Abstract
Background:
Radiostereometric analysis provides highly precise measurements of component micromotion relative to the bone that is otherwise undetectable by routine radiographs. This study compared, at a minimum of five years following surgery, the micromotion of tantalum and titanium acetabular cups and femoral head penetration in highly cross-linked polyethylene liners and conventional (ultra-high molecular weight polyethylene) liners in active patients who had undergone total hip replacement.
Methods:
This institutional review board-approved prospective, randomized, blinded study involved forty-six patients. Patients were randomized into one of four cohorts according to both acetabular cup and polyethylene liner. Patients received either a cementless cup with a titanium mesh surface or a tantalum trabecular surface and either a highly cross-linked polyethylene liner or an ultra-high molecular weight polyethylene liner. Radiostereometric analysis examinations and Short Form-36 Physical Component Summary, Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), University of California Los Angeles (UCLA) activity, and Harris hip scores were obtained preoperatively, postoperatively, at six months, and annually thereafter.
Results:
All patients had significant improvement (p < 0.05) in Short Form-36 Physical Component Summary, WOMAC, UCLA activity, and Harris hip scores postoperatively. On radiostereometric analysis examination, highly cross-linked polyethylene liners showed significantly less median femoral head penetration at five years (p < 0.05). Steady-state wear rates from one year to five years were 0.04 mm per year for ultra-high molecular weight polyethylene liners and 0.004 mm per year for highly cross-linked polyethylene liners. At the five-year follow-up, the median migration (and standard error) was 0.05 ± 0.20 mm proximally for titanium cups and 0.21 ± 0.05 mm for tantalum cups.
Conclusions:
In this young population who had undergone total hip replacement, radiostereometric analysis showed significantly less femoral head penetration in the highly cross-linked polyethylene liners compared with that in the conventional ultra-high molecular weight polyethylene liners. Penetration rates were one order of magnitude less in highly cross-linked polyethylene liners compared with ultra-high molecular weight polyethylene liners. There was no significant difference in proximal migration between the tantalum and titanium acetabular cups through the five-year follow-up (p > 0.19).
Level of Evidence:
Therapeutic Level I. See Instructions for Authors for a complete description of levels of evidence.
In the active population undergoing total hip arthroplasty, limiting polyethylene liner wear and maintaining acetabular cup stability are crucial to preventing premature implant failure and subsequent revision. The most common causes for revision total hip arthroplasty in the United States are instability and/or dislocation and mechanical loosening1. International registries have identified component loosening as the most common reason for short-term and intermediate-term revision total hip arthroplasty2,3.
The cellular-mediated inflammatory response to polyethylene liner wear debris is thought to be the primary mechanism leading to periprosthetic osteolysis and aseptic loosening4,5. The measurement of femoral head penetration, as an indicator of acetabular liner wear, provides an in vivo marker for premature implant failure; wear rates of <0.05 mm per year are associated with a low risk of osteolysis5. The interest in reducing wear and wear debris in ultra-high molecular weight polyethylene liners led to the development of highly cross-linked polyethylene liners, which have demonstrated improved resistance to wear and generation of fewer wear particles both in vitro and in vivo6,7. Despite improved wear properties, highly cross-linked polyethylene liners generate smaller wear particles and have reduced plasticity, reduced fatigue resistance, and reduced resistance to crack propagation, which may contribute to implant failure8,9. These material property trade-offs necessitate intermediate-term to long-term evaluation of highly cross-linked polyethylene liners compared with conventional ultra-high molecular weight polyethylene liners.
The design of cementless acetabular cups utilizes porous surface coatings to increase implant stability, to enhance osseous ingrowth, and to reduce aseptic loosening10-12. Titanium fiber cups have demonstrated excellent fixation with very low rates of loosening, liner disassociation, and pelvic osteolysis up to sixteen years and a 96% survival rate at twenty years13,14. Fifteen years ago, a novel porous biomaterial was developed from elemental tantalum with a unique metallic strut design resembling trabecular bone15. Compared with titanium porous coatings, tantalum cups possess higher-volume porosity (75% to 80%), a higher coefficient of friction against bone, and lower bulk stiffness, which are theorized to reduce stress shielding and enhance implant fixation15-17. Excellent clinical and radiographic results have been demonstrated at two18 and five19 years of follow-up. Many clinician researchers have called for detailed radiostereometric analysis (RSA) to quantify migration and to establish mechanical stability15. One RSA study showed minimal translation at two years using porous tantalum cups, but the authors recommended further long-term follow-up20.
In 2005, we initiated a prospective, doubly randomized trial in forty-six patients using RSA and clinical outcome measures to examine femoral head penetration in highly cross-linked polyethylene liners compared with that in standard ultra-high molecular weight polyethylene liners in patients who underwent total hip arthroplasty; our two-year results were previously reported21. In the present study, we asked whether reduced penetration into the highly cross-linked polyethylene liners with no detectable difference in clinical outcomes remained valid after five years of follow-up. Additionally, we evaluated the performance of tantalum hemispheric cups compared with that of titanium hemispheric cups.
Materials and Methods
Study Design
Patient selection and surgical technique were described previously21; demographic characteristics and preoperative evaluation are shown in Table I.
TABLE I.
