Abstract
Objective
To evaluate the incidence rate of Chronic Kidney Disease (CKD) stage 3-5 (persistent decreased kidney function under 60 mL/min per 1.73 m2) among patients with type 2 diabetes over five years, to identify the risk factors associated with CKD, and develop a risk table to predict five-year CKD stage 3-5 risk stratification for clinical use.
Design
The MADIABETES Study is a prospective cohort study of 3,443 outpatients with type 2 diabetes mellitus, sampled from 56 primary health care centers (131 general practitioners) in Madrid (Spain).
Results
The cumulative incidence of CKD stage 3-5 at five-years was 10.23% (95% CI = 9.12–11.44) and the incidence density was 2.07 (95% CI = 1.83–2.33) cases per 1,000 patient-months or 2.48 (95% CI = 2.19–2.79) cases per 100 patient-years. The highest hazard ratio (HR) for developing CKD stage 3-5 was albuminuria ≥300 mg/g (HR = 4.57; 95% CI= 2.46-8.48). Furthermore, other variables with a high HR were age over 74 years (HR = 3.20; 95% CI = 2.13–4.81), a history of Hypertension (HR = 2.02; 95% CI = 1.42–2.89), Myocardial Infarction (HR= 1.72; 95% IC= 1.25–2.37), Dyslipidemia (HR = 1.68; 95% CI 1.30–2.17), duration of diabetes mellitus ≥ 10 years (HR = 1.46; 95% CI = 1.14-1.88) and Systolic Blood Pressure >149 mmHg (HR = 1.52; 95% CI = 1.02–2.24).
Conclusions
After a five-year follow-up, the cumulative incidence of CKD is concordant with rates described in Spain and other countries. Albuminuria ≥ 300 mg/g and age over 74 years were the risk factors more strongly associated with developing CKD (Stage 3-5). Blood Pressure, lipid and albuminuria control could reduce CKD incidence of CKD in patients with T2DM.
Introduction
Diabetic nephropathy develops in approximately 40% of all type 2 diabetes mellitus (T2DM) patients and is characterized by persistent albuminuria, elevated blood pressure (BP) and a progressive decline in kidney function leading toward end-stage renal disease. In addition, these patients have a high risk of cardiovascular disease, which further increases with deteriorating renal function [1].
The definition of Chronic Kidney Disease (CKD) is based on the presence of kidney damage (proteinuria, haematuria, or anatomical abnormality) or decreased kidney function for three months or more, irrespective of clinical diagnosis. CKD stages 3–5 are defined by a glomerular filtration rate (GFR) <60 mL/min per 1.73 m2, according to the KDOQI classification [2]. The estimated GFR (eGFR) has proven to be a significant, independent risk factor for cardiovascular morbidity and mortality in patients with T2DM [3, 4].
However, to our knowledge, there are not enough studies analyzing the incidence of sustained impaired eGFR and its association with risk factors in Southern Europe [5,6].
We conducted a population based cohort study of Spanish people with T2DM to assess the incidence of CKD stage 3–5 (persistent decreased kidney function under 60 mL/min per 1.73 m2) over five years, to identify the risk factors associated with the development of this disease, and to construct a risk table to predict five-year CKD stage 3–5 risk stratification for clinical use.
Materials and Methods
Study Population and Design
The Madrid Diabetes Study (MADIABETES Study) is a prospective cohort study of 3,443 T2DM outpatients which has been described in detail elsewhere [7]. Briefly, the subjects were sampled from 56 primary health care centers in the metropolitan area of Madrid (Spain). Study participants were selected by simple random sampling by participating general practitioners (n = 131), using the list of patients with a T2DM diagnosis in their computerized clinical records. This method of sample selection, based on the computerized clinical records, has been previously validated for epidemiological studies in our setting [8]. The gold standard definition of T2DM used in our study comes from the diagnostic criteria developed by the American Diabetes Association and found in their Consensus Statement for diabetic subjects [9], and that was still in effect in 2007.
Data were collected by general practitioners at baseline visit (2007) and annually during the follow-up period (2008–2012). These data were recorded in electronic Case Report Forms. Last observation carried forward was used to impute missing anthropometric values for patients with incomplete data during the follow-up period.
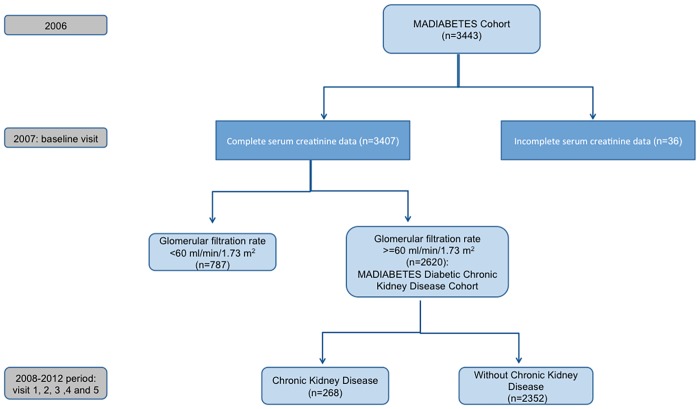
Inclusion criteria were: age ≥30 years and a previous diagnosis of T2DM. Exclusion criteria were: Type 1 Diabetes Mellitus, homebound patients, presence of CKD at baseline, defined as a baseline GFR under 60 mL/min/1.73m2 (n = 787), and incomplete serum creatinine data (n = 36). Of the 2,620 individuals followed-up until 2012, 249 died in the period 2007–2012. The flow diagram of participants is shown in Fig 1.
Fig 1. Flow diagram of participants.
After being recorded, all data were internally audited to ensure quality. This involved the random selection of 50 participating general practitioners and the review of the clinical records they produced. Strong data consistency was found (higher than 88% for all variables).
Our outcome variable was renal dysfunction incidence (CKD stage 3–5 K/DOQI) defined as estimated GFR< 60 mL/min/1.73 m2 at any visit, and an average successive estimated GFR of less than 60 mL/min/1.73 m2, among individuals free of CKD at baseline. The Modification of Diet in Renal Disease formula for estimated GFR has been shown to be an accurate indicator for CKD status [10].
To calculate incidence density the observation period for each patient was defined as the number of months from the date of their first visit in 2008 until one of the following options occurred: 1) the date CKD stage 3–5 K/DOQI was identified, 2) the date of the last visit registered, 3) date of death or, 4) 31 December 2012 (last visit).
Death data were taken from General Practitioners records. The death certificate database provided by the National Institute of Statistics was used to identify those lost to follow up due to death before the end point of the study (31 December 2012).
The median follow-up period for patients was 60 months (Interquartile range [IQR] = 24).
Clinical Examination and Biochemistry
All patients underwent anamnesis, physical examination, and biochemical tests. The following variables were collected at baseline visit: age, gender and duration of T2DM (years). Further data was collected at baseline and each follow-up visit (at least once per year in routine clinical practice conditions): fasting plasma glucose (FPG), glycated haemoglobin (HbA1c), systolic (SBP) and diastolic blood pressure (DBP), total cholesterol, triglycerides (TG), high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C), albuminuria, smoking status (current smoker, former smoker, non-smoker), use of hypoglycemic and cardiovascular medications (antihypertensive agents, statins, aspirin), body mass index (BMI), history of cardiovascular events (myocardial infarction or stroke) and hypertension.
BMI was calculated as weight/height2 (Kg/m2), and patients with a BMI >30 were considered obese. Blood Pressure (BP) was measured twice using a checked, calibrated sphygmomanometer. After a 5 minute rest period, the first reading was taken, followed by a second reading 5 minutes later. History of hypertension was defined as SBP >140 mmHg and/or DBP >90 mmHg at baseline or use of antihypertensive drugs.
Dyslipidemia was defined when any of the following lipid alterations were present: total cholesterol >250 mg/dl or triglycerides >200 mg/dl; LDL-c >130 mg/dl or HDL-c <35/45 mg/dl (male/female), and metabolic syndrome was defined according to the modified criteria of the NCEP-ATP III [11].
Persistent albuminuria was defined as a urinary albumin excretion rate >30 mg/g in at least two of three consecutive samples. HbA1c was measured using high-performance liquid chromatography (Diabetes Control and Complications Trial [DCCT]-aligned) [12].
