Abstract
Background
Treatment of overweight and obesity through body weight reduction has been monumentally ineffective as few individuals are able to sustain weight loss. Rather than treating weight gain once it has become problematic, prevention of weight gain over time may be more effective.
Objective
The aim of this research is to preclude the burden of adult obesity in women by identifying the determinants of weight gain prevention. The objective of this randomized controlled trial (RCT) is to compare a weight gain prevention intervention delivered by the registered dietitian versus counselor.
Methods
This is a 12-month parallel-arm weight gain prevention RCT designed to increase self-efficacy, self-regulation, outcome expectations and family and social support through the use of a nutrition education intervention in women, aged 18-45 years, from the Urbana-Champaign (Illinois, USA) area. Women have been randomized to registered dietitian, counselor or wait-list control groups (August 2014) and are undergoing weekly nutrition education sessions for four months, followed by monthly sessions for eight months (through August 2015). Outcome measures, including: (1) dietary intake, (2) physical activity, (3) anthropometric and blood pressure measurements, (4) biochemical markers of health, (5) eating behaviors and health perceptions, and (6) mediators of behavior change, were collected before the intervention began (baseline) and will be collected at 3, 6, 9, and 12 months of the study.
Results
In total, 87 women have been randomized to intervention groups, and 81 women have completed first week of the study. Results are expected in early 2016.
Conclusions
This RCT is one of the first to examine weight gain prevention in women across normal, overweight, and obese body mass index categories. Results of this research are expected to have application to evidence-based practice in weight gain prevention for women and possibly have implication for policy regarding decreasing the encumbrance of overweight and obesity in the United States.
Keywords: body weight, weight gain prevention, weight maintenance, women
Introduction
Adult Weight Management
Small weight gains over time, around 1-2 pounds per year [1,2], contribute to the development of overweight and obesity. Once established, obesity is difficult to treat [3], as reduction of excess body weight is rarely effective in the long term. Short-term weight loss can be achieved by a variety of methods, but few of these approaches are sustainable and effective in facilitating permanent weight loss [4-10]. On average, individuals adhere to weight loss programs for approximately six months [11]; following weight loss, most individuals regain half of the weight lost within one year, and return to baseline weight within 3-5 years [11-13]. Weight gain prevention, on the other hand, avoids the difficulties that may accompany weight loss and its maintenance and offers an alternative option for weight management.
To reduce disease risk and improve overall health, effective weight gain prevention is essential; however, few interventions have successfully examined weight gain prevention and little is known about the determinants of and strategies for preventing weight gain over the long term. Much of the existing research has focused on treatment of overweight and obesity through reduction of excess body weight [14,15] or prevention of weight regain following weight loss [16-20].
Weight Gain Prevention
In the first weight gain prevention trial, normal weight adults, aged 25-74 years, were randomized to an untreated control group or a treatment group that received monthly newsletters plus a financial incentive for weight maintenance for one year [21]. The treatment group experienced an average weight loss of 1 kg, which was significantly different from the control group; with the treatment effect being stronger in men than women [21]. Building upon the Pound of Prevention (POP) work, 3-year weight gain prevention in adults, aged 20-45 years, was investigated [22,23]. Participants were randomized to a no-contact control group or to one of two education groups that received nutrition education via monthly newsletters and semiannual nutrition and exercise classes. One education group received a lottery incentive for participation. Significant differences in weight gain between the control and education groups were not found, although weight-related behaviors did improve in participants receiving education [22,23].
The Shape Program was a medium-intensity behavioral intervention in overweight and class I obese premenopausal black women that included weekly self-monitoring, monthly counseling calls, tailored skills training and a YMCA gym membership and was compared to usual care that included newsletters covering general wellness topics every six months during the 18-month study [24]. After one year, weight loss was significantly greater in the intervention group; these changes were sustained at 18 months. No significant differences in waist circumference, blood pressure, glucose or lipid levels between the intervention and usual care groups were observed at any measurement point during the study [24]. Levine and colleagues [25] randomized normal weight and overweight women to a clinic-based group, a correspondence group or a control group for 24 months. During three years, the intervention had no influence on weight gain in either group; however, age, dieting status, and feelings of hunger were found to be predictive of weight gain.
The Groningen Overweight and Lifestyle (GOAL) study examined weight gain prevention in overweight and obese men and women with hypertension and/or dyslipidemia in the Netherlands by comparing the effects of lifestyle counseling by a nurse practitioner to usual care from a general practitioner during a 1-year period [26]. No significant differences were observed in weight change between groups at one year or after three years [26,27]. Study of Novel Approaches to Weight Gain Prevention (SNAP) is the most recently published intervention [28]. Two novel self-regulation approaches to weight gain prevention—small consistent changes and large periodic changes—were compared to a minimal treatment control for an average of three years of follow-up. Results of this study have not yet been published [28]. Without complete knowledge of the determinants of and strategies for weight gain prevention, public health will remain at risk for complications and costs related to overweight and obesity. Weight gain prevention offers a primary strategy for weight management and obesity prevention [24,26].
Women who previously participated in a weight-loss intervention identified gender-specific life transitions and stressors, including pregnancy, post pregnancy, family responsibilities, health status changes, and aging as precipitators of weight gain [29]. Young adulthood and perimenopause appear to be critical intervals for weight gain [30-32]; therefore, weight gain prevention efforts should target these lifespan stages, specifically in women.
Aims and Objectives
The current study aims to identify determinants of weight gain prevention in young adult and midlife premenopausal women through a 1-year weight gain prevention intervention that includes nutrition education. We hypothesize that compared to a wait-list control group, women who participate in a weight gain prevention intervention designed to increase self-efficacy, self-regulation, outcome expectations, and family and social support will maintain current body weight during a 12-month period. It is further hypothesized that women in an intervention group led by registered dietitians will have less weight gain during 12 months compared to women in an intervention group led by counselors.