Baseline Demographic Characteristics and Preoperative Evaluation
| All Patients (N = 46) | Ultra-High Molecular Weight Polyethylene Liner and Titanium Cup Cohort (N = 11) | Highly Cross-Linked Polyethylene Liner and Titanium Cup Cohort (N = 12) | Ultra-High Molecular Weight Polyethylene Liner and Tantalum Cup Cohort (N = 11) | Highly Cross-Linked Polyethylene Liner and Tantalum Cup Cohort (N = 12) | |
| Age* (yr) | 58 ± 7 | 56 ± 6 | 59 ± 8 | 59 ± 8 | 60 ± 7 |
| Sex† | |||||
| Male | 19 | 3 | 4 | 6 | 6 |
| Female | 27 | 8 | 8 | 5 | 5 |
| Diagnosis† | |||||
| Osteoarthritis | 42 | 11 | 11 | 10 | 10 |
| Osteonecrosis | 4 | 0 | 1 | 1 | 2 |
| BMI* (kg/m2) | 30 ± 4 | 29 ± 6 | 30 ± 4 | 28 ± 4 | 31 ± 4 |
| UCLA activity score* (points) | 5 ± 2 | 5 ± 2 | 5 ± 2 | 5 ± 2 | 4 ± 2 |
| Harris hip score* (points) | 45.2 ± 15 | 41.2 ± 10 | 46.1 ± 12 | 46.0 ± 18 | 46.0 ± 17 |
| SF-36* (points) | |||||
| PCS | 29.7 ± 8 | 34.1 ± 8 | 29.2 ± 5 | 29.6 ± 8 | 29.5 ± 10 |
| MCS | 50.6 ± 15 | 52.1 ± 15 | 54.0 ± 11 | 53.2 ± 18 | 44.5 ± 16 |
| WOMAC*‡ (points) | |||||
| Pain | 11.7 ± 4 | 11.6 ± 2 | 12.2 ± 4 | 11.7 ± 5 | 11.9 ± 5 |
| Stiffness | 4.7 ± 2 | 4.6 ± 1 | 5.0 ± 1 | 5.1 ± 2 | 4.6 ± 2 |
| Function | 40.7 ± 13 | 40.8 ± 8 | 42.1 ± 13 | 40.5 ± 15 | 37.8 ± 14 |
| Total | 57.1 ± 17 | 55.9 ± 10 | 60.0 ± 17 | 55.0 ± 21 | 52.1 ± 20 |
The values are given as the mean and the standard deviation.
The values are given as the number of patients.
Higher WOMAC scores, ranging from 0 to 100 points, represent worse pain and more physical function limitations.
Patients were randomized into one of four cohorts: ultra-high molecular weight polyethylene liner and titanium cup, highly cross-linked polyethylene liner and titanium cup, ultra-high molecular weight polyethylene liner and tantalum cup, and highly cross-linked polyethylene liner and tantalum cup.
Intraoperative RSA Technique
In addition to the tantalum markers present on the femoral implant, tantalum beads (1.0-mm diameter) were inserted into the periacetabular bone (seven beads), greater trochanter (five beads), and lesser trochanter (two beads) in a dispersed arrangement to confer precise RSA measurements22,23. Eighteen tantalum beads were also implanted along the periphery of each polyethylene liner. This method of intraoperative marker implantation has been validated in a prior study with no reported adverse events related to tantalum marker placement or migration22.
RSA and Clinical Evaluations
Two patients died because of medical oncology complications (acute myelogenous leukemia and metastatic non-small cell lung cancer) unrelated to their total hip arthroplasty.
RSA was performed at two weeks, six months, and yearly thereafter. Two pairs of standing, digitized RSA radiographs were obtained with use of a standard hip cage (model 43; RSA Biomedical, Umeå, Sweden) in a dedicated RSA imaging suite at the UMass Memorial Medical Center’s Arthritis and Joint Replacement Center with two fixed radiograph sources. Each patient had at least one set of double examinations taken at a single visit to determine the precision of the radiographic setup. A single blinded investigator (M.G.) analyzed the pairs of radiographs using the digital software package UmRSA (RSA Biomedical).
Polyethylene wear was measured with use of point motion: penetration of the center of the femoral head into the acetabular cup. Penetration in the y-plane or proximal direction was reported. The cup segment in the titanium cohort was defined by up to six polyethylene liner beads, the cup center, and two points identified on the cup with use of edge detection (Fig. 1). Because of the inability to identify the center of the femoral head with use of edge detection in the radiodense tantalum cups, we developed and tested a novel method to assess wear data from this cohort (unpublished data). The novel fictive femoral head method was based on the identification of two radiopaque tantalum markers attached to the stem proximally and a priori knowledge of the femoral head and stem configuration of the inserted total hip replacement. A stem configuration library was created from a series of radiographs, providing geometrical information that was then used to place, in a three-dimensional space, a fictive femoral head center to be used by the RSA software.
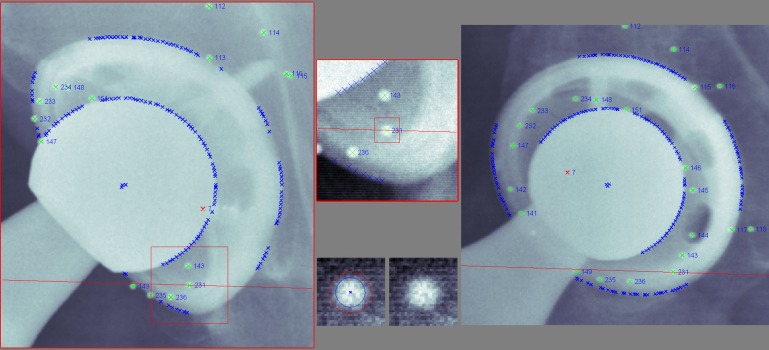
Fig. 1.
