This qualitative study suggests that African American smokers are aware of the relationship between smoking and lung cancer and are interested in smoking-cessation treatment. These data also indicate that lung cancer disparities are unlikely to be associated with differential willingness to receive care but that African Americans may perceive financial and insurance barriers to lung cancer treatment.
Keywords: Healthcare disparities, Lung neoplasms, Smoking cessation, Black, Qualitative research
Abstract
Background.
Disparities in incidence and mortality for lung cancer in African Americans are well documented; however, the extent to which disparities reflect differences in patient perceptions of tobacco and lung cancer treatment is unclear. The objective of this study was to explore African Americans’ knowledge of lung cancer, perceived risk, interest in smoking cessation, attitudes toward lung cancer treatment, and lung cancer diagnosis and treatment experiences.
Patients and Methods.
The cohort comprised 32 African-American current and former smokers without a cancer diagnosis who participated in focus groups and 10 African Americans with lung cancer who participated in in-depth interviews. Transcripts were analyzed using a modified grounded theory approach.
Results.
Participants without a cancer diagnosis were aware of the link between smoking and lung cancer, the common symptoms of the disease, and its poor prognosis. They desired specific, personalized smoking-cessation information. If diagnosed, the majority reported, they would seek medical care. Most believed that insurance and socioeconomic factors were more likely to affect treatment access than racial discrimination. Participants with a cancer diagnosis were also aware of the relationship between smoking and lung cancer. They felt their treatment plans were appropriate and trusted their physicians. Most did not believe that race affected their care.
Conclusion.
This qualitative study suggests that African-American smokers are aware of the relationship between smoking and lung cancer and are interested in smoking-cessation treatment. These data also indicate that lung cancer disparities are unlikely to be associated with differential willingness to receive care but that African Americans may perceive financial and insurance barriers to lung cancer treatment.
Implications for Practice:
Findings from this qualitative study suggest that African-American smokers recognize the relationship between smoking and lung cancer but also may attribute additional causal factors, for example, occupational and environmental factors. Smoking cessation messages and treatment approaches for African-American smokers should be personalized and specific. Further education about lung cancer symptoms also appears to be needed. Although most participants did not perceive access to or quality of care to be affected by race, and race did not affect their willingness to seek treatment for lung cancer, concerns expressed about potential insurance barriers to lung cancer treatment should researched further.
Introduction
Lung cancer is the leading cause of cancer mortality for men and women in the U.S. [1]. Survival rates are poor: only 15% survive 5 years past diagnosis [1]. African Americans have the highest incidence of and mortality from lung cancer [1–4]. Lung cancer incidence and mortality rates have decreased for all races over the past 20 years [5], likely because of decreased tobacco use; however, differences between black and white populations remain [3, 6]. Although tobacco use leads to most lung cancer diagnoses [7], it does not account for this disparity. White male smokers consume 30%–40% more cigarettes than their black counterparts, but black male smokers are 34% more likely to develop lung cancer. Black women smoke less on average than white women but have similar incidence rates [2, 8]. Reasons for these differences are not clear but may include access to surgical care, hospital-level factors, biological differences in response to tobacco smoke, and patient treatment preferences [9–18].
Black patients also tend to present with later stage lung cancer and higher symptom burden than their white counterparts [3, 19, 20]. Several studies have suggested that African-American patients may have different feelings regarding risk perception, fatalism, and fear of a cancer diagnosis [10, 21–27] that could affect interpretation of prevention messages and seeking medical care for symptoms. Few studies, however, focus on African Americans’ knowledge and beliefs associated specifically with lung cancer. Themes that have been explored include fatalism, fear of diagnosis, distrust of surgeons, treatment misconceptions, hope, and desire for more information [10, 28–30].
The high incidence of lung cancer among African Americans and aggressive targeting of African Americans by tobacco manufactures have prompted many in the public health community to focus on factors that enhance smoking-cessation campaigns [29, 31, 32]. These studies demonstrate that low income and limited education adversely affect cessation attempts and that often black smokers underestimate the link between cancer and tobacco smoking compared with white smokers. Previous analysis of the Health Information Trends Survey (HINTS) database indicated that patients of all races underestimated the lethality of lung cancer, but African Americans appeared to expect more symptoms, be more reluctant to seek care because of fear of disease, be confused about preventive recommendations, and be more likely to doubt the association of lung cancer with lifestyle [33]. The HINTS database was limited by its paucity of African American men and participants of lower socioeconomic status who would be at the highest risk for lung cancer [34, 35].
Lung cancer is unique among solid tumor cancers in its combination of social stigma and mortality rate; consequently, qualitative findings from other cancers such as breast and colon cancer cannot simply be extrapolated to lung cancer patients. This study sought to identify potentially salient but under-recognized factors that may account for differences in the care and medical outcomes of African Americans with lung cancer. We included participants at risk for lung cancer and those who had experienced it to examine (a) factors related to risk perception and interpretation of early symptoms that may contribute to diagnostic delays, and (b) beliefs about the medical establishment and efficacy of particular therapies that may contribute to underuse of proven treatment interventions.
