The aims of this study were to assess public perception of the risk factors for cancer and to assess myths and misconceptions about cancer risk. Results showed that a sizable portion of the population studied is misinformed about cancer risk. Targeted health-promotion campaigns that lead to better understanding of risk factors and increased prevention efforts will offer cost-effective, sustainable means of reducing the global cancer burden in the long term.
Keywords: Cancer, Knowledge, Risk, Diet, Lifestyle, Attitudes, Myths
Abstract
Background.
Knowledge of cancer risk factors is unknown in Ireland. An understanding of risk factors could help inform cancer prevention programs.
Aims and Methods.
A 48-question online survey was designed to gather data to assess levels of public knowledge about cancer risk factors.
Results.
There were 748 participants (648 women, 100 men). Mean age was 37 years (range: 18–74 years). For the public, 81% were concerned about developing cancer; however, 20% believed that cancer is unavoidable if a family history exists, 27% believed that >50% of cancers are inherited, and 54% believed that 10%–20% of cancers are inherited; 20% were unaware that risk increases with age. The top five risk factors listed by respondents were smoking (87%), diet (76%), genetics (47%), alcohol (42%), and obesity (33%). Only 32% of the public were aware that obesity is a risk factor, and 33% did not think the location of fat was important. Moreover, 29% and 48% believed that risk could be increased by wearing a tight bra and by a blow to the breast, respectively. In addition, 85% and 86% believed that stress and that mobile phones, respectively, “strongly” increase risk; 12% believed that luck is important in avoiding cancer; 35% thought that “detox” diets could reduce risk; and 61% believed that organic food reduces risk. The majority were aware that physical activity of 30 minutes per day can reduce risk.
Conclusion.
A sizable portion of the population is misinformed about cancer risk. Most participants were aware of classic risk factors (e.g., smoking, diet); however, many overestimated risk attributable to genetics, environment, and stress and underestimated age, obesity, and sunlight. One in seven participants believed that lifetime risk of cancer is not modifiable.
Implications for Practice:
Preventing cancer by avoiding exposure to particular carcinogens follows from knowledge of causation. This study demonstrated that Irish adults have poor awareness of established risk factors for cancer. Many participants were aware of classic risk factors, but many overestimated risk attributable to genetics, environment, and stress and underestimated age, obesity, and sunlight. Because health beliefs are strong determinants of health behaviors, these data have implications for the promotion of cancer awareness. Targeted health-promotion campaigns that lead to better understanding of risk factors and increased prevention efforts will offer cost-effective, sustainable means of reducing the global cancer burden in the long term.
Introduction
The worldwide burden of cancer continues to increase largely because of an aging population and an increase in cancer-causing behaviors [1]. New figures and projections of the global cancer burden presented in the World Cancer Report 2014 [2] estimate that incidence of cancer has increased from 12.7 million in 2008 to 14.1 million in 2012. This trend is projected to continue, with the number of new cases expected to rise another 75%, which would bring the number of annual cancer cases close to 25 million over the next two decades. Cancer causes 8 million deaths annually, and in Ireland, it is estimated that 1 in 3 men and 1 in 4 women will develop cancer during their lifetime [3].
Primary prevention through lifestyle and environmental interventions remains the main way to reduce the global burden of cancers [4]. It is estimated that at least one-third of cancers are preventable through adequate food and nutrition, physical activity, and maintenance of a healthy body weight [5]. Tobacco smoking causes an estimated 20% of all cancer deaths, with approximately 80% of lung cancer cases in men and 50% in women caused by tobacco smoking globally [5]. Dietary factors are thought to account for ∼30% of cancers in Western countries and approximately 20% in developing countries, making diet second only to tobacco as a preventable cause of cancer. The World Health Organization states that between 7% and 41% of certain cancer burdens are attributable to overweight and obesity [6]. Furthermore, between 9% and 19% of cancer cases in Europe could be linked to insufficient physical activity [7]. Diet and lifestyle (including smoking) account for 90%–95% of cancers, with only ∼5% of cancers due to an inherited gene [8]. In high-income countries, smoking, alcohol use, and overweight and obesity are the most important causes of cancer [4]. Based on a systematic review of >500,000 scientific studies, the World Cancer Research Fund (WCRF) concluded that “avoidance of tobacco in any form, together with appropriate food and nutrition, physical activity, and body composition, have the potential over time to reduce much and perhaps most of the global burden of cancer” [5].
Little is known about the knowledge level or attitudes of members of the public toward their lifetime cancer risk. Several health-promotion campaigns have targeted cardiovascular disease and diabetes through promotion of healthy eating and increased exercise, but few have specifically targeted cancer risk outside of smoking-cessation campaigns. Public perception of risk factors for general cancer risk has never been studied in Ireland before. In the American Institute for Cancer Research’s “fear before facts” survey, U.S. participants rated cancer as their primary health concern; however, they felt that cancer is unpreventable and is caused by factors outside their control [9]. More accurate knowledge is associated with protective health beliefs [10], whereas myths and misconceptions about cancer from inaccurate information can shape health behavior [11]. An understanding of these misconceptions can help shape cancer awareness programs.
The aims of this study were to assess public perception of the risk factors for cancer and to assess myths and misconceptions surrounding cancer risk.
Methods
A 48-question survey was constructed based on a thorough literature review on this topic and through the eight recommendations published in the WCRF report [5]. The survey was split into sections on demographics, diet, lifestyle, and physical activity. In total, the survey consisted of 48 questions about 12 specific diet-related and 14 lifestyle-related risk factors.
The survey was uploaded to SurveyMonkey (http://www.surveymonkey.com) and was live for 6 weeks. Most questions were set up in a manner in which response was compulsory. Participants were recruited by means of social networking sites affiliated with the Irish Cancer Society, Cork Cancer Research Centre, and Breakthrough Cancer Research and by popular Irish online discussion forums. The participants were asked to indicate their educational status and to declare whether or not they were health care professionals (HCPs). After the survey closed, the data were cleaned and coded and transferred to SPSS version 19.0 (IBM Corp., Armonk, NY, http://www-01.ibm.com/software/analytics/spss/) for analysis.