Titanium cup measurement in UmRSA software using the gold standard of beads, edge detection, and cup center to define the acetabular cup segment for both wear and cup-migration measurements. Note that the femoral head can be measured with use of edge detection to identify the head center for wear measurement.
Cup migration was measured with use of segment motion, and migration of the acetabular cup segment was compared with the fixed acetabular bone segment. The titanium cup segment was defined as described above, and the tantalum cup segment was defined with use of a beadless method, as the beads are not visible on RSA radiographs because of the dense tantalum cup. The cup center and four additional points were assigned to the tantalum cups with use of edge detection of the back of the cup and its opening (see Appendix). The maximum acceptable mean error of rigid body fitting for all comparisons was 0.25. The maximum acceptable condition number for wear measurements was 100. For cup migration, the maximum acceptable condition number was 120 in the titanium cohort and 245 in the tantalum cohort. The higher condition number was allowed in the tantalum cohort because of the lower number of points defining this segment (up to 5 points) compared with that in the titanium cohort (up to 9 points).
Clinical evaluation included standard patient history, musculoskeletal examination, and screening for postoperative complications. Several validated patient-reported outcome measures were administered preoperatively, postoperatively (at two weeks), at six months, and yearly thereafter: Short Form-36 (SF-36) Physical Component Summary (PCS) and Mental Component Summary (MCS), Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), University of California Los Angeles (UCLA) activity, and Harris hip scores.
Statistical Analysis
A power analysis revealed that a sample size of twenty patients in each group would be adequate to determine a difference in liner wear with use of RSA with a high statistical power (95%) and significance level (p < 0.05), based on a two-tailed t test of expected total liner wear of 0.1 mm per year among control liners compared with 0.002 mm per year among highly cross-linked liners following a standard nonelastic deformation of 0.1 mm during the first six months (considered the bedding-in period). This sample size also allowed for unexpected losses to follow-up due to study withdrawal, death, or other reasons. Statistical analysis of liner penetration and cup migration was performed with use of the Mann-Whitney test because of significant outliers, whereas the analysis of variance (ANOVA) with the Bonferroni multiple comparison test was used to compare differences in clinical outcome measures among study groups.
Source of Funding
Three authors of this study (C.B., D.C.A., and M.G.) received funding from Zimmer. Funds were used to pay for RSA equipment, instruments, supplies, and salaries.
Results
Baseline Data
Baseline demographic and preoperative data are presented in Table I for all four patient cohorts. Three patients were lost to follow-up before their three-year visit. On preoperative evaluation, the average results (and standard deviation) were 58 ± 7 years for patient age, 30 ± 4 kg/m2 for body mass index (BMI), 5 ± 2 points for the UCLA activity score at the time of surgery (but reported a UCLA activity score of 8 to 10 points within five years of surgery), and 45 ± 15 points for the Harris hip score. Randomization was successful, demonstrating similar preoperative age, sex distribution, BMI, UCLA activity score, Harris hip score, and SF-36 PCS, SF-36 MCS, and WOMAC subscores (all p > 0.05). Patient randomization, follow-up status, and RSA availability for each of the four cohorts are presented in the Appendix.
Femoral Head Penetration
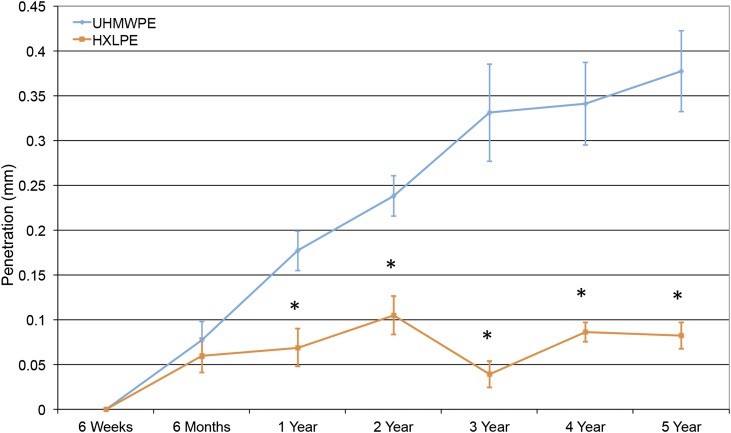
The median femoral head penetration for both the ultra-high molecular weight polyethylene liners and the highly cross-linked polyethylene liners in the titanium acetabular shells was calculated at six months and yearly thereafter through five years of follow-up (Fig. 2 and Table II). Median penetration for the ultra-high molecular weight polyethylene liner group showed a steady increase at each time point, but penetration in the highly cross-linked polyethylene liners showed only a minor increase after the six-month bedding-in period. The median penetration measurements were significantly greater in the ultra-high molecular weight polyethylene liner compared with the highly cross-linked polyethylene liner cohorts at the one through five-year follow-up (all p ≤ 0.003). There was a significant increase in head penetration from one year to five years in both polyethylene types when testing with a paired Wilcoxon signed rank test: from a median (and standard error) of 0.18 ± 0.02 mm at one year to 0.38 ± 0.05 mm at five years in ultra-high molecular weight polyethylene (p = 0.012) compared with 0.07 ± 0.02 mm at one year to 0.08 ± 0.01 mm at five years in highly cross-linked polyethylene liners (p = 0.046). The wear rates calculated from the one to five-year follow-ups were 0.04 mm per year for ultra-high molecular weight polyethylene liners and 0.004 mm per year for highly cross-linked polyethylene liners.
