Abstract
Background
Having a visual, hearing or physical impairment (defined as problems in body function or structure) may adversely influence the mental well-being of military personnel. This paper reviews the existing literature regarding the prevalence of mental health problems among (ex-)military personnel who have a permanent, predominantly, physical impairment.
Method
Multiple electronic literature databases were searched for relevant studies (EMBASE (1980–January 2014), MEDLINE (1946–January 2014), PsycINFO (2002–January 2014), Web of Science (1975–January 2014)).
Results
25 papers were included in the review, representing 17 studies. Studies conducted among US military personnel (n=8) were most represented. A range of mental health disorders were investigated; predominately post-traumatic stress disorder (PTSD), but also depression, anxiety disorder (excluding PTSD), psychological distress and alcohol misuse. The findings indicate that mental health disorders including PTSD (range 2–59%), anxiety (range 16.1–35.5%), depression (range 9.7–46.4%) and psychological distress (range 13.4–36%) are frequently found whereby alcohol misuse was least common (range 2.2–26.2%).
Conclusions
Common mental health disorders were frequently identified among (ex-)military personnel with a physical impairment. Adequate care and support is necessary during the impairment adaptation process to facilitate the psychosocial challenges (ex-)military personnel with an impairment face. Future research should be directed into factors impacting on the mental well-being of (ex-)military personnel with an impairment, how prevalence rates vary across impairment types and to identify and act on specific needs for care and support.
Keywords: anxiety, disability, military, depression, post-traumatic stress disorder
Background
In the past decade, the proportion of military personnel who died during a conflict decreased due to technological and medical progression, including protective gear and equipment, the rapid removal of severely injured personnel from the battlefield and increased use of military tourniquets.1–4 Consequently, combat-related morbidity among those returning from conflicts increased.4 5 Furthermore, it has been posited that military personnel who have served in the conflicts in Iraq or Afghanistan are more likely to sustain particular impairments than personnel who have served in other conflicts as a result of the increased use of improvised explosive devices.6–8 Wounds to the extremities are common, which may result in amputations.9 Besides amputations, other impairments are reported including vision or hearing loss and head injury.10
Recent studies assessed the mental well-being of the US and UK troops that have been deployed to Iraq and Afghanistan, suggesting that the rates of mental health problems vary but are substantial.11–13 We know that combat-related trauma experienced while on deployment is a risk factor for mental or physical health problems.11 14 15 Studies among military personnel from the US, UK and Israel suggest that, compared to uninjured personnel, those injured during deployment have significantly higher rates of post-traumatic stress disorder (PTSD).14–17 Wounded or injured US soldiers were also more likely to misuse alcohol or be diagnosed with any mental health disorders (eg, PTSD, anxiety, mood, adjustment, substance abuse).17 18 However, no increased prevalence of mental health disorders other than PTSD was identified among the UK sample.14 Furthermore, the physical and psychological issues of adapting to a life with an impairment may affect the well-being of the person.19–21
This paper reviews the prevalence of mental health disorders among, mainly physically, permanently impaired (ex-)military personnel.
Methods
Papers were retrieved from EMBASE (1980–January 2014), MEDLINE (1946–January 2014), PsycINFO (2002–January 2014) and Web of Science (1975–January 2014). A combination of the following search terms was used: ‘army’, ‘veteran’, ‘soldier’, ‘military personnel’, ‘armed forces’, ‘combat experience’, ‘military deployment’, combined with: ‘disability’, ‘disabled persons’, ‘impairment’, ‘hearing disorder’, ‘vision disorder’, ‘amputees’, ‘communication disorder’, combined with: ‘mental disorder’, ‘mental health’, ‘anxiety disorder’, ‘suicidal ideation’, ‘suicidal behaviour’, ‘post-traumatic stress disorder’, ‘mood disorder’, ‘depression’. The search was finalised in January 2014. See the online supplementary file for an example of the search strategy used.
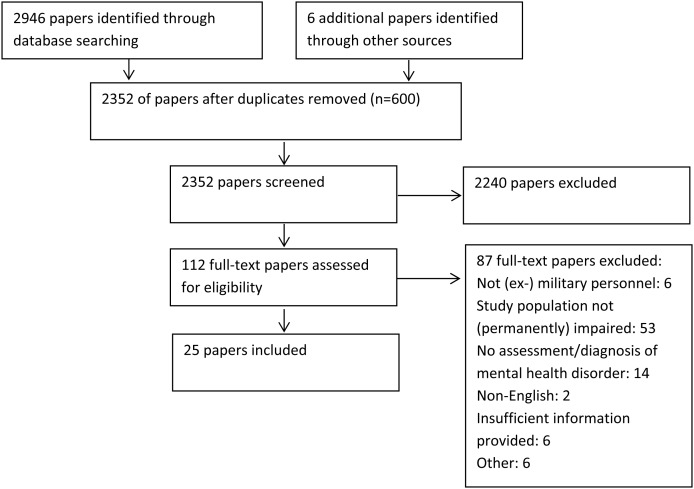
A total of 2946 papers were identified during the initial searches. Papers were included if they: (1) comprised data on (ex-)military personnel with a physical, visual or hearing impairment, (2) administered at least one validated outcome measure of mental health or participants self-reported to have a mental health problem, or hospital records/military databases indicated the presence of a mental health problem, and (3) were reported in English.