Results
Respondent Characteristics
There were 748 participants (648 women, 100 men). Mean age was 37 years (SD: 19; range: 18–74 years). The audience was educated, with 685 (92%) having completed secondary school education, 233 (31%) possessing an undergraduate degree, and 157 (21%) holding a postgraduate degree. Of the university graduates, 126 (17%) were HCPs. Five percent (n = 39) had received a cancer diagnosis in the previous 5 years.
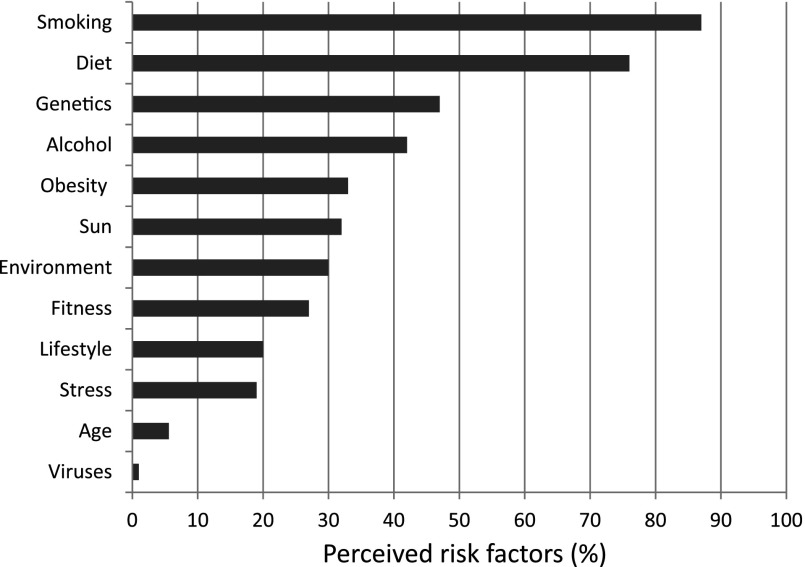
The vast majority of respondents declared they were “worried about developing cancer,” with 81% of the public and 73% of HCPs expressing this concern. Information about cancer was sought out by 79%, with the Internet cited as the resource most frequently used. When asked the question, “True or false: cancer risk increases with age,” 20% of the general public and 10% of HCPs incorrectly answered false. When respondents were asked the open-ended question, “In your opinion, what are the top 5 risk factors for cancer,” a total of 12 different answers were given (Fig. 1). Smoking was the most popular answer (87%), followed by diet (76%), genetics (47%), alcohol (42%), and obesity (32%). Stress was listed as a top five risk factor for 19% of the group, but older age was mentioned by only 6%.
Figure 1.
The top 10 risk factors listed by members of the public (n = 622) in answer to the open-ended question, “In your opinion, what are the top 5 risk factors for cancer?”
Diet
Overall, 92% of subjects agreed with the statement, “Diet has a significant role to play in cancer prevention.” However, when probed on specific aspects of diet, there were large knowledge gaps: 86% knew that processed meat is a risk factor, but 40% of the public and 28% of HCPs were unaware that red meat is a risk factor. Only 46% believed salt to be a risk factor. Although the majority knew that five fruits and vegetables a day are recommended, 33% of the public and 35% of HCPs were unaware that “frozen vegetables are as nutritious as fresh.”
Among members of the public, only 35% believed that “detox” diets reduce risk, but 61% believed that organic food reduces risk; 27% were unaware that breastfeeding can lower breast cancer risk. Moreover, 86% believed in the concept of “cancer-fighting foods,” and when given a list of various foods, the majority thought berries (94%), plant-based foods (81%), citrus fruits (80%), and garlic (66%) were protective. In contrast, the following foods were thought to increase cancer risk: cheese (27%), chocolate (28%), eggs (15%), and soy (7%).