Cardiovascular risk was calculated following the REGICOR formula (a calibration of the Framingham algorithm adapted for Spain) for each patient [13].
Patients with a cardiovascular risk of 10% over ten years were considered moderate or high risk [14].
Sample size
The sample size was estimated using the Poisson distribution and taking into account the following assumptions: 5% alpha risk, 20% beta risk and 10% loss rate. Therefore, 30 patients with albuminuria>300 mg/g and 1,800 patients with albuminuria <300 mg/g are necessary to detect a relative risk of 3.5 and a 10% of incidence of CKD in the group of not exposed patients.
Statistical Analysis
Descriptive data were expressed as mean and standard deviation and median and IQR. Comparison of continuous variables between two groups was performed using the Student’s t-test for data that were normally distributed, the Mann–Whitney U test for non-normal distributions, and the chi-square test for categorical variables.
The cumulative incidence of CKD was calculated by taking the number of new cases as the numerator, and the total initial population excluding deaths and the number of CKD cases at baseline as the denominator. Patient-years at risk of developing CKD were calculated from the baseline appointment date to either the date of death, date of CKD event, loss to follow-up or the end of the study period. Incidence density was calculated as the number of new cases divided by patient-years at risk. The cumulative incidence and incidence density of CKD were calculated for the entire sample, and stratified by duration of T2DM, and confidence intervals were compared to analyze incidence rates of differences according to duration of T2DM.
A multivariable extension of Cox proportional hazard analysis was used to estimate the adjusted hazard ratios (HR) and corresponding 95% Confidence Intervals (CI) of independently associated predictors of developing incident CKD (stage 3–5 K/DOQI). Initially, a multivariable model was constructed by applying backwards elimination to a set of candidate predictors chosen as potential risk and confounding factors according to previous studies [15,16]. The following data were analyzed: age, gender, diabetes duration, BMI, BP, albuminuria, dyslipidemia, HbA1c, use of hypoglycemic drugs (insulin, oral antidiabetic agents) and cardiovascular medications (antihypertensive agents, statins, aspirin), cardiovascular disease (hypertension, myocardial infarction [AMI], ischemic stroke, congestive heart failure, peripheral vascular disease) and diabetic microvascular complications (retinopathy, neuropathy). With the exception of age, gender, diabetes duration and history of hypertension, all predictors were included in the model as time-varying covariate, that is to say measured repeatedly across time. Only those covariates with p<0.05 were withheld in the model, except for gender, and all possible suspected interactions between independent variables were assessed. In the final model baseline SBP was also included but as a fixed variable. The proportional hazards assumptions were tested examining the covariates*time interaction. In each case, the interaction term was not significant, thus supporting the proportional hazards assumptions.
The predictive accuracy of the multivariable Cox model was evaluated using the Harrell’s C index, which is equivalent to the area under the receiver operating characteristic curve for binary dependent variables replacing time-varying covariate by average value. Results of Harrell’s C index range from 0.5 (no discrimination for predicting CKD) to 1.0 (perfect discrimination) [17]. However, the C-index must be interpreted with caution as it is not often constructed with time-dependent variables.
Finally, regression-based coefficients were used to develop a CKD predicting risk table [18]. Predictor variables were included if they were statistically significant without establishing a hierarchy between them. All possible suspected interactions between independent variables were assessed. None of these interactions yielded a significant association. A lower CKD probability (2.8%) was calculated in the absence of risk variables, and a higher one was calculated in the presence of all of them (96.7%). Between these extremes, a total of 288 combinations of CKD probabilities were obtained.
The analysis of the results with hierarchical or multilevel models was unnecessary, as there is no evidence of the variance between the primary health care centers for the HbA1c variable being different from zero (p = 0.34); in addition, the Coefficient Correlation Intraclass has a value of 0.036.
All calculations were performed using SPSS v.21.0 software for Windows and STATA v11.1SE. Significance was set at p value <0.05 for differences with a probable type I error.
Ethical aspects
The study was approved by the Institutional Review Board of the Ramón y Cajal Hospital (Madrid), and conducted in accordance with the principles of the Declaration of Helsinki. All patients signed written informed consent forms to participate in the study.
Results
Table 1 shows the socio-demographic and clinical characteristics at baseline visit of the MADIABETES CKD Cohort. Females represent 45.2% of the study population. Mean age in this patient cohort was 67.3 years (SD = 10.8) and the average T2DM duration was 8.5 years (SD = 7.4). The vast majority (91.6%) had a low risk (less or equal to 10 percent) of developing coronary events within the next ten years.
Table 1. Baseline characteristics of type 2 diabetes mellitus patients included in the cohort.
| N = 2,620 | 95% CI | |
|---|---|---|
| Female gender, (%) | 45.2 | 43.3–47.1 |
| Age (yr), mean (SD) | 67.3 (10.8) | 66.8–67.7 |
| Duration of DM (yr), mean (SD) | 8.5 (7.4) | 8.3–8.8 |
| Duration of DM (yr), median (IQR) | 6 (7) | 6.0–7.0 |
| Current smoker, (%) | 18.1 | 16.6–19.6 |
| Former smoker, (%) | 27.4 | 25.8–29.2 |
| Non-Smoker, (%) | 54.5 | 52.6–56.4 |
| Medication Profile, (%) | ||
| Oral antidiabetic | 75.2 | 73.5–76.8 |
| Insulin | 17.4 | 16–19 |
| Antihypertensive agents | 81.7 | 80.2–83.2 |
| Aspirin | 48.8 | 46.8–50.7 |
| Statins | 70.8 | 69–72.6 |
| History of, (%) | ||
| Myocardial Infarction | 11.2 | 10–11.4 |
| Stroke | 7.1 | 6.2–8.2 |
| Hypertension | 69.7 | 68–71.5 |
| Congestive heart failure | 5.6 | 4.8–6.6 |
| Neuropathy | 6.4 | 5.5–7.4 |
| Retinopathy | 7.7 | 6.8–8.8 |
| Peripheral arteriopathy | 6.2 | 5.4–7.2 |
| Risk of developing coronary events at baseline visit | ||
| Adjusted REGICOR function 10-year risk, mean (SD) | 5.9 (2.9) | 5.8–6 |
| Proportion patients with risk <5% | 52.7 | 50.6–54.7 |
| Proportion patients with risk 5–10% | 38 | 36–40 |
| Proportion patients with risk >10% | 9.4 | 8.3–10.6 |
| Anthropometric variables | ||
| BMI (Kg/m2), mean (SD) | 30 (5) | 29.8–30.2 |
| SBP (mmHg), mean (SD) | 133.5 (13.7) | 132.9–134 |
| DBP (mmHg), mean (SD) | 77.2 (8.1) | 76.9–77.6 |
| Laboratory variables | ||
| FPG (mg/dl), mean (SD) | 144.8 (41.8) | 143.1–146.4 |
| FPG (mg/dl), median (IQR) | 136 (41) | 135–138 |
| Patients with HbA1c level <7, (%) | 53.2 | 51.3–55.1 |
| HbA1c (%), mean (SD) | 7.1 (1.2) | 7–7.1 |
| HbA1c (%), median (IQR) | 6.9 (1.4) | 6.8–6.9 |
| Dyslipidemia(%) | 57.2 | 55.3–59.1 |
| Total Cholesterol (mg/dl), mean (SD) | 192.8 (35.7) | 191.5–194.2 |
| LDL-C (mg/dl), mean (SD) | 116 (29.7) | 114.9–117.2 |
| HDL-C (mg/dl), mean (SD) | 49 (12.6) | 48.6–49.5 |
| Triglycerides (mg/dl), mean (SD) | 144.3 (94) | 140.6–147.8 |
| Triglycerides (mg/dl), median (IQR) | 121 | 118–124 |
| Albuminuria 1 (%) | 20.1 | 17.4–23.1 |
1Albumin excretion rate >30 mg/g.
SD: Standard Deviation; IQR: Interquartile range; BMI: Body mass index; SBP: Systolic Blood Pressure; DBP: Dyastolic Blood Pressure; FPG: Fasting plasma glucose; HbA1c: Glycated haemoglobin; LDL-C: low-density lipoprotein cholesterol; HDL-C: high-density lipoprotein cholesterol.