Methods
Recruitment of Smokers and Former Smokers Without Cancer History
We partnered with a subsidized housing community in Boston, Massachusetts, to recruit for this study through announcements at community centers and flyers posted in the housing complex. The housing complex had a largely African-American population, with 38% of residents having income below the poverty line. Most residents had insurance: 45% had a combination of Medicare and Medicaid, and 41% had private insurance.
We decided to require a minimum age of 35 years to explore the perspectives of adults with a long enough smoking history to have a significantly elevated risk of developing lung cancer [36–38]. Other eligibility criteria included self-identifying as African American, meeting the National Cancer Institute definition of a current smoker (smoked at least one puff in the past 7 days) or a former smoker (smoked at least 100 cigarettes in one’s lifetime but has not smoked within past 7 days), and having no prior cancer history.
Recruitment of Lung Cancer Patients
Lung cancer patients were recruited from the Dana-Farber Cancer Institute (DFCI). The eligibility criteria included self-identifying as African American, having a documented diagnosis of lung cancer, and receiving treatment at DFCI. No patients with a lung cancer diagnosis were excluded from the study based on smoking status.
The study received full approval from the Dana-Farber/Harvard Cancer Center institutional review board, and informed consent was solicited from all study participants.
Focus Group and Interview Procedures
All participants received a $50 money order for participating. Four focus groups and 10 interviews were conducted in 2009 by a trained qualitative researcher (J.G.). One lung cancer participant was a patient of the lead investigator (C.S.L.); no other prior relationship existed with any study participant in a clinical or personal context.
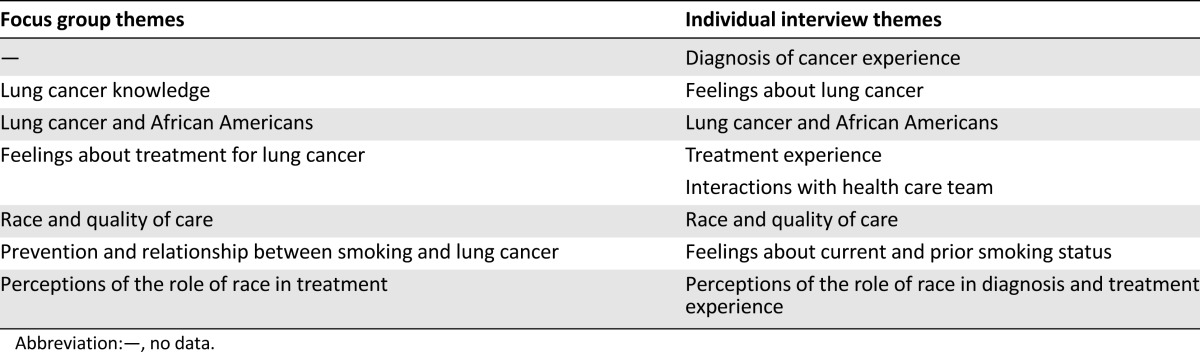
Separate semistructured discussion guides were developed for the non-lung cancer and lung cancer participants (Table 1) based on the literature and experiences of the study investigators (C.S.L., K.E.) with lung cancer patients at the cancer center and with patients at a medical center serving vulnerable populations. A unique study identifier was assigned to each participant. Focus group and interview audiotapes were transcribed, omitting any details that could potentially be used to identify participants.
Table 1.
Focus group discussion guide and individual interview guide themes
Data Analysis
A modified grounded theory approach was used for the analysis [39]. Grounded theory is suited to the exploratory nature of this study. Although we began with themes derived from the literature and clinical observations, the analysis was conducted in the context of themes and concepts that emerged from the focus group and interview data, using the constant comparative method to continually assess and refine recurrent themes [40]. Saturation, the point where no new themes emerged and no new or valuable information emerged about the themes already identified [41], was determined to have been reached when 75% of the focus groups and individual interviews had been conducted.
Audio recordings were transcribed by a professional transcriber who took reviewed all transcripts while listening to the audio recordings to confirm accuracy. Transcripts were then reviewed by two authors (C.S.L., J.G.) to identify preliminary key themes and analyzed according to a standard comprehensive qualitative analysis method composed of a two-stage coding process. Structural coding followed the structure of the focus group and interview guides, with each question receiving a structural code that was applied to the appropriate text. Thematic coding based on themes arising from the structural coding were applied in a re-review analysis [39]. These methods were enhanced by the use of an ethnographic data management software program, NVivo (QSR International, Doncaster, Australia, http://www.qsrinternational.com/products_nvivo.aspx). One author (J.G.) did all of the coding; therefore, no inter-rater reliability needed to be established. The same author then prepared a comprehensive thematic analysis report. Another author (L.T.W.) reviewed the report and cross-checked its findings against the original transcripts to confirm that a shared understanding was reached among multiple authors regarding the interpretation of participants’ narratives.