For HCPs, 96% believed that diet plays a role in cancer; however, 28% were not aware of a link with red meat, and 46% did not consider salt intake to be important. Fewer HCPs believed in the concept of cancer-fighting foods (82%), but they considered certain foods to be protective: berries (73%), raw vegetables (72%), green tea (69%), and soy (46%). They also believed that cheese (27%), chocolate (25%), and eggs (5%) increased risk. Vitamin and mineral supplements were perceived as protective against cancer by 51% of the public and 54% of HCPs, with 24% of the public and 20% of HCPs believing that supplements are “absolutely necessary” and should be recommended for cancer prevention.
Genetics
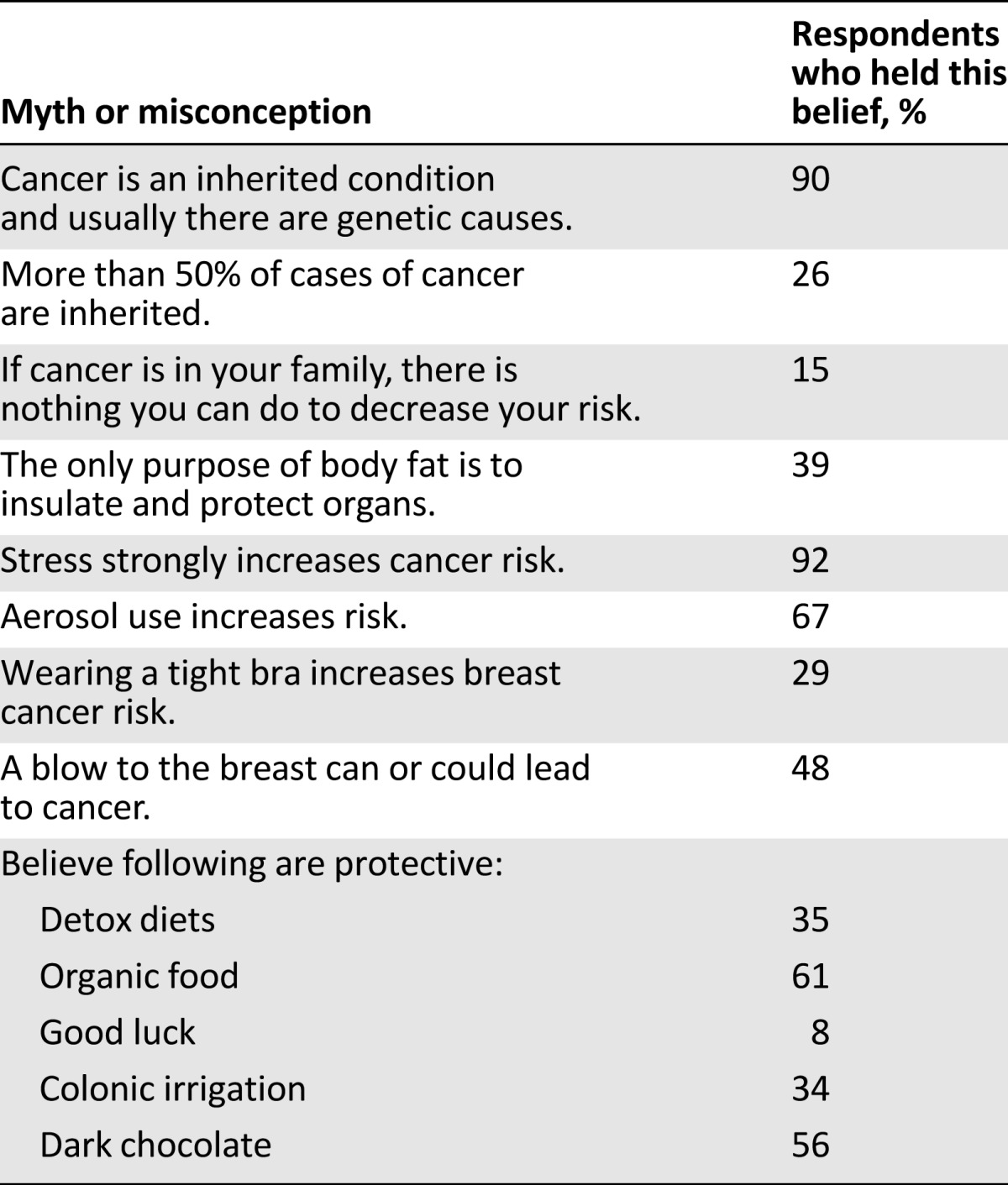
Ninety percent of both groups believed that genetics “strongly” increases risk. Among the general public, 26% believed that >50% of cancers are inherited, and 53% believed that 10%–20% of cancers are inherited. Among HCPs, 10% believed that >50% of cancers were inherited, with 63% believing that 10%–20% of cancers are inherited. Overall, 15% held fatalistic views and believed that if cancer was in their family, there was nothing they could do about their personal risk (Table 1).
Table 1.
Popular myths and misconceptions about cancer risk held by the public
Alcohol
Only 42% of the public and 46% of HCPs were aware that alcohol is a risk factor for cancer. In addition, 63% of the public and 82% of HCPs thought some alcoholic drinks were more dangerous than others, with only 37% aware that all types of alcohol have the same effect. For red wine, 39% thought it was protective, 19% thought it increased risk, and 42% thought it had no effect at all.
Obesity
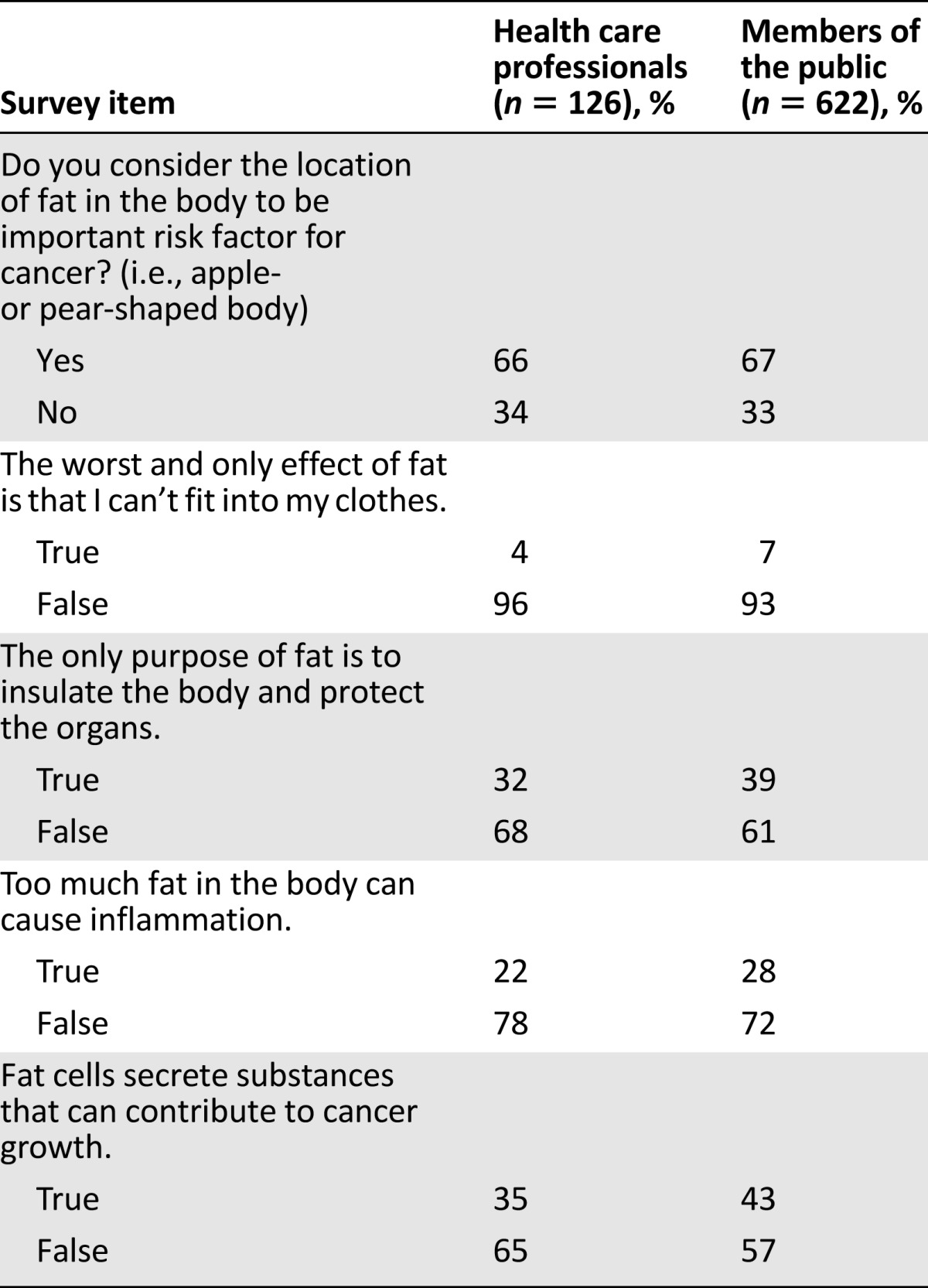
Only 32% of the public and 41% of HCPs were aware that obesity is a risk factor for cancer. Overall, 33% of the public and 34% of HCPs did not think that the location of fat was important (apple vs. pear shaped) (Table 2). In addition, 39% of the public and 32% of HCPs believed that the only purpose of fat in the body was to insulate and protect the organs. Among HCPs, 78% were unaware that excess fat can cause inflammation, and 65% were unaware that fat cells can secrete substances implicated in carcinogenesis. For women, 86% of respondents correctly identified that the desired waist circumference is <32 inches. For men, 81% correctly identified that desired waist circumference is <37 inches.
