subtype-selective inverse agonist a5IA. Pharmacol. Ther. 2010;125:11–26. doi: 10.1016/j.pharmthera.2009.09.001. [DOI] [PubMed] [Google Scholar]
- Atack JR, Maubach KA, Wafford KA, O’Connor D, Rodrigues AD, Evans DC, Tattersall FD, Chambers MS, MacLeod AM, Eng WS, et al. In vitro and in vivo properties of 3-tert-butyl-7-(5-methylisoxazol-3-yl)-2-(1-methyl-1H-1,2,4-triazol-5-ylmethoxy)-pyrazolo [1,5-d]-[1,2,4]triazine (MRK-016), a GABAA receptor a5 subtype-selective inverse agonist. J. Pharmacol. Exp. Ther. 2009;331:470–484. doi: 10.1124/jpet.109.157636. [DOI] [PubMed] [Google Scholar]
- Brickley SG, Mody I. Extrasynaptic GABA(A) receptors: their function in the CNS and implications for disease. Neuron. 2012;73:23–34. doi: 10.1016/j.neuron.2011.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burgard EC, Tietz EI, Neelands TR, Macdonald RL. Properties of recombinant g-aminobutyric acid A receptor isoforms containing the a 5 subunit subtype. Mol. Pharmacol. 1996;50:119–127. [PubMed] [Google Scholar]
- Caraiscos VB, Elliott EM, You-Ten KE, Cheng VY, Belelli D, Newell JG, Jackson MF, Lambert JJ, Rosahl TW, Wafford KA, et al. Tonic inhibition in mouse hippocampal CA1 pyramidal neurons is mediated by a5 subunit-containing g-aminobutyric acid type A receptors. Proc. Natl. Acad. Sci. USA. 2004;101:3662–3667. doi: 10.1073/pnas.0307231101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng VY, Martin LJ, Elliott EM, Kim JH, Mount HT, Taverna FA, Roder JC, Macdonald JF, Bhambri A, Collinson N, et al. a5GABAA receptors mediate the amnestic but not sedative-hypnotic effects of the general anesthetic etomidate. J. Neurosci. 2006;26:3713–3720. doi: 10.1523/JNEUROSCI.5024-05.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cibelli M, Fidalgo AR, Terrando N, Ma D, Monaco C, Feldmann M, Takata M, Lever IJ, Nanchahal J, Fanselow MS, Maze M. Role of interleukin-1b in postoperative cognitive dysfunction. Ann. Neurol. 2010;68:360–368. doi: 10.1002/ana.22082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clarkson AN, Huang BS, Macisaac SE, Mody I, Carmichael ST. Reducing excessive GABA-mediated tonic inhibition promotes functional recovery after stroke. Nature. 2010;468:305–309. doi: 10.1038/nature09511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collinson N, Kuenzi FM, Jarolimek W, Maubach KA, Cothliff R, Sur C, Smith A, Otu FM, Howell O, Atack JR, et al. Enhanced learning and memory and altered GABAergic synaptic transmission in mice lacking the a 5 subunit of the GABAA receptor. J. Neurosci. 2002;22:5572–5580. doi: 10.1523/JNEUROSCI.22-13-05572.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coogan AN, O'Neill LA, O'Connor JJ. The P38 mitogen-activated protein kinase inhibitor SB203580 antagonizes the inhibitory effects of interleukin-1b on long-term potentiation in the rat dentate gyrus in vitro. Neuro-science. 1999;93:57–69. doi: 10.1016/s0306-4522(99)00100-1. [DOI] [PubMed] [Google Scholar]
- Crestani F, Keist R, Fritschy JM, Benke D, Vogt K, Prut L, Blüthmann H, Möhler H, Rudolph U. Trace fear conditioning involves hippo-campal a5 GABA(A) receptors. Proc. Natl. Acad. Sci. USA. 2002;99:8980–8985. doi: 10.1073/pnas.142288699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dantzer R, O'Connor JC, Freund GG, Johnson RW, Kelley KW. From inflammation to sickness and depression: when the immune system subjugates the brain. Nat. Rev. Neurosci. 2008;9:46–56. doi: 10.1038/nrn2297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Groote L, Linthorst AC. Exposure to novelty and forced swimming evoke stressor-dependent changes in extracellular GABA in the rat hippocampus. Neuroscience. 2007;148:794–805. doi: 10.1016/j.neuroscience.2007.06.030. [DOI] [PubMed] [Google Scholar]
- Di Filippo M, Sarchielli P, Picconi B, Calabresi P. Neuroinflammation and synaptic plasticity: theoretical basis for a novel, immune-centred, therapeutic approach to neurological disorders. Trends Pharmacol. Sci. 2008;29:402–412. doi: 10.1016/j.tips.2008.06.005. [DOI] [PubMed] [Google Scholar]