In the current review, impairment was defined as ‘problems in body function or structure such as significant deviation or loss’.22 We used the terms visual and hearing impairment to refer to problems with vision and hearing, respectively, whereas a physical impairment included problems with extremities, mobility, spinal cord injury or missing limbs. A permanent impairment suggests an impairment that supposedly will not improve and remains for life including amputations, irreversible vision and hearing loss. It was not possible to use more stringent criteria for the different types of impairment as often limited detail about the impairment was provided in the studies published. We aimed to review studies including a variety of impairment types. However, the majority of the studies identified focused on physically impaired participants; this is therefore the main focus of the current review paper. The term (ex-)military personnel included those currently serving in the Armed Forces and those who had now left the Forces and returned to civilian life (often referred to as veterans).
After a first selection by SAMS, based on title and abstract, the remaining 112 papers were read in full by SAMS and EMM and assessed for inclusion in the review. Any discrepancies were discussed. Also the bibliographies of the selected papers were scanned for eligible studies.
A quality scoring methodology was used to critically appraise the studies included. This methodology was derived from a framework for critical appraisal.23 The quality score was calculated based on five criteria with a highest possible score of 5 and 0 as the lowest possible score. A high score indicated a better quality study. The criteria included; (1) clear statement of aims/description of target population: yes (score 1), no (score 0); (2) sample: random sampling (score 1), non-random sampling for example, opportunity or self-selected (score 0); (3) sample size >1000 (score 1), <1000 (score 0); (4) response rate/follow-up rate >60% (score 1), <60% or not stated (score 0); (5) use of standardised/validated measures yes (score 1), no (score 0). The studies were independently appraised by CM and SJ and the results compared. Any discrepancies were discussed with SS and a consensus was reached. Final quality scores are shown in online supplementary table S2.
Forest plots were created to provide an overview of the prevalence estimations from the different studies per mental health disorder. This was carried out using the Forest Plot Viewer Graphing Tool.24 The different impairment groups identified in the various studies and the few studies that included a control group are represented in the forest plots. Reference lines have been added in the forest plots at baseline (0%) and first quartile (25%) to guide the reader.
Results
A total of 2946 papers were identified during the initial searches. After removing the duplicates, 2352 papers were screened. Based on title and abstract, 2240 papers were excluded and 112 full-text papers were assessed (figure 1). Twenty-five papers were included in the review, based on 17 different studies (see table 1). Eight studies were based on a sample of US (ex-)military personnel.10 25–36 The other studies were conducted in Sri Lanka (3),37–39 Croatia (2),40–42 Iran (1),43 Korea (1),44 Nicaragua (1)45 and the UK (1).19 46 The design of the studies varied. Seven cross-sectional surveys were identified,10 19 20 26 34–37 39 41 43 46 five case–control studies30 31 38 42 44 45 47 four studies that analysed hospital records and/or military databases,27–29 32 33 and there was one cohort study.25 Out of the 17 studies, seven included male and female (ex-)military personnel.10 20 25–29 32 33 35 36
Figure 1.
Article selection strategy.
Table 1.
Overview of the studies included (alphabetical order)
| Authors, year of publication | Study design | Sample | Health measures | |||||
|---|---|---|---|---|---|---|---|---|
| Overall sample size | Number of respondents* | Response rate | Country | Service status | Deployment | |||
| Abeyasinghe et al, 2012 | Cross-sectional survey | Not reported | 96 | 88.9% | Sri Lanka | Active duty | Sri Lankan Civil War | 1. PTSD screening questionnaire† |
| Abrams et al, 2006 | Cohort | Not reported | Total: 493 123 with hearing impairment 370 controls |
Not reported | US | Not reported | Not reported | 1. ICD-9-CM 2. SF (8-item) 3. IADLs |
| Boakye et al, 2013 | Analysis of records | NA | 168 | NA | US | Veterans | Not reported | 1. Self-reported depression, PTSD, substance abuse 2. BDI 3. SF (12 item) |
| Delimar et al, 1998 Sivik et al, 2000 | Case–control | Not reported | Total: 90 (30 disabling injuries; 30 non-disabling injuries; 30 active soldiers) Total: 120 (30 non-disabling injuries; 30 permanent disabling injuries; 30 active soldiers; 30 recruits not exposed to combat) |
Not reported | Croatia | Veterans Active duty ≥3 months combat experience‡ |
Croat-Bosniak War | 1. CIDI-PTSD interview 2. MMPI (4 subscales) 3. PTSS 4. IES |
| Desmond et al, 2006, Desmond 2007 | Cross-sectional survey | 2500 questionnaires distributed 1222 returned |
582 138§ |
49% | UK | Not reported | Majority World War II | 1. HADS 2. IES 3. CSI 4. TAPES |
| Doukas et al, 2013 | Cross-sectional survey | 868 | 324 | 59.8% | US | Active duty Reservists |
Iraq Afghanistan |
1. CESD-R 2. PCL-M |
