Abstract
When approaching a case with a situs abnormality, using the proper terminology, making a specific diagnosis, and understanding the other often associated abnormalities that need to be excluded are of great importance. We present a case of situs ambiguous in the presence of intestinal nonrotation and an obstructing duodenal web. Our patient initially presented at two days old with bilious emesis and failure to pass meconium after birth. An abdominal radiograph demonstrated an unusual bowel gas pattern, a reversed “double bubble” sign. A subsequent thorough imaging survey was crucial to further characterize our patient’s unique anatomy. Overall, our case demonstrates many of the unusual plain radiographic and sonographic findings associated with our patient’s situs abnormality and allows for review of situs abnormalities and their significance.
Keywords: Situs solitus totalis, Situs ambiguous, Heterotaxy, Isolated levocardia, Double-bubble
CASE REPORT
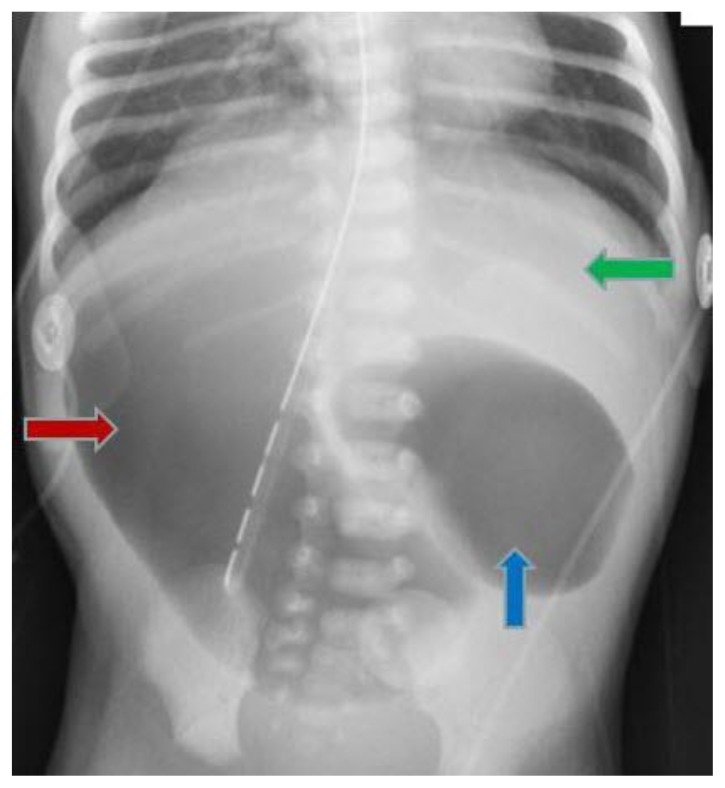
A newborn female, born at 35.5 weeks gestation via spontaneous vaginal delivery to a G4P3 mother who had poor prenatal care, underwent abdominal radiographs at 48 hours of life because of absent stooling and episodes of bilious emesis. Abdominal radiographs showed a reverse “double bubble” sign, with the stomach on the right and the liver on the left (Figures 1–4). An echocardiogram showed a patent foramen ovale, without evidence of other structural or congenital heart disease.
Figure 1.
Newborn female with situs ambiguous, levocardia, right-sided stomach, obstructing duodenal web, and intestinal nonrotation. Portable supine anterior-posterior radiograph showing a reverse “double bubble,” the stomach is in the right upper quadrant (block red arrow) and duodenum (block blue arrow) in the left upper quadrant.