Fig. 2.
The median femoral head penetration (and standard error) in the proximal direction was significantly higher at all time points, except at six months in the ultra-high molecular weight polyethylene (UHMWPE) cohort, compared with the highly cross-linked polyethylene (HXLPE) cohort (*p < 0.003). Within each cohort, there was significant change in head penetration from one to five years of follow-up (p = 0.012 for the ultra-high molecular weight polyethylene liner group and p = 0.046 for the highly cross-linked polyethylene liner group).
TABLE II.
Total Femoral Head Penetration into the Ultra-High Molecular Weight Polyethylene and Highly Cross-Linked Polyethylene Liners in the Lateral, Proximal, and Axial Dimensions at Each of the Follow-up Intervals*
| Follow-up |
||||||
| Six Months | One Year | Two Years | Three Years | Four Years | Five Years | |
| Ultra-high molecular weight polyethylene liners | ||||||
| Lateral (x-axis) | 0.01 ± 0.03 | 0.03 ± 0.02 | −0.02 ± 0.03 | −0.03 ± 0.05 | −0.06 ± 0.05 | −0.04 ± 0.04 |
| Proximal (y-axis) | 0.08 ± 0.02 | 0.18 ± 0.02 | 0.24 ± 0.02 | 0.33 ± 0.05 | 0.34 ± 0.05 | 0.38 ± 0.05 |
| Axial (z-axis) | 0.08 ± 0.05 | 0.10 ± 0.04 | 0.12 ± 0.05 | 0.22 ± 0.09 | 0.14 ± 0.06 | 0.12 ± 0.06 |
| Highly cross-linked polyethylene liners | ||||||
| Lateral (x-axis) | 0.01 ± 0.02 | −0.01 ± 0.01 | 0.01 ± 0.03 | −0.04 ± 0.03 | 0.02 ± 0.02 | 0.01 ± 0.02 |
| Proximal (y-axis) | 0.06 ± 0.02 | 0.07 ± 0.02 | 0.11 ± 0.02 | 0.04 ± 0.01 | 0.09 ± 0.01 | 0.08 ± 0.01 |
| Axial (z-axis) | −0.01 ± 0.05 | 0.02 ± 0.04 | 0.06 ± 0.03 | 0.05 ± 0.05 | −0.02 ± 0.03 | 0.03 ± 0.05 |
The values are given as the median and the standard error, in millimeters.
Two patients did not have suitable double examinations for the wear precision analysis. The 95% confidence interval for the precision of the wear measurements was −0.006 to 0.038 mm, indicating that the radiographic precision was not adequate enough to allow inclusion of these RSA examinations in further analysis.
Acetabular Cup Translation
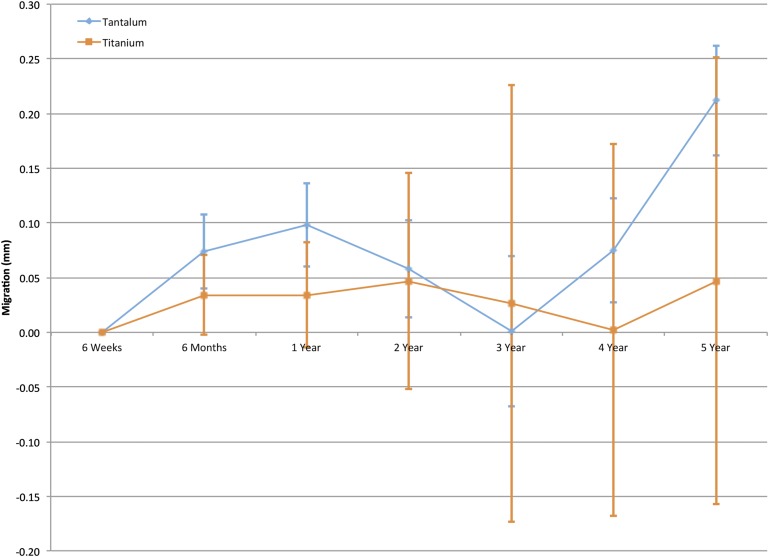
The median proximal translation for both the titanium acetabular cups (Trilogy Acetabular Hip System; Zimmer, Warsaw, Indiana) and the tantalum acetabular cups (Trabecular Metal Modular Acetabular System; Zimmer) was calculated at six months and yearly thereafter through the five-year follow-up (Fig. 3). There was no significant difference between the two cups (p > 0.19); however, the median translation was greater at all time points for the tantalum mesh cups (except at the three-year follow-up). At the five-year follow-up, the median migration (and standard error) was 0.05 ± 0.20 mm proximally for the titanium cups and 0.21 ± 0.05 mm for the tantalum cups. Two patients with titanium cups demonstrated over 2 mm of proximal migration at the five-year follow-up (see Appendix), causing large standard errors. On examination, neither patient had pain or limitation from the total hip arthroplasty nor had evidence of osteolysis or loosening on radiographs through the five-year follow-up. No significant outliers were seen in the tantalum cohort; however, variable small-scale migration patterns were evident (see Appendix).