| Ebrahimzadeh et al, 2009 | Cross-sectional survey | 200 | 31 | Not reported | Iran | Active duty | Iraq–Iran War | 1. self-reported mental health disorders |
| Fagelson et al, 2007 | Analysis of records | NA | 300 | NA | US | Not reported | Not reported | 1. Clinical Diagnosis DSMI-IV 2. M-PTSD 3. THI 4. TSI |
| Gregurek et al, 1996 | Cross-sectional survey | 60 | 53 | Not reported | Croatia | Active duty | Croatian War of Independence | 1. Clinical interview PTSD 2. M-PTSD 3. STAI |
| Gunawardena et al, 2007 | Case–control | Not reported | Total 922: 461 amputee soldiers 461 non-amputee controls |
98.3% amputee soldiers; 97.6% non-amputees controls | Sri Lanka | Active duty | Not reported | 1. GHQ-30 2. BSI 3. CAGE |
| Hume et al, 1994 | Case–control | Not reported | Total 133: 72 war-wounded (ex-)service personnel 10 severely disabled ex-Contra- guerrillas¶ 51 non-war-wounded (ex-)service personnel |
Not reported | Nicaragua | Active duty | Contra War Nicaragua | 1. GHQ-28 2. Clinical assessment PTSD |
| Kasturiaratchi et al, 2004 | Cross-sectional survey | 430 | 408 | Not reported | Sri Lanka | Active duty | Not reported | 1. GHQ-30 2. BSI 3. self-reported alcohol consumption |
| Kim et al, 2006 | Case–control | 135 | Total 132: 56 LDH conscripts (of which 49 complete data) 76 healthy conscripts |
Not reported | Korea | NA | Not reported | 1. VAS 2. BDI 3. STAI 4. MINI5. 5. mOSW |
| Martz et al, 2001 | Analysis of records/Case–control | NA | 45 320 | NA | US | Veterans | Not reported | 1. PTSD clinical diagnosis 2. ICD-9 Codes |
| Melcer et al, 2010, Melcer et al, 2013 | Analysis of records | NA | 382 656** |
NA | US | Active duty | Iraq Afghanistan |
1. ICD-9 Codes |
| Radnitz et al, 1998, Radnitz et al, 1998 | Case–control | 181 | Total: 140 97 veterans with spinal cord injuries (of which 45 paraplegic and 52 quadriplegic) 43 veterans with non-spinal cord injuries |
Not reported | US | Veterans | Not reported | 1. CAPS 2. SCID 3. IES 4. MMSE 5. TSRS |
| Reiber et al, 2010, Epstein et al, 2010, Dougherty et al, 2011 Dougherty et al, 2012, Katon et al, 2013 |
Cross-sectional survey | 1042 identified 940 contacted |
581 579†† 134 33 283‡‡ |
65.1% Vietnam war veterans; 58.7% OIF/OEF veterans 61.8% overall |
US | Active duty Reserves Veterans |
Vietnam War Iraq Afghanistan |
1. SF-36 2. QOL 3. self-reported mental health disorders 4. OPUS 5. PEQ |
*For all the studies the overall number of participants has been reported. In a few cases also the number of participants per specific impairment type has been described.
†Based on the Impact of Event Scale and PTSD symptom Scale.
‡Not professional trained soldiers but had joined the war by spontaneously defending their homes.
§Subsample of the Desmond and MacLachlan46 studies. Only selected participants with an upper-limb amputation.
¶Ex-contra guerrillas refer to soldiers who fought against the Nicaraguan government (and their government soldiers).
**Study population from Melcer et al29 combined with a group of soldiers with serious extremity injuries without amputation.
††Reporting on the same study sample or only reporting on a subsample.
‡‡Reporting on the OIF/OEF subsample from Reiber et al.20
BDI, Beck Depression Inventory; BSI, Bradford Somatic Inventory; CAGE, Screening Test for Alcohol Dependence (CAGE); CAPS, Clinician Administered PTSD Scale; CESD-R, Revised Center for Epidemiologic Studies Depression Scale; CIDI-PTSD, Composite International Diagnostic Interview—PTSD; CSI, coping strategy indicator; DSM, Diagnostic and Statistical Manual; GHQ, General Health Questionnaire; IADLs, instrumental activities of daily living; ICD, International Classification of Disease Codes; ICD-9-CM, International Classification of Disease, Ninth Revision, Clinical Modification Codes; IES, Impact of Event Scale; HADS, Hospital Anxiety and Depression Scale; LDH, lumbar disc herniation; MINI, Mini-International Neuropsychiatric Interview; MMPI, Minnesota Multiphasic Personality Inventory (Hypochondriasis, Depression, Hysteria, Alexithymia); mOSW, Modified Oswestry Low Back Pain Disability Questionnaire; MMSE, Mini-Mental State Examination;M-PTSD, Mississippi Scale for Combat-Related PTSD; NA, not applicable; OIF, Operation Iraqi Freedom; OEF, operation enduring freedom; OPUS, Orthotic and Prosthetic User's Survey; PEQ, Prosthetic Evaluation Questionnaire; PTSD, post-traumatic stress disorder; PCL, PTSD Checklist Military version; PTSS, Post-Traumatic Symptom Scale; QOL, single item measure of Quality of Life; SCI, spinal cord injury; SCID, Structured Clinical Interview for DSM-III-R; SF, Short-Form Health Survey; STAI, State-Trait Anxiety Inventory; TAPES, Trinity Amputation and Prosthesis Experience Scales; THI, Tinnitus Handicap Inventory; TSI, Tinnitus Severity Index; TSRS, Trauma Severity Rating Scale; VAS, Visual Analogue Scale (pain).
The majority of the studies involved (ex-)military personnel with a physical impairment, such as an extremity amputation or spinal cord injury.19 28–34 36–38 41–44 46 47 Two studies focused solely on hearing impairments25 27 and three studies included participants with a range of impairments, including physical, vision and hearing impairment.10 20 26 39 45 A wide variety of diagnostic and screening measures were used as well as data records and self-report, to identify a variety of mental health disorders (table 1).