Methods
Recruitment, Screening, and Enrollment
Participants were recruited by word-of-mouth, electronic mail messages, and posted flyers from the University of Illinois campus and the Urbana-Champaign (IL, USA) communities. A flow diagram of response, screening, and randomization steps is displayed in Figure 1. A total of 330 women responded to recruitment methods, between June and August 2014. Of these, 266 women met prescreening criteria (appropriate age, body mass index [BMI], and desire to prevent weight gain) and received screening materials including a medical history form, Zung Self-Rating Depression Scale/Status Inventory [33], and informed consent. A total of 146 women returned screening materials, which were reviewed by investigators. One hundred two women met eligibility criteria for participation, and 87 women were randomized, with 81 women completing baseline testing.
Figure 1.
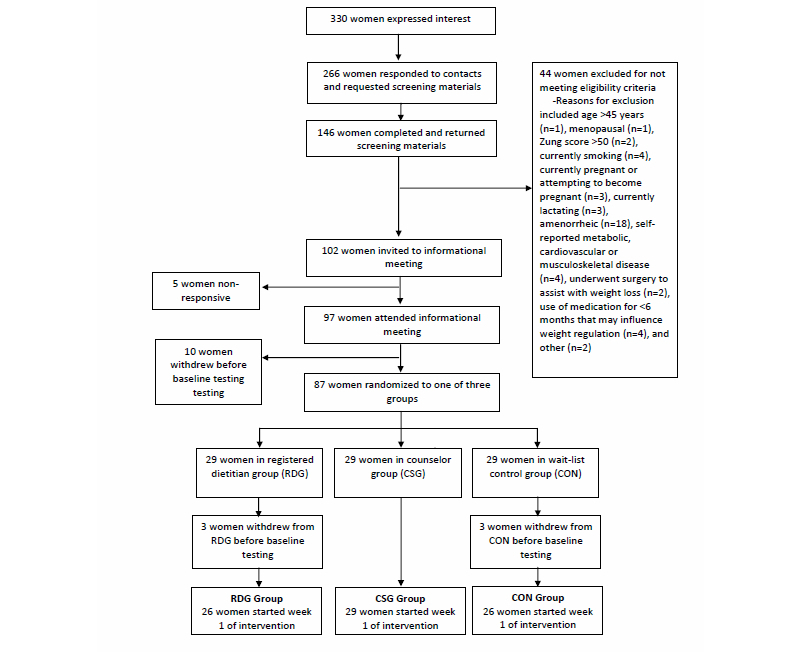
Diagram of recruitment, enrollment and randomization of participants in a study examining weight gain prevention in young adult and midlife women.
The current study included premenopausal women between the ages of 18-45 years with a BMI of >18.5 kg/m2. There were no additional criteria for body weight and BMI to ensure participation by women from a range of weight status categories. Further inclusion criteria included eumenorrhea (≥8 menstrual cycles/year), score of <50 on the Zung Self-Rating Depression Scale/Status Inventory [33], and no self-reported metabolic, cardiovascular or musculoskeletal diseases or use of medications or supplements to manage a chronic health condition. Exclusion criteria included women who currently smoked, were pregnant or attempting to become pregnant or were currently lactating. Women using medications influencing weight regulation, such as steroid or thyroid hormones or oral contraceptives, were excluded if use was for <2 months before the start of the study. Gastric bypass surgery was also an exclusion criterion.
The Institutional Review Board (IRB) for the protection of human subjects at the University of Illinois at Urbana-Champaign (UIUC) approved the study protocol (UIUC IRB#14397). Each participant provided written informed consent before study participation.
Study Design
The current study is a 12-month parallel-arm weight gain prevention randomized controlled trial. After enrollment, women were randomized to one of three intervention groups: (1) weight gain prevention intervention delivered by a registered dietitian (RDG); (2) weight gain prevention intervention delivered by a counselor (CSG), or (3) wait-list control (CON) group. The RDG and CSG weight gain prevention interventions are identical in materials and content; the only difference is the credentialing of the individuals leading the intervention. Women in the CON group receive no intervention; upon completion of the 12-month waiting period, these women will be randomized to the RDG group or CSG group and will receive the respective intervention for the next 12-month period.
Intervention
During the 1-year study, women randomized to the RDG and CSG groups will attend a total of 24, 1-hour nutrition education sessions that are based on effective weight-loss programs/plans which address energy balance through sustainable diet, exercise, and behavior modifications [30,34-39]. These sessions will be held weekly for 16 weeks (months 1-4) and monthly thereafter (months 5-12) [30]. Vegetable consumption, planning ahead for food intake and portion control will be emphasized [34,35], and general nutrition information, eating away from home, food selection, food preparation, and recipe modification also will be addressed [34-37]. Other topics will include fitness and physical activity, culinary skills, breakfast consumption, healthy snacking and beverage choices, nutrient density, family menu planning, and grocery shopping. Problem solving, motivational concerns, and stress management will be encouraged [30,34-39]. Education sessions will relay constructs of the Social Cognitive Theory (SCT) [40].
Education sessions will follow a three-part format. Each session will begin with a brief review of information covered in the previous session and will address participant progress, including successes, challenges and questions. Next, the leader will deliver the nutrition education component of the session using an interactive group discussion format. Participants will be provided with handouts addressing food choices, dietary patterns, menu plans, and other information pertaining to the lesson. Finally, the content for the lesson will be summarized and participants will have a chance to ask questions, address concerns and set specific behavioral goals for the next session. Education sessions will be randomly selected for evaluation by a process observer who will rate the sessions based on investigator-established criteria.
Four registered dietitians will deliver the intervention to women in the RDG group. All women in the RDG group will equally interact with all four registered dietitians during the study. Four counselors will deliver the intervention to women in the CSG group, with these women having equal interaction with all four counselors across the study. The credentials of the professionals delivering the intervention will not be revealed to participants until after completion of the study. The registered dietitians are all female and have been practicing for <5 years. The counselors are all female and are graduate teaching assistants at UIUC in programs unrelated to nutrition or dietetics. Compliance will be defined as attendance of >85% of education sessions. If women are unable to attend an education session, virtual make-up sessions will be offered, along with a quiz. Completion and return of the quiz will indicate that the materials were studied and reviewed and that the participant was compliant.