Fig. 3.
The median acetabular cup migration (and standard error) in the proximal direction for both tantalum and titanium cup cohorts. There were no significant differences at any time points between the cup groups.
In the titanium cohort, two patients did not have suitable double examinations for the cup-migration precision analysis. The 95% confidence interval for the precision of the titanium cup-migration measurements was −0.005 to 0.069 mm. Excluding the one patient without suitable double examinations, the 95% confidence interval for the precision of the tantalum cup-migration measurements was larger, from −0.028 to 0.063 mm. The median translation of the titanium cups was within the error of the radiographic setup, indicating that true motion was not measured in the majority of patients in this cohort.
Clinical Outcomes
Standardized patient outcome assessments were completed preoperatively, postoperatively (at two weeks), at six months, and yearly thereafter. The mean scores were calculated for each cohort with preoperative, one-year, four-year, and five-year scores compared in Table III. Patient activity measured by the UCLA activity score had improved at one year following surgery and remained elevated through the five-year follow-up. Patient pain and physical function (SF-36 PCS score) improved at one year following surgery, continued to improve at four years, and remained elevated at the five-year follow-up. A similar trend was seen in the Harris hip score. Patient emotional health, interpreted through the SF-36 MCS score, did not change significantly throughout the five-year follow-up (p ≥ 0.05). WOMAC scores improved significantly (p < 0.05) and remained low (less pain) through the five-year follow-up. No significant difference was observed among the four cohorts at each follow-up (p ≥ 0.05).
TABLE III.
Comparison of Clinical Outcomes Between Randomized Polyethylene Liner and Acetabular Cup Cohorts
| Preoperative Outcomes* | One-Year Outcomes* | Four-Year Outcomes* | Five-Year Outcomes* | |
| SF-36 PCS† | ||||
| Ultra-high molecular weight polyethylene liner and titanium cup | 34 ± 8 | 49 ± 9 | 51 ± 8 | 51 ± 9 |
| Highly cross-linked polyethylene liner and titanium cup | 29 ± 5 | 50 ± 9 | 46 ± 14 | 44 ± 10 |
| Ultra-high molecular weight polyethylene liner and tantalum cup | 29 ± 8 | 48 ± 9 | 53 ± 6 | 52 ± 7 |
| Highly cross-linked polyethylene liner and tantalum cup | 29 ± 10 | 44 ± 12 | 50 ± 11 | 48 ± 10 |
| SF-36 MCS‡ | ||||
| Ultra-high molecular weight polyethylene liner and titanium cup | 52 ± 15 | 59 ± 4 | 56 ± 5 | 54 ± 10 |
| Highly cross-linked polyethylene liner and titanium cup | 54 ± 11 | 54 ± 9 | 50 ± 13 | 50 ± 16 |
| Ultra-high molecular weight polyethylene liner and tantalum cup | 53 ± 18 | 59 ± 6 | 50 ± 14 | 55 ± 8 |
| Highly cross-linked polyethylene liner and tantalum cup | 44 ± 16 | 52 ± 10 | 52 ± 12 | 54 ± 9 |
| WOMAC†§ | ||||
| Ultra-high molecular weight polyethylene liner and titanium cup | 55 ± 10 | 8 ± 9 | 1 ± 2 | 6 ± 7 |
| Highly cross-linked polyethylene liner and titanium cup | 60 ± 17 | 4 ± 7 | 5 ± 10 | 3 ± 4 |
| Ultra-high molecular weight polyethylene liner and tantalum cup | 55 ± 21 | 8 ± 7 | 4 ± 4 | 5 ± 6 |
| Highly cross-linked polyethylene liner and tantalum cup | 52 ± 10 | 11 ± 14 | 10 ± 22 | 3 ± 5 |
| UCLA activity score† | ||||
| Ultra-high molecular weight polyethylene liner and titanium cup | 5 ± 2 | 7 ± 1 | 7 ± 1 | 7 ± 1 |
| Highly cross-linked polyethylene liner and titanium cup | 5 ± 2 | 7 ± 1 | 7 ± 1 | 6 ± 2 |
| Ultra-high molecular weight polyethylene liner and tantalum cup | 5 ± 2 | 6 ± 2 | 7 ± 1 | 7 ± 2 |
| Highly cross-linked polyethylene liner and tantalum cup | 4 ± 2 | 6 ± 2 | 7 ± 2 | 7 ± 1 |
| Harris hip score† | ||||
| Ultra-high molecular weight polyethylene liner and titanium cup | 41 ± 10 | 86 ± 12 | 97 ± 3 | 92 ± 8 |
| Highly cross-linked polyethylene liner and titanium cup | 41 ± 12 | 89 ± 11 | 92 ± 14 | 93 ± 8 |
| Ultra-high molecular weight polyethylene liner and tantalum cup | 41 ± 18 | 87 ± 10 | 96 ± 3 | 92 ± 8 |
| Highly cross-linked polyethylene liner and tantalum cup | 46 ± 17 | 84 ± 20 | 90 ± 22 | 91 ± 11 |
The values are given as the mean and the standard deviation, in points.
The one-year, four-year, and five-year outcome values for the SF-36 PCS, WOMAC, and Harris hip scores were significantly different from preoperative values (all p < 0.05) as well as the four-year and five-year outcome values for the UCLA activity score (p < 0.05).
