Abstract
Objective
To clarify the relationship between IQ and subsequent risk for schizophrenia.
Method
IQ was assessed at ages 18-20 in 1,204,983 Swedish males born 1951-1975. Schizophrenia was assessed by hospital diagnosis through 2010.
Results
IQ had a monotonic relationship with schizophrenia risk across the IQ range with a mean change of 3.8% in risk per IQ point. This association, stronger in the lower versus higher IQ range, was similar if onsets within five years of testing were censored. No increased risk for schizophrenia was seen in those with highest intelligence. Co-relative control analyses showed a similar IQ-schizophrenia association in the general population and in cousin, half-sibling and full-sibling pairs. A robust interaction was seen between genetic liability to schizophrenia and IQ in predicting schizophrenia risk. Genetic susceptibility for schizophrenia had a much stronger impact on risk of illness for those with low versus high intelligence. The IQ-genetic liability interaction arose largely from IQ differences between close relatives.
Conclusions
IQ assessed in late adolescence is a robust risk factor for subsequent onset of schizophrenia. This association is not the result of a declining IQ associated with insidious onset. In this large, representative sample, we found no evidence for a link between genius and schizophrenia. Co-relative control analyses show that the association between lower IQ and schizophrenia is not the result of shared familial risk factors and may be causal. The strongest effect was seen with IQ differences within families. High intelligence substantially attenuates the impact of genetic liability on the risk for schizophrenia.
Speculations about the nature of the relationship between IQ and severe psychiatric illness began in the early 1900s shortly after the development of standardized intelligence tests (1;2). A recent meta-analysis of 12 studies including over 750,000 subjects examined the prospective relationship between IQ and schizophrenia, and concluded that IQ had a relatively consistent dose-response relationship with an increased risk for schizophrenia of ∼ 3.7% for every IQ point decrease (3). We here undertake a further study of this question in a prospective sample larger than all the prior published studies combined.
We address four questions about the IQ-schizophrenia relationship, the first two of which attempt to refine earlier findings. First, can we confirm the prior association of IQ and schizophrenia risk, and rule out the possibility that this association reflects prodromal effects of an impending schizophrenic illness? Second, can we clarify, in more detail than previously possible, the “dose-response” relationship between IQ and risk for schizophrenia? Is the association linear or non-linear, and if non-linear is the association stronger at lower or at higher IQs (3)? Furthermore, is the association monotonic so that the lowest risk for schizophrenia is seen with the highest IQ? Or, as suggested by some prior analyses (3), is the function U-shaped with the lowest risk at moderately high IQs and the highest IQ scores associated with a greater risk of illness?
We then examine two important questions about the IQ-schizophrenia association that have not, to our knowledge, been previously addressed. First, using a co-relative design, can we determine the degree to which the association between IQ and schizophrenia arises from shared familial/genetic factors or from a possible causal relationship? Second, what is the etiologic relationship between genetic liability to schizophrenia and premorbid IQ? Do these two risk factors add together in their effect or do they interact? If they interact, does a high genetic liability to schizophrenia have a greater impact on those with low, or those with high IQ?
Methods
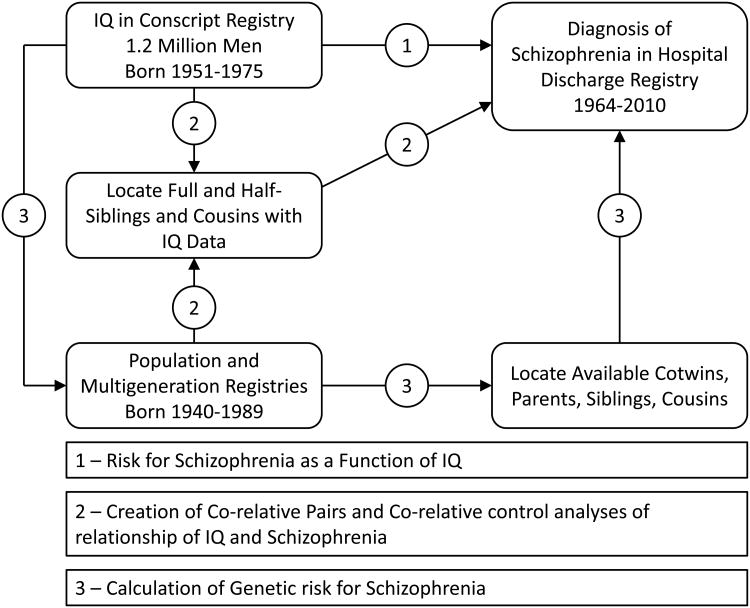
We used data from multiple Swedish nationwide registries linked by the unique individual Swedish 10-digit personal ID number assigned at birth or immigration to all Swedish residents. This ID number was replaced by a random number to preserve confidentiality. As illustrated in figure 1, the analyses here reported were largely based on four Swedish registries: i) the Military Conscription Register, which includes cognitive assessments for nearly all 18-year-old men in Sweden; ii) the Total Population Register, containing annual data on family status; iii) the Multi-Generation Register, providing information on family relations; and iv) the Swedish Hospital Discharge Register, containing all hospitalizations for Swedish inhabitants from 1964-2010. We also used data from the Swedish Mortality Register to calculate the follow-up time in our hazard models. The Swedish military service conscription examination involves a full medical assessment including cognitive function (IQ) measured by four subtests representing logical, spatial, verbal, and technical abilities. During the years covered by this study, this examination was required by law. Of men born in Sweden, only those with serious medical conditions or disabilities were excused (∼4.2 % of individuals). The global IQ score, derived from a summation of the four subtests, was standardized to give a Gaussian distributed score between one and nine. We translated this into units of the Wechsler Adult Intelligence Scale with a mean of 100, SD=15.
