Highlights
-
•
LRYGB plus HHR is safe and feasible.
-
•
LRYGB plus HHR results in additional weight loss and improvement of co-morbidity.
-
•
LRYGB plus HHR is a good alternative for antireflux surgery in obese HH-patients.
-
•
HH-patients meeting bariatric surgery criteria should be informed about LRYGB plus HHR.
-
•
Randomized trials comparing fundoplication with LRYGB plus HHR are needed.
Keywords: Laparoscopic gastric bypass, Hiatal paraesophageal hernia, Morbid obesity, Surgery, GERD, Bariatric
Abstract
Introduction
Obesity is a risk factor for hiatal hernia. In addition, much higher recurrence rates are reported after standard surgical treatment of hiatal hernia in morbidly obese patients. Laparoscopic Roux-en-Y gastric bypass (LRYGB) is an effective surgical treatment for morbid obesity and is known to effectively control symptoms of gastroesophageal reflux (GERD).
Case presentation
Two patients suffering from giant hiatal hernias where a combined LRYGB and hiatal hernia repair (HHR) with mesh was performed are presented in this paper. There were no postoperative complications and at 1 year follow-up, there was no sign of recurrence of the hernia.
Discussion
The gold standard for all symptomatic reflux patients is still surgical correction of the paraesophageal hernia, including complete reduction of the hernia sac, resection of the sac, hiatal closure and fundoplication. However, HHR outcome is adversely affected by higher BMI levels, leading to increased HH recurrence rates in the obese.
Conclusion
Concomitant giant hiatal hernia repair with LRYGB appears to be safe and feasible. Moreover, LRYGB plus HHR appears to be a good alternative for HH patients suffering from morbid obesity as well than antireflux surgery alone because of the additional benefit of significant weight loss and improvement of obesity related co-morbidity.
1. Introduction
Obesity is a significant independent risk factor for gastroesophageal reflux disease (GERD) and hiatal hernia (HH). The probability of HH increases with Body Mass Index (BMI) [1]. In addition, obesity is associated with a higher risk of erosive esophagitis and esophageal adenocarcinoma [2]. Hiatal hernia repair (HHR) and fundoplication is the standard surgical treatment for HH. However, much higher recurrence rates are observed in morbid obese patients with BMI levels over 35 kg/m2 [3]. Laparoscopic Roux-en-Y gastric bypass (LRYGB) is one of the most performed surgical treatment for morbid obesity and also controls symptoms and complications of GERD [4]. Only several cases are reported of morbidly obese patients with paraesophageal hernias in which LRYGB was combined with primary crurae closure [5,6]. These procedures appeared to be feasible and safe. Combining HHR with a LRYGB procedure may be a better option for morbidly obese patients suffering from giant hiatal hernias than HHR and fundoplication.
Here, we report two patients with a giant HH where LRYGB with HHR was performed.
2. Case presentation
2.1. Case 1
A 47-year old woman weighing 71 kg and being 165 cm tall (BMI 26.1 kg/m2) presented herself at our outpatient clinic with regurgitation, belching, nausea and vomiting. She had previously undergone gastric band surgery (at that time she weighed 87 kg, resulting in a BMI of 32.0 kg/m2) combined with a partial closure of the wide hiatus in another hospital. The gastric band was removed 3 months after placing, because of a recurrence of her HH, resulting in the gastric band residing intrathoracally. Gastroscopy, chest X-ray and barium swallow test showed that the entire stomach was in the thorax (type 4 hiatal hernia). Because earlier HHR alone had failed, we performed a surgical intervention combining a LRYGB with HHR. We used a five-port technique for obesity surgery. During surgery, the complete hernia sac was excised, although this was difficult due to the many adhesions as a result of earlier operations. After replacing the stomach in the abdomen the hiatus was narrowed with interrupted ethibond sutures [7]. A small gastric pouch was created after calibration with a 34 french boogie. Treitz was identified and the jejunum was transsected 60 cm distal from Treitz, after which a 3-cm long linear stapled gastroenterostomy was realized. A stapled jejunojejunostomy with a alimentary limb of 100 cm was created. The mesenterial defects were closed with an EMS stapler (Ethicon) [8]. There were no post-operative complications; however, 1.5 year after surgery the patient presented herself at our emergency room with abdominal pain, nausea and vomiting. Chest X-ray and CT scan showed a recurrence, having the pouch and the residual stomach herniated through a 7 cm wide hiatal hernia (Fig. 1). A laparoscopic hiatal hernia repair with a mesh was performed after repositioning of the remnant of the stomach out of the thorax. A crural repair with interrupted sutures was performed and reinforced with a Ultrapromesh (Ethicon, Johnson & Johnson) fixed with non-absorbable tackers (Covidien®). In addition, omentum was attached to the mesh to prevent erosion of the mesh into the pouch. 1 year after surgery patient weighed 68 kg (BMI 24.9 kg/m2) and there were no signs of recurrence of the paraesophageal hernia.