Results
Focus Groups
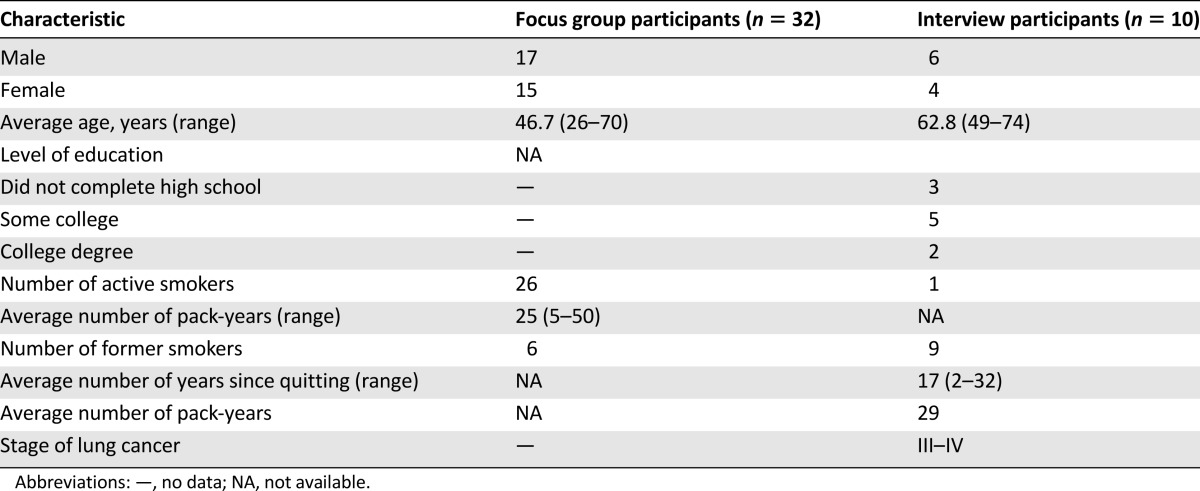
A total of 17 men and 15 women participated in 4 focus group sessions. Characteristics of the sample are presented in Table 2.
Table 2.
Demographic and health characteristics of study sample
Focus Group Themes
Lung Cancer Knowledge
Participants discussed what they had heard about lung cancer, including causes, characteristics, and prognosis of the disease. Most participants expressed clear understanding of its symptomatology, particularly noting shortness of breath, coughing, coughing up blood, and chest pain, and awareness of its poor prognosis.
The mortality rate is greater than other cancers. [Focus group 1, participant 4]
Everybody I know that has contracted lung cancer, including our father, has died within 6 months of their diagnosis. [Focus group 3, participant 4]
Most participants were aware that cigarette smoking was the main environmental exposure. Several also mentioned that some patients are diagnosed with lung cancer without a smoking history and that other environmental agents can also cause lung cancer. Asbestos, second-hand smoke, and air pollution were all mentioned as possible causes.
Personal Risk for Lung Cancer
Most focus group participants worried about getting lung cancer as a result of their smoking history.
I really need to put this down ‘cause, I mean, this is no good for nobody. I might end up with lung cancer. This is ridiculous, but you keep puffin’! [Focus group 3, participant 7]
One participant, however, believed the risk of lung cancer was not limited to smokers.
I think anybody can have lung cancer with everything around them, so everybody’s at risk. [Focus group 2, participant 3]
When asked what they would do if diagnosed with lung cancer, participants most commonly responded that they would seek information about treatment options from their doctor. Only one participant reported that he would not seek treatment because of his father’s experience.
My father died from cancer, and I’ve seen what he went through. All these chemos and stuff ... I don’t want to put myself through that. [Focus group 1, participant 1]
A few participants expressed uncertainty about what they would do.
That’s so hard to answer because ... even though you have all these options, uh, what’s the outcome on any of them? I mean, are you gonna live? Is there a chance you’re gonna live? And what is the best treatment? [Focus group 3, participant 4]
Causes of Lung Cancer Disparities
Most participants felt that African Americans were at high risk for lung cancer because they smoked more cigarettes. The targeting of African Americans in tobacco advertising was a key theme that emerged. Newport cigarettes [Lorillard, Greensboro, NC, http://www.lorillard.com] were mentioned repeatedly as an example of the marketing done in African-American communities.
I’ve lived in predominantly black communities, and I’ve lived in predominantly white neighborhoods, and I never see a 2-for-1 sale on Newports in white neighborhoods. [Focus group 4, participant 7]
Smoking Cessation
Participants expressed concern about the lack of insurance coverage and relatively high out-of-pocket costs for cessation aids. They wanted increased access to cessation programs and products. They also wanted their doctors to be more proactive in helping them to quit smoking based on their individual health status.