Online supplementary table S2 summarises the findings, limitations and quality score of the included studies. The majority of the studies investigated the prevalence of PTSD (n=13),10 20 26–37 41 43 45–47 followed by depression (n=9),10 19 20 25 26 29 32 34–36 42–44 46 anxiety (n=5),19 29 41 43 44 46 substance misuse (n=5)29 32 38 39 45 and psychological distress (n=3).32 38 39 45 The majority of the papers received a quality score of 2 (n=14), followed by a quality score of 3 (n=9) and 1 (n=2) (see online supplementary table S2).
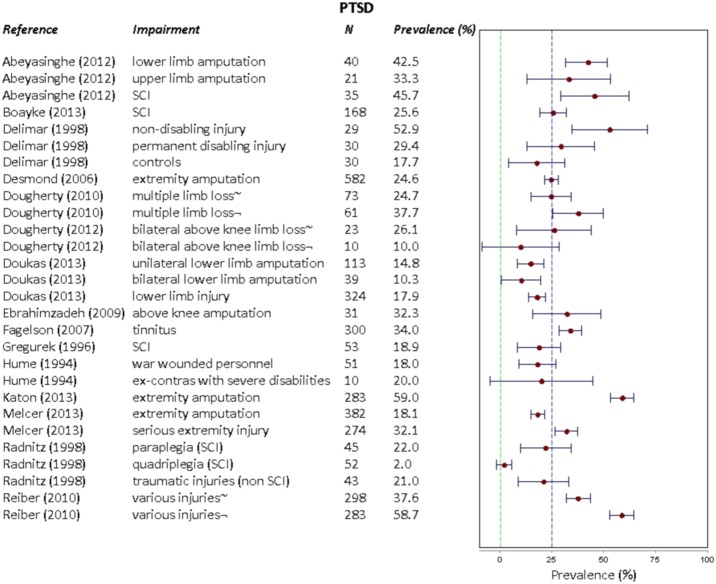
Post-traumatic stress disorder
Overall, the prevalence of PTSD was highest in a study of US military personnel with different types of amputations that returned from deployment in Iraq or Afghanistan; 59% self-reported suffering from PTSD (total sample size n=283).35 The lowest prevalence of PTSD was identified among quadriplegic US military personnel (2%; n=52).30 In a study of 89 Croatian soldiers, those with non-disabling injuries had a higher prevalence of PTSD, 52.9% (n=29), followed by those with a permanent disabling injury (at least one extremity amputation) (29.4%; n=30)47 and soldiers who were still actively serving (17.7%; n=30).47
The only study that examined the prevalence of PTSD among soldiers with a hearing impairment suggested that 34% of the US soldiers (n=300) fulfilled the criteria for probable PTSD27 (figure 2).
Figure 2.
Forest plot describing the prevalence of post-traumatic stress disorder PTSD across studies. ∼ Vietnam veterans. ¬ Service personnel who were deployed on Operation Iraqi Freedom (OIF)/Operation Enduring Freedom (OEF). SCI, spinal cord injury.
Depression
Levels of self-reported depression were highest among US veterans with a spinal cord injury (46.4%; n=168), compared to a study among Iran soldiers with a lower limb amputation (9.7%; n=31).32 43 However, the former also filled in the Beck Depression Inventory, resulting in a smaller proportion moderately or severely depressed; 40%.32 In addition, depression levels were high among 49 Korean conscripts with lumbar disc herniation, 40.8%.44
Abrams and colleagues found that 29.3% (n=123) of US veterans with a hearing impairment were depressed whereas 6.5% of the controls, US veterans without a hearing impairment, were depressed (n=370).25 In a separate study, military personnel with hearing loss were not more likely to report depression compared to those without hearing loss20 (figure 3).
Figure 3.
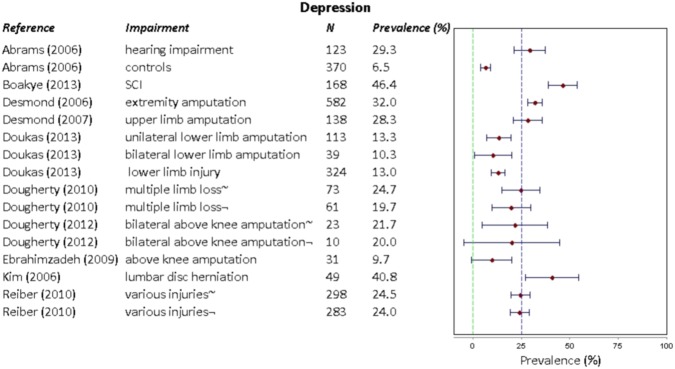
Forest plot describing the prevalence of depression across studies. ∼ Vietnam veterans. ¬ Service personnel who were deployed on Operation Iraqi Freedom (OIF)/Operation Enduring Freedom (OEF). SCI, spinal cord injury.
Anxiety
The levels of probable anxiety disorder ranged from 16.1% to 35.5% among Iranian soldiers with above knee amputations (self-reported anxiety; n=31)43 and UK service men (n=138)19 with an upper limb amputation, respectively. Among UK soldiers with an extremity amputation, the diagnosis of probable clinical anxiety was considerable, 34% (n=582;46 figure 4).
Figure 4.
