Highlights
-
•
The origin from perirenal fat is very uncommon.
-
•
The occurrence of hematogenous metastasis is a rare finding at the time of diagnosis.
-
•
The undifferentiated and pleomorphic type are neoplasm with high grade of malignancy.
-
•
In case of diagnostic doubt and in presence of recurrence, magnetic resonance imaging (MRI) may be useful because can identifying in a reliable manner the satellite localizations of the main lesion.
-
•
The complete surgical (R0) resection represents the only possibility of radical treatment.
-
•
Following surgical resection, the 50–100% of liposarcomas recur from residual tissue, which is the primary cause of death.
-
•
Percutaneous biopsy has low accuracy in the diagnosis of retroperitoneal dedifferentiated liposarcoma (DDLS).
Keywords: Retroperitoneal liposarcoma, Soft tissue sarcomas, Myxoid areas, Radical treatment
Abstract
Aim
Retroperitoneal soft-tissue sarcomas are relatively uncommon diseases, the most frequent histotype, ranging from 20% to 45% of all cases, is represented by liposarcoma, which is a hard-to treat condition for its local aggressiveness and clinical aspecificity.
Presentation of case
We report a case of a 64-years-old woman who underwent surgical resection for a giant pleomorphic retroperitoneal liposarcoma.
Discussion
Currently chemotherapy for retroperitoneal soft-tissue sarcomas is no effective, and radiotherapy has limited efficacy due to the toxicity affecting adjacent intra-abdominal structures, showed validity only in case of high-grade malignancy by reducing local recurrence, but with no advantage in overall survival. Nowadays only, the complete surgical resection remains the most important predictor of local recurrence and overall survival.
Conclusion
The removal of a retroperitoneal sarcoma of remarkable size is a challenge for the surgeon owing to the anatomical site, to the absence of an anatomically evident vascular-lymphatic peduncle and to the adhesions contracted with the contiguous organs and with the great vessels. Therefore, we believe that, particularly for large-size diseases associated to high-grade malignancy, a complete surgical resection with removal of the contiguous intra and retroperitoneal organs when infiltrated represents the only therapeutic option to obtain a negative margin and therefore an oncological radicality.
1. Introduction
Among the retroperitoneal sarcomas, that represent the 10–15% of all soft tissue sarcoma [1], the most common histotype is represented by liposarcoma, which ranges from 20% to 45% of all cases [2]. It commonly occurs in patients with 40–60 years-old with a 1:1 ratio between male and female [3]. The liposarcoma may have weight and dimension variable; those over 20 kg are called “giant liposarcomas” and are extremely rare [3]; some authors have reported masses between 18 and 46.6 kg [4–6]. We report a rare case of a giant retroperitoneal liposarcoma even more uncommon for its origin from perirenal fat: infact approximately 13% are located in the retroperitoneal area, and less than 1/3 of these arise from perinephric fat [7].
2. Case report
We report a case of a 64 year-old woman that was referred to our observation for a progressive volumetric increase of the abdomen. The computed tomography (CT) of the abdomen demonstrated the presence of a voluminous mass, extending from the sub-hepatic space up to the pelvic cavity with dislocation of the right kidney to the left (Figs. 1 and 2). The mass appeared as mixed structure, characterized by the coexistence of areas with different density, adipose with thick septa and solid with superfluid density, with cranio–caudal extension of over 30 cm. Therefore the patient was submitted to an explorative laparotomy which revealed the presence of a bulky lesion with a multinodular appearance, originating from the right retroperitoneal region. The lesion had produced a remarkable dislocation of intra- and retro-peritoneal organs to the left side dislocating pancreas, kidney and whole intestinal mass to a space between the left flank and homolateral iliac fossa. For the apparent infiltration of the right kidney (Fig. 3) was performed a biopsy that confirmed its neoplastic infiltration. We proceeded to release the neoplasm from the adhesions by retroperitoneal contiguous organs including the vena cava and common iliac vessels, with its subsequent removal en bloc with the right kidney (Fig. 4). The postoperative course was uneventful and the patient was discharged on the 3th postoperative day. The definitive histological diagnosis was pleomorphic liposarcoma with myxoid areas, (42 × 37 × 18 cm) (Fig. 5), originating from the right perirenal fat and infiltrating the periureteral tissue, with free resection margin. At 24 months of follow-up the patient is disease free.