When, you know, they’re hearin’ your breathin’, like, I always ask ’em ... “Do you think ... ” [and] they always say, “Oh, your lungs are good. I can hear your lungs.” So there weren’t any time when my lungs were bad, so ... I don’t be thinkin’ I have cancer or anything, but ... if my doctors had concerns, like, you know, you’re breathing, and she, if she would say somethin’ like, “Your breathin’s kind of slow,” that’d give me more incentive ... incentive to stop, if somebody told me they ... feel that I am gonna get it if I continue smoking. [Focus group 4, participant 4]
I actually had a doctor say, “Oh, you just need to cut down a little. You don’t need to stop smoking.” But I think if I really felt like the doctors were concerned and that I had their support, and there was someone ... who was really sort of looking out for me, I would probably ... make more of an attempt. [Focus group 4, participant 7].
Several participants expressed a desire to have their lungs scanned and compared with normal lungs. They felt that seeing a graphic display of the damage done to their lungs would help them to quit.
I think it’s the only thing they can to do to stop a ... a serious smoker, you know what I mean? Say, “Listen. We’re gonna do this. We’re gonna take a picture of your lungs. Each year you keep smoking,” you know what I mean ... ? [Focus group 1, participant 7]
Treatment for Lung Cancer
Participants seemed well aware of treatment options for lung cancer, including surgery, radiation, and chemotherapy. Several spoke specifically about chemotherapy, focusing on its side effects. Although some participants believed it was effective, others believed it could be fatal.
I have heard the treatment of chemotherapy. You get sicker faster ... some people can get over it and get well, but some people ... just ... drizzle away and die. [Focus group 3, participant 8]
Several participants had a negative perception of surgery, stemming from fear of surgery, belief that radiation or chemotherapy treatments would be more effective, or concern that the surgeon would be unable to remove all of the cancer.
Haven’t they got a better chance of missin’ some of the cancer ... with surgery? And they got a better chance of gettin’ most of it with chemo? [Focus group 2, participant 6]
Despite their concerns, only three participants stated that they would refuse surgery or chemotherapy. Most indicated that they would consider the treatments their doctors recommended.
A few participants discussed personalized medicine for lung cancer. They believed gene therapy shrinks the tumor but does not cure the disease and only works for some people.
I heard it only works in a percent of the people, and they have to have a certain type of cancer, and it has to be at a certain, uh, stage. [Focus group 1, participant 4]
Participants concurred that if they needed to seek treatment for lung cancer, they would trust the oncologist about cancer-specific information but would need to build rapport.
You gotta get to know him. I’m not gonna trust nobody from the one damn time. [Focus group 1, participant 3]
Several participants further discussed seeking a second opinion regardless of the physician’s recommendation.
You gotta get more. You just don’t take one. [Focus group 3, participant 6]
Race and Quality of Care
Half of the focus group participants felt that insurance status and income level determined quality of care more than race.
I don’t care what color you are. If your money ain’t right ... they’ll let you die. [Focus group 2, participant 1]
Five participants felt that race affected treatment and quality of care. They discussed history, their observations, and racial profiling.
I also think that there’s always been a disparity in terms of the medical treatment that black people get versus white people. I mean, you can literally walk downtown, and you see all these very healthy-looking white people walking down, and you see all these black people with, like, canes, and they’re, like, coughing, and their skin’s all screwed up. ... I remember, years ago, seeing something ... some PBS documentary about how doctors kind of profile patients? And black people are considered “dramatic,” so they’ll come and complain about something, and they’re not taken as seriously as somebody who’s Asian who never complains about anything. [Focus group 4, participant 7]
Five participants believed quality of care was affected by a combination of race, economics, and insurance coverage. Another four felt it was the patient’s responsibility to obtain the best care possible.
If you demand good care, you get good care. [Focus group 1, participant 4]
Lung Cancer Patient Interviews
Six African-American men and four African-American women treated at our cancer center participated in in-depth interviews to explore themes involving the treatment experience. Sample characteristics are presented in Table 2. One had never smoked, one remained a current smoker, and the others had stopped smoking prior to diagnosis.
Interview Themes
Diagnosis Experience, Treatment, and Provider Trust
Most participants presented with specific symptoms (four with cough, three with flu- or cold-like symptoms, two with back pain), and one was found through a screening computed tomography scan. Most did not suspect that they had lung cancer prior to diagnosis. A few reported that the initial shock they experienced made it difficult to interact with their care team or to recall their initial conversations.
So, this guy’s like, “Oh, adadadadadad” ... and all I could hear was ... “you could die,” and “cancer” ... I’m sure he was compassionate, I’m sure he was nice. I didn’t hear it ... I just was so ... too much in shock, too overwhelmed, couldn’t hear it. [Interview participant 3]
Most participants were happy with their treatment plans and felt comfortable asking questions of their oncologists. Two were dissatisfied with the proposed care plans and communications at the institutions where they had received their initial diagnoses but were happy with the cancer center. Six participants agreed to their physician’s choice of treatment, whereas the other four sought second opinions and changed physicians before agreeing to a treatment plan. All felt the treatment plans they pursued were appropriate and trusted their medical teams.
They knew what they were doin’, as far as I was concerned. [Interview participant 5]
Participants overwhelmingly reported that they did not fear the treatments but had different reasons. Some expressed confidence in the environment, whereas other noted their age and life experience.