Outcome Measures
Before the intervention (baseline), data on dietary intake, physical activity, anthropometric, and blood pressure measurements, biochemical markers of health, eating behaviors and health perceptions, and SCT mediators of behavioral change were collected. These outcome measures also will be obtained at 3, 6, 9 and 12 months.
Dietary Intake and Physical Activity Assessment
Participants were taught to accurately complete 4-day food records and the Stanford 7-Day Physical Activity Recall Scale [41]. To ensure accuracy in recording foods and beverage consumption, handouts containing examples of standard serving sizes were provided. Participants recorded all food and beverages consumed for three non-consecutive weekdays and one weekend day before the baseline testing session [35]. Four-day food records will be analyzed using the Nutrition Data System for Research (NDSR) dietary analysis software (Nutrition Coordinating Center, Minneapolis, MN, USA) to estimate average daily dietary intake of total energy (kcal/day), carbohydrate (g/day), protein (g/day), fat (g/day), and fiber (g/day) in addition to intake by food groups (svgs/day).
For seven consecutive days before the baseline testing session, participants recorded the number of hours slept, spent in front of a television or computer screen, and engaged in moderate, hard, and very hard physical activity [35]. Participants wore accelerometers at the waist, wrist, or ankle during all waking hours for seven consecutive days while also recording physical activity to provide an objective assessment of energy expenditure. Approximately 70% of participants in each group wore accelerometers as they were not available for all individuals. Physical activity records will be analyzed by summing total hours of moderate, hard, and very hard activity and dividing by seven to estimate hours of physical activity per day. These records will be further analyzed by converting activities into metabolic equivalents (METs) (hr/d), which will be evaluated as light activity (1-3 METs), moderate activity (>3-6 METs), and vigorous activity (>6 METs) to estimate the number of calories expended per day. Accelerometry data will be analyzed using ActiLife 6.11 (ActiGraph, Pensacola, FL, USA) to estimate the number of calories expended per day, the MET rate per day, and the length of time (minutes) spent in sedentary, light, moderate, vigorous, and very vigorous activities.
Anthropometric and Blood Pressure Measurements
Baseline standing height (cm) was recorded to the nearest 0.1 cm using a calibrated scale-mounted stadiometer (Seca 700, Hanover, MD, USA). Body weight (kg) was measured using a calibrated scale (Tanita 410GS, Arlington Heights, IL, USA) to the nearest 0.1 kg. BMI (kg/m2) was calculated using height and body weight measurements. A retractable measuring tape (Gulik II, Country Technology, Inc, Gay Mills, WI) was used to measure waist (cm) and hip (cm) circumferences, in duplicate, to the nearest 0.1 cm according to standard protocol [34]. Waist circumference was measured at the narrowest point of the waist, approximately one inch above the navel, and hip circumference was measured at the widest part of the buttocks [35]. Waist and hip circumference measurements were averaged to obtain a single value for each site; these values were used to calculate the waist:hip ratio. Fat mass (FM; kg) and body fat percentage (BF%) were measured using a Tanita scale (410GS).
Seated systolic and diastolic blood pressures (mm Hg) were measured by a trained study investigator using a standard sphygmomanometer (Baumanometer® Desk Model, Copiague, NY, USA) following a 5-minute rest period. Blood pressure measurements were taken in duplicate with a 2-3-minute rest period between readings; mean systolic arterial pressure values and diastolic arterial pressure values will be used in data analyses. Resting heart rate was also measured after the 5-minute rest period.
Biochemical Markers of Health
Venous blood samples (~30 mL) were collected by a trained phlebotomist between 7:00 to 9:30 AM after a 12-hour fast. Whole blood samples were processed and stored at -80⁰C. Serum will be analyzed for concentrations of insulin, glucose, total cholesterol, high-density lipoprotein-cholesterol (HDL-C), low-density lipoprotein-cholesterol (LDL-C), triacylglycerides (TG), leptin, adiponectin, and resistin.
Serum insulin (µU/mL) (LINCO Research, St Charles, MO, USA) will be measured using enzyme-linked immunosorbent assay (ELISA), and serum glucose (mg/dL) (Stanbio Labs, Boerne, TX, USA) will be measured by spectrophotometry. Total cholesterol (mg/dL), HDL-C (mg/dL) and TG (mg/dL) concentrations will be measured by spectrophotometry using the total cholesterol, HDL-C and TG kits, respectively (Stanbio Labs). Total cholesterol, HDL-C and TG concentrations will be used to calculate LDL-C concentration (mg/dL) using the equation: LDL-C=total cholesterol - HDL-C - (TG/5) [42]. Serum leptin (ng/mL), adiponectin (ng/mL), and resistin (ng/mL) will be measured using ELISA (R&D Systems, Minneapolis, MN, USA). All serum samples for each biomarker will be analyzed in duplicate at corresponding study intervals. Intra- and inter-assay coefficients of variations (CV) are <15% for all kits.
Eating Behaviors, Health Perceptions, and SCT Mediators of Behavioral Change
Participants completed questionnaires designed to evaluate eating behaviors, health perceptions, perseverance, and SCT mediators. The Eating Inventory [43] will evaluate ratings of cognitive eating restraint, hunger, and disinhibition. The Short-Form 36 Health Survey (SF-36) [44] will assess self-reported health issues. Perseverance will be examined using the Short Grit Scale (Grit-S) [45], and an investigator-designed questionnaire will evaluate SCT mediators, including self-efficacy, outcome expectations, self-regulation, and social and family support. Standard scoring and interpretation methods will be used to evaluate all questionnaires [43-45].
Statistical Analysis
Baseline characteristics of study participants were characterized using descriptive statistics: mean (SD). Participants in the three intervention groups (Treatment) will participate in five data collection sessions at specified intervals (Time). The Shapiro-Wilk test for normality will be used to test for normality and homogeneity of variance within groups; data will be transformed if necessary. Body weight, BMI, waist : hip ratio, FM, BF%, systolic and diastolic blood pressure, serum insulin, glucose, TC, HDL-C, LDL-C, TG, leptin, adiponectin, and resistin will be analyzed as dependent variables. Baseline variables that differ between groups will be included as covariates in the analysis. Dietary intake of macronutrients as estimated from 4-day food records, estimated energy expenditures, eating behaviors, health perceptions, and ratings of SCT mediators also will be compared among groups. A 3 x 5 (3 treatment groups x 5 time intervals) ANOVA with repeated measures on the time factor will be used to assess differences in outcomes within and between treatment groups over time. The group by time interaction will be examined for differences in time trend among intervention groups. Tukey pairwise comparisons will be used in conjunction with ANOVA to detect differences between treatment groups.