Table 2.
The effect of adiposity on cancer risk as perceived by subjects
Physical Activity
The vast majority (97% of HCPs and 90% of the public) agreed that remaining physically active throughout life greatly reduces cancer risk. The majority of respondents (69%) interpreted “moderate” physical activity to mean 30 minutes per day. With regard to the number of days that respondents felt it was important to engage in physical activity, the answers were very mixed. Only 24% felt that it was important to engage in physical activity 7 days a week; 25% believed that 1–3 days per week was sufficient, and the remainder (51%) believed that 4–6 days per week was beneficial.
Other Risks and Cancer Myths
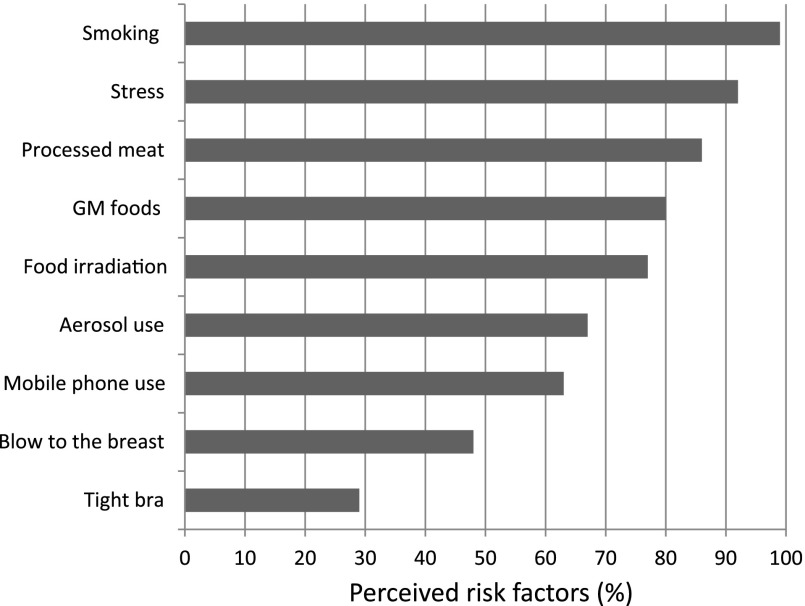
Participants were given a list of potential behaviors and asked to either agree or disagree that they were risk factors for cancer (Fig. 2). Overall, 99% agreed that smoking increased risk. Stress was perceived as a strong risk factor by 92%. The use of aerosols was perceived as important for 67%, and wearing tight underwear was considered important by 29%. Finally, a blow to the breast was perceived as a risk for breast cancer by 48% of respondents. Factors that were believed to be protective against cancer included breastfeeding (63%), detox diets (35%), colonic irrigation (34%), red wine (39%), organic food (61%), dark chocolate (56%), and good luck (8%) (Table 1).
Figure 2.
Illustration of the perceived increased risk of cancer according to factors listed by investigators.
Abbreviation: GM, genetically modified.
Discussion
Cancer-related myths and stigma about cancer are important problems that must be addressed because they present significant challenges to cancer control [12–14]. The new figures and projections of the global cancer burden presented in the World Cancer Report 2014 starkly highlight the problem: the incidence of cancer has increased from 12.7 million in 2008 to 14.1 million in 2012, and this trend is projected to continue, with the number of new cases expected to rise by another 75% [2]. Prevention is central to reducing or reversing the rise in cancer burden, and awareness is the primary strategy to improve cancer prevention and control.
Our findings of low levels of awareness of cancer risk factors among the general population concur with previous research [15–20]. Low awareness of the links among diet, exercise, and cancer likely reflects the short time during which genuinely convincing evidence of these associations has been available [20]. Moreover, until recently, publicity about lifestyle and cancer (except lung cancer) has been limited.
Previous research has shown that the public often believes that nothing can be done to prevent cancer and that cancer is always fatal [14]. As far back as 1986, a national survey in the U.S. found that half of the population believed that “everything causes cancer” and that “there’s not much a person can do to prevent cancer” [21]. Recent findings from a large cross-sectional sample of 6,369 U.S. adults reported that 47% agreed that “it seems like almost everything causes cancer,” 27% agreed that “there’s not much people can do to lower their chances of getting cancer,” and a staggering 71% agreed that “there are so many recommendations about preventing cancer, it’s hard to know which ones to follow” [22, 23]. Stein et al. [23] reported that 25% of a sample of 1,002 U.S. adults believed that “what someone does as a young adult has little effect on their chance of getting cancer later in life.” The present study found that 15% held fatalistic views that if cancer was in their family, “there was nothing a person could do to reduce their own personal cancer risk.” Fatalistic views about cancer prevention may decrease the likelihood of a person engaging in behaviors that reduce cancer incidence or mortality [22].