I’m 71 years old, and my daddy died at 76 ... so, you know, I don’t fear ... really fear nothing. You understand? If it’s gonna happen, it’s gonna happen ... it’s not like I’m a young man and who’s lookin’ 50 years from now. [Interview participant 8]
Perceptions of What Causes Lung Cancer
Although 9 of the 10 participants had a smoking history, only 2 identified smoking as the sole or primary cause of their lung cancer. Four male participants believed occupational exposure to hazardous chemicals may have also been a contributing factor, and two female participants noted that they had quit smoking decades earlier. Three participants further mentioned that nonsmokers can also develop lung cancer, and one suggested that heredity was an additional factor because not everyone who smokes develops lung cancer. Nevertheless, most reported wishing they had quit sooner or never smoked at all.
I wished to heck that I had never smoked ... that’s somethin’ that was in my control. I’m not too sure that my occupation, um, was in my control ... but at that time, we never, nobody knew that asbestos did cause lung cancer. [Interview participant 6]
All participants believed that others assume lung cancer patients are smokers and that many use it to judge their character.
It is probably viewed as one of those cancers that’s caused by somethin’ that you did, um, ... but ...when I say lung cancer, the first thought that probably went through somebody’s mind is that she was smoker. [Interview participant 1]
The lethality of lung cancer was also discussed, but a majority of participants maintained a positive outlook on their personal circumstances. When asked how they currently felt about their diagnosis, three described themselves as happy and satisfied with their treatment, and another three reported feeling physically and mentally well.
Well, physically, I feel much better, and mentally, also ... I know it’s somethin’ that I’ll have, but I feel better that ... we have it under remission at the moment. [Interview participant 7]
Two patients reported that they had made progress in learning to cope with their diagnosis.
I look at it more like a ... a disease? Not ... somethin’ that I’m gonna die from ... I’m ... like a person with diabetes ... it’s somethin’ that I have, and ... I take a pill daily, and I go in to see the doctor ... but it doesn’t affect my daily life. [Interview participant 1]
No one reported having considered refusing or discontinuing treatment, but one participant felt that her initial providers had failed to inform her about the side effects of treatment and to discuss the emotional and psychological side of having cancer and cancer treatments.
I wish ... at the very beginning they had been a lot more honest about ... you know, the roller coaster that you’re on. [Interview participant 3]
Race and Quality of Care
Most participants did not feel like race factored into their treatment or communication at any of the institutions where they had received care.
I was a patient, and everybody just pitched right in and gave me the best advice and care that ... they had at their disposal. I don’t think I could have gotten any better care, you know, if I were ... like a billionaire, if I were Oprah Winfrey! [Interview participant 10]
Two participants, however, suspected that race might have affected the care they had received at prior institutions. Another participant felt that race affected his communications with health care providers but not his treatment.
I would think that it’s in the back of any African American’s ... mind ... I mean ... there’s certainly racism in ... in this country ... and yeah, things are changing but ... I always felt that there’s still racism ... in people’s actions and ... it’s subtle, but it is somethin’ that, yeah, I did think about. [Interview participant 6]
Lung Cancer and African Americans
All but one participant felt that lung cancer was not viewed as a prevalent issue among African Americans and that there was more emphasis on other illnesses and cancers.
I think it’s too low. I mean, I don’t think the lung ... related to African-American cancers, been ... put out there enough that people are like, “Oh, we should get checked.” Where, you know, breast cancer’s been so ... it’s been so loud that everybody, you know, goes and gets checked and, you know, gets mammograms and self-testing. [Interview participant 3]
Discussion
A majority of focus group and individual interview participants were well aware of the links between smoking and lung cancer, although several noted that smoking was not the only risk factor. Focus group members desired specific, personalized cessation aids and recommendations from their physicians. The literature similarly suggests that smoking-cessation assistance should be coupled with specific recommendations [42, 43]. Participants also felt that being able to see imaging of their lungs could help motivate them to quit smoking. This sentiment is intriguing in light of recent data on low-dose computed tomography for screening smokers for lung cancer [44, 45]. A systematic review found that although abnormal test results correlated with higher cessation rates, no relationship was found between smoking behaviors and negative test results [46]. Future research should examine the potential for cessation information to be provided in conjunction with lung cancer screenings.
Our study findings differ from previous reports of African-American treatment preferences and the HINTS database regarding lung cancer knowledge. Study participants appeared to have good working knowledge of lung cancer and its behavioral risk factors, although they also noted risk factors that were beyond their control such as occupational exposures and genetics. Although focus group participants displayed knowledge of lung cancer symptoms, most lung cancer participants did not suspect their symptoms to be lung cancer prior to diagnosis, suggesting a need for further education.
Whereas the HINTS data suggested that African Americans were reluctant to seek medical attention due to fear, most focus group participants indicated they would consider treatments for lung cancer, including surgery, chemotherapy, and radiation, if recommended by their physician. Similarly, lung cancer participants proactively sought treatment, trusted their health care team, and were happy with their treatment plan. There could be many reasons for these differences. Our patient population was of lower socioeconomic status than those included in HINTS. In addition, we had equal representation of African-American men, who were underrepresented in the HINTS analysis.