Figure 1.
Key Features of the Research Design – Data was obtained from 4 major Swedish National Registries: the Conscript Registry, the Population and Multigeneration Registries and the Hospital Discharge Registry. The three major analyses of this paper are illustrated. Examining the risk for schizophrenia as a function of priori IQ is accomplished by matching information from the Conscript Registry, via path 1, to the discharge registry. Performing co-relative analyses of the relationship between IQ and schizophrenia required obtaining male-male co-relative pairs with IQ data from the population, multigeneration and conscript registries and then matching those pairs with the discharge registry. These steps are indicated as path 2. Calculating the genetic risk for schizophrenia, used to jointly predict, along with IQ, the risk for schizophrenia, required the location of available cotwins, parents, siblings and cousins of individuals from the conscript registry in the population and multigeneration registries and then matching them to the discharge registry. These steps are indicated as path 3.
Schizophrenia was defined in the Swedish Hospital Discharge Register by the following ICD codes: ICD8: 295.1, 295.2, 295.3, 295.5, 295.6; ICD9: 295B, 295C, 295D, 295G, 295X; and ICD10: F20.0, F20.1, F20.2, F20.3, F20.5, F20.8, and F20.9. Non-affective psychosis was defined according to the following ICD codes: ICD8: 295, 297, 298.2, 298.3, 298.9; ICD9: 295, 297, 298C, 298E, 298W, 298X; and ICD10: F2. The ratio of NAP to schizophrenia cases in our sample is 2.14:1. We secured ethical approval for this study from the Regional Ethical Review Board of Lund University.
The database began with all male individuals in the Swedish population born 1951 to 1975 who were registered in the Military Conscription Register (N=1,324,117). 85,432 had no information for the IQ variable; 33,376 were missing data for the conscription examination; and 326 had a registration of schizophrenia prior to their conscription examination. In total we investigated 1,204,983 male individuals, 87.2% of all male individuals born in Sweden during 1951-1975 who survived to age 18.
We used Cox proportional hazards models to investigate the future risk for schizophrenia in individuals as a function of their IQ score. Robust standard errors were used to adjust the 95% confidence intervals (CIs) as we had several individuals from the same family. Follow-up time in number of years was measured from year of conscription examination until year of first registration for schizophrenia, death, emigration, or end of follow-up (year 2010), whichever came first. In all models, we investigated the proportionality assumption. In a second step, we wanted to compare the results from the entire population with the results from a co-relative design. By means of the Swedish Multi-Generation Register, we identified all full-sibling, half-sibling pairs, and first-cousin pairs. Using stratified Cox proportional hazards models, we performed three analyses on all full-sibling, all half-sibling and all first-cousin pairs that did not have the same IQ score from the conscription register, with a separate stratum for each relative pair. The co-relative design allows us to contrast the rates of schizophrenia in relatives with different levels of IQ. The stratified Cox proportional hazards models provides a Hazard ratio (HR) for IQ that is adjusted for the familial cluster, and, therefore, accounts for an array of shared genetic and environmental factors.
To investigate the etiologic relationship between genetic liability to schizophrenia and IQ, we calculated a genetic liability score for schizophrenia. First, we calculated the morbid risk for schizophrenia for the population born 1940-1989 using an abridged Weinberg age correction (4). We defined three age groups defined as the first, second+third, and fourth quartiles of the age distribution of first schizophrenia registration: <28 years weighted 0; 28-42 years weighted 0.5; and individuals > 42 years weighted 1. Thereafter, we performed a logistic regression analysis based on information from the Swedish population born 1940-1989 (n=5,646,776), and their relatives (MZ twins, DZ twins and full-siblings, half-siblings, mother, father, and cousins). The model outcome variable was schizophrenia and the predictor variable the morbid risk of schizophrenia among the different relative types. The resulting beta weights for the genetic liability score, which followed quantitative genetic expectations, are seen in table A1. We did not use standard family history scores (5) because they pool relatives thereby ignoring the large impact on risk of schizophrenia in specific relatives resulting from fitness effects (6;7). We generated the beta weights in the same sample to which we applied them. While this traditionally might result in “over-fitting,” this is a minimal concern when the entire population is being assessed.