Some attrition is expected, as participants may be unable to comply with the intervention or may choose not to continue participation in the study. Participants who withdraw from the intervention will be asked to complete any remaining data collection sessions, and these data will be included in the statistical analyses (ie, intention-to-treat model). Data also will be analyzed using measurements only from those participants who complete all testing sessions. Statistical tests will be two-tailed with significance set at P<.01 to reduce the potential for Type I error. All statistical analyses will be conducted using Statistical Package for the Social Sciences (version 22.0, 2013, IBM Corp, Armonk, NY, USA).
Results
Eighty-one women completed baseline testing. Baseline descriptive characteristics of the sample are displayed in Tables 1 and 2. Overall, these women were highly educated, with a majority of participants having at least a 4-year college degree. The racial/ethnic breakdown was reflective of the larger population, with non-Hispanic whites representing the majority. Age range was 18-45 years, and BMI range was 18.5-49.6 kg/m2. On average, participants were overweight and normotensive. Participants have been recruited, enrolled, and randomized to one of the three intervention groups. Education sessions will continue through August 2015, and results are expected by early 2016.
Table 1.
Baseline characteristics of women (n=81) participating in a 12-month weight gain prevention intervention and completing baseline testing.
| Characteristic | All participants mean (SD) |
| Age (years) | 31.4 (8.1) |
| Height (cm) | 165.2 (5.9) |
| Weight (kg) | 76.1 (19.0) |
| Body mass index (kg/m2) | 27.9 (6.8) |
| Waist circumference (cm) | 83.3 (13.6) |
| Hip circumference (cm) | 110.7 (14.6) |
| Waist: hip ratio | 0.8 (0.1) |
| Body fat (%) | 34.6 (9.1) |
| Fat mass (kg) | 27.9 (14.2) |
| Fat free mass (kg) | 48.2 (5.4) |
| Systolic blood pressure (mmHg) | 106.2 (11.0) |
| Diastolic blood pressure (mmHg) | 70.9 (9.9) |
| Resting heart rate (bpm) | 65.8 (6.0) |
Table 2.
Demographic and education characteristics of all women (n=81) randomized to all groups.
| Characteristic | All participants No (%) |
|
| Education |
|
|
|
|
High school graduate | 2 (3) |
|
|
Some college | 15 (18) |
|
|
2-year associate degree/graduate | 2 (3) |
|
|
4-year college degree/graduate | 21 (26) |
|
|
Some graduate school | 8 (10) |
|
|
Master’s degree | 27 (33) |
|
|
Doctorate degree | 6 (7) |
| Race/ethnicity |
|
|
|
|
White, non-Hispanic | 53 (66) |
|
|
Black, non-Hispanic | 10 (12) |
|
|
Asian | 8 (10) |
|
|
Non-white Hispanic or Latino | 4 (5) |
|
|
Other (including multiracial) | 6 (7) |
| Total annual household income |
|
|
|
|
<$15,000 | 7 (9) |
|
|
$15,000 - $49,999 | 30 (37) |
|
|
$50,000 – $99,999 | 25 (31) |
|
|
>$100,000 – $199,999 | 18 (22) |
|
|
No response | 1 (1) |
After 8 weeks, the halfway point for weekly education sessions, 75 (93%) of the original sample remained in the study. For those randomized to the two intervention groups, 49 (89%) women were still enrolled.
Discussion
Principal Findings
The importance of weight gain prevention and maintenance of current weight has recently been recognized by the American College of Sports Medicine [18] and Healthy People 2020 [46] as critical; yet, there are currently no treatment guidelines for weight gain prevention. The gap in the understanding of the determinants, facilitators, and barriers to weight gain prevention likely exists due to the limited number of studies addressing prospective weight changes in adulthood. Awareness and identification of the determinants of weight gain prevention are necessary in order to increase the practicality of weight gain prevention for managing obesity.
While it may seem counterintuitive to promote weight gain prevention in overweight and obese individuals rather than weight loss, weight gain prevention is relevant for individuals of all BMI categories [47]. Preventing weight gain over time offers the opportunity to slow the progression of overweight and obesity and to avoid further exacerbations related to excess body weight in individuals who are already overweight or obese [48]. Additionally, weight gain prevention may require less intensive treatment than that required to achieve weight loss [2], and may be more successful in the long term as it avoids the problems associated with weight loss and its maintenance [27]. Weight maintenance, regardless of whether an individual is normal weight, overweight or obese, may be more beneficial and practical than repeated, minimally successful weight-loss attempts. While modest weight losses of 5-10% of body weight have significant effects on risk factors of disease, these benefits may be ameliorated with weight regain. Even with weight loss, metabolically healthy obese individuals may not show improvement in health outcomes, and weight loss in these individuals may promote weight cycling, or periods of weight loss followed by weight gain, which may have detrimental effects on mental, metabolic, and psychological outcomes [48-52]. Further, the adverse effects associated with weight cycling may be as harmful as maintenance of a high “unhealthy” body weight [51]. However, a recent study by Mason and colleagues [53] found that weight cycling was not associated with negative metabolic outcomes and a history of weight cycling was not related to the ability to lose and successfully maintain weight in the long term.
In a recent qualitative study of women who completed a weight-loss intervention conducted by a registered dietitian, women perceived the registered dietitian to be a credible source of nutrition information and found lack of access to a registered dietitian following completion of the intervention to be a barrier to weight-loss maintenance [29]. As a credible source of nutrition information [37], registered dietitians have a specialized skill set to support and encourage sustainable behavior changes to achieve weight management. Registered dietitians are generally regarded as the experts in weight management, but no studies have compared registered dietitians to other health professionals in the delivery of weight management information. The current study will fill this scientific gap by testing the ability of the registered dietitian to promote weight gain prevention as compared to an untrained professional. If registered dietitians are more effective in promoting weight gain prevention, these findings will support the notion that registered dietitians should be at the forefront in helping individuals attain successful weight management.