- Fanselow MS, Poulos AM. The neuroscience of mammalian associative learning. Annu. Rev. Psychol. 2005;56:207–234. doi: 10.1146/annurev.psych.56.091103.070213. [DOI] [PubMed] [Google Scholar]
- Fleischmann RM, Tesser J, Schiff MH, Schechtman J, Burmester GR, Bennett R, Modafferi D, Zhou L, Bell D, Appleton B. Safety of extended treatment with anakinra in patients with rheumatoid arthritis. Ann. Rheum. Dis. 2006;65:1006–1012. doi: 10.1136/ard.2005.048371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glykys J, Mody I. Activation of GABAA receptors: views from outside the synaptic cleft. Neuron. 2007;56:763–770. doi: 10.1016/j.neuron.2007.11.002. [DOI] [PubMed] [Google Scholar]
- Hansen MK, Nguyen KT, Fleshner M, Goehler LE, Gaykema RP, Maier SF, Watkins LR. Effects of vagotomy on serum endotoxin, cytokines, and corticosterone after intraperitoneal lipopolysaccharide. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2000;278:R331–R336. doi: 10.1152/ajpregu.2000.278.2.R331. [DOI] [PubMed] [Google Scholar]
- Ju YH, Guzzo A, Chiu MW, Taylor P, Moran MF, Gurd JW, MacDonald JF, Orser BA. Distinct properties of murine α 5 γ-aminobutyric acid type a receptors revealed by biochemical fractionation and mass spectroscopy. J. Neurosci. Res. 2009;87:1737–1747. doi: 10.1002/jnr.21991. [DOI] [PubMed] [Google Scholar]
- Kelly A, Vereker E, Nolan Y, Brady M, Barry C, Loscher CE, Mills KH, Lynch MA. Activation of p38 plays a pivotal role in the inhibitory effect of lipopolysaccharide and interleukin-1 b on long term potentiation in rat dentate gyrus. J. Biol. Chem. 2003;278:19453–19462. doi: 10.1074/jbc.M301938200. [DOI] [PubMed] [Google Scholar]
- Kipnis J, Derecki NC, Yang C, Scrable H. Immunity and cognition: what do age-related dementia, HIV-dementia and ‘chemo-brain’ have in common? Trends Immunol. 2008;29:455–463. doi: 10.1016/j.it.2008.07.007. [DOI] [PubMed] [Google Scholar]
- Koss M, Pfeiffer GR, 2nd, Wang Y, Thomas ST, Yerukhimovich M, Gaarde WA, Doerschuk CM, Wang Q. Ezrin/radixin/moesin proteins are phosphorylated by TNF-α and modulate permeability increases in human pulmonary microvascular endothelial cells. J. Immunol. 2006;176:1218–1227. doi: 10.4049/jimmunol.176.2.1218. [DOI] [PubMed] [Google Scholar]
- Kupers R, Danielsen ER, Kehlet H, Christensen R, Thomsen C. Painful tonic heat stimulation induces GABA accumulation in the prefrontal cortex in man. Pain. 2009;142:89–93. doi: 10.1016/j.pain.2008.12.008. [DOI] [PubMed] [Google Scholar]
- Lee S, Yoon BE, Berglund K, Oh SJ, Park H, Shin HS, Augustine GJ, Lee CJ. Channel-mediated tonic GABA release from glia. Science. 2010;330:790–796. doi: 10.1126/science.1184334. [DOI] [PubMed] [Google Scholar]
- Li Y, Liu L, Barger SW, Griffin WS. Interleukin-1 mediates pathological effects of microglia on tau phosphorylation and on synaptophysin synthesis in cortical neurons through a p38-MAPK pathway. J. Neurosci. 2003;23:1605–1611. doi: 10.1523/JNEUROSCI.23-05-01605.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loebrich S, Bähring R, Katsuno T, Tsukita S, Kneussel M. Activated radixin is essential for GABAA receptor a5 subunit anchoring at the actin cytoskeleton. EMBO J. 2006;25:987–999. doi: 10.1038/sj.emboj.7600995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luscher B, Fuchs T, Kilpatrick CL. GABAA receptor trafficking-mediated plasticity of inhibitory synapses. Neuron. 2011;70:385–409. doi: 10.1016/j.neuron.2011.03.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lynch AM, Walsh C, Delaney A, Nolan Y, Campbell VA, Lynch MA. Lipopolysaccharide-induced increase in signalling in hippo-campus is abrogated by IL-10—a role for IL-1 beta? J. Neurochem. 2004;88:635–646. doi: 10.1046/j.1471-4159.2003.02157.x. [DOI] [PubMed] [Google Scholar]
- Lynch MA. Long-term potentiation and memory. Physiol. Rev. 2004;84:87–136. doi: 10.1152/physrev.00014.2003. [DOI] [PubMed] [Google Scholar]
- Martin LJ, Oh GH, Orser BA. Etomidate targets α5 γ-amino-butyric acid subtype A receptors to regulate synaptic plasticity and memory blockade. Anesthesiology. 2009;111:1025–1035. doi: 10.1097/ALN.0b013e3181bbc961. [DOI] [PubMed] [Google Scholar]