All values for the SF-36 MCS were not significantly different from preoperative values (p > 0.05).
Higher WOMAC scores, ranging from 0 to 100 points, represent worse pain and more physical function limitations.
Discussion
In this study, separating the patients into four cohorts based upon the type of polyethylene liner and acetabular cup did not reveal any significant differences in pain or function over the five-year follow-up. These analyses show that activity, pain, and well-being were unaffected by the type of polyethylene liner or acetabular cup, and clinical gains following total hip arthroplasty were largely realized by six months following surgery, as we have previously reported21.
In our young population of patients who underwent total hip arthroplasty, RSA revealed significantly less femoral head penetration in the highly cross-linked polyethylene liners compared with the ultra-high molecular weight polyethylene liners at the one-year follow-up; this persisted through the five-year follow-up, at which point there was four times less penetration in the highly cross-linked polyethylene liners compared with the ultra-high molecular weight polyethylene liners. A recent meta-analysis of twelve studies with an average follow-up duration of 5.1 years found 0.23-mm less wear in the highly cross-linked polyethylene liners compared with the ultra-high molecular weight polyethylene liners, consistent with our analysis24. Three other randomized controlled studies showed comparable penetration rates25-27. The difference between studies falls within the precision of the different measurement techniques used (as high as 0.1 mm in the off-the-shelf RSA system to 0.022 in the implanted RSA marker technique)27,28.
As we previously reported, a similar degree of femoral head penetration was evident through the six-month follow-up in both polyethylene liner types, representing the plastic creep-dominated phase of penetration known as bedding-in21. After six months, the ultra-high molecular weight polyethylene liner penetration continued to increase through the five-year follow-up, whereas the highly cross-linked polyethylene liner penetration plateaued. Any penetration after one year is thought to be dominated by wear, which is dependent upon the mechanical properties, oxidation resistance, and wear resistance of the polyethylene29.
The femoral head penetration rate was one order of magnitude lower in the highly cross-linked polyethylene liners (0.004 mm per year) compared with the ultra-high molecular weight polyethylene liners (0.04 mm per year) beginning in year 2. We therefore discontinued further randomization of the polyethylene liners at the end of year 2, and, throughout the remainder of the study, all patients received highly cross-linked polyethylene liners.
RSA cup-migration analyses in this study were also influenced by the tantalum cup use. The gold-standard RSA method was utilized for the titanium cup cohort, and a beadless edge-detection technique was implemented for the tantalum cup cohort30. We used the more precise gold-standard method (95% confidence intervals) that allowed the analyses to incorporate the most radiographic information available. Although the beadless edge detection was less precise, this technique was the best option for measuring radiodense cups.
The RSA examination showed no significant difference in migration in tantalum cups compared with titanium cups through a five-year follow-up. However, there was a trend toward greater migration in the tantalum cups. The tantalum difference was evident as early as six months after surgery and persisted through five years—except for the three-year follow-up, at which titanium cup migration was found to be greater. Kärrholm and Snorrason reported that migration over two years was comparable with cemented cups31. The only published RSA study that we are aware of that compared migration in patients randomized to receive either titanium cups (Trilogy) or Trabecular Metal cups found no significant difference in longitudinal migration at two years20. A systematic review comparing studies using RSA to measure acetabular cup migration found that every millimeter of proximal migration increased the rate of revision surgery at ten years after total hip arthroplasty32.
Including the two titanium outliers, no implants were loose on radiographs, there was no evidence of osteolysis, and no revisions were needed through the five-year follow-up. Although there was proximal motion of the acetabular component in the two titanium outliers, both patients were doing well clinically according to patient-recorded outcomes that showed improved function and excellent pain relief. They will continue to be monitored closely by clinical and radiographic follow-up. Trilogy titanium mesh and Trabecular Metal cups showed excellent fixation, similar to the findings in other reports2,19,33-35.
Appendix
Figures showing tantalum cup measurement in UmRSA software with use of the beadless edge-detection technique to define the acetabular cup segment for cup-migration measurements, the allocation of randomized patients, Trilogy titanium acetabular cup proximal translation in millimeters for individual patients, and Tantalum acetabular cup proximal translation in millimeters for individual patients showing variable small-scale migration patterns are available with the online version of this article as a data supplement at jbjs.org.
Acknowledgments
Note: We would like to thank Marie Walcott, MD, Peyton Hays, Mark Eskander, MD, Christina Kane, MD, and Anthony Porter Jr., MD, for their contribution in the acquisition of the data as well as Sylvie Puig, PhD, for her editorial contribution.
Footnotes
Investigation performed at the Department of Orthopedics and Physical Rehabilitation, University of Massachusetts Medical School, UMass Memorial Health Care, Worcester, Massachusetts
A commentary by Adolph V. Lombardi Jr., MD, is linked to the online version of this article at jbjs.org.
Disclosure: One or more of the authors received payments or services, either directly or indirectly (i.e., via his or her institution), from a third party in support of an aspect of this work. None of the authors, or their institution(s), have had any financial relationship, in the thirty-six months prior to submission of this work, with any entity in the biomedical arena that could be perceived to influence or have the potential to influence what is written in this work. Also, no author has had any other relationships, or has engaged in any other activities, that could be perceived to influence or have the potential to influence what is written in this work. The complete Disclosures of Potential Conflicts of Interest submitted by authors are always provided with the online version of the article.