Women in the qualitative study [29] identified social support, basic nutrition education, accountability to others, self-motivation, mindfulness and awareness of food choices, planning ahead, portion control, and exercise as facilitators to weight loss and weight-loss maintenance while health status changes, environmental pressures, life transitions, absence of social support, lack of accountability, and internal factors were perceived as barriers. Additionally, women expressed their desire for continual contact with the registered dietitian as well as the group support offered by the education sessions [29].
Although there is no standardized definition of weight gain prevention or weight maintenance, a weight change of ±3% from baseline weight will be considered successful weight gain prevention. A 3% change criterion allows for normal day-to-day fluctuations that may result from measurement error, clothing, food consumption, and/or fluid balance [54].
Limitations
Results from this study will be limited in generalizability to premenopausal women. Future research should examine pre- and post-menopausal women, as these physiological changes appear to be other critical life stage intervals for weight gain. Weight gain prevention should also be examined exclusively in men, as determinants of and strategies for weight gain prevention may differ between men and women. Further, our results may be limited by the length of the study, as the current intervention is only for one year. Surveys, testing sessions or focus groups following completion of the intervention may be useful in order to garner more information about the feasibility of long-term weight gain prevention. There are limitations with using self-reported dietary intake and physical activity; however, participants have been taught to accurately complete food records, and accelerometry data will be used to validate written physical activity records. Finally, our intervention contains multiple components that address weight gain prevention, and the study design does not allow for examination of independent effects of the different elements of this weight gain prevention intervention. Investigator-designed surveys will be used to assist with determining the effects of individual intervention components.
Conclusions
The current study targets women who are at greater risk for weight gain compared to men; with the goal to help further the understanding of the determinants of weight gain prevention [29]. This study will fill a scientific gap in testing the ability of a registered dietitian to promote weight gain prevention as compared to another health professional that lacks formal nutrition and dietetics training. Although several studies have explored weight gain prevention with limited success, this may be the first study that targets young adult and midlife women of all weight status categories (normal weight, overweight, obese) and focuses on prospective weight gain prevention. Results of this research will be expected to have implications for policy development and recommendations for decreasing the burden of overweight and obesity in the United States through weight gain prevention.
Acknowledgments
This research is supported by a grant from the United States Department of Agriculture, National Institute of Food and Agriculture, Illinois Agricultural Experiment Station, #ILLU-698-337. Graduate research assistantship support is provided by The Hershey Company, Hershey, PA, USA.
Abbreviations
- BF%
body fat percentage
- BMI
body mass index
- CON
control group
- CSG
counselor group
- CV
coefficients of variations
- FM
fat mass
- GOAL
Groningen Overweight and Lifestyle
- Grit-S
Short Grit Scale
- HDL-C
high-density lipoprotein cholesterol
- IRB
Institutional Review Board
- LDL-C
low-density lipoprotein cholesterol
- MET
metabolic equivalent
- NDSR
Nutrition Data System for Research
- POP
Pound of Prevention
- RDG
registered dietitian group
- SCT
social cognitive theory
- SF-36
Short-Form 36 Health Survey
- SNAP
Study of Novel Approaches to Weight Gain Prevention
- TG
triacylglycerides
- UIUC
University of Illinois at Urbana-Champaign
Multimedia Appendix 1
CONSORT-EHEALTH checklist V1.6.2 [55].
Footnotes
Authors' Contributions: CJM and SMN-R contributed equally to the conceptual development, research design, and drafting of the manuscript. CJM was the lead investigator for data collection and analysis, to date. Both authors contributed equally to data interpretation and critical revision of the manuscript.
Conflicts of Interest: CJM discloses Graduate Research Fellowship funding from The Hershey Company. SMN-R discloses research funding from The Hershey Company; the Bell Institute of Health and Nutrition, General Mills, Inc; Dairy Research Institute; and the United States Department of Agriculture. Research funding provided to SMN-R is unrelated to the present study.
References
- 1.Williamson D F, Kahn H S, Remington P L, Anda R F. The 10-year incidence of overweight and major weight gain in US adults. Arch Intern Med. 1990 Mar;150(3):665–72. [PubMed] [Google Scholar]
- 2.Truesdale K P, Stevens J, Lewis C E, Schreiner P J, Loria C M, Cai J. Changes in risk factors for cardiovascular disease by baseline weight status in young adults who maintain or gain weight over 15 years: the CARDIA study. Int J Obes (Lond) 2006 Sep;30(9):1397–407. doi: 10.1038/sj.ijo.0803307. http://europepmc.org/abstract/MED/16534519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gill T P. Key issues in the prevention of obesity. Br Med Bull. 1997;53(2):359–88. doi: 10.1093/oxfordjournals.bmb.a011618. http://bmb.oxfordjournals.org/cgi/pmidlookup?view=long&pmid=9246841. [DOI] [PubMed] [Google Scholar]