Fig. 1.
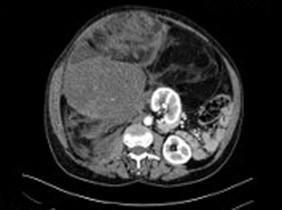
CT scan showing the presence of the bulky lesion stretching from the subhepatic region to the pelvic cavity, displacing the right kidney to the left.
Fig. 2.
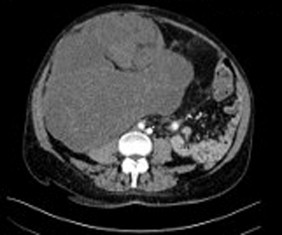
CT scan showing the macroscopic intralesional characteristics, consisting of the presence of areas with different fat density and thick septa associated with an inhomogeneous solid component featuring sovrafluid-density coarse components.
Fig. 3.

Evidence of the close relationship between the lesion and the right kidney and the origin from the right retroperitoneal region at the level of the ipsilateral parietocolica space.
Fig. 4.

Right retroperitoneal cavity as it appeared once the lesion had been removed and the right nephrectomy had been performed, with evidence of the structures that had close relations of contiguity with it. The inferior vena cava is easily recognizable as well as the iliopsoas muscle, gonadal blood vessels and right iliac vessels.
Fig. 5.
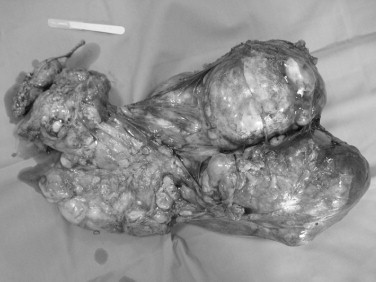
Picture of the removed surgical specimen including the right kidney.
3. Discussion
The retroperitoneal liposarcomas are generally neoplasms with a low or intermediate grade of malignancy. The occurrence of hematogenous metastasis is a rare finding at the time of diagnosis; the lung represents the main site of distant metastases [8]. From a histological point of view, in according to the morphological characteristics and on the strength of cytogenetic aberrations, now widely accepted, we can divide the liposarcoma in 4 types [8]: (1) undifferentiated, (2) pleomorphic, (3) well differentiated, (4) myxoid/round cell. The undifferentiated and pleomorphic type are neoplasm with high grade of malignancy accompanied by remarkable biological aggressiveness and with metastatic potential while well-differentiated and myxoid/round cell forms are tumours with a low grade of malignancy, associated with a more favourable prognosis [9]. The well-differentiated and undifferentiated tumours represent the most common biological group. The former is characterized by local aggressiveness with low metastatic potential, its clinical manifestation occurs through the compression of adjacent organs or structures, and to the CT imaging usually appears as a homogeneous lesion with the same density of adipose tissue, well encapsulated, with the presence of thick septa. Instead, the latter usually originates from a histological aberration occurring in the context of a well-differentiated liposarcoma. The further loss of differentiation determines a cellular transformation, which is even more characteristic of the relapse of disease, it occurs in 20% at the first recurrence and in 44% at the second one [2]. The CT imaging of the undifferentiated sarcoma demonstrates a heterogeneous, no lipogenic mass [8,10]. In case of diagnostic doubt and in presence of recurrence, Magnetic Resonance Imaging (MRI) may be useful because can identifying in a reliable manner the satellite localizations of the main lesion. The resection of a retroperitoneal sarcoma of remarkable size is a challenge for the surgeon owing to the anatomical site, to the absence of an anatomically evident vascular-lymphatic peduncle that makes it hard to obtain safe margin and to the adherences with the contiguous organs and with the great vessels. Therefore the retroperitoneal liposarcoma shows a high rate of local recurrence after surgical excision. Actually, the complete surgical (R0) resection represents the only possibility of radical treatment, in fact as reported in a study [11] carried out on 177 patients with retroperitoneal liposarcoma operated with curative intent, the percentage of patients disease free at 3 and 5 years was 73% and 60% respectively. The prognostic factors statistically associated with survival were found to be the histotype and the type of resection performed (complete vs. partial). Actually the overall survival at 5-years reported in literature for the various histological subtypes well differentiated, myxoid/round cell, undifferentiated and pleomorphic, ranging from 90%, 60 to 90%, 75% and 30 to 50%, respectively [11].