Table 2 also shows the characteristics of patients that developed CKD compared with those that did not. There were statistically significant differences between CKD and non-CKD patients with respect to age, duration of T2DM, smoking status, and medication profile (aspirin, antihypertensive agents, and insulin). CKD patients had a higher prevalence of cardiovascular events (myocardial infarction, stroke, peripheral arteriopathy, and congestive heart failure), cardiovascular risk factors (hypertension), and chronic diabetic complications (retinopathy and nephropathy). However, there were no differences between the groups in the use of oral antidiabetic agents, statins, risk of developing coronary events (Score REGICOR function) and control parameters (BP, HbA1c, LDL-cholesterol, BMI). The CKD patients had a significantly higher crude mortality rate (18.3% vs. 8.5%; p<0.001).
Table 2. Comparison of characteristics according to the presence of CKD (Stage 3–5).
| Chronic Kidney Disease 1 (n = 268) | No Chronic Kidney Disease (n = 2,352) | p value * | |
|---|---|---|---|
| Female gender, (%) | 48.5 | 44.8 | 0.247 |
| Age (yr), mean (SD) | 71.8 (9.8) | 66.7 (10.8) | <0.001 |
| Duration of DM (yr), mean (SD) | 10.4 (8.2) | 8.3 (7.2) | <0.001 |
| Duration of DM (yr), median (IQR) | 8 (9) | 6 (7) | <0.001 |
| Current smoker, (%) | 11.7 | 18.8 | 0.004 |
| Former smoker, (%) | 29.7 | 27.2 | 0.384 |
| Non-Smoker, (%) | 58.6 | 54 | 0.152 |
| Medication Profile, (%) | |||
| Oral antidiabetic | 79.8 | 74.7 | 0.068 |
| Insulin | 25.2 | 16.6 | 0.001 |
| Antihypertensive agents | 95.7 | 80.1 | <0.001 |
| Aspirin | 55.8 | 48 | 0.017 |
| Statins | 74.4 | 70.4 | 0.183 |
| History of, (%) | |||
| Myocardial Infarction | 18.7 | 10.3 | <0.001 |
| Stroke | 11.6 | 6.6 | 0.003 |
| Hipertensión | 85.4 | 68 | <0.001 |
| Congestive heart failure | 9.7 | 5.2 | 0.02 |
| Neuropathy | 7.5 | 6.2 | 0.44 |
| Retinopathy | 12.7 | 7.2 | 0.001 |
| Peripheral arteriopathy | 11.2 | 5.7 | <0.001 |
| Risk of developing coronary events | |||
| Adjusted REGICOR function 10-year risk, mean (SD) | 6 (3.4) | 5.9 (2.9) | 0.504 |
| Proportion patients with risk <5% | 53 | 52.6 | 0.905 |
| Proportion patients with risk 5–10% | 35.1 | 38.3 | 0.323 |
| Proportion patients with risk >10% | 12 | 9.1 | 0.137 |
| Anthropometric variables | |||
| BMI (Kg/m2), mean (SD) | 30.3 (5.3) | 30 (4.9) | 0.381 |
| SBP (mmHg), mean (SD) | 136.7 (13) | 133.1 (13.7) | 0.288 |
| DBP (mmHg), mean (SD) | 76.7 (7.4) | 77.3 (8.1) | 0.983 |
| Laboratory variables | |||
| FPG (mg/dl), mean (SD) | 142.5 (45.9) | 145 (41.3) | 0.381 |
| FPG (mg/dl), median (IQR) | 134 (47) | 136 (42) | 0.288 |
| Patients with HbA1c level <7, (%) | 52.3 | 53.3 | 0.751 |
| HbA1c (%), mean (SD) | 7.1 (1.2) | 7.1 (1.8) | 0.868 |
| HbA1c (%), median (IQR) | 6.9 (1.1) | 6.9 (1.4) | 0.954 |
| Dyslipidemia, (%) | 54.5 | 57.5 | 0.336 |
| Total Cholesterol (mg/dl), mean (SD) | 191.8 (36.9) | 193 (35.5) | 0.616 |
| LDL-C (mg/dl), mean (SD) | 113.3 (28.8) | 116.4 (29.7) | 0.12 |
| HDL-C (mg/dl), mean (SD) | 49.4 (13) | 49 (12.5) | 0.619 |
| Triglycerides (mg/dl), mean (SD) | 151.8 (100.5) | 143.4 (93.2) | 0.178 |
| Triglycerides (mg/dl), median (IQR) | 126 (79) | 120 (77) | 0.07 |
| Albuminuria2, (%) | 36 | 18 | <0.001 |
| Microalbuminuria (%) | 30.3 | 17 | 0.002 |
| Macroalbuminuria (%) | 5.7 | 1 | 0.001 |
| Crude All-Cause Mortality at 5 years (%) | 18.3 | 8.5 | <0.001 |
1. Stage 3–5 of K/DOQI
2. Albumin excretion rate > 30 mg/g
SD: Standard Deviation; IQR: Interquartile range; BMI: Body mass index; SBP: Systolic Blood Pressure; DBP: Dyastolic Blood Pressure; FPG: Fasting plasma glucose; HbA1c: Glycated haemoglobin; LDL-C: low-density lipoprotein cholesterol; HDL-C: high-density lipoprotein cholesterol.
* Pearson’s chi-square method was applied for categorical variables, and Student’s t-test for continuous variables. Mann-Whitney U-test was applied to compare medians of duration of DM2.
The cumulative incidence of CKD at five-years was 10.23% (95% CI = 9.12–11.43) and the incidence density was 2.07 (95% CI = 1.83–2.33) cases per 1,000 patient-months or 2.48 (95% CI = 2.19–2.79) cases per 100 patient-years. Among patients living T2DM for <10 years, the cumulative incidence of CKD was 8.48% (95% CI = 7.29–9.84) vs. 14.25% (95% CI = 11.99–16.86) in patients with T2DM for ≥ 10 years. Incidence density was 2.03 cases per 100 patient-years (95% CI = 1.73–2.38) among T2DM <10 years and 3.54 (95% CI = 2.92–4.25) among patients living with T2DM for longer. The cumulative incidence rates stratified by duration of T2DM can be considered significantly different because their 95% CI do not overlap. This was equally the case for incidence density rates.
The adjusted Hazard Ratios (HR) of risk factors associated with incidence of CKD are shown in Table 3. The highest HR was albuminuria ≥ 300 mg/g (HR = 4.57; 95% CI = 2.46–8.48). Furthermore, the other variables with high HR were age over 74 years (HR = 3.20; 95% CI = 2.13–4.81), history of Hypertension (HR = 2.02; 95% CI = 1.42–2.89), Myocardial Infarction (HR = 1.72; 95% CI = 1.25–2.37), dyslipidemia (HR = 1.68; 95% CI = 1.30–2.17), SBP >149 mmHg (HR = 1.52; 95% CI = 1.02–2.24) and duration of T2DM ≥ 10 years (HR = 1.46; 95% CI = 1.14–1.88). Moreover, an exploratory analysis of the metabolic syndrome data showed a non-significant association with incidence of CKD (HR = 1.08, 95% CI = 0.8–1.5; p = 0.617).
Table 3. Associated Risk Factors for Incident CKD (Stage 3–5) (n = 268) after five-year follow-up of 2,620 patients (Multivariable Cox Regression).
| Variables | aHR | HR 95% CI | p value |
|---|---|---|---|
| Age | |||
| <60 years | 1 | ||
| 60–74 years | 1.86 | 1.25–2.77 | 0.002 |
| >74 | 3.20 | 2.13–4.81 | <0.001 |
| Albuminuria | |||
| < 30 mg/g | 1 | ||
| 30–299 mg/g | 1.67 | 1.11–2.50 | 0.013 |
| ≥ 300 mg/g | 4.57 | 2.46–8.48 | <0.001 |
| Gender | |||
| Male | 1 | ||
| Female | 1.15 | 0.89–1.49 | 0.283 |
| History of prior Hypertension | |||
| No | 1 | ||
| Yes | 2.02 | 1.42–2.89 | <0.001 |
| Duration of Diabetes Mellitus | |||
| <10 years | 1 | ||
| ≥10 years | 1.46 | 1.14–1.88 | 0.003 |
| Myocardial infarction | |||
| No | 1 | ||
| Yes | 1.72 | 1.25–2.37 | 0.001 |
| Dyslipidemia | |||
| No | 1 | ||
| Yes | 1.68 | 1.30–2.17 | <0.001 |
| SBP | |||
| <130 mmHg | 1 | ||
| 130–149 mmHg | 1.22 | 0.91–1.64 | 0.184 |
| >149 mmHg | 1.52 | 1.02–2.24 | 0.037 |
aHR: Adjusted Hazard Ratio; CI: Confidence Interval; CKD: Chronic Kidney Disease; SBP: Systolic Blood Pressure.