An overemphasis on the role of genetics as a cause of chronic diseases is not a new phenomenon. Sanderson et al. reported that even in high-risk populations of heart disease, awareness of the role of lifestyle in causation is low [20]. In fact, high-risk populations have tended to have stronger beliefs that hereditary, genetic, or biological factors cause heart disease rather than lifestyles [24, 25]. Carlsson and Strang [26] reported that 49% of control subjects and 43% of cancer patients believed that ≥30% of all types of cancer are heredity. Breslow et al. [16] reported that 70% of a large sample of >12,000 people identified family history as an important risk factor for breast cancer. In the present study, 90% believed that “genes” were a strong etiological factor, and 26% believed that >50% of cancers are inherited. In fact, a relatively small percentage of cancers occur in those with family history, and a much larger percentage are thought to be sporadic.
Previous studies have consistently reported higher levels of awareness among women than men [10, 15–18, 27]. The accuracy of knowledge also appears to increase with higher education attainment [28, 29] and annual household income [10, 28]. Although we did not evaluate knowledge on the basis of income or education in the present study, a large percentage of respondents had completed secondary school education (92%), and 31% had a third-level degree, with 21% holding a postgraduate degree. Further research is necessary to evaluate knowledge among less educated groups because those groups often have higher risks of chronic diseases including cancer.
Epidemiological studies have provided convincing evidence that obesity increases the risk of many cancers and that the association generally follows a dose-response relationship [2]. For an increase in body mass index (BMI) of 10 kg/m2, relative risks are approximately 2.3 for esophageal adenocarcinoma, 1.5 for colon cancer (men), 1.3 for pancreatic cancer (women), 1.4 for postmenopausal breast cancer, 2.9 for endometrial cancer, and 1.5 for kidney cancer [2]. Cancer mortality (all sites combined) is ∼70% higher in people who are extremely obese than in people of normal weight. Estimates for the U.K. for 2007 suggested that ∼40% of cancers of the esophagus (adenocarcinoma), gall bladder (women), and endometrium are attributable to overweight or obesity [30]. Estimates for the U.S. for 1999–2000 suggest that overweight or obesity were responsible for 4.2% and 14.3% of cancer mortality in men and women, respectively, rising to 14.2% and 19.8%, respectively, in men and women who had never smoked [31]. Our study showed that only 32% of respondents were aware of the link between obesity and cancer, and this is similar to findings of other groups. Other studies have reported that between 4% and 39% of the public are aware of the relationship between obesity and cancer [32–34].
In the present study, >90% of respondents recognized that physical activity is important in cancer prevention, and 69% interpreted this to mean 30 minutes of exercise; however, only 24% were aware that this is a daily recommendation. Physical activity can protect against weight gain and obesity [2], but it also reduces the risk of colon and breast cancer and improves survival [35] independent of its effects on BMI. The general recommendation is at least 30–60 minutes of moderate-intensity exercise per day [36].
Environmental pollution with carcinogenic chemicals accounts for 1%–4% of all cancers [2]. The environment was cited by 30% of respondents in this study as a causative factor for cancer. Carlsson and Strang [26] previously reported that subjects suspected environmental toxins to be one of the most important risk factors in cancer development. This agrees with a Greek study in which harmful environmental substances were given a very high ranking [37]. Because people are exposed to hundreds, if not thousands, of chemicals and other agents through their environments, research on this issue is exceedingly complex. Although exposure to carcinogenic chemicals in the environment is a risk factor for cancer, it appears to be more important in certain developing countries and in countries in which indoor air pollution from coal fires is common [2].
Age is the strongest risk factor for most adult cancers including breast, colon and prostate cancers [2]. In the present study, only 6% of participants cited age as a risk factor. Breslow et al. [16] reported a study of 12,035 subjects of whom 75% did not recognize that age is a risk factor for cancer. Wardle et al. [15], in a sample of 3,693 U.K. adults, reported that older age was a little-known risk factor. In a study of 1,556 patients attending general practice in England, just 14% identified age as a risk factor for cancer [38]. More recently, in a population-based telephone interview survey of 19,079 adults in six different countries, Forbes et al. [39] found that awareness of age-related risk was lowest in the U.K. (14%) and highest in Sweden (38%).
Tobacco smoke contains >7,000 chemical compounds, including numerous known carcinogens [2, 40]. In the present study, 98% of participants agreed that smoking was a strong risk factor. This reflects the success of numerous antismoking campaigns funded by the Irish and international communities and the positive impact of the Public Health (Tobacco) Act [41], which made Ireland the first country in the world to institute an outright ban on smoking in workplaces. In addition, in 2013, any tobacco product placed on the Irish market must have graphic warnings, and legislation to introduce plain cigarette packets is currently in preparation. Ireland would be the second country to pass such legislation, after Australia.
In the present study, only 42% of the public were aware that alcohol is a risk factor for cancer, and among those who knew it was a risk factor, only 37% were aware that all types of alcohol have the same effect. These findings are in agreement with other studies, which have shown a low level of awareness [32, 33]. The association between alcohol consumption and risk of cancer has been known since the beginning of the 20th century [2]. The International Agency for Research of Cancer has classified alcohol as a group 1 carcinogen since 1988 [42]. There is now convincing evidence that heavy or regular alcohol consumption increases the risk of developing cancers of the oral cavity, pharynx, larynx, esophagus, liver, breast, colon, and rectum [5, 43]. Alcohol-attributable cancers were estimated to be responsible for 337,400 deaths worldwide, predominantly among men, in 2010. Based on data from 2009, an estimated 3.5% of all cancer deaths in the U.S. (∼19,500 deaths) were alcohol related [44]. Parkin et al. [45] estimated that alcohol is responsible for ∼4% of U.K. cancers (∼12,500 cases) annually. The relationship between alcohol consumption and cancer has been observed as monotonic and without threshold [46, 47]. The effect persists even after cessation of consumption [48]. There appeared to be a large degree of confusion in the present study about the role of red wine in either prevention or causation. Although red wine contains resveratrol, which may have anticancer properties [49], clinical trials in humans have not provided evidence that resveratrol is effective in preventing or treating cancer [50].