Most focus group participants felt that income and insurance were more significant than race in obtaining high-quality care. Lung cancer participants were also less likely to view race as an impediment to treatment and felt comfortable with the treatment choices recommended by their physicians. Focus group and lung cancer participants alike discussed the stigma associated with a lung cancer diagnosis and the lack of attention lung cancer gets in relation to other diseases in African American communities. This is similar to previously reported findings about the excessive stigma and shame that can accompany lung cancer [30, 47, 48].
Our study is based on a small sample size, and because not every participant responded to each question in the semistructured focus group and interview format, the full range of views among the sample cannot be known. It is also possible that study findings may have been influenced by self-selection bias, particularly among the lung cancer participants, because those who chose to participate may have done so because they were satisfied with their care. In addition, because all lung cancer participants were patients at a cancer center, we were not able to elicit views from lung cancer patients who had chosen not to pursue treatment. Further research would be needed to determine whether our results can be generalized to other clinical or geographical settings.
Conclusion
Study findings suggest that a more specific program for smoking cessation is needed. The extent that patient preference plays a role in racial disparities in cancer outcomes remains unclear; however, study findings point to a desire for further education and communication about prevention, cessation, and treatment options. In addition, the perception of barriers based on insurance appeared to be a major concern for the participants. Future research should focus on both real and perceived barriers to ensure access to effective, appropriate cancer care.
This article is available for continuing medical education credit at CME.TheOncologist.com.
Acknowledgments
We thank all of the study participants. We also thank Elyse Park for her valuable comments on an earlier draft. These data were presented in part at the 2010 American Association for Cancer Research conference on the Science of Cancer Health Disparities in Racial/Ethnic Minorities and the Medically Underserved. This study received funding from the National Cancer Institute (K01 CA124581 and 5K05CA124415-05).
Author Contributions
Conception/Design: Christopher S. Lathan, Karen Emmons
Provision of study material or patients: Christopher S. Lathan, Emily Browning, Karen Emmons
Collection and/or assembly of data: Christopher S. Lathan, Emily Browning, Joshua Gagne
Data analysis and interpretation: Christopher S. Lathan, Laura Tesler Waldman, Joshua Gagne
Manuscript writing: Christopher S. Lathan, Laura Tesler Waldman, Joshua Gagne
Final approval of manuscript: Christopher S. Lathan, Laura Tesler Waldman, Emily Browning, Joshua Gagne, Karen Emmons
Disclosures
Karen Emmons: Kaiser Permanente (E). The other authors indicated no financial relationships.
(C/A) Consulting/advisory relationship; (RF) Research funding; (E) Employment; (ET) Expert testimony; (H) Honoraria received; (OI) Ownership interests; (IP) Intellectual property rights/inventor/patent holder; (SAB) Scientific advisory board
References
- 1.Cancer facts and figures 2008. Atlanta, GA: American Cancer Society; 2008. [Google Scholar]
- 2.United States cancer statistics: 1999-2011 cancer incidence and mortality data. Available at http://www.cdc.gov/uscs. Accessed April 28, 2014.
- 3.Stewart J. Lung carcinoma in African Americans: A review of the current literature. Cancer. 2001;91:2476–2482. [PubMed] [Google Scholar]
- 4.Racial/ethnic disparities and geographic differences in lung cancer incidence — 38 states and the District of Columbia, 1998-2006. MMWR Morb Mortal Wkly Rep. 2010;59:1434–1438. [PubMed] [Google Scholar]
- 5.Pratt-Chapman M, Simon MA, Patterson AK, et al. Survivorship navigation outcome measures: A report from the ACS patient navigation working group on survivorship navigation. Cancer. 2011;117(suppl):3575–3584. doi: 10.1002/cncr.26261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gadgeel SM, Kalemkerian GP. Racial differences in lung cancer. Cancer Metastasis Rev. 2003;22:39–46. doi: 10.1023/a:1022207917249. [DOI] [PubMed] [Google Scholar]
- 7.Molina JR, Yang P, Cassivi SD, et al. Non-small cell lung cancer: Epidemiology, risk factors, treatment, and survivorship. Mayo Clin Proc. 2008;83:584–594. doi: 10.4065/83.5.584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.African Americans. Available at http://www.lung.org/stop-smoking/about-smoking/facts-figures/african-americans-and-tobacco.html#6. Accessed April 28, 2014.