This model produced a predicted probability for schizophrenia ranging between 0.36% and 79%, termed the genetic liability score. We repeated this approach applied to genetic liability to non-affective psychosis (table A2). We sought to examine the interaction between IQ and genetic liability on risk for schizophrenia. Along with Rothman (8), we favor a risk difference over a risk ratio approach to this question because it adopts a public health perspective asking if more cases of illness will arise when individuals at low versus high disease liability from one factor (genetic risk) are exposed to low versus high levels of another risk factor (IQ) (9). Therefore, we analyzed interactions using an identity link function. In the first model we estimated the interaction between IQ and genetic liability using the identity link. We, thereafter, sought to investigate whether this interaction was driven by between-families or within-families IQ effects. Within each set of full-siblings, we calculated the between and the within value of IQ (the between value is the mean value for each set of full-siblings, while the within value is each sibling's deviation from the mean value in the sibling set). In these models the genetic liability was averaged over all siblings within each set of siblings. We then performed a regression model using the identity link and robust standard errors, with the genetic liability score, the between-sibling sets IQ score, the within-siblings sets IQ score, and the two interaction terms: one with the between IQ score and the genetic liability score; and one with the within IQ score and the genetic liability score. We could then see if the interaction effect was due to between or within IQ effects, as the genetic liability score was held constant for all siblings within a sibling set. All statistical analyses were performed using SAS 9.3 (10).
Results
The Nature of the IQ-Schizophrenia Relationship
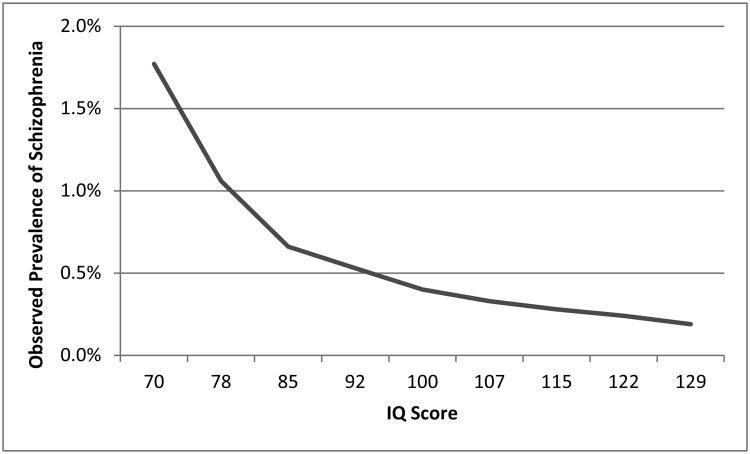
Our first analyses examined, in all males born 1951-1975 for whom conscript registry data was available (n= 1,204,983), whether an onset of schizophrenia was recorded in the hospital discharge registry after the conscription examination (path 1 in figure 1). Such an onset was found in 0.49% of these individuals (n=5,948). The risk for schizophrenia in each of the IQ deciles declined monotonically (figure 2), although the slope of the decline was steeper in the lower than in the higher IQ range.
Figure 2.
Observed Prevalence of Schizophrenia as a Function of Premorbid IQ score. Schizophrenia is assessed using hospital diagnoses. Only onsets after IQ testing are included.
A linear model fitted to these data produced a hazard ratio (HR) of 0.962 (95% 0.960-0.964), a change of 3.8% in risk for schizophrenia per IQ point. We next added a quadratic function to capture the steeper then more shallow function seen in figure 2. It was also significant, producing the following model: linear effect 0.967 (0.965; 0.969) and quadratic effect 1.001 (1.000; 1.001).
The Possible Effect of a Prodrome
One possible mechanism for an association between IQ and schizophrenia risk would be a decline in IQ as individuals entered a prodromal state associated with an insidious onset. If this mechanism were important, then the IQ-schizophrenia association should decline substantially if we censor onsets of schizophrenia occurring soon after IQ testing. We repeated analyses predicting the linear risk for first-onset of schizophrenia in those who were free of recorded schizophrenia episodes during the five-year period after administration of the IQ test (N=682, 11% of all cases). The linear association (0.963 (0.961; 0.965)) was nearly identical to that seen initially.