The fifth target of the World Cancer Declaration [51] states, “In 2020, public attitudes toward cancer will improve and damaging myths and misconceptions about the disease will be dispelled.” Myths and misconceptions derived from inaccurate information shape health behaviors [11]. Identifying and dispelling myths is critical to the development of health education programs designed to promote protective health behaviors [10]. There is a vast array of mythic causes of cancers including food additives, overhead power lines, pollution, stress, tight underwear, exposure to microwaves, lack of vitamin C and iron in the blood, even bad luck [15, 28, 38, 52]. Such causes are more likely to be reported by men and by people with lower education levels [15]. In several large studies, stress and/or “emotional/mental disturbances” were perceived to be implicated in 27%–67% of cancers [15, 26, 28, 52] and often were given much higher importance than established risk factors [33]. Physical injury and wearing tight underwear are other myths that have been reported previously [23, 26, 52]. In the present study, 48% of respondents believed that physical injury could cause breast cancer, and 29% believed that wearing a tight bra could increase risk. Furthermore, almost 63% believed that use of electronic devices, like mobile phones, could cause cancer. Associations between heavy use of mobile phones and certain brain cancers have been observed, but causal interpretation is controversial; more data are needed, particularly on longer-term use of mobile phones [2].
The limitations of this study include an imbalance of sexes with six times more women than men. However, previous studies have consistently reported higher levels of awareness among women than men [10, 15–18, 27]. Further research on knowledge and attitudes of men is important and would help inform health promotion campaigns. Another limitation is that the majority of respondents were aged <50 years (87%). Consequently it was not feasible to run comparisons between younger (aged <60 years) and older (aged >60 years) groups. A poor knowledge base among our younger adults (aged 20–50 years) is of huge concern because lifestyle choices in these decades of life can significantly affect later cancer risk. Educating people about risky behaviors in youth (sun exposure, known carcinogens) and encouraging younger people to sustain preventative behaviors over the long time periods necessary for primary prevention of cancer (e.g., avoidance of weight gain, physical activity, healthy eating) could potentially have a greater impact on cancer rates than the education of older adults alone (aged >60 years). Even simple measures like encouraging every adult to reduce BMI by 1% could lower the increase in the number of cancer cases and actually result in the avoidance of ∼100,000 new cases of cancer [53].
Conclusion
Preventing cancer by avoiding exposure to particular carcinogens follows from knowledge of causation [20]. Many causes of cancer are modifiable, and it is widely agreed that changes in behavior could prevent many cancers [15]. Although age is not modifiable, awareness could promote appropriate consultation.
The results of the present study demonstrate that Irish adults have poor awareness of established risk factors for cancer, in line with research in other countries [15, 20, 33, 38, 54]. Furthermore a sizable portion of the Irish population is misinformed about cancer risk. Many participants were aware of classic risk factors (e.g., smoking, diet), but many overestimated risk attributable to genetics, environment, and stress and underestimated age, obesity, and sunlight. Fifteen percent held fatalistic views that risk of cancer is not modifiable. Because health beliefs are strong determinants of health behaviors, these data have big implications for the promotion of cancer awareness. Targeted health-promotion campaigns that lead to better understanding of risk factors and increased prevention efforts will offer cost-effective and sustainable means of reducing the global cancer burden in the long term.
Acknowledgments
There was no funding source for this study. The study was performed in conjunction with the Irish Cancer Society and Breakthrough Cancer Research in Ireland.
Footnotes
For Further Reading: Electra D. Paskett, James L. Fisher, Eugene J. Lengerich. Disparities in Underserved White Populations: The Case of Cancer-Related Disparities in Appalachia. The Oncologist 2011;16:1072–1081.
Abstract: There are meaningful cancer-related disparities in the Appalachian region of the U.S. To address these disparities, the Appalachia Community Cancer Network (ACCN), a collaboration of investigators and community partners in five states (Kentucky, Ohio, Pennsylvania, Virginia, and West Virginia), is involved in increasing cancer education and awareness, conducting community-based participatory research (CBPR), and creating mentorship and training opportunities. The primary objective of this paper is to describe cancer-related disparities in the Appalachian region of the U.S. as an example of the disparities experienced by underserved, predominantly white, rural populations, and to describe ACCN activities designed to intervene regarding these disparities. An ACCN overview/history and the diverse activities of ACCN-participating states are presented in an effort to suggest potential useful strategies for working to reduce health-related disparities in underserved white populations. Strengths that have emerged from the ACCN approach (e.g., innovative collaborations, long-standing established networks) and remaining challenges (e.g., difficulties with continually changing communities, scarce resources) are described. Important recommendations that have emerged from the ACCN are also presented, including the value of allowing communities to lead CBPR efforts. Characteristics of the community-based work of the ACCN provide a framework for reducing health-related disparities in Appalachia and in other underserved white and rural populations.
Author Contributions
Conception/Design: Aoife M. Ryan
Provision of study material or patients: Aoife M. Ryan, Derek G. Power
Collection and/or assembly of data: Aoife M. Ryan, Lisa Burns, Ursula Kenny
Data analysis and interpretation: Aoife M. Ryan, Samantha Cushen, Harriët Schellekens, Eadaoin Ni Bhuachalla, Derek G. Power
Manuscript writing: Aoife M. Ryan, Samantha Cushen, Harriët Schellekens, Eadaoin Ni Bhuachalla, Derek G. Power
Final approval of manuscript: Aoife M. Ryan, Samantha Cushen, Harriët Schellekens, Eadaoin Ni Bhuachalla, Derek G. Power
Disclosures
The authors indicated no financial relationships.
References
- 1.Jemal A, Bray F, Center MM, et al. Global cancer statistics. CA Cancer J Clin. 2011;61:69–90. doi: 10.3322/caac.20107. [DOI] [PubMed] [Google Scholar]
- 2.Steward BW, Wild CP, editors. World Cancer Report 2014. Lyon, France: International Agency for Research on Cancer; 2014. [PubMed] [Google Scholar]
- 3. National Cancer Registry Ireland. Available at http://www.ncri.ie. Accessed July 21, 2014.