References
- 1.Bozic KJ, Kurtz SM, Lau E, Ong K, Vail TP, Berry DJ. The epidemiology of revision total hip arthroplasty in the United States. J Bone Joint Surg Am. 2009January;91(1):128-33. [DOI] [PubMed] [Google Scholar]
- 2.Havelin LI, Engesaeter LB, Espehaug B, Furnes O, Lie SA, Vollset SE. The Norwegian Arthroplasty Register: 11 years and 73,000 arthroplasties. Acta Orthop Scand. 2000August;71(4):337-53. [DOI] [PubMed] [Google Scholar]
- 3.Australian Orthopaedic Association. Hip and knee arthroplasty. National joint replacement registry annual report 2008. 2008. https://aoanjrr.dmac.adelaide.edu.au/documents/10180/42662/Annual%20Report%202008?version=1.1&t=1349406277970. Accessed 2014 Dec 2.
- 4.Amstutz HC, Campbell P, Kossovsky N, Clarke IC. Mechanism and clinical significance of wear debris-induced osteolysis. Clin Orthop Relat Res. 1992March;(276):7-18. [PubMed] [Google Scholar]
- 5.Dumbleton JH, Manley MT, Edidin AA. A literature review of the association between wear rate and osteolysis in total hip arthroplasty. J Arthroplasty. 2002August;17(5):649-61. [DOI] [PubMed] [Google Scholar]
- 6.Muratoglu OK, Bragdon CR, O’Connor DO, Jasty M, Harris WH. A novel method of cross-linking ultra-high-molecular-weight polyethylene to improve wear, reduce oxidation, and retain mechanical properties. Recipient of the 1999 HAP Paul Award. J Arthroplasty. 2001February;16(2):149-60. [DOI] [PubMed] [Google Scholar]
- 7.Jacobs CA, Christensen CP, Greenwald AS, McKellop H. Clinical performance of highly cross-linked polyethylenes in total hip arthroplasty. J Bone Joint Surg Am. 2007December;89(12):2779-86. [DOI] [PubMed] [Google Scholar]
- 8.Ingram JH, Stone M, Fisher J, Ingham E. The influence of molecular weight, crosslinking and counterface roughness on TNF-alpha production by macrophages in response to ultra high molecular weight polyethylene particles. Biomaterials. 2004August;25(17):3511-22. [DOI] [PubMed] [Google Scholar]
- 9.Pruitt LA. Deformation, yielding, fracture and fatigue behavior of conventional and highly cross-linked ultra high molecular weight polyethylene. Biomaterials. 2005March;26(8):905-15. [DOI] [PubMed] [Google Scholar]
- 10.Friedman RJ, Black J, Galante JO, Jacobs JJ, Skinner HB. Current concepts in orthopaedic biomaterials and implant fixation. J Bone Joint Surg Am. 1993;75(7):1086-11. [Google Scholar]
- 11.Clohisy JC, Harris WH. Primary hybrid total hip replacement, performed with insertion of the acetabular component without cement and a precoat femoral component with cement. An average ten-year follow-up study. J Bone Joint Surg Am. 1999February;81(2):247-55. [DOI] [PubMed] [Google Scholar]
- 12.Engh CA, Hopper RH Jr, Engh CA Jr. Long-term porous-coated cup survivorship using spikes, screws, and press-fitting for initial fixation. J Arthroplasty. 2004October;19(7)(Suppl 2):54-60. [DOI] [PubMed] [Google Scholar]
- 13.Della Valle CJ, Mesko NW, Quigley L, Rosenberg AG, Jacobs JJ, Galante JO. Primary total hip arthroplasty with a porous-coated acetabular component. A concise follow-up, at a minimum of twenty years, of previous reports. J Bone Joint Surg Am. 2009May;91(5):1130-5. [DOI] [PubMed] [Google Scholar]
- 14.Lachiewicz PF, Soileau ES. Second-generation modular acetabular components provide fixation at 10 to 16 years. Clin Orthop Relat Res. 2012February;470(2):366-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bobyn JD, Poggie RA, Krygier JJ, Lewallen DG, Hanssen AD, Lewis RJ, Unger AS, O’Keefe TJ, Christie MJ, Nasser S, Wood JE, Stulberg SD, Tanzer M. Clinical validation of a structural porous tantalum biomaterial for adult reconstruction. J Bone Joint Surg Am. 2004;86(Suppl 2):123-9. [DOI] [PubMed] [Google Scholar]
- 16.Bobyn JD, Toh KK, Hacking SA, Tanzer M, Krygier JJ. Tissue response to porous tantalum acetabular cups: a canine model. J Arthroplasty. 1999April;14(3):347-54. [DOI] [PubMed] [Google Scholar]
- 17.Cohen R. A porous tantalum trabecular metal: basic science. Am J Orthop (Belle Mead NJ). 2002April;31(4):216-7. [PubMed] [Google Scholar]
- 18.Unger AS, Lewis RJ, Gruen T. Evaluation of a porous tantalum uncemented acetabular cup in revision total hip arthroplasty: clinical and radiological results of 60 hips. J Arthroplasty. 2005December;20(8):1002-9. [DOI] [PubMed] [Google Scholar]