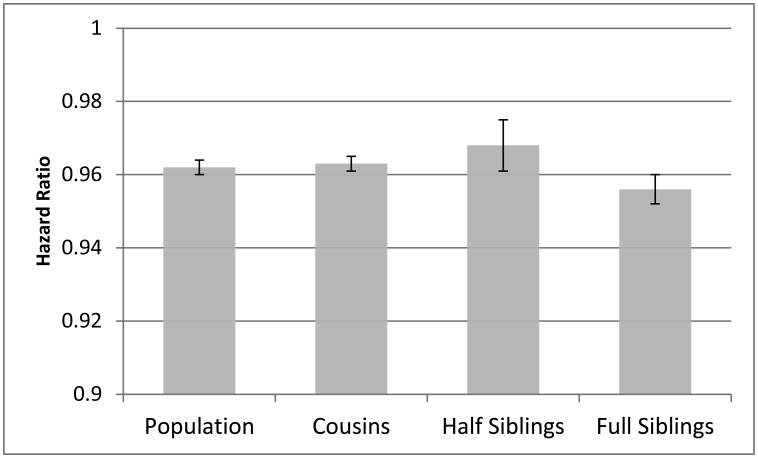
Co-Relative Analyses
For our co-relative analyses, we located male-male full-sibling, half-sibling and cousin pairs from the population and multigenerational registries who also had IQ data in the conscript registry and matched them to the discharge registry (paths 2 in figure 1). For simplicity, our co-relative analyses utilized the linear model only. In our entire sample, the HR for schizophrenia was 0.962 (0.960; 0.964). As seen in figure 3, the observed schizophrenia-IQ associations in co-relative pairs with differing IQs (that is, their IQ scores were not in the same decile) were: first-cousin pairs (ntotal=514,692; concordant affected n=12; discordant n=3,643; concordant unaffected n=511,037) 0.963 (0.961; 0.966); half-sibling pairs (ntotal=52,137; concordant affected n=3; discordant n=644; concordant unaffected n=51,490) 0.968 (0.961; 0.974); and full-sibling pairs discordant for IQ (ntotal=232,648; concordant affected n=52; discordant n=2,239; concordant unaffected n=230,357) 0.956 (0.952; 0.960). We were unable to estimate this effect within MZ pairs due to the very small available sample size (6 pairs discordant for both IQ and schizophrenia).
Figure 3.
Hazard Ratios with 95% confidence intervals for schizophrenia as a function of the premorbid IQ score in the general population and in first cousins, half-siblings and full siblings discordant for IQ score. Within these relative pairs with differing IQs, the association between IQ and schizophrenia is as strong as that seen in the general population.
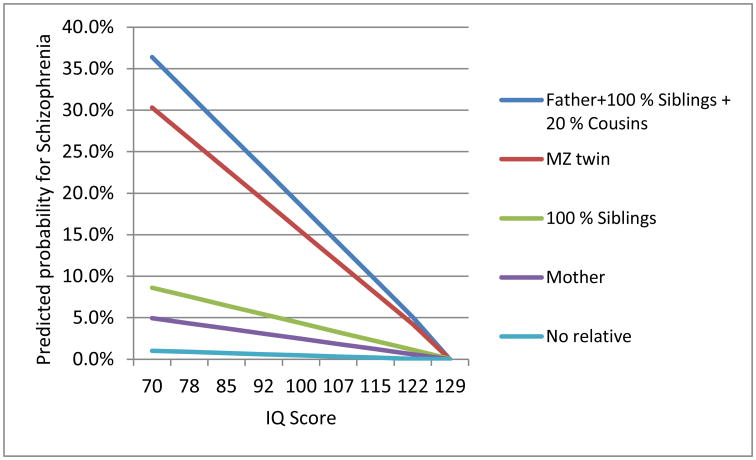
Interaction between IQ and Genetic Liability
Using the population and multigeneration registries, we located all available cotwins, parents, full- and half-siblings, and first cousins of our sample and matched these individuals to the discharge registry to calculate a genetic liability score (paths 3 in figure 1) which equaled the weighted function of the risk for schizophrenia in relatives. As seen in table 1, our regression model, implementing a risk difference approach to interactions, showed strong main effects for both IQ and genetic liability score, and a robust negative interaction: -0.0019 (SE - 0.0001) (p<< 0.0001). Figure 4 illustrates the predicted risk for schizophrenia as a function of premorbid IQ at five levels of increasing genetic liability. In the lower IQ range, large differences in risk for schizophrenia are seen in individuals with varying levels of genetic liability. However, at higher IQs, the impact of genetic liability on risk for schizophrenia decreases substantially and nearly disappears at the highest IQ level.
Table 1. Prediction of Future Risk for Schizophrenia from IQ, Genetic Liability to Schizophrenia and their Interaction Using an Identity Link Function.
| Genetic liability Assessed Using Schizophrenia in Relatives | Genetic liability Assessed Using Non-Affective Psychosis in Relatives | |||||
|---|---|---|---|---|---|---|
| Beta | SE | P-value | Beta | SE | P-value | |
| Intercept | 0.0053 | 0.0002 | <0.0001 | 0.0062 | 0.0002 | <0.0001 |
| IQ | -0.0007 | 0.0001 | <0.0001 | -0.0006 | 0.0001 | <0.0001 |
| Genetic Liability Score | 0.0174 | 0.0004 | <0.0001 | 0.0147 | 0.0004 | <0.0001 |
| Interaction (Genetic liability and IQ) | -0.0019 | 0.0001 | <0.0001 | -0.0019 | 0.0001 | <0.0001 |
Figure 4.
Predicted probability of schizophrenia as a function of premorbid IQ score and five increasing levels of genetic liability to schizophrenia as predicted by risk of illness in parents, full and half-siblings and cousins. These levels correspond to the following familial configurations: i) no relatives affected with schizophrenia; ii) an affected mother; iii) all full siblings affected; iv) an affected monozygotic cotwin and v) an affected father, all full siblings affected and 20% of first cousins affected.