- 4.Hill James O, Thompson Helen, Wyatt Holly. Weight maintenance: what's missing? J Am Diet Assoc. 2005 May;105(5 Suppl 1):S63–6. doi: 10.1016/j.jada.2005.02.016. [DOI] [PubMed] [Google Scholar]
- 5.Dansinger Michael L, Gleason Joi Augustin, Griffith John L, Selker Harry P, Schaefer Ernst J. Comparison of the Atkins, Ornish, Weight Watchers, and Zone diets for weight loss and heart disease risk reduction: a randomized trial. JAMA. 2005 Jan 5;293(1):43–53. doi: 10.1001/jama.293.1.43. [DOI] [PubMed] [Google Scholar]
- 6.Gardner Christopher D, Kiazand Alexandre, Alhassan Sofiya, Kim Soowon, Stafford Randall S, Balise Raymond R, Kraemer Helena C, King Abby C. Comparison of the Atkins, Zone, Ornish, and LEARN diets for change in weight and related risk factors among overweight premenopausal women: the A TO Z Weight Loss Study: a randomized trial. JAMA. 2007 Mar 7;297(9):969–77. doi: 10.1001/jama.297.9.969. [DOI] [PubMed] [Google Scholar]
- 7.Shai Iris, Schwarzfuchs Dan, Henkin Yaakov, Shahar Danit R, Witkow Shula, Greenberg Ilana, Golan Rachel, Fraser Drora, Bolotin Arkady, Vardi Hilel, Tangi-Rozental Osnat, Zuk-Ramot Rachel, Sarusi Benjamin, Brickner Dov, Schwartz Ziva, Sheiner Einat, Marko Rachel, Katorza Esther, Thiery Joachim, Fiedler Georg Martin, Blüher Matthias, Stumvoll Michael, Stampfer Meir J, Dietary Intervention Randomized Controlled Trial (DIRECT) Group Weight loss with a low-carbohydrate, Mediterranean, or low-fat diet. N Engl J Med. 2008 Jul 17;359(3):229–41. doi: 10.1056/NEJMoa0708681. [DOI] [PubMed] [Google Scholar]
- 8.Makris Angela, Foster Gary D. Dietary approaches to the treatment of obesity. Psychiatr Clin North Am. 2011 Dec;34(4):813–27. doi: 10.1016/j.psc.2011.08.004. http://europepmc.org/abstract/MED/22098806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sacks Frank M, Bray George A, Carey Vincent J, Smith Steven R, Ryan Donna H, Anton Stephen D, McManus Katherine, Champagne Catherine M, Bishop Louise M, Laranjo Nancy, Leboff Meryl S, Rood Jennifer C, de Jonge Lilian, Greenway Frank L, Loria Catherine M, Obarzanek Eva, Williamson Donald A. Comparison of weight-loss diets with different compositions of fat, protein, and carbohydrates. N Engl J Med. 2009 Feb 26;360(9):859–73. doi: 10.1056/NEJMoa0804748. http://europepmc.org/abstract/MED/19246357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McGuire M T, Wing R R, Klem M L, Seagle H M, Hill J O. Long-term maintenance of weight loss: do people who lose weight through various weight loss methods use different behaviors to maintain their weight? Int J Obes Relat Metab Disord. 1998 Jun;22(6):572–7. doi: 10.1038/sj.ijo.0800627. [DOI] [PubMed] [Google Scholar]
- 11.Goodrick G K, Poston W S, Foreyt J P. Methods for voluntary weight loss and control: update 1996. Nutrition. 1996 Oct;12(10):672–6. doi: 10.1016/s0899-9007(96)00243-2. [DOI] [PubMed] [Google Scholar]
- 12.Jeffery R W, Drewnowski A, Epstein L H, Stunkard A J, Wilson G T, Wing R R, Hill D R. Long-term maintenance of weight loss: current status. Health Psychol. 2000 Jan;19(1 Suppl):5–16. doi: 10.1037/0278-6133.19.suppl1.5. [DOI] [PubMed] [Google Scholar]
- 13.Byrne S, Cooper Z, Fairburn C. Weight maintenance and relapse in obesity: a qualitative study. Int J Obes Relat Metab Disord. 2003 Aug;27(8):955–62. doi: 10.1038/sj.ijo.0802305. [DOI] [PubMed] [Google Scholar]
- 14.Kumanyika Shiriki K, Obarzanek Eva, Stettler Nicolas, Bell Ronny, Field Alison E, Fortmann Stephen P, Franklin Barry A, Gillman Matthew W, Lewis Cora E, Poston Walker Carlos, Stevens June, Hong Yuling, American Heart Association Council on EpidemiologyPrevention‚ Interdisciplinary Committee for Prevention Population-based prevention of obesity: the need for comprehensive promotion of healthful eating, physical activity, and energy balance: a scientific statement from American Heart Association Council on Epidemiology and Prevention, Interdisciplinary Committee for Prevention (formerly the expert panel on population and prevention science) Circulation. 2008 Jul 22;118(4):428–64. doi: 10.1161/CIRCULATIONAHA.108.189702. http://circ.ahajournals.org/cgi/pmidlookup?view=long&pmid=18591433. [DOI] [PubMed] [Google Scholar]
- 15.Lee IM, Djoussé L, Sesso HD, Wang L, Buring JE. Physical activity and weight gain prevention. JAMA. 2010 Mar 24;303(12):1173–9. doi: 10.1001/jama.2010.312. http://europepmc.org/abstract/MED/20332403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Reyes Naomi R, Oliver Tracy L, Klotz Alicia A, Lagrotte Caitlin A, Vander Veur Stephanie S. Virus Amy, Bailer Brooke A, Foster Gary D. Similarities and differences between weight loss maintainers and regainers: a qualitative analysis. J Acad Nutr Diet. 2012 Apr;112(4):499–505. doi: 10.1016/j.jand.2011.11.014. [DOI] [PubMed] [Google Scholar]
- 17.Lowe M R, Miller-Kovach K, Phelan S. Weight-loss maintenance in overweight individuals one to five years following successful completion of a commercial weight loss program. Int J Obes Relat Metab Disord. 2001 Mar;25(3):325–31. doi: 10.1038/sj.ijo.0801521. [DOI] [PubMed] [Google Scholar]