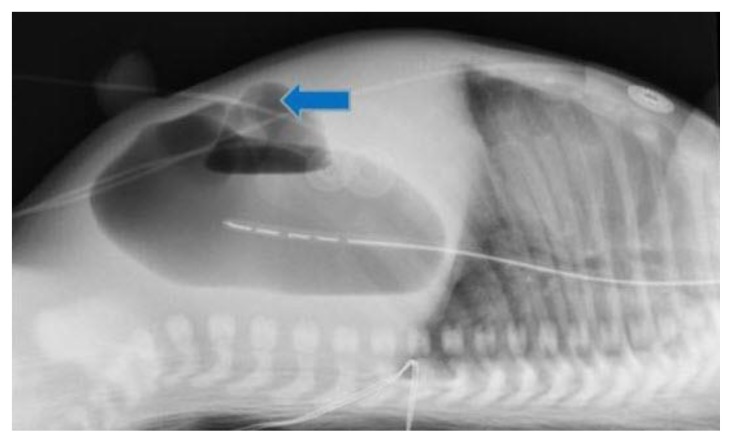
Figure 4.
Newborn female with situs ambiguous, levocardia, right-sided stomach, obstructing duodenal web, and intestinal nonrotation. Left lateral recumbent radiograph showing enteric tube in the stomach, located in right upper quadrant and duodenum in the left upper quadrant (block blue arrow).
An exploratory laparotomy was performed to further assess the cause of the proximal small bowel obstruction demonstrated radiographically, relieve the obstruction, and, given the concern for a situs abnormality raised on the initial abdominal radiographs, attempt to assess the exact locations of the solid and visceral organs of the abdominopelvic cavity. A completely obstructing duodenal web was resected, relieving the bowel obstruction, with a primary anastomosis of the separated ends. The distal bowel and the entire small bowel were insufflated with air, without any evidence of a more distal atresia (Figure 5). Intraoperatively, the duodenal sweep was found to be toward the left and the stomach was seen on the right. The small bowel was located within the right side of the abdomen, and the colon in the left hemiabdomen, consistent with intestinal nonrotation. The appendix was removed, because of its atypical location in the left lower quadrant. The spleen was not visualized during the surgery.
Figure 5.
Newborn female with situs ambiguous, levocardia, right-sided stomach, obstructing duodenal web, and intestinal nonrotation. Postoperative radiograph demonstrates lower gastrointestinal gas (block blue arrow). Enteric tube is in the stomach.
Imaging Findings
Abdominal radiographs were obtained and showed the “double bubble” sign (Figures 1–4), with the stomach on the right and the duodenum in the left hemi-abdomen. A complete abdominal ultrasound was performed to better characterize the intra-abdominopelvic anatomy. This study demonstrated the bulk of the liver in the left upper quadrant (Figure 6). The aorta was to the left of the Inferior Vena Cava (IVC). The stomach was located in the right upper quadrant. The pancreas and kidneys were normal. The spleen was initially equivocally identified in the abdominopelvic right upper quadrant. There was concern about the definite presence and location of a spleen, a limited abdominal ultrasound exam was performed the next day. The limited abdominal ultrasound verified the presence of a spleen, with a 3.4 cm spleen seen in the right upper quadrant (Figures 7–8).
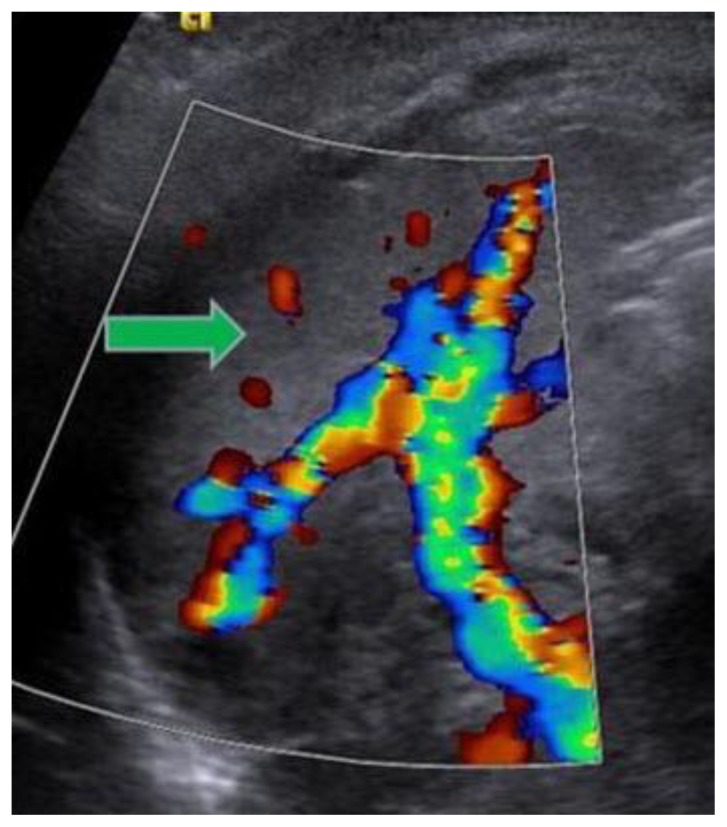
Figure 6.