We repeated these analyses using a broader definition of genetic liability based on rates of nonaffective psychosis (NAP) in relatives. The results were similar (table 1), although differences in risk at the highest IQ level were somewhat greater than that seen with the narrower definition of genetic liability (Figure A.1).
Finally, we examined in full-sibships (488,794 individuals from 224,003 families), the prediction of schizophrenia onset as a function of: i) genetic liability to schizophrenia, ii) a within-sibship IQ effect, and iii) a between-sibships IQ effect, and iv) the interactions between genetic liability and the within- and between-sibship IQ effects. As seen in table 2, while both interaction effects were significant, the interaction between genetic liability to schizophrenia and the within-sibship IQ effect was an order of magnitude stronger than that seen between genetic liability and the between-sibship IQ effects. These results suggest that, congruent with our co-relative findings, the overall interaction observed in our sample between IQ and genetic liability to schizophrenia is largely driven by a greater pathogenic effect of genetic risk on individuals with a lower IQs compared to their close relatives.
Table 2. Prediction of Future Risk for Schizophrenia from Genetic Liability to Schizophrenia, a Within-Sibship Effect of IQ, a Between-Sibships Effect of IQ and Their Interaction Using an Identity Link Function.
| Between/Within Model | |||
|---|---|---|---|
| Beta | SE | P-value | |
| Intercept | -0.006 | 0.0016 | 0.0003 |
| Between effect of IQ | -0.0004 | 0.0003 | 0.2254 |
| Within effect of IQ | 0.0074 | 0.0012 | <0.0001 |
| Genetic Liability to Schizophrenia | 0.0442 | 0.0043 | <0.0001 |
| Interaction (within)* | -0.0239 | 0.0032 | <0.0001 |
| Interaction (between)** | -0.0021 | 0.0008 | 0.0093 |
Interaction between the within sibship effect of IQ and Genetic liability to schizophrenia
Interaction between the between sibship effect of IQ and Genetic liability to schizophrenia
Discussion
We sought in this paper to address, in a nearly complete sample of Swedish males born 1951-1975, four questions about the relationship between IQ as assessed in late adolescence and subsequent risk for schizophrenia. First, we sought to replicate prior associations between IQ and future risk for schizophrenia. A linear hazard ratio model showed an increase in risk of onset of 3.8% with the decline of one IQ point. This estimate is nearly identical to the estimate of 3.7% obtained from the most recent meta-analysis (3). We also examined whether this association declined if we began our follow-up 5 years after IQ assessment, thereby eliminating most schizophrenia cases that would have been in a prodromal stage of schizophrenia at testing. Congruent with a prior Finnish study that examined a 1 year “blocked out” interval, (11), we found no change in the association with our delayed follow-up period. The observed IQ-schizophrenia association does not, to any appreciable degree, appear to result from declines in intelligence in subjects undergoing an insidious schizophrenic onset at the time of testing.
Our second goal was to clarify, with our large sample, the nature of the “dose-response” relationship between IQ and risk for schizophrenia. Inspection of the raw data (figure 2) revealed a monotonic relationship beginning with a relatively steep slope in the low IQ range with the slope declining as IQ increased. Model fitting, consistent with results of the recent meta-analysis (3), verified these impressions showing both a significant linear and a significant quadratic function.
In an examination of the five strongest prior studies of the IQ-schizophrenia relationship, three of these studies showed, compared to subjects with a moderately high IQ (∼120), greater risks of illness in those at the highest IQ levels (3). A Finnish study found substantial enrichment for cases of schizophrenia among those with the highest level of academic achievement in high school (12). Such findings suggest a relationship between schizophrenia and “genius” (13-15). However, our results show no evidence for this. Risk for schizophrenia in our highest IQ category (mean IQ 129; 0.19%) was lower than that in the next highest group (mean IQ 122; 0.24%).
Third, we sought to clarify the nature of the association between IQ and schizophrenia. Both intelligence and schizophrenia risk are strongly familial largely because of genetic factors (16-18). Therefore, the IQ-schizophrenia association could plausibly arise because of genetic and/or familial-environment factors predisposing both to low IQ and risk for schizophrenia. This hypothesis is consistent with evidence that: i) several candidate genes for schizophrenia are associated with lowered IQ (19;20); ii) identified copy number variants increase risk both for schizophrenia and intellectual disability (21); iii) an exome study in schizophrenia found enrichment in intellectual disability loss-of-function de novo mutations (22); iv) children at high genetic risk for schizophrenia were shown to have lowered IQ (23) and v) one prior twin study demonstrated a strong negative genetic correlation between IQ and schizophrenia liability (24).