- 18.Donnelly Joseph E, Blair Steven N, Jakicic John M, Manore Melinda M, Rankin Janet W, Smith Bryan K, American College of Sports Medicine American College of Sports Medicine Position Stand. Appropriate physical activity intervention strategies for weight loss and prevention of weight regain for adults. Med Sci Sports Exerc. 2009 Feb;41(2):459–71. doi: 10.1249/MSS.0b013e3181949333. [DOI] [PubMed] [Google Scholar]
- 19.Wing R R, Hill J O. Successful weight loss maintenance. Annu Rev Nutr. 2001;21:323–41. doi: 10.1146/annurev.nutr.21.1.323. [DOI] [PubMed] [Google Scholar]
- 20.McGuire M T, Wing R R, Hill J O. The prevalence of weight loss maintenance among American adults. Int J Obes Relat Metab Disord. 1999 Dec;23(12):1314–9. doi: 10.1038/sj.ijo.0801075. [DOI] [PubMed] [Google Scholar]
- 21.Forster J L, Jeffery R W, Schmid T L, Kramer F M. Preventing weight gain in adults: a pound of prevention. Health Psychol. 1988;7(6):515–25. doi: 10.1037//0278-6133.7.6.515. [DOI] [PubMed] [Google Scholar]
- 22.Jeffery R W, French S A. Preventing weight gain in adults: design, methods and one year results from the Pound of Prevention study. Int J Obes Relat Metab Disord. 1997 Jun;21(6):457–64. doi: 10.1038/sj.ijo.0800431. [DOI] [PubMed] [Google Scholar]
- 23.Jeffery R W, French S A. Preventing weight gain in adults: the pound of prevention study. Am J Public Health. 1999 May;89(5):747–51. doi: 10.2105/ajph.89.5.747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bennett Gary G, Foley Perry, Levine Erica, Whiteley Jessica, Askew Sandy, Steinberg Dori M, Batch Bryan, Greaney Mary L, Miranda Heather, Wroth Thomas H, Holder Marni Gwyther, Emmons Karen M, Puleo Elaine. Behavioral treatment for weight gain prevention among black women in primary care practice: a randomized clinical trial. JAMA Intern Med. 2013 Oct 28;173(19):1770–7. doi: 10.1001/jamainternmed.2013.9263. http://europepmc.org/abstract/MED/23979005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Levine Michele D, Klem Mary Lou, Kalarchian Melissa A, Wing Rena R, Weissfeld Lisa, Qin Li, Marcus Marsha D. Weight gain prevention among women. Obesity (Silver Spring) 2007 May;15(5):1267–77. doi: 10.1038/oby.2007.148. http://europepmc.org/abstract/MED/17495203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.ter Bogt NC, Milder IE, Bemelmans WJ, Beltman FW, Broer J, Smit AJ, van der Meer K. Changes in lifestyle habits after counselling by nurse practitioners: 1-year results of the Groningen Overweight and Lifestyle study. Public Health Nutr. 2011 Jun;14(6):995–1000. doi: 10.1017/S1368980010003708. [DOI] [PubMed] [Google Scholar]
- 27.ter Bogt NC. Bemelmans Wanda JE. Beltman FW, Broer J, Smit AJ, van der Meer Klaas Preventing weight gain by lifestyle intervention in a general practice setting: three-year results of a randomized controlled trial. Arch Intern Med. 2011 Feb 28;171(4):306–313. doi: 10.1001/archinternmed.2011.22. [DOI] [PubMed] [Google Scholar]
- 28.Wing Rena R, Tate Deborah, Espeland Mark, Gorin Amy, LaRose Jessica Gokee, Robichaud Erica Ferguson, Erickson Karen, Perdue Letitia, Bahnson Judy, Lewis Cora E. Weight gain prevention in young adults: design of the study of novel approaches to weight gain prevention (SNAP) randomized controlled trial. BMC Public Health. 2013;13:300. doi: 10.1186/1471-2458-13-300. http://www.biomedcentral.com/1471-2458/13/300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Metzgar C J, Preston A G, Miller D L, Nickols-Richardson S M. Facilitators and barriers to weight loss and weight loss maintenance: a qualitative exploration. J Hum Nutr Diet. 2014 Sep 18; doi: 10.1111/jhn.12273. [DOI] [PubMed] [Google Scholar]
- 30.Wing RR. Changing diet and exercise behaviors in individuals at risk for weight gain. Obes Res. 1995 Sep;3 Suppl 2:277s–282s. doi: 10.1002/j.1550-8528.1995.tb00474.x. [DOI] [PubMed] [Google Scholar]
- 31.Ball K, Brown W, Crawford D. Who does not gain weight? Prevalence and predictors of weight maintenance in young women. Int J Obes Relat Metab Disord. 2002 Dec;26(12):1570–8. doi: 10.1038/sj.ijo.0802150. [DOI] [PubMed] [Google Scholar]
- 32.Wane Sarah, van Uffelen Jannique G Z. Brown Wendy. Determinants of weight gain in young women: a review of the literature. J Womens Health (Larchmt) 2010 Jul;19(7):1327–40. doi: 10.1089/jwh.2009.1738. [DOI] [PubMed] [Google Scholar]
- 33.Zung WWK, Sartorius N, Ban TA. Zung self-rating depression scale and depression status inventory. Berlin: Springer; 1986. Assessment of depression; pp. 221–231. [Google Scholar]
- 34.Piehowski KE, Preston AG, Miller DL, Nickols-Richardson SM. A reduced-calorie dietary pattern including a daily sweet snack promotes body weight reduction and body composition improvements in premenopausal women who are overweight and obese: a pilot study. J Am Diet Assoc. 2011 Aug;111(8):1198–203. doi: 10.1016/j.jada.2011.05.013. http://europepmc.org/abstract/MED/21802567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Nickols-Richardson Sharon M, Piehowski Kathryn E, Metzgar Catherine J, Miller Debra L, Preston Amy G. Changes in body weight, blood pressure and selected metabolic biomarkers with an energy-restricted diet including twice daily sweet snacks and once daily sugar-free beverage. Nutr Res Pract. 2014 Dec;8(6):695–704. doi: 10.4162/nrp.2014.8.6.695. http://e-nrp.org/DOIx.php?id=10.4162/nrp.2014.8.6.695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lutes Lesley D, Winett Richard A, Barger Steven D, Wojcik Janet R, Herbert William G, Nickols-Richardson Sharon M, Anderson Eileen S. Small changes in nutrition and physical activity promote weight loss and maintenance: 3-month evidence from the ASPIRE randomized trial. Ann Behav Med. 2008 Jun;35(3):351–7. doi: 10.1007/s12160-008-9033-z. [DOI] [PubMed] [Google Scholar]