Finally, the development of a probability table of CKD risk can be seen in Table 4. The greatest risk is observed in patients over 75 years, with T2DM duration ≥10 years, with hypertension, albuminuria ≥ 300 mg/g, SBP ≥150 mmHg, dyslipidemia and AMI.
Table 4. Risk Table: Probability of developing sustained impaired Glomerular Filtration Rate (Stage 3–5 K/DOQI), in five years.
| AMI | DISLYPEMIA | BPS | <75 YEARS | ≥75 YEARS | ||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| DURATION OF DIABETES MELLITUS < 10 YEARS | DURATION OF DIABETES MELLITUS ≥10 YEARS | DURATION OF DIABETES MELLITUS < 10 YEARS | DURATION OF DIABETES MELLITUS ≥10 YEARS | |||||||||||||||||||||||
| HYPERTENSION | HYPERTENSION | HYPERTENSION | HYPERTENSION | |||||||||||||||||||||||
| NO | YES | NO | YES | NO | YES | NO | YES | |||||||||||||||||||
| ALBUMINURIA | ALBUMINURIA | ALBUMINURIA | ALBUMINURIA | ALBUMINURIA | ALBUMINURIA | ALBUMINURIA | ALBUMINURIA | |||||||||||||||||||
| NO | 30–299 | ≥300 | NO | 30–299 | ≥300 | NO | 30–299 | ≥300 | NO | 30–299 | ≥300 | NO | 30–299 | ≥300 | NO | 30–299 | ≥300 | NO | 30–299 | ≥300 | NO | 30–299 | > = 300 | |||
| NO | NO | < 130 | 2.8 | 4.4 | 11.3 | 5.9 | 9.3 | 22.8 | 4.2 | 6.7 | 16.9 | 8.9 | 13.9 | 32.8 | 5.6 | 8.8 | 21.6 | 11.6 | 17.9 | 40.7 | 8.4 | 13.2 | 31.2 | 17.2 | 26.2 | 55.2 |
| 130–149 | 3.5 | 5.6 | 14.2 | 7.4 | 11.7 | 28.0 | 5.4 | 8.5 | 20.9 | 11.2 | 17.4 | 39.6 | 7.0 | 11.0 | 26.6 | 14.5 | 22.2 | 48.6 | 10.6 | 16.4 | 37.8 | 21.3 | 32.0 | 64.0 | ||
| > = 150 | 4.3 | 6.8 | 17.1 | 9.0 | 14.1 | 33.1 | 6.5 | 10.3 | 25.0 | 13.5 | 20.8 | 46.1 | 8.5 | 13.3 | 31.5 | 17.4 | 26.5 | 55.7 | 12.8 | 19.8 | 44.1 | 25.5 | 37.7 | 71.4 | ||
| YES | < 130 | 4.4 | 7.0 | 17.4 | 9.2 | 14.4 | 33.7 | 6.7 | 10.5 | 25.5 | 13.8 | 21.2 | 46.8 | 8.7 | 13.6 | 32.1 | 17.8 | 27.0 | 56.5 | 13.0 | 20.1 | 44.8 | 26.0 | 38.3 | 72.2 | |
| 130–149 | 5.6 | 8.8 | 21.6 | 11.6 | 17.9 | 40.7 | 8.4 | 13.2 | 31.2 | 17.2 | 26.2 | 55.2 | 10.9 | 17.0 | 38.9 | 22.0 | 33.0 | 65.3 | 16.3 | 24.9 | 53.1 | 31.8 | 45.9 | 80.3 | ||
| > = 150 | 6.8 | 10.6 | 25.8 | 14.0 | 21.5 | 47.3 | 10.2 | 15.9 | 36.7 | 20.6 | 31.1 | 62.6 | 13.2 | 20.4 | 45.3 | 26.3 | 38.7 | 72.7 | 19.6 | 29.6 | 60.4 | 37.4 | 52.9 | 86.4 | ||
| YES | NO | < 130 | 4.7 | 7.4 | 18.5 | 9.8 | 15.3 | 35.6 | 7.1 | 11.2 | 27.0 | 14.7 | 22.6 | 49.2 | 9.3 | 14.5 | 33.9 | 18.9 | 28.6 | 59.0 | 13.9 | 21.4 | 47.1 | 27.5 | 40.4 | 74.6 |
| 130–149 | 5.9 | 9.4 | 22.9 | 12.3 | 19.1 | 42.9 | 9.0 | 14.0 | 33.0 | 18.3 | 27.8 | 57.7 | 11.7 | 18.1 | 41.0 | 23.4 | 34.8 | 67.8 | 17.3 | 26.4 | 55.5 | 33.6 | 48.2 | 82.5 | ||
| > = 150 | 7.2 | 11.4 | 27.3 | 14.9 | 22.8 | 49.6 | 10.9 | 16.9 | 38.7 | 21.9 | 32.9 | 65.1 | 14.1 | 21.7 | 47.6 | 27.8 | 40.8 | 75.1 | 20.8 | 31.3 | 62.9 | 39.4 | 55.4 | 88.2 | ||
| YES | < 130 | 7.4 | 11.6 | 27.8 | 15.2 | 23.3 | 50.4 | 11.1 | 17.3 | 39.4 | 22.4 | 33.4 | 65.9 | 14.4 | 22.1 | 48.3 | 28.4 | 41.5 | 75.8 | 21.2 | 31.9 | 63.7 | 40.1 | 56.2 | 88.7 | |
| 130–149 | 9.3 | 14.5 | 33.9 | 18.9 | 28.6 | 59.0 | 13.9 | 21.4 | 47.1 | 27.5 | 40.4 | 74.6 | 17.9 | 27.2 | 56.8 | 34.6 | 49.4 | 83.5 | 26.1 | 38.6 | 72.5 | 47.9 | 64.9 | 93.7 | ||
| > = 150 | 11.2 | 17.5 | 39.8 | 22.6 | 33.8 | 66.4 | 16.8 | 25.5 | 54.2 | 32.6 | 47.0 | 81.3 | 21.5 | 32.2 | 64.2 | 40.5 | 56.6 | 89.0 | 31.0 | 45.0 | 79.4 | 55.0 | 72.3 | 96.7 | ||
AMI: Acute Myocardial Infarction
SBP: Systolic Blood Pressure
Bold type indicated the minimum and maximum values.
The Harrell’s C-index value for the CKD model was 70.3 (95% CI = 66.5–73.9), this implies a good prediction ability to discriminate between patients with and without CKD.
Discussion
Incidence of CKD
Our CKD (stage 3–5) incidence density is high (2.48 cases per 100 patient-years) compared to other studies among T2DM patients that reported a lower incidence density, between 0.133 to 0.200 cases per 100 patient-years [19,20]. These differences may be explained, in part, as these studies use data from the 1990s when the prevalence of impaired renal function in diabetic patients was lower than today [21]. The higher current prevalence of reduced GFR is because the age of onset of type 2 diabetes is decreasing, allowing patients enough duration of diabetes to develop microvascular complications. Furthermore, survival of diabetic patients with overt diabetic nephropathy has been improved therefore increasing the prevalence [22]. Also, recently, de Boer et al. has shown incidence densities between 0.16 per 100 patient-years in subjects from the DCCT/EDIC study assigned to intensive therapy and 0.3 per 100 patient-years in those assigned to conventional therapy [23].