- 9.Mulligan CR, Meram AD, Proctor CD, et al. Unlimited access to care: Effect on racial disparity and prognostic factors in lung cancer. Cancer Epidemiol Biomarkers Prev. 2006;15:25–31. doi: 10.1158/1055-9965.EPI-05-0537. [DOI] [PubMed] [Google Scholar]
- 10.Margolis ML, Christie JD, Silvestri GA, et al. Racial differences pertaining to a belief about lung cancer surgery: Results of a multicenter survey. Ann Intern Med. 2003;139:558–563. doi: 10.7326/0003-4819-139-7-200310070-00007. [DOI] [PubMed] [Google Scholar]
- 11.Earle CC, Neumann PJ, Gelber RD, et al. Impact of referral patterns on the use of chemotherapy for lung cancer. J Clin Oncol. 2002;20:1786–1792. doi: 10.1200/JCO.2002.07.142. [DOI] [PubMed] [Google Scholar]
- 12.Earle CC, Venditti LN, Neumann PJ, et al. Who gets chemotherapy for metastatic lung cancer? Chest. 2000;117:1239–1246. doi: 10.1378/chest.117.5.1239. [DOI] [PubMed] [Google Scholar]
- 13.Lathan CS, Neville BA, Earle CC. Racial composition of hospitals: Effects on surgery for early-stage non-small-cell lung cancer. J Clin Oncol. 2008;26:4347–4352. doi: 10.1200/JCO.2007.15.5291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Esnaola NF, Gebregziabher M, Knott K, et al. Underuse of surgical resection for localized, non-small cell lung cancer among whites and African Americans in South Carolina. Ann Thorac Surg. 2008;86:220–226; discussion 227. doi: 10.1016/j.athoracsur.2008.02.072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Farjah F, Wood DE, Yanez ND, III, et al. Racial disparities among patients with lung cancer who were recommended operative therapy. Arch Surg. 2009;144:14–18. doi: 10.1001/archsurg.2008.519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Geyer S. Social inequalities in the incidence and case fatality of cancers of the lung, the stomach, the bowels, and the breast. Cancer Causes Control. 2008;19:965–974. doi: 10.1007/s10552-008-9162-5. [DOI] [PubMed] [Google Scholar]
- 17.Greenwald HP, Polissar NL, Borgatta EF, et al. Social factors, treatment, and survival in early-stage non-small cell lung cancer. Am J Public Health. 1998;88:1681–1684. doi: 10.2105/ajph.88.11.1681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Haiman CA, Stram DO, Wilkens LR, et al. Ethnic and racial differences in the smoking-related risk of lung cancer. N Engl J Med. 2006;354:333–342. doi: 10.1056/NEJMoa033250. [DOI] [PubMed] [Google Scholar]
- 19.Blackstock AW, Herndon JE, II, Paskett ED, et al. Outcomes among African-American/non-African-American patients with advanced non-small-cell lung carcinoma: Report from the Cancer and Leukemia Group B. J Natl Cancer Inst. 2002;94:284–290. doi: 10.1093/jnci/94.4.284. [DOI] [PubMed] [Google Scholar]
- 20.Hayat MJ, Howlader N, Reichman ME, et al. Cancer statistics, trends, and multiple primary cancer analyses from the Surveillance, Epidemiology, and End Results (SEER) program. The Oncologist. 2007;12:20–37. doi: 10.1634/theoncologist.12-1-20. [DOI] [PubMed] [Google Scholar]
- 21.Gordon HS, Street RL, Jr, Sharf BF, et al. Racial differences in trust and lung cancer patients’ perceptions of physician communication. J Clin Oncol. 2006;24:904–909. doi: 10.1200/JCO.2005.03.1955. [DOI] [PubMed] [Google Scholar]
- 22.Morgan PD, Tyler ID, Fogel J. Fatalism revisited. Semin Oncol Nurs. 2008;24:237–245. doi: 10.1016/j.soncn.2008.08.003. [DOI] [PubMed] [Google Scholar]
- 23.Niederdeppe J, Levy AG. Fatalistic beliefs about cancer prevention and three prevention behaviors. Cancer Epidemiol Biomarkers Prev. 2007;16:998–1003. doi: 10.1158/1055-9965.EPI-06-0608. [DOI] [PubMed] [Google Scholar]
- 24.Shankar S, Selvin E, Alberg AJ. Perceptions of cancer in an African-American community: A focus group report. Ethn Dis. 2002;12:276–283. [PubMed] [Google Scholar]
- 25.Greiner KA, Born W, Nollen N, et al. Knowledge and perceptions of colorectal cancer screening among urban African Americans. J Gen Intern Med. 2005;20:977–983. doi: 10.1111/j.1525-1497.2005.00165.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Forrester-Anderson IT. Prostate cancer screening perceptions, knowledge and behaviors among African American men: Focus group findings. J Health Care Poor Underserved. 2005;16(suppl A):22–30. doi: 10.1353/hpu.2005.0122. [DOI] [PubMed] [Google Scholar]
- 27.Powe BD, Daniels EC, Finnie R. Comparing perceptions of cancer fatalism among African American patients and their providers. J Am Acad Nurse Pract. 2005;17:318–324. doi: 10.1111/j.1745-7599.2005.0049.x. [DOI] [PubMed] [Google Scholar]