- 37.Slawson Deborah Leachman, Fitzgerald Nurgul, Morgan Kathleen T. Position of the Academy of Nutrition and Dietetics: the role of nutrition in health promotion and chronic disease prevention. J Acad Nutr Diet. 2013 Jul;113(7):972–9. doi: 10.1016/j.jand.2013.05.005. [DOI] [PubMed] [Google Scholar]
- 38.Perri MG, Limacher MC, Durning PE, Janicke DM, Lutes LD, Bobroff LB, Dale MS, Daniels MJ, Radcliff TA, Martin AD. Extended-care programs for weight management in rural communities: the treatment of obesity in underserved rural settings (TOURS) randomized trial. Arch Intern Med. 2008 Nov 24;168(21):2347–54. doi: 10.1001/archinte.168.21.2347. http://europepmc.org/abstract/MED/19029500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Knowler William C, Barrett-Connor Elizabeth, Fowler Sarah E, Hamman Richard F, Lachin John M, Walker Elizabeth A, Nathan David M, Diabetes Prevention Program Research Group Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002 Feb 7;346(6):393–403. doi: 10.1056/NEJMoa012512. http://europepmc.org/abstract/MED/11832527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bandura A. Social foundations of thought and action: a social cognitive theory. Englewood Cliffs, N.J: Prentice-Hall; 1986. [Google Scholar]
- 41.Richardson M T, Ainsworth B E, Jacobs D R, Leon A S. Validation of the Stanford 7-day recall to assess habitual physical activity. Ann Epidemiol. 2001 Feb;11(2):145–53. doi: 10.1016/s1047-2797(00)00190-3. [DOI] [PubMed] [Google Scholar]
- 42.Friedewald W T, Levy R I, Fredrickson D S. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972 Jun;18(6):499–502. http://www.clinchem.org/cgi/pmidlookup?view=long&pmid=4337382. [PubMed] [Google Scholar]
- 43. Stunkard- A, McLaren-Hume M. The results of treatment for obesity: a review of the literature and report of a series. AMA Arch Intern Med. 1959 Jan;103(1):79–85. doi: 10.1001/archinte.1959.00270010085011. [DOI] [PubMed] [Google Scholar]
- 44.Keller S D, Bayliss M S, Ware J E, Hsu M A, Damiano A M, Goss T F. Comparison of responses to SF-36 Health Survey questions with one-week and four-week recall periods. Health Serv Res. 1997 Aug;32(3):367–84. http://europepmc.org/abstract/MED/9240286. [PMC free article] [PubMed] [Google Scholar]
- 45.Duckworth Angela Lee, Quinn Patrick D. Development and validation of the short grit scale (grit-s) J Pers Assess. 2009 Mar;91(2):166–74. doi: 10.1080/00223890802634290. [DOI] [PubMed] [Google Scholar]
- 46.US Department of Health and Human Services: Healthy People 2020 . Washington, DC: [2014-10-10]. Office of Disease Prevention and Health Promotion http://www.healthypeople.gov/2020/topicsobjectives2020/objectiveslist.aspx?topicId=29[accessed. [Google Scholar]
- 47.Durward C M, Hartman T J, Nickols-Richardson S M. All-cause mortality risk of metabolically healthy obese individuals in NHANES III. J Obes. 2012;2012:460321. doi: 10.1155/2012/460321. http://dx.doi.org/10.1155/2012/460321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.St Jeor ST. Brunner RL, Harrington ME, Scott BJ, Daugherty SA, Cutter GR, Brownell KD, Dyer AR, Foreyt JP. A classification system to evaluate weight maintainers, gainers, and losers. J Am Diet Assoc. 1997 May;97(5):481–488. doi: 10.1016/S0002-8223(97)00126-0. [DOI] [PubMed] [Google Scholar]
- 49.Kayman S, Bruvold W, Stern J S. Maintenance and relapse after weight loss in women: behavioral aspects. Am J Clin Nutr. 1990 Nov;52(5):800–7. doi: 10.1093/ajcn/52.5.800. http://www.ajcn.org/cgi/pmidlookup?view=long&pmid=2239754. [DOI] [PubMed] [Google Scholar]
- 50.Jeffery RW. Does weight cycling present a health risk? Am J Clin Nutr. 1996 Mar;63(3 Suppl):452S–455S. doi: 10.1093/ajcn/63.3.452. http://www.ajcn.org/cgi/pmidlookup?view=long&pmid=8615341. [DOI] [PubMed] [Google Scholar]
- 51.Vergnaud A-C, Bertrais S, Oppert J-M, Maillard-Teyssier L, Galan P, Hercberg S, Czernichow S. Weight fluctuations and risk for metabolic syndrome in an adult cohort. Int J Obes (Lond) 2008 Feb;32(2):315–21. doi: 10.1038/sj.ijo.0803739. [DOI] [PubMed] [Google Scholar]
- 52.French S A, Jeffery R W, Folsom A R, McGovern P, Williamson D F. Weight loss maintenance in young adulthood: prevalence and correlations with health behavior and disease in a population-based sample of women aged 55-69 years. Int J Obes Relat Metab Disord. 1996 Apr;20(4):303–10. [PubMed] [Google Scholar]
- 53.Mason Caitlin, Foster-Schubert Karen E, Imayama Ikuyo, Xiao Liren, Kong Angela, Campbell Kristin L, Duggan Catherine R, Wang Ching-Yun, Alfano Catherine M, Ulrich Cornelia M, Blackburn George L, McTiernan Anne. History of weight cycling does not impede future weight loss or metabolic improvements in postmenopausal women. Metabolism. 2013 Jan;62(1):127–36. doi: 10.1016/j.metabol.2012.06.012. http://europepmc.org/abstract/MED/22898251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Stevens J, Truesdale K P, McClain J E, Cai J. The definition of weight maintenance. Int J Obes (Lond) 2006 Mar;30(3):391–9. doi: 10.1038/sj.ijo.0803175. [DOI] [PubMed] [Google Scholar]
- 55.Eysenbach Gunther, Consort- EHEALTHGroup. CONSORT-EHEALTH: improving and standardizing evaluation reports of Web-based and mobile health interventions. J Med Internet Res. 2011;13(4):e126. doi: 10.2196/jmir.1923. http://www.jmir.org/2011/4/e126/ [DOI] [PMC free article] [PubMed] [Google Scholar]