Newborn female with situs ambiguous, levocardia, right-sided stomach, obstructing duodenal web, and intestinal nonrotation. Postoperative transverse grayscale sonographic image demonstrates normal liver parenchyma (block red arrow) in the left upper quadrant.
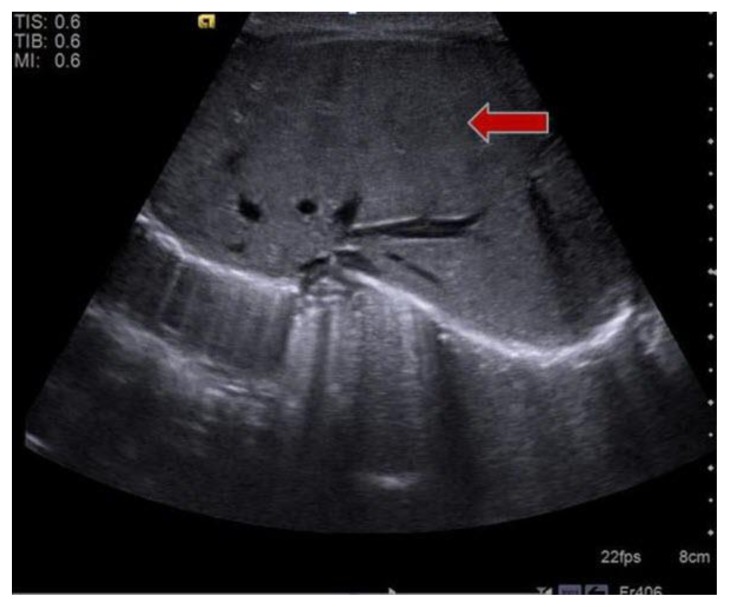
Figure 7.
Newborn female with situs ambiguous, levocardia, right-sided stomach, obstructing duodenal web, and intestinal nonrotation. Postoperative transverse grayscale sonographic image shows normal internal architecture of the spleen (block red arrow) in the right upper quadrant.
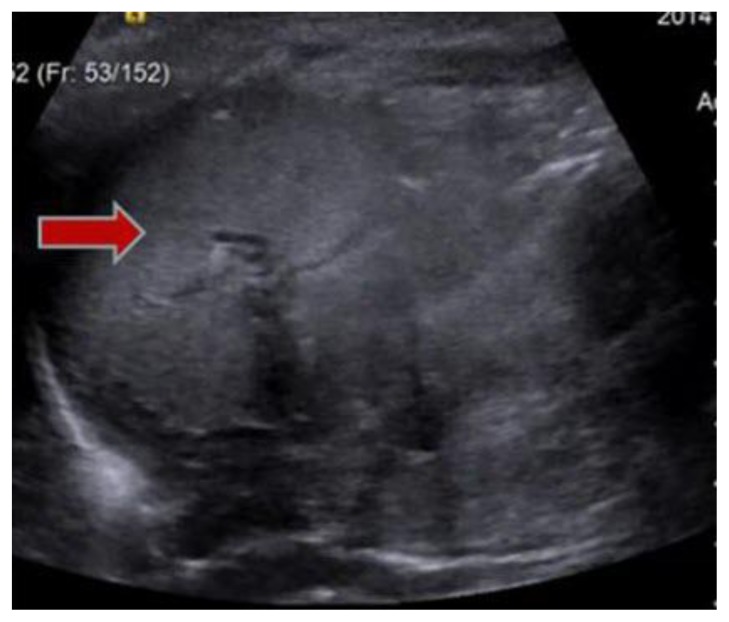
Figure 8.