Our results were inconsistent with this hypothesis. Within relative pairs with differing IQs, the association between intelligence and schizophrenia was as strong as in the general population. Furthermore, no trend was seen for the association to be attenuated (i.e., the HR to approach unity) in siblings who share half their genes and are typically reared together compared to that seen in cousin pairs (who share 1/8th of their genes and are rarely reared together) or, to that seen in the general population with no control for familial influences. However, our results are broadly congruent with a previous Swedish twin-sibling analysis that reports a very modest genetic correlation between IQ, as assessed at conscription, and schizophrenia (25). Our co-relative results are most consistent with the hypothesis that some environmental risk factors not shared with close relatives impact on brain functioning in a way that both lowers IQ and predisposes to risk for schizophrenia.
Our final goal was to illuminate the nature of the joint effects of genetic liability to schizophrenia and IQ on the risk for schizophrenia. We were particularly interested in distinguishing between additive effects – where liability to schizophrenia would reflect the independent contributions of genetic risk and IQ – versus an interactive model in which the impact of genetic liability to schizophrenia is moderated by IQ. If we found an interactive model, would sensitivity to genetic effects be greatest in those with low or with high IQ?
Our results robustly supported an interactive rather than the additive model for the joint effects of genetic liability and IQ on risk for schizophrenia. Furthermore, the interaction arose because individuals with low IQ were much more sensitive to the effect of genetic liability than those with high IQ. That is, high IQ substantially attenuated the impact of genetic liability on risk for schizophrenia. We extended these findings by examining a broader definition of genetic liability as assessed in relatives (non-affective psychosis) and produced similar findings. Follow-up analyses demonstrated that, consistent with our co-relative findings, the IQ-genetic liability interaction arose largely from IQ differences between close relatives.
This is not the place for speculative theories about why the still poorly understood genetic pathways of risk for schizophrenia might be more penetrant in individuals at low versus high intelligence. If our results are replicated, we can provide one important clue for neuroscientists and molecular geneticists. The changes in brain function that are expressed as low or high intelligence, and that convey sensitivity or resistance to the pathogenic effects of genetic liability to schizophrenia, appear to arise environmentally and will be seen most clearly in close relatives who differ in intelligence.
We are not the first to examine the relationship between IQ assessed in Swedish conscripts and subsequent risk for schizophrenia. Gunnell et al (26) and Zammit et al (27) examined 109,643 and 50,087 conscripts evaluated in 1990-1997 and 1969-1970, respectively. As expected, our results on the association of IQ and schizophrenia are congruent with their prior findings both of which were included in the recent meta-analysis (3). The agreement between our results and those of the meta-analysis are thus slightly biased because of sample sharing, although only 9.6% of schizophrenia cases from the meta-analysis came from these two Swedish studies (3).
Limitations
These results should be interpreted in the context of five potentially important methodological limitations. First, our sample was restricted to Swedish males. Second, we required a single hospital diagnosis of schizophrenia. Two studies found, using record reviews (28) and diagnostic interviews (29), that 96 and 94% of Swedish cases with hospital diagnoses of schizophrenia, respectively, met DSM-IV criteria for schizophrenia (30). When we narrowed our diagnosis to require ≥ 2 hospital diagnoses, the prevalence declined to 0.37%. Neither the linear (0.962 (0.959; 0.964)) effect of IQ on schizophrenia nor the results of the full-sibling co-relative control analyses (0.957 (0.952; 0.962)) changed appreciably. Third, IQ was available only as a global score in 9 categories, the uppermost with a mean of 129. Therefore, we might have failed to detect small increases in risk for schizophrenia associated with very high IQ scores or with high levels of specific cognitive abilities. Fourth, using a planned risk-difference approach (9), we observed a robust interaction in predicting schizophrenia from IQ and genetic liability. However, when these results were analyzed using a risk ratio approach, as implemented in Cox proportional hazards models, no significant interaction was found (p=0.27). To a first approximation, the impact of IQ and genetic liability to schizophrenia on risk for schizophrenia in this sample is the product of the two individual risks, not the sum. Fifth, diagnostic practices might differ by social class and indirectly by IQ. Such a bias is unlikely to explain much of the observed IQ-schizophrenia association because, in this sample, IQ also strongly predicts the HR for other non-affective psychoses: 0.971 (95% CIs 0.969-0.972).
Conclusions
IQ as assessed in late adolescence is a robust predictor for subsequent risk for schizophrenia and this association is not the result of a declining IQ associated with insidious onset. The nature of the association is monotonic, although stronger in the lower than in the higher IQ range. In our large and representative sample, we found no evidence for a link between genius and schizophrenia. Rather, the risk for schizophrenia was lowest in the group with the highest premorbid IQ. Co-relative control analyses show that the IQ-schizophrenia association does not result from shared genetic or familial-environmental risk factors and may be causal. Using a risk-difference model, a robust interaction was seen between genetic liability to schizophrenia and IQ in predicting schizophrenia risk. Genetic susceptibility for schizophrenia had a much stronger impact on risk of illness for those with a low versus a high IQ. This IQ-genetic liability interaction arose largely from IQ differences between close relatives.