The cumulative incidence rate at 5 years was 10.23% (2.04% / year) in our study. This rate is concordant with rates found in previously published literature among patients with T2DM. For example, in a Swedish observational population-based study, Afghahi et al. found that 11% (2.2% / year) of 3,667 T2DM patients developed renal impairment [24]. Also, a recent analysis of 1,449 patients with T2DM performed within the framework of the Verona Diabetes Study [25] reported a 13.4% incidence of developed CKD during a mean follow-up of 5 years. In the UKPDS-74, 29% developed renal impairment (1.93%/year) after a median follow-up of 15 years [26].
Patients with long duration of T2DM showed higher cumulative incidence and incidence density of CKD than patients who were recently diagnosed. These findings are in agreement with published studies [5], showing that patients diagnosed with T2DM for more than 15 years show an annual decline of eGFR of -1.0 mL/min per 1.73 m2 per year and a -1.4 annual eGFR decline (% per year) compared to -0.7 mL/min per 1.73 m2 per year and -0.8 annual eGFR decline (% per year) in more recently diagnosed patients. However, other studies did not find an association between duration of T2DM and eGFR decline [27].
Risk Factors
In the present Cohort, the main variables associated with incidence of CKD stage 3–5 were albuminuria ≥ 300 mg/g and age >74 years. Several predictive models of kidney failure have included age and history of albuminuria, both in the general population and in T2DM patients [24,26–28]. However, Tangri et al. [16] identified age as a protective factor for developing kidney failure, defined as the need for dialysis or kidney transplantation. In this study the HR was 0.61 (p<0.05) for each increase of 5 mL/min/1.73m2. This finding is not consistent with the vast majority of studies, and is probably due to the fact that dialysis and transplantation are primarily offered to younger patients.
Albuminuria (microalbuminuria and macroalbuminuria) is a well-established risk factor for deterioration of renal function. Observational studies have shown a relationship between increasing albuminuria and declining GFR. In T2DM patients, a relative risk of 3.6 (95% CI = 1.6–8.4) has been identified [28]. In addition, a greater decline in GFR has been seen in patients with microalbuminuria (1.7 ml per minute per year) compared with those that have normoalbuminuria [28].
Similarly to previous studies, our data show a comparable risk value of albuminuria ≥ 300 mg/g for developing CKD (HR = 4.57; 95% CI = 2.46–8.48). On the other hand, dissociation between albumin excretion rate and GFR has been reported in T2DM patients [29,30].
As is documented in the specialist literature [31], albuminuria > 300 mg/g is a well established risk factor for CKD incidence and this is reflected in our data. Thus, we strongly advise health care providers to increase their efforts to prevent and/or reverse albuminuria in their patients. In this line, a pooled analysis of interventional studies has demonstrated that the initial percentage decrease in albumin excretion rate was 20.8% in T2DM with late diabetic nephropathy (macroalbuminuria) and the corresponding annual percentage rate of decline in GFR was 9.2% [32].
Additionally, two studies demonstrated that some patients with DM develop a low creatinine clearance while remaining normoalbuminuric [33,34]. Similarly, in the UKPDS-74 Study the majority (51%) of patients who developed CKD stage 3–5 did not have preceding microalbuminuria [26].
Hypertension is both a cause and effect of renal impairment. A meta-analysis of several large intervention studies has shown that a lower mean BP during therapy is associated with slower rates of decline of GFR [35]. One standard deviation increase in 24h ambulatory SBP increases the risk of end- stage renal disease by 3.04 (95% CI = 2.13–4.35) and by 2.20 (95% CI = 1.43–2.39) when it is adjusted for standard clinic SBP [36]. Also, BP control has been shown to reduce the incidence of albuminuria and for each decrement of 10 mmHg of SBP the incidence of CKD is reduced by approximately 10% [37]. Numerous studies have reported an increased risk of CKD in hypertensive patients [24,38–40] with the HR ranging from 1.4 to 3.0. Our study showed that having SBP in the upper range (>149 mmHg) was associated with an approximately 50% higher CKD incidence (HR = 1.52; 95% CI = 1.02–2.24; p = 0.037). Herget-Rosenthal et al. [41] found hypertension to be a risk factor (HR 4.83; CI 95% = 1.18–19.35) to developing eGFR decline >7.5 mL/min/1.73 m2 in high risk primary care patients after three years follow-up. However, other studies did not find a relationship between SBP and incidences of CKD 3–5 after adjustment for age [42].
Dyslipidemia has exhibited inconsistent association with CKD stage 3–5 incidence in the general population and diabetic cohorts. While a large body of evidence suggests that dyslipidemia has an important role in the progression of kidney disease in patients with diabetes [43], other studies have shown that high triglycerides [44] and low HDL cholesterol, but not LDL cholesterol, predict an increased risk of renal dysfunction [45] and decline of GFR [46]. In fact, the largest study evaluating this question included 2,193 patients with T2DM and normal renal function at baseline. In this study, each 0.26 mmol/L higher level of HDL was associated with a 24% lower risk of developing stage 3 CKD [47]. In our cohort, dyslipidemia increased the risk of CKD by 68% (HR = 1.68; CI 95% = 1.30–2.17; p<0.001). However, the UKPDS 74 study did not find this association [26].
Female gender is usually significantly associated with a decline of GFR [24,26,40]. However, other studies have found a higher association with male gender [42]. We found a non-significant association between female gender and Stage 3–5 CKD incidence (HR = 1.15; CI 95% = 0.89–1.49; p = 0.283).
Coronary Heart Disease has been shown to be a risk factor to developing CKD [48]. The time course of renal function after Myocardial Infarction, adjusted for baseline GFR, has been well defined: a loss of renal function of 2–3 ml min−1 year−1 in the first days after an acute MI, with a subsequent steady decline of approximately 3 ml min−1 year−1 in excess of the normal age-related rate of renal function loss [49]. However, several studies have not found this association [16,24,40–42,50,51]. In the present study, myocardial infarction showed a HR of 1.72 (95% CI = 1.25–2.37; p<0.001).
The association between CKD and Acute Myocardial Infarction incidence is well established with HRs ranging from 1.4 (GFR 45–59 mL/ min/ 1.73 m2) to 3.4 (GFR <15 mL/ min/ 1.73 m2) [52].
The effect of CKD (stage 3–5) on mortality rate at 5 years (18.3% vs. 8.5%; p<0.001) is consistent with previous reports [53–56] that show a more than 2-fold increase in mortality rate in patients with reduced GFR compared to patients with normal GFR.
Although a recent meta-analysis [57] showed that Metabolic Syndrome was associated with development of an eGFR <60 mL/ min/ 1.73 m2, with OR = 1.55 (95%CI = 1.34–1.80), our study did not find such an association. Thus, metabolic syndrome was not included in our model and we instead decided to include the history of hypertension and dyslipidemia.
Finally, other factors such as the Mediterranean diet may be considered a factor in the development of CKD incidence in patients with T2DM. For example, Dunkler et al. [58] show, using the modified Alternate Healthy Eating Index (mAHEI) tool, that compared to participants in the least healthy mAHEI score tertile, participants in the healthiest tertile had a lower risk of CKD (OR = 0.74; 95% CI = 0.64–0.84) and a lower risk of mortality (OR = 0.61; 95% CI = 0.48–0.78). Also, participants consuming more than 3 servings of fruit per week had a lower risk of CKD compared with participants consuming these food items less frequently. In this sense it is possible that the Mediterranean diet had a similar effect. However, different studies in Mediterranean populations have not shown lower incidence rates of CKD compared to non-Mediterranean populations [59]. In our study, we did not collect data on food consumption, so we cannot analyze the effect of diet.
Risk Table
To our knowledge, this is the first study that has developed a simple risk table to predict five-year CKD risk in patients with T2DM. Taking a high-risk person as an example: age over 75 years old, hypertension, myocardial infarction, albuminuria ≥ 300 mg/g, dyslipidemia, duration of T2DM ≥ ten years, and SBP ≥150 mmHg; the risk of developing CKD at five-year follow-up is 96.7%. However, in the same patient, without albuminuria the risk is reduced to 55%, and without albuminuria and SBP <130 mmHg the risk is further reduced to 40.1%. Thus, after changing SBP and albuminuria values the risk decreases from 96.7% to 40.1% (56.6 percentage points less).