Fig. 1.
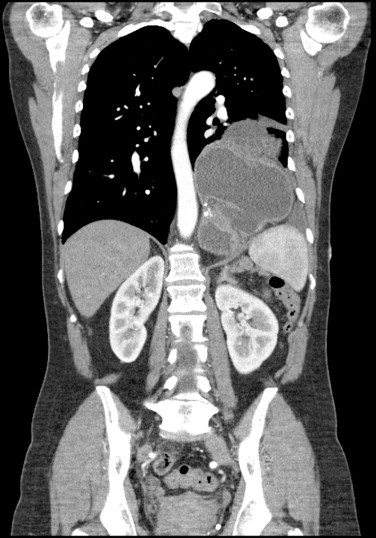
CT scan of patient 1, showing the pouch and residual stomach in the thorax.
2.2. Case 2
A 59-year old woman with a length of 169 cm and weight of 129 kg (BMI 45.2 kg/m2) presented with progressive dyspnea, mostly present when bending over, coughing, belching, regurgitation and pyrosis. Medical history revealed an appendectomy earlier and diabetes mellitus type 2. Besides her morbid obesity, there were no other findings revealed by physical examination. CT scan revealed a mixed sliding and paraesophageal hernia, with the entire stomach in the chest (type 4 hiatal hernia). A surgical intervention combining a LRYGB with HHR with techniques as described in the first case was performed.
There were no postoperative complications. At 1 year follow-up, the patient weighed 94 kg (BMI 32.9 kg/m2) and control CT scan showed no recurrence of the paraesophageal hernia. There were no signs of recurrence of the hernia.
3. Discussion
Both GERD and HH are highly prevalent among the morbidly obese population with prevalence rates ranging from 39–61% for GERD [9] and 20–53% for HH [10], respectively. Increased intra-abdominal pressure as a result of central obesity predisposes obese patients for both GERD and HH [11].
Morbid obese patients that want bariatric surgery are most frequently treated with LRYGB if they are also suffering from GERD, because it results in a reduction of the gastric content, prevention of bile reflux to the gastric pouch and a decrease of intra-abdominal pressure due to the weight loss. As a consequence LRYGB results in a very good control of GERD [4,12]. But contrariwise not many patients presenting with GERD symptoms who also have morbid obesity are offered this option. The gold standard for all symptomatic reflux patients is still surgical correction of the paraesophageal hernia, including complete reduction of the hernia sac, resection of the sac, hiatal closure and fundoplication [13]. However, HHR outcome is adversely affected by higher BMI levels, leading to increased HH recurrence rates in the obese [14]. Therefore, it makes sense to combine HHR with bariatric surgery, preferably LRYGB, since this is considered the gold standard for bariatric surgery [15] and has proven to be effective in controlling GERD in obese patients [4,12].
In our first patient, we decided not to use a mesh to reinforce the sutured crurae as we believed weight loss induced by the LRYGB would lower the abdominal pressure and therefore the chance of HH recurrence. Furthermore, using a mesh in potentially infected areas such as the gastrojejunal anastomosis might cause infection of the mesh as well as erosion of a mesh in the GI-anastomosis. However, after having observed a recurrence of the HH in the first case we decided to use a dorsal semicircular mesh graft for closure of the HH in future similar cases as the use of mesh prevents short term hernia recurrence and has shown a low complication rate in giant paraesophageal hernias [16]. Biologic meshes as an alternative have do not result in more complications and might be considered to reinforce the sutured crural defect [17].
Our first patient had already undergone anti-reflux surgery prior to our procedure. Several case reports describing LRYGB and HHR after earlier anti-reflux surgery concluded that the procedure was feasible and effective, but however, was associated with higher morbidity and the majority of patients was still using anti-reflux medication after treatment [18,19]. In our first patient, we also observed a much more complicated post-operative course. Taking this in consideration, we would advocate that combined LRYGB and HHR should be considered as the first treatment of choice in patients with a symptomatic paraesophageal hernia and morbid obesity. In addition, using a mesh could be useful in patients suffering from giant hiatal hernias.