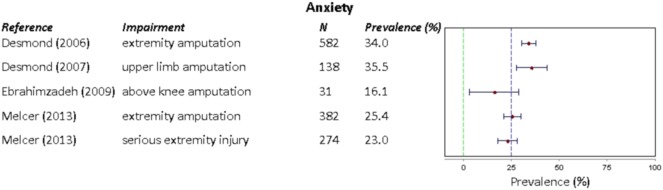
Forest plot describing the prevalence of anxiety across studies.
Substance misuse
More than a quarter of US veterans with a spinal cord injury self-reported alcoholism or intravenous drug use (26.2%; n=168).32 Gunawardena et al,38 suggested that only 2.2% (n=461) of the Sri Lankan soldiers with amputations had a substance abuse problem compared to 0.7% (n=461) of the controls (non-amputee civilians; figure 5).
Figure 5.
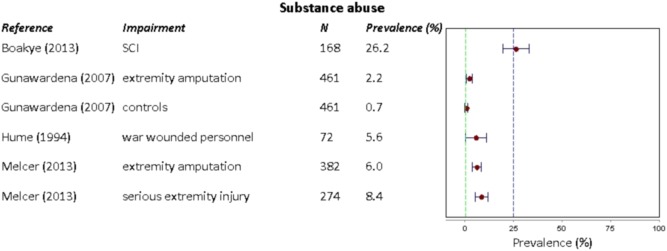
Forest plot describing the prevalence of substance abuse (alcohol and/or drug use) across studies. SCI, spinal cord injury.
Psychological and somatic symptoms of distress
Levels of psychological distress were higher among Sri Lankan soldiers who had undergone an amputation (36%; n=461), compared to healthy controls (8.9%; n=461).38 Another study among permanently disabled Sri Lankan soldiers (n=408) suggested that a positive General Health Questionnaire score, measuring psychological distress, was associated with increased alcohol consumption.39 A study conducted in Nicaragua suggested that war-wounded soldiers (n=72) were more likely to be identified with probable psychological distress (33.3%) compared to those not wounded (9.8%; n=51;45 see online supplementary table S2; figure 6).
Figure 6.
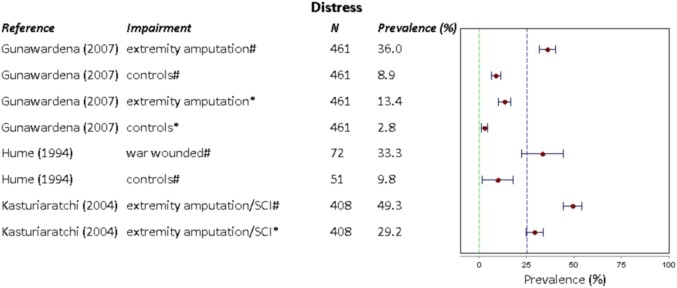
Forest plot describing the prevalence of distress (psychological or somatic) across studies.
Discussion
Principal findings
We identified 25 papers, reflecting 17 studies, which reported on the association between having predominantly a physical impairment and mental health problems among (ex-)military personnel. Overall, the reviewed studies indicate that mental health disorders including PTSD (range 2–59%), anxiety (range 16.1–35.5%), depression (range 9.7–46.4%) and psychological distress (range 13.4–36%) are prevalent and highly variable among (ex-)military personnel with an impairment. Substance misuse was less common, but still present (range 2.2–26.2%).
Strengths and weaknesses
A strength of the study was the search of four literature databases using a broad search strategy. Furthermore, the eligibility assessment of full-text articles and the critical appraisal of the studies included by two independent reviewers also strengthened the review. The present review has several weaknesses. First, only English language papers were included in the review. Second, the majority of the studies only investigated the mental well-being of personnel with an impairment at one point in time. Therefore, no causal inference can be made whether becoming impaired triggered or contributed to the development of mental health problems. Longitudinal studies following military personnel over time may provide more insight in the actual process of coping and adaptation when becoming impaired. Third, the type of measures used to assess mental health problems as well as cut-off points for diagnostic criteria varied widely, and findings are difficult to compare. However, combining these papers in a single review contributes to the broader understanding. Fourth, studies often lacked information that would have been helpful for the contextualisation and interpretation of the findings. For example, time since being impaired, actual cause of impairment, service arm, rank and details on combat exposure were often missing. Finally, the sample size of studies varied (range n=31–45 320) as well as the selection procedures and study populations. The above limitations are also reflected in a poor to moderate quality score of the studies (average 2.3). Owing to the heterogeneity of the studies included, the current review provides a broad overview on the impact of impairment on the mental well-being in different military populations and provides directions for future research. Despite these limitations, the review has implications as military personnel are currently coming back with service attributable injuries and their physical and mental health needs careful consideration.
Comparison literature
There is a wealth of information on the prevalence of mental health disorders in military personnel. Therefore, we will only compare our results with the main UK, USA and other relevant (literature review) studies.