This risk table enables the calculation of individual risk estimates and can help in the development of risk reduction strategies by highlighting certain parameters such as SBP, or albuminuria regression, that need controlling. Therefore, it is particularly useful for general practitioners caring for patients with T2DM in our setting, as it allows the monitoring of risk over time and could be used by general physician at primary health care centers to identify high risk patients and improve prevention of CKD.
Strengths and Limitations
There are several potential implications of this paper. Selection bias is an important limitation to this study and may affect the external validity of our results. The study sample was not population based as it was drawn from outpatients visiting Primary Health Care Centers. Patients who attend private clinics, who may have a higher socioeconomic status, are possibly under-represented in our sample. Furthermore, the study was conducted in Madrid, a large city in Spain, which may not represent the entire Spanish population in terms of income, educational level, lifestyle, and health profile.
The MADIABETES cohort is well described, made up of people living with T2DM and analyzed under usual clinical practice conditions. As expected, some patients had incomplete serum creatinine data at baseline (n = 36; 1%) or follow-up (n = 49; 1.4%). Owing to this feature of the study, patients were observed until last contact with general practitioner or until death; a total of 249 subjects died during follow-up. This must be considered when generalizing the study findings.
Finally, it is important to consider that some confounding variables, such as compliance with medical treatments, may not have been collected in this study and we cannot completely rule out the possibility of residual confounding. Also, it is necessary to validate the multivariate model in a simple over a longer time frame in order to improve accuracy and reliability.
Importantly, general practitioners can improve the quality of care delivered to their T2DM patients by being able to calculate risk probabilities. This will enable them to provide better clinical counseling and improve decision-making. Strengths of this study include the prospective design, which ensured that measurement of risk factors preceded the development of impaired eGFR. In addition, the requirement of sustained impaired eGFR (one event of eGFR <60 mL/ min/ 1.73 m2 and average of successive eGFR less 60 mL/ min/ 1.73 m2) when defining outcomes helped improve the specificity, because a decrease in eGFR may represent transient changes in kidney perfusion or function that are not necessarily related to the casual pathway that is driving the development of diabetic kidney disease.
Conclusions
After a five-year follow-up, the cumulative incidence of CKD is concordant with rates previously published in the literature. Age over 74 years and albuminuria ≥ 300 mg/g were the risk factors more strongly associated with incidence of CKD stage 3–5. Our results suggest that a greater control of BP, lipid and albuminuria could reduce the incidence of CKD in patients with T2DM. Further studies are necessary to confirm the role of these variables as risk factors and elucidate their causal relationship on CKD.
Acknowledgments
The members of the MADIABETES Group are: JC Abánades-Herranz; AM Alayeto-Sánchez; A Alonso-Menéndez; B Álvarez-Embarba; E Álvarez-Navarro; AM Arias-Salgado-Robsy; A Arnaiz-Kompanietz; M Arnalte-Barrera; FJ Arrieta-Blanco; G Artiach-Geiser; S Artola-Menéndez; E Barrios-Martos; L Barutell-Rubio; D Beamud-Victoria; MJ Bedoya-Frutos; C Bello-González; A Benítez-Arroyo; F Blanco-Urzaiz; M Caballero-Sánchez; ME Calonge-García; R Calvo-Arregui; E Calvo-García; M Camarero-Shelly; M Canals-Aracil; A Cano-Espín; PP Carreño-Freire; E Carrillo-De Santa Pau; S Casado-González; P Casado-Pérez; C Casella-Barban; S Castellanos-Redondo; MJ Castillo-Lizarraga; J Castro-Martín; MA Cava-Rosado; I Cerrada-Somolinos; C Chamorro-Escobar; R de Felipe-Medina; MC de Hoyos-Alonso; G de la Fuente-de la Fuente; S de la Iglesia-Moreno; O de la Peña-Gutierrez; B de Llama-Arauz; A de Miguel-Ballano; ML De Santiago-De Hernando; L De Vicente-Aymat; M de Vicente-Martínez; MA Díaz-Crespo; M Domínguez-Paniagua; EM Donaire-Jimenez; F Endrino-Gómez; J Escobar-Moreno; R Fernández-Fernández; MI Fernández-Ferrero; J Fernández-García; MR Fernández-García; MR Ferreras-Eleta; E Fonseca-Capdevilla; P Gallego-Gómez; MA García-Alonso; S García-Carmona; MC García-Cubero; F García-García; MI García-García; JN García-Pascual; B García-Serrano;E García-Virosta; P Gil-Díaz; M Gil-Díaz; MJ Gomara-Martínez; MS Gómez-Criado; E Gomez-Navarro; C González-Benito; C González-Fernández; MI González-García; A González-González; E González-Romero; C Gonzalo-Hernández; I Herreros-Hernanz; P Huelin-Martín; R Iglesias-González; MJ Iglesias-Iglesias; J Innerarity-Martínez; Á Jaime-Siso; A Jiménez-Moreno; BE León-Morales; E López-Burillo; MC López-Gutiérrez; I López-Noguero; E López-Parra; C López-Rodríguez; MB López-Sabater; L López-Sediles; A Maestro-Martín; MJ Mansilla-Bermejo; M Martín-Bun; P Martín-Calvo; MR Martín-Cano; M Martínez-García; J Martínez-Irazusta; C Martín-Madrazo; F Mata-Benjumea; AI Menéndez-Fernández; S Merino-Martin; T Mesonero-Grandes; M Miguel-Garzón; C Montejo-Martínez; MC Montero-García; C Montero-Lizana; A Montilla-Bernabé; A Moran-Escudero; A Muñoz-Cildoz; S Muñoz-Quiros-Aliaga; MA Murchante; E Muro-Díaz; P Nogales-Aguado; S Núñez-Palomo; O Olmos-Carrasco; MC Ortega-Huerta; I Parra-Álvarez; ME Pejenaute-Labari; MA Pellus-Pardines; E Peña-Rodríguez; I Peña-Sainz; C Pérez-de la Campa; FC Pérez-Sánchez; N Pertierra-Galindo; A Pinilla-Carrasco; M Piñera-Tamés; A Pozo-Teruel; MP Puebla-Sanz; S Pulido-Fernández; AB Ramírez-Puerta; G Reviriego-Jaén; C Revuelto-García; C Reyes-Madridejos; P Ríus-Fortea; G Rodríguez-Castro; C Rodríguez-Gallego; MA Rodríguez-Posada; J Roldan-San Juan; MT Rollán-Landeras; A Rosillo-González; C Ruiz-Tuñón; J Sagredo-Pérez; MT Salamanca-Sánchez-Escalonilla; JM San Vicente-Rodríguez; R Santana-Alonso; MT Sanz-de la Fuente; MM Sanz-Pascual; R Sartre-De la Fuente; L Serrano-González; R Serrano-Martín; AM Serrano-Ortíz; ME Serrano-Serrano; P Serrano-Simarro; D Serrano-Tomat; A Siguero-Anguí; AM Sobrado-de Vicente-Tutor; S Soto-Díaz; M Suárez-Baraza; J Suero-Palancar; T Torices-Rasines; P Tovar-García; E Tutor-Pellicer-Palacín; MA Usero-Martín; E Vaquero-Lucas; I Vázquez-Burgos; B Vázquez-Rodríguez; MP Vich-Pérez; R Yehuda-Salama; MM Zamora-Gómez; MP Zazo-Lázaro; C Zúñiga-Bartolomé.
Data Availability
All relevant data are within the paper.