Few case reports show that concomitant primary crus closure of the HH and LRYGB is feasible and safe [5,6] and their results are in accordance with ours reporting a EWL of 30% at a follow-up of 6 months [5] and a mean EWL of 46.1% at a follow-up of 12 months [6] and a 100% improvement in GERD symptoms in all cases. In addition, Kothari et al. [20] showed no increase in morbidity and mortality after LRYGB with HHR compared to LRYGB alone.
4. Conclusion
In conclusion, concomitant giant hiatal hernia repair with LRYGB appears to be safe and feasible. These patients did not have any significant differences in morbidity, mortality, length of stay, readmission rate, or cost. Moreover, LRYGB plus HHR appears to be a good alternative for GERD patients suffering from morbid obesity as well than antireflux surgery alone because of the additional benefit of significant weight loss and improvement of obesity related co-morbidity. For this reason these patients should be informed preoperatively for such possibilities, if they meet the criteria for bariatric surgery. However, randomized trials comparing laparoscopic fundoplication with LRYGB plus HH repair as a treatment for morbidly obese patients with symptomatic paraesophageal hernias are needed.
Ethical approval
For this type of study, no formal ethical approval is necessary.
Conflict of interest
The authors have no conflicts of interest to disclose.
Funding
None.
Authors contribution
Lucia Duinhouwer wrote the first version of the manuscript, collected and analyzed the data and was involved in patient care.
Lacer Ulas Biter was involved in patient care, analyzed the data and contributed to the manuscript.
Bas Wijnhoven was involved in patient care, analyzed the data and contributed to the manuscript.
Guido Mannaerts was involved in patient care, analyzed the data, proposed the study concept and contributed to the manuscript.
All authors approved the final version of the manuscript.
Consent
Written informed consent was obtained from the patients for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Guarantor
All authors accept full responsibility for the work, had access to the data and controlled the decision to publish.
Contributor Information
Lucia E. Duinhouwer, Email: l.duinhouwer@erasmusmc.nl.
L. Ulas Biter, Email: u.biter@sfg.nl.
Bas P. Wijnhoven, Email: b.wijnhoven@erasmusmc.nl.
Guido H. Mannaerts, Email: dr.mannaerts@gmail.com.
References
- 1.Nocon M., Labenz J., Willich S.N. Lifestyle factors and symptoms of gastro-oesophageal reflux – a population-based study. Aliment. Pharmacol. Ther. 2006;23:169–174. doi: 10.1111/j.1365-2036.2006.02727.x. [DOI] [PubMed] [Google Scholar]
- 2.Hampel H., Abraham N.S., El-Serag H.B. Meta-analysis: obesity and the risk for gastroesophageal reflux disease and its complications. Ann. Intern. Med. 2005;143:199–211. doi: 10.7326/0003-4819-143-3-200508020-00006. [DOI] [PubMed] [Google Scholar]
- 3.Perez A.R., Moncure A.C., Rattner D.W. Obesity adversely affects the outcome of antireflux operations. Surg. Endosc. 2001;15:986–996. doi: 10.1007/s004640000392. [DOI] [PubMed] [Google Scholar]
- 4.Perry Y., Courcoulas A.P., Fernando H.C., Buenaventura P.O., McCaughan J.S., Luketich J.D. Laparoscopic Roux-en-Y gastric bypass for recalcitrant gastroesophageal reflux disease in morbidly obese patients. JSLS. 2004;8:19–23. [PMC free article] [PubMed] [Google Scholar]
- 5.Salvador-Sanchis J.L., Martinez-Ramos D., Herfarth A., Rivadulla-Serrano I., Ibanez-Belenguer M., Hoashi J.S. Treatment of morbid obesity and hiatal paraesophageal hernia by laparoscopic Roux-en-Y gastric bypass. Obes. Surg. 2010;20:801–803. doi: 10.1007/s11695-008-9656-y. [DOI] [PubMed] [Google Scholar]