- 19.Nakashima Y, Mashima N, Imai H, Mitsugi N, Taki N, Mochida Y, Owan I, Arakaki K, Yamamoto T, Mawatari T, Motomura G, Ohishi M, Doi T, Kanazawa M, Iwamoto Y. Clinical and radiographic evaluation of total hip arthroplasties using porous tantalum modular acetabular components: 5-year follow-up of clinical trial. Mod Rheumatol. 2013January;23(1):112-8 Epub 2012 Mar 7. [DOI] [PubMed] [Google Scholar]
- 20.Baad-Hansen T, Kold S, Nielsen PT, Laursen MB, Christensen PH, Soballe K. Comparison of trabecular metal cups and titanium fiber-mesh cups in primary hip arthroplasty: a randomized RSA and bone mineral densitometry study of 50 hips. Acta Orthop. 2011April;82(2):155-60 Epub 2011 Mar 25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ayers DC, Hays PL, Drew JM, Eskander MS, Osuch D, Bragdon CR. Two-year radiostereometric analysis evaluation of femoral head penetration in a challenging population of young total hip arthroplasty patients. J Arthroplasty. 2009September;24(6)(Suppl):9-14. [DOI] [PubMed] [Google Scholar]
- 22.Kärrholm J, Herberts P, Hultmark P, Malchau H, Nivbrant B, Thanner J. Radiostereometry of hip prostheses. Review of methodology and clinical results. Clin Orthop Relat Res. 1997November;(344):94-110. [PubMed] [Google Scholar]
- 23.Bragdon CR, Malchau H, Yuan X, Perinchief R, Kärrholm J, Börlin N, Estok DM, Harris WH. Experimental assessment of precision and accuracy of radiostereometric analysis for the determination of polyethylene wear in a total hip replacement model. J Orthop Res. 2002July;20(4):688-95. [DOI] [PubMed] [Google Scholar]
- 24.Kuzyk PR, Saccone M, Sprague S, Simunovic N, Bhandari M, Schemitsch EH. Cross-linked versus conventional polyethylene for total hip replacement: a meta-analysis of randomised controlled trials. J Bone Joint Surg Br. 2011May;93(5):593-600. [DOI] [PubMed] [Google Scholar]
- 25.Digas G, Kärrholm J, Thanner J, Herberts P. 5-year experience of highly cross-linked polyethylene in cemented and uncemented sockets: two randomized studies using radiostereometric analysis. Acta Orthop. 2007December;78(6):746-54. [DOI] [PubMed] [Google Scholar]
- 26.McCalden RW, MacDonald SJ, Rorabeck CH, Bourne RB, Chess DG, Charron KD. Wear rate of highly cross-linked polyethylene in total hip arthroplasty. A randomized controlled trial. J Bone Joint Surg Am. 2009April;91(4):773-82. [DOI] [PubMed] [Google Scholar]
- 27.Thomas GE, Simpson DJ, Mehmood S, Taylor A, McLardy-Smith P, Gill HS, Murray DW, Glyn-Jones S. The seven-year wear of highly cross-linked polyethylene in total hip arthroplasty: a double-blind, randomized controlled trial using radiostereometric analysis. J Bone Joint Surg Am. 2011April20;93(8):716-22. [DOI] [PubMed] [Google Scholar]
- 28.McCalden RW, Naudie DD, Yuan X, Bourne RB. Radiographic methods for the assessment of polyethylene wear after total hip arthroplasty. J Bone Joint Surg Am. 2005October;87(10):2323-34. [DOI] [PubMed] [Google Scholar]
- 29.Glyn-Jones S, McLardy-Smith P, Gill HS, Murray DW. The creep and wear of highly cross-linked polyethylene: a three-year randomised, controlled trial using radiostereometric analysis. J Bone Joint Surg Br. 2008May;90(5):556-61. [DOI] [PubMed] [Google Scholar]
- 30.Börlin N, Röhrl SM, Bragdon CR. RSA wear measurements with or without markers in total hip arthroplasty. J Biomech. 2006;39(9):1641-50 Epub 2005 Jun 28. [DOI] [PubMed] [Google Scholar]
- 31.Kärrholm J, Snorrason F. Migration of porous coated acetabular prostheses fixed with screws: roentgen stereophotogrammetric analysis. J Orthop Res. 1992November;10(6):826-35. [DOI] [PubMed] [Google Scholar]
- 32.Pijls BG, Nieuwenhuijse MJ, Fiocco M, Plevier JW, Middeldorp S, Nelissen RG, Valstar ER. Early proximal migration of cups is associated with late revision in THA: a systematic review and meta-analysis of 26 RSA studies and 49 survival studies. Acta Orthop. 2012December;83(6):583-91 Epub 2012 Nov 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lachiewicz PF, Hubbard JB, Soileau ES. Polyethylene wear and osteolysis with a new modular titanium acetabular component: results at 7 to 13 years. J Arthroplasty. 2008October;23(7):971-6 Epub 2008 Mar 4. [DOI] [PubMed] [Google Scholar]
- 34.Moen TC, Ghate R, Salaz N, Ghodasra J, Stulberg SD. A monoblock porous tantalum acetabular cup has no osteolysis on CT at 10 years. Clin Orthop Relat Res. 2011February;469(2):382-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Xenakis TA, Macheras GA, Stafilas KS, Kostakos AT, Bargiotas K, Malizos KN. Multicentre use of a porous tantalum monoblock acetabular component. Int Orthop. 2009August;33(4):911-6 Epub 2008 May 29. [DOI] [PMC free article] [PubMed] [Google Scholar]