Newborn female with situs ambiguous, levocardia, right-sided stomach, obstructing duodenal web, and intestinal nonrotation. Postoperative transverse grayscale sonographic image, with superimposed Doppler color flow imaging shows the spleen (block green arrow) in the right upper quadrant. Vascular flow is demonstrated in the hilum.
Follow-up
Following the operative repair of the patient’s proximal small bowel obstruction, the patient did well, without a further major medical problem. No follow-up imaging was recommended.
DISCUSSION
Etiology and demographics
Situs solitus totalis (with levocardia) is the normal anatomic state, seen in the vast majority of births, with the right atrium receiving systemic venous blood on the right. There is a right-sided trilobed lung, right liver, and gallbladder. Furthermore, in patients with levocardia, the cardiac apex is pointed to the left. Situs solitus with dextrocardia (right sided cardiac apex) has an incidence of 1:29,000 and is due to failure of shift of the cardiac apex to the left [1]. Situs inversus totalis is the mirror image of situs solitus totalis, with an incidence of 1:8,000 newborn births. Of these, 20% have Kartagener syndrome, a genetically heterogeneous disorder also known as immotile cilia syndrome [2].
Situs Inversus with Isolated Levocardia, or simply Isolated Levocardia (ILC), is rare, with an incidence of 1:22,000, and refers to a normal cardiac situs with the cardiac apex in the left hemithorax, in the presence of an aberrant arrangement of the abdominal organs [3, 4]. In ILC, the anomalous IVC and right atrium are often located on opposite sides of midline due to the discordant location of the venous atria and the abdominal viscera; thus, requiring the IVC cross the midline to join the heart, which often occurs via azygos vein or hemiazygos vein continuation [5].
Situs ambiguous, or heterotaxy syndrome, refers to an abnormal positioning of internal organs relative to the normal. There have been no specific risk factors identified, and it is thought that the underlying etiology of these abnormalities is a primary defect in lateralization around day 28 of gestation, which leads to a deviation from the normal position of viscera [5]. Such arrangements are thought to be multifactorial in their inheritance pattern, and the co-incidence of aneuploidy or other chromosomal abnormalities is very low [6]. Heterotaxy syndromes have an incidence of 1:10,000 newborn births but account for about 4% of all congenital heart disease (CHD) [6]. Situs ambiguous is traditionally divided into two general categories: left isomerism (situs ambiguous with polysplenia) and right isomerism (situs ambiguous with asplenia).
Left isomerism, or situs ambiguous with polysplenia, has an incidence of between 1:10,000 and 1:20,000 newborn births and a female predominance [7]. It often comes to medical attention because of a suspected heart defect, as the coincidence of CHD is between 50 and 90%. Commonly associated cardiac malformations include partial anomalous pulmonary venous return, atrial septal defect (ASD), and a common atrioventricular (AV) canal [5]. Although the term polysplenia is used, the number of spleens ranges from one to ten or more; spleens may be located either bilaterally or, if unilateral, ipsilateral to the stomach, due to the fact that the spleen arises from the dorsal mesogastrium [5]. Another common finding is IVC interruption with azygos or hemiazygos continuation; this has been reported to be the most specific finding of situs ambiguous with polysplenia [5]. In keeping with the term “left isomerism,” the lungs are bilaterally bilobed with hyparterial bronchi.