- 6.Kasotakis G., Mittal S.K., Sudan R. Combined treatment of symptomatic massive paraesophageal hernia in the morbidly obese. JSLS. 2011;15:188–192. doi: 10.4293/108680811X13022985132164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jacobsen H., Dalenback J., Ekelund M., Gislason H., Hedenbro J.L. Tensile strength after closure of mesenteric gaps in laparoscopic gastric bypass: three techniques tested in a porcine model. Obes. Surg. 2013;23:320–324. doi: 10.1007/s11695-012-0800-3. [DOI] [PubMed] [Google Scholar]
- 8.Aghajani E., Jacobsen H.J., Nergaard B.J., Hedenbro J.L., Leifson B.G., Gislason H. Internal hernia after gastric bypass: a new and simplified technique for laparoscopic primary closure of the mesenteric defects. J. Gastrointest. Surg. 2012;16:641–645. doi: 10.1007/s11605-011-1790-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.El-Serag H.B., Graham D.Y., Satia J.A., Rabeneck L. Obesity is an independent risk factor for GERD symptoms and erosive esophagitis. Am. J. Gastroenterol. 2005;100:1243–1250. doi: 10.1111/j.1572-0241.2005.41703.x. [DOI] [PubMed] [Google Scholar]
- 10.Suter M., Dorta G., Giusti V., Calmes J.M. Gastro-esophageal reflux and esophageal motility disorders in morbidly obese patients. Obes. Surg. 2004;14:959–966. doi: 10.1381/0960892041719581. [DOI] [PubMed] [Google Scholar]
- 11.Frezza E.E., Shebani K.O., Robertson J., Wachtel M.S. Morbid obesity causes chronic increase of intraabdominal pressure. Dig. Dis. Sci. 2007;52:1038–1041. doi: 10.1007/s10620-006-9203-4. [DOI] [PubMed] [Google Scholar]
- 12.El-Hadi M., Birch D.W., Gill R.S., Karmali S. The effect of bariatric surgery on gastroesophageal reflux disease. Can. J. Surg. 2014;57:139–144. doi: 10.1503/cjs.030612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Aly A., Munt J., Jamieson G.G., Ludemann R., Devitt P.G., Watson D.I. Laparoscopic repair of large hiatal hernias. Br. J. Surg. 2005;92:648–653. doi: 10.1002/bjs.4916. [DOI] [PubMed] [Google Scholar]
- 14.Hinder R.A., Raiser F., Katada N., McBride P.J., Perdikis G., Lund R.J. Results of Nissen fundoplication. A cost analysis. Surg. Endosc. 1995;9:1328–1332. [PubMed] [Google Scholar]
- 15.Buchwald H., Williams S.E. Bariatric surgery worldwide 2003. Obes. Surg. 2004;14:1157–1164. doi: 10.1381/0960892042387057. [DOI] [PubMed] [Google Scholar]
- 16.Targarona E.M., Bendahan G., Balague C., Garriga J., Trias M. Mesh in the hiatus: a controversial issue. Arch. Surg. 2004;139:1286–1296. doi: 10.1001/archsurg.139.12.1286. Discussion 96. [DOI] [PubMed] [Google Scholar]
- 17.Oelschlager B.K., Pellegrini C.A., Hunter J.G., Brunt M.L., Soper N.J., Sheppard B.C. Biologic prosthesis to prevent recurrence after laparoscopic paraesophageal hernia repair: long-term follow-up from a multicenter, prospective, randomized trial. J. Am. Coll. Surg. 2011;213:461–468. doi: 10.1016/j.jamcollsurg.2011.05.017. [DOI] [PubMed] [Google Scholar]
- 18.Raftopoulos I., Awais O., Courcoulas A.P., Luketich J.D. Laparoscopic gastric bypass after antireflux surgery for the treatment of gastroesophageal reflux in morbidly obese patients: initial experience. Obes. Surg. 2004;14:1373–1380. doi: 10.1381/0960892042583950. [DOI] [PubMed] [Google Scholar]
- 19.Zainabadi K., Courcoulas A.P., Awais O., Raftopoulos I. Laparoscopic revision of Nissen fundoplication to Roux-en-Y gastric bypass in morbidly obese patients. Surg. Endosc. 2008;22:2737–2740. doi: 10.1007/s00464-008-9848-5. [DOI] [PubMed] [Google Scholar]
- 20.Kothari V., Shaligram A., Reynoso J., Schmidt E., McBride C.L., Oleynikov D. Impact on perioperative outcomes of concomitant hiatal hernia repair with laparoscopic gastric bypass. Obes. Surg. 2012;22:1607–1610. doi: 10.1007/s11695-012-0714-0. [DOI] [PubMed] [Google Scholar]