The US Millennium cohort study is a very large population-based cohort study that started in 2001 and aims to follow-up approximately 200 000 military personnel. Their baseline data suggested a prevalence of 3.2% for depression, 2% for anxiety, 12.6% for alcohol misuse and 2.4% for PTSD.48 Results from a large study conducted among four US combat infantry units recorded that predeployment levels of mental disorders (eg, symptoms of anxiety, depression and PTSD) were between 9% and 15% compared to between 11% and 17% 3–4 months postdeployment to Iraq or Afghanistan.15 An extensive study carried out among 103 788 US veterans who had been deployed to Iraq or Afghanistan found that 13% of those who visited a veterans affair healthcare facility had a PTSD diagnosis, followed by depression and substance use disorder (both 5%).49 A baseline study among UK Armed Forces personnel suggested a prevalence of 20% for symptoms of common mental disorders, 4% for probable PTSD and 13% for alcohol misuse after deployment to Iraq and/or Afghanistan.11 The findings from their follow-up study were comparable to the baseline study that included soldiers who had not been deployed and those deployed during the first stage of the operation in Iraq.13 Also 4% were identified as having probable PTSD and approximately 20% recorded symptoms of common mental disorders.13 Only a small increase was found in the level of alcohol misuse after deployment in the follow-up study (2007–2009) and in the levels of PTSD among those in combat-roles.11 Woodhead et al (2011) examined the mental health of UK veterans and compared these with non-veterans matched for age and sex. Levels of PTSD and severe alcohol misuse were similar; 2.2% and 4.6% for the veterans and 2.9% and 7.6% for the non-veterans.50
A literature review concerning the prevalence of combat-related PTSD among military personnel and veterans who had been deployed to Iraq suggested that the prevalence range of combat-related PTSD was higher among US veterans compared to UK veterans, between the 4–17% and 3–6%, respectively.51 According to the authors these different findings might be influenced by various study design factors as well as issues related to the deployment and sociopolitical and cultural context.51 Gadermann et al,52 reported a best estimate for the prevalence of current major depression in US military personnel after conducting a meta-analysis of 25 studies; 12% for US serving personnel who are currently deployed, 13.1% for those who had been deployed and 5.7% for US serving personnel who had not been deployed yet. Comparing the findings from the current literature with the findings from the studies outlined before, mental health disorders seem to be more prevalent among (ex-)military personnel with a physical impairment. However, we need to be cautious due the heterogeneity across studies.
Some of the studies included in the review showed findings that were counterintuitive and warrant discussion. The study by Delimar et al47 suggested that the PTSD prevalence rate was highest among soldiers with non-disabling injuries, followed by those with a permanent disabling injury and healthy active duty soldiers. The authors suggested that those with a non-disabling injury experienced more stress because they feared being sent back to the front. Furthermore, they may have experienced a stronger sense of helplessness during the traumatic event as they often did not lose consciousness, in contrast to soldiers with permanent disabling injuries.47 Amputees were less likely to have PTSD compared to non-amputees with serious extremity injuries in a study conducted among US military personnel, 18.1% vs 32.1%, respectively.33 Several factors including differences in care after the injury, social and emotional support from colleagues and/or family may explain the difference but further investigation is necessary. It is important to note that these studies were cross-sectional in design and no information is available about the onset of the mental health disorder. Participants could have experienced other traumatic life events before or after their injury that may have triggered the development of PTSD or other mental health disorders.
The majority of the studies included in the review focused solely on (ex-)military personnel with an amputation. Besides high levels of PTSD, also substantial levels of depression, anxiety and psychological distress were found. A review of the psychological challenges identified among people with a lower limb amputation concluded that depression and anxiety are more prevalent among lower limb amputees up to 2 years after amputation.21 This is followed by a gradual decline to levels similar to the general population.21 The only study included in our review that examined this relationship did not find a significant association between time since amputation and PTSD, depression or anxiety, however all their participants had their amputation at least 5 years ago.19
Implications
The physical health of those severely injured during an operational deployment needs to be priority. Yet, clinicians should be aware that once physical recovery is progressing, the mental health of the patient needs evaluation. Adaptation and coping skills should be provided to facilitate the psychosocial challenges (ex-)military personnel with an impairment face.
Conclusions
Common mental health disorders are frequently reported among (ex-)military personnel with a physical impairment but rates vary considerably. Only few studies have looked into the association between various mental health disorders and different forms of impairments. Therefore, the results should be interpreted with caution and research should be directed into comparing prevalence rates of mental health disorders across impairment types and factors impacting this association.
Supplementary Material
Footnotes
Contributors: SAMS drafted and revised the manuscript. EMM contributed to the article search, article selection and commented on the manuscript. CM and SJ rated the articles included and commented on the manuscript. JS commented on the manuscript. NTF commented and revised the manuscript.
Funding: Blind Veterans UK. SAMS and EMM are funded by Blind Veterans UK. CM, SJ and NTF are funded by the UK Ministry of Defence. The authors’ work was independent of the funders.