Right isomerism, or situs ambiguous with asplenia, has an incidence of between 1:10,000 and 1:20,000 newborn births and has a male predominance, and has a very high incidence of CHD (nearly 100%) and thus, often presents in childhood with a cyanotic heart defect such as a common AV canal, univentricular heart, transposition of the great arteries, or total anomalous pulmonary venous return [5, 7, 8]. In contrast to left isomerism, the spleen is absent, the IVC typically runs ipsilateral to the aorta, and the patient will have bilateral trilobed lungs with eparterial bronchi [5].
Intestinal malrotation, including cases of nonrotation, is seen in 1:500 births and is associated with both situs ambiguous syndromes in approximately 70% of cases [9, 10, 11]. It arises from a failure of 270-degree counterclockwise rotation around the superior mesenteric artery. Complete duodenal obstruction by a duodenal web, found in 1:10,000 to 1:40,000 births, likely results from failure of gut recanalization during the ninth to eleventh weeks of gestation [9]. Symptomatic patients often present with bilious emesis, absent stooling, and a “double bubble” sign on abdominal radiographs. Karyotype analysis is often warranted in any form of complete duodenal obstruction, as 30% of patients with duodenal atresia also have Trisomy 21 or Down syndrome [12].
Clinical and imaging findings
Patients with heterotaxy syndromes present in a number of ways due to the wide spectrum of anatomic abnormalities that may be present. Unlike situs inversus totalis, a more benign arrangement that often is discovered in adulthood because of its relatively few associated abnormalities, the anatomy of situs ambiguous does not follow a specific pattern. Because most patients will not fit neatly into one of the two categories outlined above, it is thought that asplenia and polysplenia are two ends of a spectrum, with many patients falling somewhere in between, and that the specific individual abnormalities should be stated in the diagnosis, rather than simply using the terms left isomerism or polysplenia and right sided isomerism or asplenia.
A thorough imaging survey is essential for patients to have their unique anatomy classified. Interpreting such studies requires a meticulous segmental approach to delineate all abnormalities. A common initial finding on a chest radiograph is the presence of the heart and the stomach located on opposite sites of the body; such a finding, as in our case, necessitates further imaging and evaluation. It is recommended that several critical structures be evaluated by the radiologist: position of the cardiac apex and atria, position of aorta and venous drainage below the diaphragm relative to midline, position of the stomach and presence or absence of malrotation, position of the liver and gallbladder, presence and number of spleens, and presence of tri- or bilobed lungs [5]. Describing all of these, when possible, will aid in classifying the patient’s anatomy on the situs ambiguous spectrum and allow for more timely and targeted therapeutic interventions.
Treatment and prognosis
Congenital heart disease is one of the major causes of morbidity and mortality in patients with situs abnormalities and its incidence can be predicted when the patient’s situs is known. Specifically, the incidence of CHD in patients with situs solitus totalis (with levocardia) is very low (0.6–0.8 %) [5]. However, patients with situs solitus and dextrocardia have a very high incidence of CHD, reported as greater than 90% [5]. The most common types of CHD seen in patients with situs solitus and dextrocardia are tricuspid atresia and pulmonic stenosis [8]. In patients with situs inversus totalis, the incidence of CHD is relatively low at 3–5 % [5, 13]. Conversely, situs inversus with levocardia is accompanied by CHD in greater than 90% of patients [8]. Therefore, excluding situs ambiguous (discussed below), a simplified way of thinking about the likelihood of CHD in a patient with a situs abnormality is to see if the stomach and cardiac apex are on the same side of the body. If the stomach and cardiac apex are on the same side of the body, the risk of associated CHD is relatively low, whereas if the stomach and cardiac apex are on opposite sides of the body, the risk of associated CHD is relatively high. This is because the severity of congenital heart disease is proportional to the failure of cardiac shift with respect to the cardiac situs within the thorax [8, 13].