- Martin LJ, Zurek AA, MacDonald JF, Roder JC, Jackson MF, Orser BA. a5GABAA receptor activity sets the threshold for long-term potentiation and constrains hippocampus-dependent memory. J. Neurosci. 2010;30:5269–5282. doi: 10.1523/JNEUROSCI.4209-09.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Neill LA. Signal transduction pathways activated by the IL-1 receptor/toll-like receptor superfamily. Curr. Top. Microbiol. Immunol. 2002;270:47–61. [PubMed] [Google Scholar]
- Pirker S, Schwarzer C, Wieselthaler A, Sieghart W, Sperk G. GABA(A) receptors: immunocytochemical distribution of 13 subunits in the adult rat brain. Neuroscience. 2000;101:815–850. doi: 10.1016/s0306-4522(00)00442-5. [DOI] [PubMed] [Google Scholar]
- Polazzi E, Contestabile A. Overactivation of LPS-stimulated microglial cells by co-cultured neurons or neuron-conditioned medium. J. Neuroimmunol. 2006;172:104–111. doi: 10.1016/j.jneuroim.2005.11.005. [DOI] [PubMed] [Google Scholar]
- Quirk K, Blurton P, Fletcher S, Leeson P, Tang F, Mellilo D, Ragan CI, McKernan RM. [3H]L-655,708, a novel ligand selective for the benzodiazepine site of GABAA receptors which contain the a 5 subunit. Neuro-pharmacology. 1996;35:1331–1335. doi: 10.1016/s0028-3908(96)00061-5. [DOI] [PubMed] [Google Scholar]
- Serantes R, Arnalich F, Figueroa M, Salinas M, Andrés-Mateos E, Codoceo R, Renart J, Matute C, Cavada C, Cuadrado A, Montiel C. Interleukin-1β enhances GABAA receptor cell-surface expression by a phosphatidylinositol 3-kinase/Akt pathway: relevance to sepsis-associated encephalopathy. J. Biol. Chem. 2006;281:14632–14643. doi: 10.1074/jbc.M512489200. [DOI] [PubMed] [Google Scholar]
- Srinivasan D, Yen JH, Joseph DJ, Friedman W. Cell type-specific interleukin-1b signaling in the CNS. J. Neurosci. 2004;24:6482–6488. doi: 10.1523/JNEUROSCI.5712-03.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stellwagen D, Beattie EC, Seo JY, Malenka RC. Differential regulation of AMPA receptor and GABA receptor trafficking by tumor necrosis factor-alpha. J. Neurosci. 2005;25:3219–3228. doi: 10.1523/JNEUROSCI.4486-04.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terrando N, Eriksson LI, Ryu JK, Yang T, Monaco C, Feldmann M, Jonsson Fagerlund M, Charo IF, Akassoglou K, Maze M. Resolving postoperative neuroinflammation and cognitive decline. Ann. Neurol. 2011;70:986–995. doi: 10.1002/ana.22664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trompet S, de Craen AJ, Slagboom P, Shepherd J, Blauw GJ, Murphy MB, Bollen EL, Buckley BM, Ford I, Gaw A, et al. PROSPER Group Genetic variation in the interleukin-1 b-converting enzyme associates with cognitive function. The PROSPER study. Brain. 2008;131:1069–1077. doi: 10.1093/brain/awn023. [DOI] [PubMed] [Google Scholar]
- Viviani B, Bartesaghi S, Gardoni F, Vezzani A, Behrens MM, Bartfai T, Binaglia M, Corsini E, Di Luca M, Galli CL, Marinovich M. Interleukin-1β enhances NMDA receptor-mediated intracellular calcium increase through activation of the Src family of kinases. J. Neurosci. 2003;23:8692–8700. doi: 10.1523/JNEUROSCI.23-25-08692.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watanabe M, Maemura K, Kanbara K, Tamayama T, Hayasaki H. GABA and GABA receptors in the central nervous system and other organs. Int. Rev. Cytol. 2002;213:1–47. doi: 10.1016/s0074-7696(02)13011-7. [DOI] [PubMed] [Google Scholar]
- Wu Y, Wang W, Díez-Sampedro A, Richerson GB. Nonvesicular inhibitory neurotransmission via reversal of the GABA transporter GAT-1. Neuron. 2007;56:851–865. doi: 10.1016/j.neuron.2007.10.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yirmiya R, Goshen I. Immune modulation of learning, memory, neural plasticity and neurogenesis. Brain Behav. Immun. 2011;25:181–213. doi: 10.1016/j.bbi.2010.10.015. [DOI] [PubMed] [Google Scholar]
- Zurek AA, Bridgwater EM, Orser BA. Inhibition of α5 γ-Amino-butyric acid type A receptors restores recognition memory after general anesthesia. Anesth. Analg. 2012;114:845–855. doi: 10.1213/ANE.0b013e31824720da. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.