Supplementary Material
Acknowledgments
This study was funded by grant RO1 MH083094 from the National Institute of Mental Health, the Swedish Research Council 2011-3340, 2012-2378, the ALF project grant, Lund, Sweden, and by the Swedish Research Council for Health, Working Life and Welfare (In Swedish: Forte; Reg.nr: 2013-1836).
Footnotes
Conflict of Interest Disclosures: None of the authors have conflicts to report.
References
- 1.Aylward E, Walker E, Bettes B. Intelligence in schizophrenia: meta-analysis of the research. Schizophr Bull. 1984;10(3):430–59. doi: 10.1093/schbul/10.3.430. [DOI] [PubMed] [Google Scholar]
- 2.Woodberry KA, Giuliano AJ, Seidman LJ. Premorbid IQ in schizophrenia: a meta-analytic review. Am J Psychiatry. 2008 May;165(5):579–87. doi: 10.1176/appi.ajp.2008.07081242. [DOI] [PubMed] [Google Scholar]
- 3.Khandaker GM, Barnett JH, White IR, Jones PB. A quantitative meta-analysis of population-based studies of premorbid intelligence and schizophrenia. Schizophr Res. 2011 Nov;132(2-3):220–7. doi: 10.1016/j.schres.2011.06.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Slater E, Cowie V. The Genetics of Mental Disorders. London: Oxford University Press; 1971. [Google Scholar]
- 5.Milne BJ, Moffitt TE, Crump R, Poulton R, Rutter M, Sears MR, Taylor A, Caspi A. How should we construct psychiatric family history scores? A comparison of alternative approaches from the Dunedin Family Health History Study. Psychol Med. 2008 Dec;38(12):1793–802. doi: 10.1017/S0033291708003115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Risch N. Estimating morbidity risks in relatives: the effect of reduced fertility. Behav Genet. 1983 Sep;13(5):441–51. doi: 10.1007/BF01065920. [DOI] [PubMed] [Google Scholar]
- 7.Kendler KS, MacLean CJ. The impact of altered fitness on the risk of illness in relatives. Genet Epidemiol. 1989;6(4):481–91. doi: 10.1002/gepi.1370060403. [DOI] [PubMed] [Google Scholar]
- 8.Rothman KJ, Greenland S, Lash TL. Modern Epidemiology. Third. Philadelphia, PA: Lippincott Williams & Wilkins; 2008. [Google Scholar]
- 9.Kendler KS, Gardner CO. Interpretation of interactions: guide for the perplexed. Br J Psychiatry. 2010 Sep;197(3):170–1. doi: 10.1192/bjp.bp.110.081331. [DOI] [PubMed] [Google Scholar]
- 10.Trull TJ, Sher KJ, Minks-Brown C, Durbin J, Burr R. Borderline personality disorder and substance use disorders: a review and integration. Clin Psychol Rev. 2000 Mar;20(2):235–53. doi: 10.1016/s0272-7358(99)00028-8. [DOI] [PubMed] [Google Scholar]
- 11.Tiihonen J, Haukka J, Henriksson M, Cannon M, Kieseppa T, Laaksonen I, Sinivuo J, Lonnqvist J. Premorbid intellectual functioning in bipolar disorder and schizophrenia: results from a cohort study of male conscripts. Am J Psychiatry. 2005 Oct;162(10):1904–10. doi: 10.1176/appi.ajp.162.10.1904. [DOI] [PubMed] [Google Scholar]
- 12.Isohanni I, Jarvelin MR, Jones P, Jokelainen J, Isohanni M. Can excellent school performance be a precursor of schizophrenia? A 28-year follow-up in the Northern Finland 1966 birth cohort. Acta Psychiatr Scand. 1999 Jul;100(1):17–26. doi: 10.1111/j.1600-0447.1999.tb10909.x. [DOI] [PubMed] [Google Scholar]
- 13.Waddell C. Creativity and mental illness: is there a link? Can J Psychiatry. 1998 Mar;43(2):166–72. doi: 10.1177/070674379804300206. [DOI] [PubMed] [Google Scholar]
- 14.Post F. Creativity and psychopathology. A study of 291 world-famous men. Br J Psychiatry. 1994 Jul;165(1):22–34. doi: 10.1192/bjp.165.1.22. [DOI] [PubMed] [Google Scholar]
- 15.Nasar SA. Beautiful Mind. London, UK: Faber and Faber; 1998. [Google Scholar]
- 16.Bouchard TJ, Jr, McGue M. Familial studies of intelligence: a review. Science. 1981 May 29;212(4498):1055–9. doi: 10.1126/science.7195071. [DOI] [PubMed] [Google Scholar]
- 17.Deary IJ, Spinath FM, Bates TC. Genetics of intelligence. Eur J Hum Genet. 2006 Jun;14(6):690–700. doi: 10.1038/sj.ejhg.5201588. [DOI] [PubMed] [Google Scholar]