Competing interests: None.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Blood CG, Puyana JC, Pitlyk PJ, et al. An assessment of the potential for reducing future combat deaths through medical technologies and training. J Trauma 2002;53:1160–5. [DOI] [PubMed] [Google Scholar]
- 2.Eastridge BJ, Jenkins D, Flaherty S, et al. Trauma system development in a theater of war: experiences from Operation Iraqi Freedom and Operation Enduring Freedom. J Trauma 2006;61:1366–72; discussion 1372–3. [DOI] [PubMed] [Google Scholar]
- 3.Stansbury LG, Lalliss SJ, Branstetter JG, et al. Amputations in US military personnel in the current conflicts in Afghanistan and Iraq. J Orthop Trauma 2008;22:43–6. [DOI] [PubMed] [Google Scholar]
- 4.Bellamy RF. A note on American combat mortality in Iraq. Mil Med 2007;172:i, 1023. [PubMed] [Google Scholar]
- 5.Holcomb JB, McMullin NR, Pearse L, et al. Causes of death in US Special Operations Forces in the global war on terrorism: 2001–2004. Ann Surg 2007;245:986–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Breeze J. Saving faces: the UK future facial protection programme. J R Army Med Corps 2012;158:284–7. [DOI] [PubMed] [Google Scholar]
- 7.Wade M. Brain injury and stress disorder strong indicators of vision problems for veterans. Insight 2013;38:22. [PubMed] [Google Scholar]
- 8.Smith D. Wounds of war: part one: eye surgeons in Iraq and Afghanistan. EyeNet: The American Academy of Ophthalmology, The Eye M.D. Association, 2012. [Google Scholar]
- 9.Owens BD, Kragh JF, Jr, Macaitis J, et al. Characterization of extremity wounds in Operation Iraqi Freedom and Operation Enduring Freedom. J Orthop Trauma 2007;21:254–7. [DOI] [PubMed] [Google Scholar]
- 10.Epstein RA, Heinemann AW, McFarland LV. Quality of life for veterans and service members with major traumatic limb loss from Vietnam and OIF/OEF conflicts. J Rehabil Res Dev 2010;47:373–85. [DOI] [PubMed] [Google Scholar]
- 11.Fear NT, Jones M, Murphy D, et al. What are the consequences of deployment to Iraq and Afghanistan on the mental health of the UK armed forces? A cohort study. Lancet 2010;375:1783–97. [DOI] [PubMed] [Google Scholar]
- 12.Hoge CW, Auchterlonie JL, Milliken CS. Mental health problems, use of mental health services, and attrition from military service after returning from deployment to Iraq or Afghanistan. JAMA 2006;295:1023–32. [DOI] [PubMed] [Google Scholar]
- 13.Hotopf M, Hull L, Fear NT, et al. The health of UK military personnel who deployed to the 2003 Iraq war: a cohort study. Lancet 2006;367:1731–41. [DOI] [PubMed] [Google Scholar]
- 14.Forbes HJ, Jones N, Woodhead C, et al. What are the effects of having an illness or injury whilst deployed on post deployment mental health? A population based record linkage study of UK Army personnel who have served in Iraq or Afghanistan. BMC Psychiatry 2012;12:178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hoge CW, Castro CA, Messer SC, et al. Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. N Engl J Med 2004;351:13–22. [DOI] [PubMed] [Google Scholar]
- 16.Koren D, Norman D, Cohen A, et al. Increased PTSD risk with combat-related injury: a matched comparison study of injured and uninjured soldiers experiencing the same combat events. Am J Psychiatry 2005;162:276–82. [DOI] [PubMed] [Google Scholar]
- 17.MacGregor AJ, Shaffer RA, Dougherty AL, et al. Psychological correlates of battle and nonbattle injury among Operation Iraqi Freedom veterans. Mil Med 2009;174:224–31. [DOI] [PubMed] [Google Scholar]
- 18.Wilk JE, Bliese PD, Kim PY, et al. Relationship of combat experiences to alcohol misuse among US soldiers returning from the Iraq war. Drug Alcohol Depend 2010;108:115–21. [DOI] [PubMed] [Google Scholar]
- 19.Desmond DM. Coping, affective distress, and psychosocial adjustment among people with traumatic upper limb amputations. J Psychosom Res 2007;62:15–21. [DOI] [PubMed] [Google Scholar]
- 20.Reiber GE, McFarland LV, Hubbard S, et al. Service members and veterans with major traumatic limb loss from Vietnam war and OIF/OEF conflicts: survey methods, participants, and summary findings. J Rehabil Res Dev 2010;47:275–97. [DOI] [PubMed] [Google Scholar]
- 21.Horgan O, MacLachlan M. Psychosocial adjustment to lower-limb amputation: a review. Disabil Rehabil 2004;26:837–50. [DOI] [PubMed] [Google Scholar]
- 22.WHO. Towards a common language for functioning, disability and health. ICF Geneva, World Health Organization, 2002. [Google Scholar]
- 23.Ajetunmobi O. Making sense of critical appraisal. London: Arnold, 2002. [Google Scholar]
- 24.Boyles AL, Harris SF, Rooney AA, et al. Forest Plot Viewer: a new graphing tool. Epidemiology 2011;22:746–7. [DOI] [PubMed] [Google Scholar]
- 25.Abrams TE, Barnett MJ, Hoth A, et al. The relationship between hearing impairment and depression in older veterans. J Am Geriatr Soc 2006;54:1475–7. [DOI] [PubMed] [Google Scholar]
- 26.Dougherty AL, MacGregor AJ, Han PP, et al. Visual dysfunction following blast-related traumatic brain injury from the battlefield. Brain Inj 2011;25:8–13. [DOI] [PubMed] [Google Scholar]
- 27.Fagelson MA. The association between tinnitus and posttraumatic stress disorder. Am J Audiol 2007;16:107–17. [DOI] [PubMed] [Google Scholar]