- 28.Jonnalagadda S, Lin JJ, Nelson JE, et al. Racial and ethnic differences in beliefs about lung cancer care. Chest. 2012;142:1251–1258. doi: 10.1378/chest.12-0330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.George M, Margolis ML. Race and lung cancer surgery—a qualitative analysis of relevant beliefs and management preferences. Oncol Nurs Forum. 2010;37:740–748. doi: 10.1188/10.ONF.740-748. [DOI] [PubMed] [Google Scholar]
- 30.Chapple A, Ziebland S, McPherson A. Stigma, shame, and blame experienced by patients with lung cancer: Qualitative study. BMJ. 2004;328:1470. doi: 10.1136/bmj.38111.639734.7C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Manfredi C, Lacey L, Warnecke R, et al. Smoking-related behavior, beliefs, and social environment of young black women in subsidized public housing in Chicago. Am J Public Health. 1992;82:267–272. doi: 10.2105/ajph.82.2.267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Klesges RC, Somes G, Pascale RW, et al. Knowledge and beliefs regarding the consequences of cigarette smoking and their relationships to smoking status in a biracial sample. Health Psychol. 1988;7:387–401. doi: 10.1037//0278-6133.7.5.387. [DOI] [PubMed] [Google Scholar]
- 33.Lathan CS, Okechukwu C, Drake BF, et al. Racial differences in the perception of lung cancer: The 2005 Health Information National Trends Survey. Cancer. 2010;116:1981–1986. doi: 10.1002/cncr.24923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Albano JD, Ward E, Jemal A, et al. Cancer mortality in the United States by education level and race. J Natl Cancer Inst. 2007;99:1384–1394. doi: 10.1093/jnci/djm127. [DOI] [PubMed] [Google Scholar]
- 35.Alberg AJ, Brock MV, Samet JM. Epidemiology of lung cancer: Looking to the future. J Clin Oncol. 2005;23:3175–3185. doi: 10.1200/JCO.2005.10.462. [DOI] [PubMed] [Google Scholar]
- 36.Jha P, Ramasundarahettige C, Landsman V, et al. 21st-century hazards of smoking and benefits of cessation in the United States. N Engl J Med. 2013;368:341–350. doi: 10.1056/NEJMsa1211128. [DOI] [PubMed] [Google Scholar]
- 37.Thun MJ, Carter BD, Feskanich D, et al. 50-year trends in smoking-related mortality in the United States. N Engl J Med. 2013;368:351–364. doi: 10.1056/NEJMsa1211127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Pirie K, Peto R, Reeves GK, et al. The 21st century hazards of smoking and benefits of stopping: A prospective study of one million women in the UK. Lancet. 2013;381:133–141. doi: 10.1016/S0140-6736(12)61720-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Walker D, Myrick F. Grounded theory: An exploration of process and procedure. Qual Health Res. 2006;16:547–559. doi: 10.1177/1049732305285972. [DOI] [PubMed] [Google Scholar]
- 40.Glaser BG. The constant comparative method of qualitative analysis. Soc Probl. 1965;12:436–445. [Google Scholar]
- 41.Cutcliffe JR. Methodological issues in grounded theory. J Adv Nurs. 2000;31:1476–1484. doi: 10.1046/j.1365-2648.2000.01430.x. [DOI] [PubMed] [Google Scholar]
- 42.Glock S, Unz D, Kovacs C. Beyond fear appeals: Contradicting positive smoking outcome expectancies to influence smokers' implicit attitudes, perception, and behavior. Addict Behav. 2012;37:548–551. doi: 10.1016/j.addbeh.2011.11.032. [DOI] [PubMed] [Google Scholar]
- 43.Clark E, McCann TV. The influence of friends on smoking commencement and cessation in undergraduate nursing students: A survey. Contemp Nurse. 2008;27:185–193. doi: 10.5555/conu.2008.27.2.185. [DOI] [PubMed] [Google Scholar]
- 44.Aberle DR, Adams AM, Berg CD, et al. Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med. 2011;365:395–409. doi: 10.1056/NEJMoa1102873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Peres J. Lung cancer screening: Ready for prime time? J Natl Cancer Inst. 2010. [Epub ahead of print] [DOI] [PubMed]
- 46.Slatore C, Baumann C, Pappas M, et al. Smoking behaviors among patients receiving computed tomography for lung cancer screening: Systematic review in support of the U.S. Preventive Services Task Force. Ann Am Thorac Soc. 2014;11:619–627. doi: 10.1513/AnnalsATS.201312-460OC. [DOI] [PubMed] [Google Scholar]
- 47.Chapple A, Ziebland S, McPherson A, et al. Lung cancer patients’ perceptions of access to financial benefits: A qualitative study. Br J Gen Pract. 2004;54:589–594. [PMC free article] [PubMed] [Google Scholar]
- 48.Clegg LX, Reichman ME, Miller BA, et al. Impact of socioeconomic status on cancer incidence and stage at diagnosis: Selected findings from the Surveillance, Epidemiology, and End Results: National Longitudinal Mortality Study. Cancer Causes Control. 2009;20:417–435. doi: 10.1007/s10552-008-9256-0. [DOI] [PMC free article] [PubMed] [Google Scholar]