- 18.Sullivan PF, Kendler KS, Neale MC. Schizophrenia as a complex trait: evidence from a meta-analysis of twin studies. Arch Gen Psychiatry. 2003 Dec;60(12):1187–92. doi: 10.1001/archpsyc.60.12.1187. [DOI] [PubMed] [Google Scholar]
- 19.Luciano M, Miyajima F, Lind PA, Bates TC, Horan M, Harris SE, Wright MJ, Ollier WE, Hayward C, Pendleton N, Gow AJ, Visscher PM, Starr JM, Deary IJ, Martin NG, Payton A. Variation in the dysbindin gene and normal cognitive function in three independent population samples. Genes Brain Behav. 2009 Mar;8(2):218–27. doi: 10.1111/j.1601-183X.2008.00462.x. [DOI] [PubMed] [Google Scholar]
- 20.Harrison PJ, Weinberger DR. Schizophrenia genes, gene expression, and neuropathology: on the matter of their convergence. Mol Psychiatry. 2005 Jan;10(1):40–68. doi: 10.1038/sj.mp.4001558. [DOI] [PubMed] [Google Scholar]
- 21.Guilmatre A, Dubourg C, Mosca AL, Legallic S, Goldenberg A, Drouin-Garraud V, Layet V, Rosier A, Briault S, Bonnet-Brilhault F, Laumonnier F, Odent S, Le VG, Joly-Helas G, David V, Bendavid C, Pinoit JM, Henry C, Impallomeni C, Germano E, Tortorella G, Di RG, Barthelemy C, Andres C, Faivre L, Frebourg T, Saugier VP, Campion D. Recurrent rearrangements in synaptic and neurodevelopmental genes and shared biologic pathways in schizophrenia, autism, and mental retardation. Arch Gen Psychiatry. 2009 Sep;66(9):947–56. doi: 10.1001/archgenpsychiatry.2009.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fromer M, Pocklington AJ, Kavanagh DH, Williams HJ, Dwyer S, Gormley P, Georgieva L, Rees E, Palta P, Ruderfer DM, Carrera N, Humphreys I, Johnson JS, Roussos P, Barker DD, Banks E, Milanova V, Grant SG, Hannon E, Rose SA, Chambert K, Mahajan M, Scolnick EM, Moran JL, Kirov G, Palotie A, McCarroll SA, Holmans P, Sklar P, Owen MJ, Purcell SM, O'Donovan MC. De novo mutations in schizophrenia implicate synaptic networks. Nature. 2014 Feb 13;506(7487):179–84. doi: 10.1038/nature12929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dickson H, Cullen AE, Reichenberg A, Hodgins S, Campbell DD, Morris RG, Laurens R. Cognitive impairment among children at-risk for schizophrenia. J Psychiatr Res. 2014 Mar;:50, 92–9. doi: 10.1016/j.jpsychires.2013.12.003. [DOI] [PubMed] [Google Scholar]
- 24.Toulopoulou T, Picchioni M, Rijsdijk F, Hua-Hall M, Ettinger U, Sham P, Murray R. Substantial genetic overlap between neurocognition and schizophrenia: genetic modeling in twin samples. Arch Gen Psychiatry. 2007 Dec;64(12):1348–55. doi: 10.1001/archpsyc.64.12.1348. [DOI] [PubMed] [Google Scholar]
- 25.Fowler T, Zammit S, Owen MJ, Rasmussen F. A population-based study of shared genetic variation between premorbid IQ and psychosis among male twin pairs and sibling pairs from Sweden. Arch Gen Psychiatry. 2012 May;69(5):460–6. doi: 10.1001/archgenpsychiatry.2011.1370. [DOI] [PubMed] [Google Scholar]
- 26.Gunnell D, Harrison G, Rasmussen F, Fouskakis D, Tynelius P. Associations between premorbid intellectual performance, early-life exposures and early-onset schizophrenia. Cohort study. Br J Psychiatry. 2002 Oct;:181, 298–305. doi: 10.1192/bjp.181.4.298. [DOI] [PubMed] [Google Scholar]
- 27.Zammit S, Allebeck P, David AS, Dalman C, Hemmingsson T, Lundberg I, Lewis G. A longitudinal study of premorbid IQ Score and risk of developing schizophrenia, bipolar disorder, severe depression, and other nonaffective psychoses. Arch Gen Psychiatry. 2004 Apr;61(4):354–60. doi: 10.1001/archpsyc.61.4.354. [DOI] [PubMed] [Google Scholar]
- 28.Lichtenstein P, Bjork C, Hultman CM, Scolnick E, Sklar P, Sullivan PF. Recurrence risks for schizophrenia in a Swedish national cohort. Psychol Med. 2006 Oct;36(10):1417–25. doi: 10.1017/S0033291706008385. [DOI] [PubMed] [Google Scholar]
- 29.Ekholm B, Ekholm A, Adolfsson R, Vares M, Osby U, Sedvall GC, Jonsson EG. Evaluation of diagnostic procedures in Swedish patients with schizophrenia and related psychoses. Nordic Journal of Psychiatry. 2005;59(1):457–64. doi: 10.1080/08039480500360906. [DOI] [PubMed] [Google Scholar]
- 30.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. Fourth. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.