- 28.Martz E, Cook DW. Physical impairments as risk factors for the development of posttraumatic stress disorder. Rehabil Couns Bull 2001;44:217–21. [Google Scholar]
- 29.Melcer T, Walker GJ, Galarneau M, et al. Midterm health and personnel outcomes of recent combat amputees. Mil Med 2010;175:147–54. [DOI] [PubMed] [Google Scholar]
- 30.Radnitz CL, Hsu L, Tirch DD, et al. A comparison of posttraumatic stress disorder in veterans with and without spinal cord injury. J Abnorm Psychol 1998;107:676–80. [DOI] [PubMed] [Google Scholar]
- 31.Radnitz CL, Hsu L, Willard J, et al. Posttraumatic stress disorder in veterans with spinal cord injury: trauma-related risk factors. J Trauma Stress 1998;11:505–20. [DOI] [PubMed] [Google Scholar]
- 32.Boakye M, Moore R, Kong M, et al. Health-related quality-of-life status in veterans with spinal disorders. Qual Life Res 2013;22:45–52. [DOI] [PubMed] [Google Scholar]
- 33.Melcer T, Walker GJ, Sechriest VF, et al. Short-term physical and mental health outcomes for combat amputee and nonamputee extremity injury patients. J Orthop Trauma 2013;27:E31–7. [DOI] [PubMed] [Google Scholar]
- 34.Dougherty PJ, McFarland LV, Smith DG, et al. Combat-incurred bilateral transfemoral limb loss: a comparison of the Vietnam War to the wars in Afghanistan and Iraq. J Trauma Acute Care Surg 2012;73:1590–5. [DOI] [PubMed] [Google Scholar]
- 35.Katon JG, Reiber GE. Major traumatic limb loss among women veterans and service members. J Rehabil Res Dev 2013;50:173–82. [DOI] [PubMed] [Google Scholar]
- 36.Doukas WC, Hayda RA, Frisch HM, et al. The Military Extremity Trauma Amputation/Limb Salvage (METALS) Study outcomes of amputation versus limb salvage following major lower-extremity trauma. J Bone Joint Surg Am 2013;95A:138–45. [DOI] [PubMed] [Google Scholar]
- 37.Abeyasinghe N, de Zoysa P, Bandara K, et al. The prevalence of symptoms of post-traumatic stress disorder among soldiers with amputation of a limb or spinal injury: a report from a rehabilitation centre in Sri Lanka. Psychol Health Med 2012;17:376–81. [DOI] [PubMed] [Google Scholar]
- 38.Gunawardena N, Senevirathne RDA, Athauda T. Mental health outcome of unilateral lower limb amputee soldiers in two districts of Sri Lanka. Int J Soc Psychiatry 2007;53:135–47. [DOI] [PubMed] [Google Scholar]
- 39.Kasturiaratchi S, Jayawardana PL. Psychological status and physical disabilities of permanently disabled Sri Lankan servicemen. Hong Kong J Psychiatry 2004;14:9–14. [Google Scholar]
- 40.Delimar D, Sivik T, Korenjak P, et al. The effect of different traumatic experiences on the development of post-traumatic stress disorder. Mil Med 1995;160:635–9. [PubMed] [Google Scholar]
- 41.Gregurek R, Vukusic H, Baretic V, et al. Anxiety and post-traumatic stress disorder in disabled war veterans. Croat Med J 1996;37:38–41. [PubMed] [Google Scholar]
- 42.Sivik T, Delimar D, Korenjak P, et al. Certain psychological characteristics of soldiers injured in the 1991–1993 war in Croatia. Stress Med 2000;16:3–10. [Google Scholar]
- 43.Ebrahimzadeh MH, Fattahi AS. Long-term clinical outcomes of Iranian veterans with unilateral transfemoral amputation. Disabil Rehabil 2009;31:1873–7. [DOI] [PubMed] [Google Scholar]
- 44.Kim T-S, Pae C-U, Hong C-K, et al. Interrelationships among pain, disability, and psychological factors in young Korean conscripts with lumbar disc herniation. Military Med 2006;171:1113–16. [DOI] [PubMed] [Google Scholar]
- 45.Hume F, Summerfield D. After the war in Nicaragua: a psychosocial study of war wounded ex-combatants. Med War 1994;10:4–25. [DOI] [PubMed] [Google Scholar]
- 46.Desmond DM, MacLachlan M. Affective distress and amputation-related pain among older men with long-term, traumatic limb amputations. J Pain Symptom Manage 2006;31:362–8. [DOI] [PubMed] [Google Scholar]
- 47.Delimar D, Sivik T, Delimar N, et al. Post-traumatic stress disorder among Croat soldiers in the defence war in Croatia 1991–1993. Stress Med 1998;14:43–7. [Google Scholar]
- 48.Riddle JR, Smith TC, Smith B, et al. Millennium cohort: the 2001–2003 baseline prevalence of mental disorders in the US military. J Clin Epidemiol 2007;60:192–201. [DOI] [PubMed] [Google Scholar]
- 49.Seal KH, Bertenthal D, Miner CR, et al. Bringing the war back home: mental health disorders among 103,788 US veterans returning from Iraq and Afghanistan seen at department of veterans affairs facilities. Arch Intern Med 2007;167:476–82. [DOI] [PubMed] [Google Scholar]
- 50.Woodhead C, Rona RJ, Iversen A, et al. Mental health and health service use among post-national service veterans: results from the 2007 Adult Psychiatric Morbidity Survey of England. Psychol Med 2011;41:363–72. [DOI] [PubMed] [Google Scholar]
- 51.Richardson LK, Frueh BC, Acierno R. Prevalence estimates of combat-related post-traumatic stress disorder: critical review. Aust N Z J Psychiatry 2010;44:4–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Gadermann AM, Engel CC, Naifeh JA, et al. Prevalence of DSM-IV major depression among US military personnel: meta-analysis and simulation. Mil Med 2012;177:47–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.