The incidence of CHD in patients with situs ambiguous depends upon whether the situs ambiguous syndrome can be further sub-classified as either right-sided isomerism (situs ambiguous with asplenia) or left-sided isomerism (situs ambiguous with polysplenia), both of which have a relatively high incidence of associated CHD. Patients with right-sided isomerism have a very high incidence of CHD (nearly 100%) and patients with left isomerism have a high incidence of CHD (50%–90%) [13].
Approximately 20% of patients with situs inversus will also have Kartagener syndrome. Kartagener syndrome is a subtype of primary ciliary dyskinesia, presenting with a triad of situs inversus, nasal polyposis with chronic sinusitis, and bronchiectasis [2]. This syndrome is also associated with male infertility, most likely also to an abnormality in number or function of the dynein arms of spermatozoa.
Another consideration in patients found to have situs ambiguous with asplenia is the risk of severe sepsis secondary to the absence of spleen-mediated immunity. Absence of the spleen can often be detected early with abdominal ultrasound. Because of the risk of overwhelming sepsis caused by encapsulated bacteria, such as Streptococcus pneumoniae, Haemophilus influenzae type B, and Neisseria meningitidis, early vaccinations against these specific pathogens are recommended.
While situs abnormalities in adults may not cause symptoms, they can cause confusing presentations of otherwise common conditions. In particular, appendicitis, cholecystitis, and splenic infarction can be a diagnostic dilemma in the absence of imaging because of the altered anatomy [14].
Differential Diagnoses
1. Situs ambiguous
As in our case, patients with generalized situs ambiguous present with an abnormal arrangement of thoracoabdominal organs that does not follow a specific pattern. More specifically, cardiac looping is often affected, and the abdominal organs may be frankly reversed or arranged in a more unusual fashion, such as in the midline or bilaterally symmetric. Commonly associated findings are intestinal malrotation, abnormal venous drainage patterns, and congenital heart disease.
a) Situs ambiguous with asplenia (right isomerism)
While this does present with discordant location of the abdominal viscera relative to the cardiac situs, several other findings are characteristically present. The most specific has been reported to be the common path of the IVC with the aorta to the left of the spine. Of course, absence of the spleen and bilateral trilobed lungs with eparterial bronchi are also characteristic. Our patient had a spleen and therefore, this is not the correct diagnosis for our patient.
b) Situs ambiguous with polysplenia (left isomerism)
While this also presents with discordant location of the abdominal viscera relative to the cardiac situs, the most specific finding has been reported to be IVC interruption with azygos or hemiazygos continuation. At least one spleen is present, although its location is variable. Bilateral bilobed lungs with hyparterial bronchi are also typically found. Our patient’s imaging demonstrated no evidence of IVC interruption or bilateral bilobed lungs to suggest this diagnosis.
2. Situs inversus totalis
In situs inversus totalis, the organs are arranged in a complete mirror-image configuration to the normal situs solitus. Thus, the cardiac apex would be dextroverted with a corresponding right-sided stomach and left-sided liver. Besides a mirror-image arrangement, no specific abnormalities of venous drainage would be noted. The right lung would be bilobed, and the left lung would be trilobed. This diagnosis would be incorrect for our patient because her stomach and cardiac apex are on opposite sides of her body, whereas in situs inversus totalis the cardiac apex and stomach would both be on the patient’s right.
TEACHING POINT
Situs ambiguous describes an abnormal position of the thoracoabdominal organs and can be categorized between two extremes; right-sided isomerism with asplenia and left sided isomerism with polysplenia. Situs ambiguous describes a wide range of possible anatomic arrangements which are associated with different likelihoods of coexistent congenital heart disease. Therefore, a detailed imaging survey should be undertaken to delineate a patient’s particular anatomy.
Figure 2.