- 4.Danaei G, Vander Hoorn S, Lopez AD, et al. Causes of cancer in the world: Comparative risk assessment of nine behavioural and environmental risk factors. Lancet. 2005;366:1784–1793. doi: 10.1016/S0140-6736(05)67725-2. [DOI] [PubMed] [Google Scholar]
- 5.The Second Expert Report: Food, Nutrition, Physical Activity and the Prevention of Cancer: A Global Perspective. Washington, DC: American Institute for Cancer Research; 2007. [DOI] [PubMed] [Google Scholar]
- 6.Cancer Control: Knowledge Into Action. WHO Guide for Effective Programmes. Geneva, Switzerland: World Health Organization; 2007. [PubMed] [Google Scholar]
- 7.Friedenreich CM, Neilson HK, Lynch BM. State of the epidemiological evidence on physical activity and cancer prevention. Eur J Cancer. 2010;46:2593–2604. doi: 10.1016/j.ejca.2010.07.028. [DOI] [PubMed] [Google Scholar]
- 8.Anand P, Kunnumakkara AB, Sundaram C, et al. Cancer is a preventable disease that requires major lifestyle changes. Pharm Res. 2008;25:2097–2116. doi: 10.1007/s11095-008-9661-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. AICR survey uncovers distorted perceptions about what causes cancer [press release]. Available at http://preventcancer.aicr.org/site/News2?page=NewsArticle&id=12900&news_iv_ctrl=0&abbr=pr_. Accessed July 21, 2014.
- 10.Wilkinson AV, Vasudevan V, Honn SE, et al. Sociodemographic characteristics, health beliefs, and the accuracy of cancer knowledge. J Cancer Educ. 2009;24:58–64. doi: 10.1080/08858190802664834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gansler T, Henley SJ, Stein K, et al. Sociodemographic determinants of cancer treatment health literacy. Cancer. 2005;104:653–660. doi: 10.1002/cncr.21194. [DOI] [PubMed] [Google Scholar]
- 12.Keusch GT, Wilentz J, Kleinman A. Stigma and global health: Developing a research agenda. Lancet. 2006;367:525–527. doi: 10.1016/S0140-6736(06)68183-X. [DOI] [PubMed] [Google Scholar]
- 13.Link BG, Phelan JC. Stigma and its public health implications. Lancet. 2006;367:528–529. doi: 10.1016/S0140-6736(06)68184-1. [DOI] [PubMed] [Google Scholar]
- 14.Daher M. Cultural beliefs and values in cancer patients. Ann Oncol. 2012;23(suppl 3):66–69. doi: 10.1093/annonc/mds091. [DOI] [PubMed] [Google Scholar]
- 15.Wardle J, Waller J, Brunswick N, et al. Awareness of risk factors for cancer among British adults. Public Health. 2001;115:173–174. doi: 10.1038/sj/ph/1900752. [DOI] [PubMed] [Google Scholar]
- 16.Breslow RA, Sorkin JD, Frey CM, et al. Americans’ knowledge of cancer risk and survival. Prev Med. 1997;26:170–177. doi: 10.1006/pmed.1996.0136. [DOI] [PubMed] [Google Scholar]
- 17.Brunswick N, Wardle J, Jarvis MJ. Public awareness of warning signs for cancer in Britain. Cancer Causes Control. 2001;12:33–37. doi: 10.1023/a:1008975416756. [DOI] [PubMed] [Google Scholar]
- 18.McCaffery K, Wardle J, Waller J. Knowledge, attitudes, and behavioral intentions in relation to the early detection of colorectal cancer in the United Kingdom. Prev Med. 2003;36:525–535. doi: 10.1016/s0091-7435(03)00016-1. [DOI] [PubMed] [Google Scholar]
- 19.Waller J, McCaffery K, Wardle J. Beliefs about the risk factors for cervical cancer in a British population. Prev Med. 2004;38:745–753. doi: 10.1016/j.ypmed.2004.01.003. [DOI] [PubMed] [Google Scholar]
- 20.Sanderson SC, Waller J, Jarvis MJ, et al. Awareness of lifestyle risk factors for cancer and heart disease among adults in the UK. Patient Educ Couns. 2009;74:221–227. doi: 10.1016/j.pec.2008.08.003. [DOI] [PubMed] [Google Scholar]
- 21.Technical Report: Cancer Prevention Awareness Survey, Wave II. Bethesda, MD: National Cancer Institute; 1986. [Google Scholar]
- 22.Niedereppe J, Levy AG. Fatalistic beliefs about cancer prevention and three prevention behaviours. Cancer Epidemiol Biomarkers Prev. 2007;16:998–1003. doi: 10.1158/1055-9965.EPI-06-0608. [DOI] [PubMed] [Google Scholar]
- 23.Stein K, Zhao L, Crammer C, et al. Prevalence and sociodemographic correlates of beliefs regarding cancer risks. Cancer. 2007;110:1139–1148. doi: 10.1002/cncr.22880. [DOI] [PubMed] [Google Scholar]
- 24.Byrne M, Walsh J, Murphy AW. Secondary prevention of coronary heart disease: Patient beliefs and health-related behaviour. J Psychosom Res. 2005;58:403–415. doi: 10.1016/j.jpsychores.2004.11.010. [DOI] [PubMed] [Google Scholar]
- 25.Senior V, Marteau TM, Weinman J. Perception of control over heart disease in people with an inherited predisposition to raised cholesterol. Psychol Health Med. 2005;10:16–30. [Google Scholar]
- 26.Carlsson ME, Strang PM. Facts, misconceptions, and myths about cancer. What do patients with gynecological cancer and the female public at large know? Gynecol Oncol. 1997;65:46–53. doi: 10.1006/gyno.1997.4626. [DOI] [PubMed] [Google Scholar]
- 27.Yardley C, Glover C, Allen-Mersh TG. Demographic factors associated with knowledge of colorectal cancer symptoms in a UK population-based survey. Ann R Coll Surg Engl. 2000;82:205–209. [PMC free article] [PubMed] [Google Scholar]
- 28.McMenamin M, Barry H, Lennon AM, et al. A survey of breast cancer awareness and knowledge in a Western population: Lots of light but little illumination. Eur J Cancer. 2005;41:393–397. doi: 10.1016/j.ejca.2004.11.015. [DOI] [PubMed] [Google Scholar]
- 29.Sim HL, Seah M, Tan SM. Breast cancer knowledge and screening practices: A survey of 1,000 Asian women. Singapore Med J. 2009;50:132–138. [PubMed] [Google Scholar]
- 30.Key TJ, Spencer EA, Reeves GK. Symposium 1: Overnutrition: Consequences and solutions. Obesity and cancer risk. Proc Nutr Soc. 2010;69:86–90. doi: 10.1017/S0029665109991698. [DOI] [PubMed] [Google Scholar]
- 31.Calle EE, Rodriguez C, Walker-Thurmond K, et al. Overweight, obesity, and mortality from cancer in a prospectively studied cohort of U.S. adults. N Engl J Med. 2003;348:1625–1638. doi: 10.1056/NEJMoa021423. [DOI] [PubMed] [Google Scholar]
- 32.Ong CS, Ooi G, Tan XQ, et al. Prevalence of limited cancer knowledge in Singaporeans, its determinants and association with cancer screening. Prev Med. 2010;50:304–305. doi: 10.1016/j.ypmed.2010.02.013. [DOI] [PubMed] [Google Scholar]
- 33.Peacey V, Steptoe A, Davídsdóttir S, et al. Low levels of breast cancer risk awareness in young women: An international survey. Eur J Cancer. 2006;42:2585–2589. doi: 10.1016/j.ejca.2006.03.017. [DOI] [PubMed] [Google Scholar]
- 34.Hwang LL. Cancer awareness changes after an educational intervention among undergraduate students. J Cancer Educ. 2013;28:247–253. doi: 10.1007/s13187-013-0461-5. [DOI] [PubMed] [Google Scholar]
- 35.Holmes MD, Chen WY, Feskanich D, et al. Physical activity and survival after breast cancer diagnosis. JAMA. 2005;293:2479–2486. doi: 10.1001/jama.293.20.2479. [DOI] [PubMed] [Google Scholar]
- 36. Physical activity and health: A report of the Surgeon General. Available at http://www.cdc.gov/nccdphp/sgr/sgr.htm. Accessed April 16, 2014.