Funding Statement
This work was supported by a grant from the 2008-2011 National R+D+I (Research + Development + Innovation) Plan of the Spanish Ministry of Science and Innovation via the Instituto de Salud Carlos III (PI10/02796 and PI12/01806). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Parving HH, Mauer M, Ritz E. Diabetic nephropaty In: Brenner BM, editor. Brenner and Rector`s The Kidney. 7th ed. Philadelphia: WB Saunders; 2004. p. 1777–818. [Google Scholar]
- 2. National Kidney Foundation. K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis 2002;39(2 Suppl 1):S1–266. [PubMed] [Google Scholar]
- 3. Drury PL, Ting R, Zannino D, Ehnholm C, Flack J, et al. Estimated glomerular rate and albuminuria are independent predictors of cardiovascular events and death in type 2 diabetes mellitus: the Fenofibrate Intervention and Event Lowering in Diabetes (FIELD) study. Diabetologia 2011;54(1):32–43. 10.1007/s00125-010-1854-1 [DOI] [PubMed] [Google Scholar]
- 4. So WY, Kong AP, Ma RC, Ozaki R, Szeto CC, Chan NN, et al. Glomerular filtration rate, cardiorenal end points, and all-cause mortality in type 2 diabetic patients. Diabetes Care 2006;29(9):2046–52. [DOI] [PubMed] [Google Scholar]
- 5. Zoppini G, Tahger G, Chonchol M, Ortalda V, Negri C, Stoico V, et al. Predictors of estimated GFR decline in patients with type 2 diabetes and preserved kidney function. Clin J Am Soc Nephrol 2012;7(3):401–8. 10.2215/CJN.07650711 [DOI] [PubMed] [Google Scholar]
- 6. ESRD Incidence Study Group, Stewart JH, McCredie MR, Williams SM. Divergent trends in the incidence of end-stage renal disease due to Type 1 and Type 2 diabetes in Europe, Canada and Australia during 1998–2002. Diabet Med 2006; 23(12):1364–69. [DOI] [PubMed] [Google Scholar]
- 7. Salinero-Fort MÁ, San Andrés-Rebollo FJ, de Burgos-Lunar C, Arrieta-Blanco FJ, Gómez-Campelo P, MADIABETES Group. Four-year incidence of diabetic retinopathy in a Spanish cohort: the MADIABETES study. Plos One 2013;8(10):e76417 10.1371/journal.pone.0076417 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. De Burgos-Lunar C, Salinero-Fort MA, Cárdenas-Valladolid J, Soto-Díaz S, Fuentes-Rodriguez CY, Abánades-Herranz JC, et al. Validation of diabetes mellitus and hypertension diagnosis in computerized medical records in primary health care. BMC Med Res Methodol 2011;11:146 10.1186/1471-2288-11-146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Arauz-Pacheco C, Parrott MA, Raskin P, American Diabetes Association. Treatment of hypertension in adults with diabetes. Diabetes Care 2003;26 Suppl 1:S80–S82. [DOI] [PubMed] [Google Scholar]
- 10. Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D. A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Modification of Diet in Renal Disease Study Group. Ann Intern Med 1999;130(6):461–70. [DOI] [PubMed] [Google Scholar]
- 11. Wassink AM, van der Graaf Y, Olijhoek JK, Visseren FL, SMART Study Group. Metabolic syndrome and the risk of new vascular events and all-cause mortality in patients with coronary artery disease, cerebrovascular disease, peripheral arterial disease or abdominal aortic aneurysm. Eur Heart J 2008;29(2):213–23. 10.1093/eurheartj/ehm582 [DOI] [PubMed] [Google Scholar]
- 12. Selvin E, Coresh J, Zhu H, Folsom A, Steffes MW. Measurement of HbA1c from stored whole blood samples in the Atherosclerosis Risk in Communities study. J Diabetes 2010;2(2):118–24. 10.1111/j.1753-0407.2010.00070.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Marrugat J, Solanas P, D’Agostino R, Sullivan L, Ordovas J, Cordón F, et al. Coronary risk estimation in Spain using a calibrated Framingham function. Rev Esp Cardiol 2003;56(3):253–61. [DOI] [PubMed] [Google Scholar]
- 14. Bosomworth NJ. Practical use of Framingham risk score in primary prevention: Canadian perspective. Can Fam Physician 2011;57(4):417–23. [PMC free article] [PubMed] [Google Scholar]
- 15. Kshirsagar AV, Bang H, Bomback AS, Vupputuri S, Shoham DA, Kem LM, et al. A simple algorithm to predict incident kidney disease. Arch Intern Med 2008;168(22):2466–73. 10.1001/archinte.168.22.2466 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Tangri N, Stevens LA, Griffith J, Tighiouart H, Djurdjev O, Naimark D, et al. A predictive model for progression of chronic kidney disease to kidney failure. JAMA 2011;305(15):1553–9. 10.1001/jama.2011.451 [DOI] [PubMed] [Google Scholar]
- 17. Harrel FE, Lee KL, Mark DB. Multivariable prognostic models: issues in developing models, evaluating assumptions and adequacy, and measuring and reducing errors. Stat Med 1996;15(4):361–87. [DOI] [PubMed] [Google Scholar]
- 18.Domenech JM, Navarro JB. Análisis de la supervivencia y modelo de riesgos proporcionales de Cox. Barcelona:Signo;2008.
- 19. Humphrey LL, Ballard DJ, Frohnert PP, Chu CP, O’Fallon WM, Palumbo PJ. Chronic renal failure in non-insulin-dependent diabetes mellitus. A population-based study in Rochester, Minnesota. Ann Intern Med 1989;111(10):788–96. [DOI] [PubMed] [Google Scholar]
- 20. Brancati FL, Whelton PK, Randall BL, Neaton JD, Stamier J, Klag MJ. Risk of end-stage renal disease in diabetes mellitus: a prospective cohort study of men screened for MRFIT. Multiple Risk Factor Intervention Trial. JAMA 1997;278(23):2069–74. [PubMed] [Google Scholar]
- 21. De Boer IH, Rue TC, Hall YN, Heagerty PJ, Weiss NS, Himmelfarb J. Temporal trends in the prevalence of diabetic kidney disease in the United States. JAMA 2011;305(24):2532–39. 10.1001/jama.2011.861 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Rossing P. Diabetic nephropathy: worldwide epidemic and effects of current treatment and natural history. Curr Diab Rep 2006;6(6):479–83. [DOI] [PubMed] [Google Scholar]
- 23. DCCT/EDIC Research Group, de Boer IH, Sun W, Cleary PA, Lachin JM, Molitch M, et al. Intensive diabetes therapy and glomerular filtration rate in type 1 diabetes. N Engl J Med 2011;365(25):2366–76. 10.1056/NEJMoa1111732 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Afghari H, Cederholm J, Eliasson B, Zethelius B, Gudbjömsdottir S, Hadimeri H, et al. Risk factors for the development of albuminria and renal impairment in type 2 diabetes-the Swedish National Diabetes Register (NDR). Nephrol Dial Transplant 2011;26(4):1236–43. 10.1093/ndt/gfq535 [DOI] [PubMed] [Google Scholar]
- 25. Zoppini G, Targher G, Choncol M, Ortalda V, Abaterusso C, Pichiri I, et al. Serum uric acid levels and incident chronic kidney disease in patients with type 2 diabetes and preserved kidney function. Diabetes Care 2012;35(1):99–104. 10.2337/dc11-1346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Retnakaran R, Cull CA, Thorne KI, Adler AI, Holman RR, UKPDS Study Group. Risk factors for renal dysfunction in type 2 diabetes: U.K. Prospective Diabetes Study 74. Diabetes 2006;55(6):1832–39. [DOI] [PubMed] [Google Scholar]
- 27. Gunzler D, Bleyer AJ, Thomas RL, O’Brien A, Russel GB, Sattar A, et al. Diabetic nephropathy in a sibling and albuminuria predict early GFR decline: a prospective cohort study. BMC Nephrol 2013;14:124 10.1186/1471-2369-14-124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Newman DJ, Mattock MB, Dawnay AB, Kerry S, McGuire A, Yaqoob M, et al. Systematic review on urine albumin testing for early detection of diabetic complications. Health Technol Asses 2005;9(30):iii–vi,xiii–163. [DOI] [PubMed] [Google Scholar]
- 29. Kramer HJ, Nguyen QD, Curhan G, Hsu CY. Renal insufficiency in the absence of albuminuria and retinopathy among adults with type 2 diabetes mellitus. JAMA 2003;289(24):3273–7. [DOI] [PubMed] [Google Scholar]
- 30. Maclsaac RJ, Tsalamandris C, Panagiotopoulos S, Smith TJ, McNeil KJ, et al. Nonalbuminuric renal insufficiency in type 2 diabetes. Diabetes Care 2004;27(1):195–200. [DOI] [PubMed] [Google Scholar]