Newborn female with situs ambiguous, levocardia, right-sided stomach, obstructing duodenal web, and intestinal nonrotation. Portable supine anterior-posterior radiograph obtained after enteric tube placement in the stomach. Stomach in right upper quadrant (block red arrow) and duodenum (block blue arrow) in left upper quadrant. Liver is in left upper quadrant (block green arrow).
Figure 3.
Newborn female with situs ambiguous, levocardia, right-sided stomach, obstructing duodenal web, and intestinal nonrotation. Crosstable lateral radiograph demonstrates no free air. Enteric tube is in the stomach. The block blue arrow points the duodenum.
Table 1.
Summary table of major features of the situs ambiguous subtypes.
| Situs Ambiguous | Situs ambiguous with polysplenia (left isomerism) | Situs ambiguous with asplenia (right isomerism) |
|---|---|---|
| Etiology | Sporadic defect in body lateralization around day 28 of gestation | Sporadic defect in body lateralization around day 28 of gestation |
| Incidence | Between 1:10,000 and 1:20,000 | Between 1:10,000 and 1:20,000 |
| Gender ratio | 2:1 female ratio | 2:1 male ratio |
| Age predilection | Congenital aberration seen at birth, but may be diagnosed in infancy or later in life depending on patient’s need for imaging | Congenital aberration seen at birth, but may be diagnosed in infancy or later in life depending on patient’s need for imaging |
| Risk factors | No known risk factors | No known risk factors |
| Treatment | None if patient truly has isolated levocardia. Surgery if cyanotic heart lesion present | None if patient truly has isolated levocardia. Surgery if cyanotic heart lesion present; vaccination if anatomically asplenic |
| Prognosis | Often comorbid with CHD (50–90%), which, if severe, may cause death at a young age. Prognosis is good if heart lesion not present or is repaired. | Often comorbid with CHD (nearly 100%), which, if severe, may cause death at a young age. Prognosis otherwise guarded due to risk of overwhelming sepsis. |
| Findings on imaging | Discordant position of cardiac situs relative to abdominal viscera. Stomach often on right side, with one or more spleens. Intestine may be mal- or non-rotated. Liver is often bridging with midline gallbladder. IVC interruption with azygos or hemiazygos continuation. Bilateral bilobed lungs with hyparterial bronchi. | Discordant position of cardiac situs relative to abdominal viscera. Stomach often on right side, with no spleen present. Intestine may be mal- or non-rotated. Liver is often bridging with midline gallbladder. IVC ipsilateral to aorta. Bilateral trilobed lungs with eparterial bronchi. |
Table 2.
Differential diagnostic considerations in case of suspected situs abnormality. Pertinent imaging findings listed for each type of situs arrangement.
| Differential Diagnosis | X-Ray Findings | Abdominal US Findings | CT Findings |
|---|---|---|---|
| Situs ambiguous | Heart in left hemithorax with cardiac apex directed to the left; stomach bubble on right | Stomach on right; variable presence and number of spleens (if present, spleen typically located ipsilateral to stomach); liver typically bridging or on left side | Intestine may be mal- or non-rotated with variable location of appendix; venous drainage below diaphragm may be variable |
| Situs ambiguous with polysplenia (left isomerism) | Heart in left hemithorax with cardiac apex directed to the left; stomach bubble on right | Stomach on right; one or more spleens typically located along greater curvature of stomach; liver often bridging with midline gallbladder | Intestine may be mal- or non-rotated; bilateral bilobed lungs with hyparterial bronchi; IVC interruption with azygos or hemiazygos continuation |