- 37.Makris G, Charalampopoulos KA, Athanasiou K. Estimating the level of knowledge of Greek students on cancer aetiology and ways of prevention. Eur J Cancer Prev. 1994;3:443–450. doi: 10.1097/00008469-199409000-00009. [DOI] [PubMed] [Google Scholar]
- 38.Knowles J, Hamilton W. Knowledge of risk factors in cancer. Br J Gen Pract. 2008;58:650–651. doi: 10.3399/bjgp08X342039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Forbes LJL, Simon AE, Warburton F, et al. Differences in cancer awareness and beliefs between Australia, Canada, Denmark, Norway, Sweden and the UK (the International Cancer Benchmarking Partnership): Do they contribute to differences in cancer survival? Br J Cancer. 2013;108:292–300. doi: 10.1038/bjc.2012.542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.The Health Consequences of Smoking: A Report of the Surgeon General. Atlanta, GA: Centers for Disease Control and Prevention; 2004. [PubMed] [Google Scholar]
- 41. S.I. No. 110/2004 - Public Health (Tobacco) Act 2002 (Commencement) Order 2004. Available at http://www.irishstatutebook.ie/2004/en/si/0110.html. Accessed July 21, 2014.
- 42.Lyon, France: International Agency for Research on Cancer; 1988. IARC Monographs on the Evaluation of Carcinogenic Risks to Humans: Alcohol Drinking. Vol 44. [Google Scholar]
- 43.Boyle P, Autier P, Bartelink H, et al. European Code Against Cancer and scientific justification: Third version (2003) Ann Oncol. 2003;14:973–1005. doi: 10.1093/annonc/mdg305. [DOI] [PubMed] [Google Scholar]
- 44.Nelson DE, Jarman DW, Rehm J, et al. Alcohol-attributable cancer deaths and years of potential life lost in the United States. Am J Public Health. 2013;103:641–648. doi: 10.2105/AJPH.2012.301199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Parkin DM. 3. Cancers attributable to consumption of alcohol in the UK in 2010. Br J Cancer. 2011;105(suppl 2):S14–S18. doi: 10.1038/bjc.2011.476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lyon, France: International Agency for Research on Cancer; 2010. IARC Monographs on the Evaluation of Carcinogenic Risks to Humans: Alcohol Consumption and Ethyl Carbamate. Vol 96. [PMC free article] [PubMed] [Google Scholar]
- 47.Lyon, France: International Agency for Research on Cancer; 2012. IARC Monographs on the Evaluation of Carcinogenic Risks to Humans: Personal Habits and Indoor Combustions. Vol 100E. [PMC free article] [PubMed] [Google Scholar]
- 48.Rehm J, Patra J, Popova S. Alcohol drinking cessation and its effect on esophageal and head and neck cancers: A pooled analysis. Int J Cancer. 2007;121:1132–1137. doi: 10.1002/ijc.22798. [DOI] [PubMed] [Google Scholar]
- 49.Athar M, Back JH, Tang X, et al. Resveratrol: A review of preclinical studies for human cancer prevention. Toxicol Appl Pharmacol. 2007;224:274–283. doi: 10.1016/j.taap.2006.12.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Patel KR, Scott E, Brown VA, et al. Clinical trials of resveratrol. Ann N Y Acad Sci. 2011;1215:161–169. doi: 10.1111/j.1749-6632.2010.05853.x. [DOI] [PubMed] [Google Scholar]
- 51.Cavalli F. The World Cancer Declaration: A roadmap for change. Lancet Oncol. 2008;9:810–811. doi: 10.1016/S1470-2045(08)70213-4. [DOI] [PubMed] [Google Scholar]
- 52.Grunfeld EA, Ramirez AJ, Hunter MS, et al. Women’s knowledge and beliefs regarding breast cancer. Br J Cancer. 2002;86:1373–1378. doi: 10.1038/sj.bjc.6600260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Wang YC, McPherson K, Marsh T, et al. Health and economic burden of the projected obesity trends in the USA and the UK. Lancet. 2011;378:815–825. doi: 10.1016/S0140-6736(11)60814-3. [DOI] [PubMed] [Google Scholar]
- 54.Adlard JW, Hume MJ. Cancer knowledge of the general public in the United Kingdom: Survey in a primary care setting and review of the literature. Clin Oncol (R Coll Radiol) 2003;15:174–180. doi: 10.1016/s0936-6555(02)00416-8. [DOI] [PubMed] [Google Scholar]