- 31. Gansevoort RT, Matsushita K, van der Velde M, Astor BC, Woodward M, Levey AS, et al. Lower estimated GFR and higher albuminuria are associated with adverse kidney outcomes. A collaborative meta-analysis of general and high-risk population cohorts. Kidney Int 2011;80(1):93–104. 10.1038/ki.2010.531 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Jerums G, Panagiotopoulos S, Premaratne E, Power DA, Maclsaac RJ. Lowering of proteinria in response to antihypertensive therapy predicts improved renal function in late but not in early diabetic nephropaty: a pooled analysis. Am J Nephrol 2008;28(4):614–27. 10.1159/000117461 [DOI] [PubMed] [Google Scholar]
- 33. Lane PH, Steffes MW, Mauer SM. Glomerular structure in IDDM women with low glomerular filtration rate and normal urinary albumin excretion. Diabetes 1992;41(5):581–6. [DOI] [PubMed] [Google Scholar]
- 34. Tsalamandris C, Allen TJ, Gilbert RE, Sinha A, Panagiotopoulos S, Cooper ME, et al. Progressive decline in renal function in diabetic patients with and without albuminuria. Diabetes 1994;43(5):649–55. [DOI] [PubMed] [Google Scholar]
- 35. Bakris GL, Williams M, Dworkin L, Elliot WJ, Epstein M, et al. Preserving renal function in adults with hypertension and diabetes: a consensus approach. National Kidney Foundation Hypertension and Diabetes Executive Committees Working Group. Am J Kidney Dis 2000;36(3):646–61. [DOI] [PubMed] [Google Scholar]
- 36. Agarwal R, Andersen MJ. Prognostic importance of ambulatory blood pressure recordings in patients with chronic kidney disease. Kidney Int 2006;69(7):1175–80. [DOI] [PubMed] [Google Scholar]
- 37. UK Prospective Diabetes Study Group. Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38. BMJ 1998;317(7160):703–13. [PMC free article] [PubMed] [Google Scholar]
- 38. O’Seaghdha CM, Lyass A, Massaro JM, Meigs JB, Coresh J, D’Agostino RB, et al. A risk score for chronic kidney disease in the general population. Am J Med 2012;125(3):270–7. 10.1016/j.amjmed.2011.09.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Hippisley-Cox J, Coupland C. Predicting the risk of chronic Kidney Disease in men and women in England and Wales: prospective derivation and external validation of the QKidney Scores. BMC Fam Pract 2010;11:49 10.1186/1471-2296-11-49 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Yamagata K, Ishida K, Sairenchi T, Takahashi H, Ohba S, Shiigai T, et al. Risk factors for chronic kidney disease in a community-based population: a 10-year follow-up study. Kidney Int 2007;71(2):159–66. [DOI] [PubMed] [Google Scholar]
- 41. Herget-Rosenthal S, Dehnen D, Kribben A, Quellmann T. Progressive chronic kidney disease in primary care: modifiable risk factors and predictive model. Prev Med 2013;57(4):357–62. 10.1016/j.ypmed.2013.06.010 [DOI] [PubMed] [Google Scholar]
- 42. Gall MA, Hougard P, Borch-Johnsen K, Parving HH. Risk factors for development of incipient and overt diabetic nephropathy in patients with non-insulin dependent diabetes mellitus: prospective, observational study. BMJ 1997;314(7083):738–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Rutledge JC, Ng KF, Aung HH, Wilson DW. Role of triglyceride-rich lipoproteins in diabetic nephropathy. Nat Rev Nephrol 2010;6(6):361–70. 10.1038/nrneph.2010.59 [DOI] [PubMed] [Google Scholar]
- 44. Jenkins AJ, Lyons TJ, Zheng D, Otvos JD, Lackland DT, McGee D, et al. Lipoproteins in the DCCT/EDIC cohort: associations with diabetic nephropathy. Kidney Int 2003;64(3):817–28. [DOI] [PubMed] [Google Scholar]
- 45. Muntner P, Coresh J, Smith JC, Eckfeldt J, Klag MJ. Plasma lipids and risk of developing renal dysfunction: the atherosclerosis risk in communities study. Kidney Int 2000;58(1):293–301. [DOI] [PubMed] [Google Scholar]
- 46. Tozawa M, Iseki K, Iseki C, Oshiro S, Ikemiya Y, Takishita S. Triglyceride, but not total cholesterol or low-density lipoprotein cholesterol levels, predict development of proteinuria. Kidney Int 2002;62(5):1743–9. [DOI] [PubMed] [Google Scholar]
- 47. Zoppini G, Targher G, Chonchol M, Perrone F, Lippi G, Muggeo M. Higher HDL cholesterol levels are associated with a lower incidence of chronic kidney disease in patients with type 2 diabetes. Nutr Metab ardiovasc Dis 2009;19(8):580–6. 10.1016/j.numecd.2008.11.003 [DOI] [PubMed] [Google Scholar]
- 48. Rodriguez-Poncelas A, Garre-Olmo J, Franch-Nadal J, Diez-Espino J,Mundet-Tuduri X, Barrot-De la Puente J, et al. Prevalence of chronic kidney disease in patients with type 2 diabetes in Spain: PERCEDIME2 study. BMC Nephrol 2013;14:46 10.1186/1471-2369-14-46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Hillege HL, van Gilst WH, van Veldhuisen DJ, Navis G, Grobbee DE, de Graeff PA, et al. Accelerated decline and prognostic impact of renal function after myocardial infarction and the benefits of ACE inhibition: the CATS randomizef trial. Eur Heart J 2003;24(5):412–20. [DOI] [PubMed] [Google Scholar]
- 50. Lee ET, Lee VS, Lu M, Lee JS, Russell D, Yeh J. Incidence of renl failure in NIDDM. The Oklahoma Indian Diabetes Study. Diabetes 1994;43(4):572–9. [DOI] [PubMed] [Google Scholar]
- 51. Thakar CV, Christianson A, Himmelfarb J, Leonard AC. Acute kidney injury episodes and chronic kidney disease risk in diabetes mellitus. Clin J Am Soc Nephrol 2011,6(11):2567–72. 10.2215/CJN.01120211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Go AS, Chertow GM, Fan D, McCulloch CE, Hsu C. Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med 2004;351(13):1296–305. [DOI] [PubMed] [Google Scholar]
- 53. Nitsch D, Grams M, Sang Y, Black C, Cirillo M, Djurdjev O, et al. Associations of estimated glomerular filtration rate and albuminuria with mortality and renal failure by sex: a meta-analysis. BMJ 2013;346:f324 10.1136/bmj.f324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Fox CS, Matsushita K, Woodward M, Bilo HJ, Chalmers J, Heerspink HJ, et al. Associations of kidney disease measures with mortality and end-stage renal disease in individuals with and without diabetes: a meta-analysis. Lancet 2012;380(9854):1662–73. 10.1016/S0140-6736(12)61350-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Chronic Kidney Disease Pognosis Consortium, Matsushita K, van der Velde M, Astor BC, Woodward M, Levey AS, et al. Association of estimated glomerular filtration rate and albuminuria with all-cause and cardiovascular mortality in general population cohorts: a collaborative meta-analysis. Lancet 2010;375(9731):2073–81. 10.1016/S0140-6736(10)60674-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Hallan SI, Matsushita K, Sang Y, Mahmoodi BK, Black C, Ishani A, et al. Age and association of kidney measures with mortality and end-stage renal disease. JAMA 2012;308(22):2349–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Thomas G, Sehgal AR, Kashyap SR, Srinivas TR, Kirwan JP, Navaneethan SD, et al. Metabolic Syndrome and kidney disease: a systematic review and meta-analysis. Clin J Am Soc Nephrol 2011;6(10):2364–73. 10.2215/CJN.02180311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Dunkler D, Deghan M, Teo KK, Heinze G, Gao P, Kohl M, et al. Diet and kidney disease in high-risk individuals with type 2 diabetes mellitus. JAMA Intern Med 2013;173(18):1682–92. [DOI] [PubMed] [Google Scholar]
- 59. Díaz-López A, Bulló M, Martínez-González MÁ, Guasch-Ferré M, Ros E, Basora J, et al. Effects of Mediterranean diets on kidney function: a report from the PREDIMED trial. Am J Kidney Dis 2012;60(3):380–9. 10.1053/j.ajkd.2012.02.334 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All relevant data are within the paper.