| Situs ambiguous with asplenia (right isomerism) | Heart in left hemithorax with cardiac apex directed to the left; stomach bubble on right | Stomach on right; characteristic absence of spleen; liver often bridging with midline gallbladder | Intestine may be mal- or non-rotated; bilateral trilobed lungs with eparterial bronchi; IVC ipsilateral to aorta |
| Situs inversus totalis | Concordant location of cardiac situs (dextroverted) relative to mirror-image abdominal viscera | Stomach on right side; one spleen on right side along greater curvature of stomach; liver on left side with left- sided gallbladder | Thoracoabdominal viscera are in complete mirror-image configuration compared to normal situs solitus; no distinct venous drainage patterns |
ABBREVIATIONS
- ASD
Atrial Septal Defect
- AV
Atrioventricular
- CHD
Congenital Heart Disease
- ILC
Isolated Levocardia
- IVC
Inferior Vena Cava
REFERENCES
- 1.McMillan JA. Oski’s Pediatrics: Principles & Practice. Lippincott Williams & Wilkins; 2006. [Google Scholar]
- 2.Roongruangchai J, Narongsak W, Plakornkul V. Situs inversus totalis and ultrastructure of respiratory cilia: report of a cadaveric case. J Med Assoc Thai. 2012;95(1):132–138. [PubMed] [Google Scholar]
- 3.Ghawi H, Zghouzi MM, Emahbes TM, Awad SM. Prenatal diagnosis of isolated levocardia and a structurally normal heart: two case reports and a review of the literature. Pediatr Cardiol. 2013;34(4):1034–1037. doi: 10.1007/s00246-012-0359-8. [DOI] [PubMed] [Google Scholar]
- 4.Vijayakumar V, Brandt T. Prolonged survival with isolated levocardia and situs inversus. Cleve Clin J Med. 1991 May-Jun;58(3):243–7. doi: 10.3949/ccjm.58.3.243. [DOI] [PubMed] [Google Scholar]
- 5.Applegate KE, Goske MJ, Pierce G, et al. Situs revisted: imaging of the heterotaxy syndrome. Radiographics. 1999;19(4):837–854. doi: 10.1148/radiographics.19.4.g99jl31837. [DOI] [PubMed] [Google Scholar]
- 6.Paladini D, Volpe P. Informa. 2007. Ultrasound of congenital fetal anomalies: differential diagnosis and prognostic indicators. [Google Scholar]
- 7.Durán MA, Guereña A. Sequence of right laterality with spleen: widening the spectrum of heterotaxy. Pediatr Pathol Mol Med. 2002;21(5):461–465. doi: 10.1080/15227950290104779. [DOI] [PubMed] [Google Scholar]
- 8.Ghosh S, Yarmish G, Godelman A, et al. Anomalies of visceroatrial situs. AJR Am J Roentgenol. 2009;193(4):1107–1117. doi: 10.2214/AJR.09.2411. [DOI] [PubMed] [Google Scholar]
- 9.Eksarko P, Nazir S, Kessler E, et al. Duodenal web associated with malrotation and review of literature. J Surg Case Rep. 2013;12 doi: 10.1093/jscr/rjt110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mahalik SK, Khanna S, Menon P. Malrotation and volvulus associated with heterotaxy syndrome. J Indian Assoc Pediatr Surg. 2012;17(3):138–140. doi: 10.4103/0971-9261.98138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jo DS, Jung SS, Joo CU. A case of unusual visceral heterotaxy syndrome with isolated levocardia. Korean Circ J. 2013 Oct;43(10):705–9. doi: 10.4070/kcj.2013.43.10.705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Van Laschot JJB, Gouma DJ, Tytgat GNJ, et al. Integrated medical and surgical gastroenterology. Bohn Stafleu Van Loghum; Houten: 2004. [Google Scholar]
- 13.Fulcher AS, Turner MA. Abdominal manifestations of situs anomalies in adults. Radiographics. 2002;22(6):1439–1456. doi: 10.1148/rg.226025016. [DOI] [PubMed] [Google Scholar]
- 14.Donnelly LF. Pediatric Imaging: The Fundamentals. Edition 1. Saunders; 2008. pp. 86–124. [Google Scholar]