The resection of neighbor organs is usually required to facilitate dissection, but can be essential to get a radical macroscopic removal, that significantly influence the prognosis. Neuhaus et al. [12] reported a study carried out on 190 patients, of whom 72 were submitted to curative surgery for retroperitoneal liposarcoma (RPLS), and other 47 had undergone palliative resection for recurrent RPLS. Over half of the patients underwent resection with curative intention had excision of a contiguous organ to achieve macroscopic clearance at primary surgery. However, organs were directly infiltrated by tumour in only 4% of patients. However, as in our patient about the 15% of retroperitoneal liposarcomas originate from the perirenal fat [7,13]. As in our case report, the kidneys are often dislocated or rotated by the mass and can be the site of neoplastic infiltration with possible onset of pyelo-ureteralnephrosis. Consequently they are the organs most involved in the resection, immediately followed by the colon [14]. Following surgical resection, the 50 - 100% of liposarcomas recur from residual tissue, which is the primary cause of death [1]. Therefore an aggressive surgical behaviour is justified, with the resection of the structures and viscera adjacent to the pathological process in the attempt to obtain free disease margin allowing to obtain a 5-year recurrence rate of 22% that results nevertheless in an increase morbidity respect to the past [12,15,16]. In fact for this reason being difficult to discriminate intraoperatively the pathological tissue, from those normal, the tumours should be resected by including a more abundant quantity of retroperitoneal fat. However, the resection of organs or structures invaded by the tumour, although infrequent, should occur only in case in which is not possible to identify a safe plane of dissection between the tumour and the organs adjacent to it, with an en bloc resection. Lewis attributes a peri-operative mortality of 4% identifying haemorrhage, sepsis, acute myocardial infraction, and multiorganic failure as the principal causes of death [2]. Actually the chemotherapy treatment used in the adjuvant or neoadjuvant setting have no benefit in the clinical course of the disease and therefore is no utilized in a routine manner [17]. Doxorubicin only yields a response rate of 18–29%. The antibiotic salinomycin, a potassium ionophore, appears to increase the chemosensitivity to the doxorubicin; so it may be used to decrease the doxorubicin dosage and its toxic side effects [18]. Neoadjuvant therapy may be took into account in cases of dedifferentiated liposarcoma (DDLS), which has an increased risk of recurrence and metastasis. It's necessary an accurate subtype-specific diagnosis to evaluate the neoadjuvant therapy. In a retrospective study of 120 patients who underwent 137 preoperative percutaneous biopsies followed by surgical resections, Ikoma [19] has demonstrated that percutaneous biopsy has low accuracy in the diagnosis of retroperitoneal DDLS. This can potentially mislead the decision to adopt the neoadjuvant treatment.
Some retrospective studies have underlined the benefits of the adjuvant radiotherapy, used in tumours with a diameter greater than 5 cm and positive surgical margin, with better control of local recurrence but without increases in long-term survival [20].
4. Conclusion
Our case shows some peculiar characteristics: firstly its origin from perirenal fat, infact approximately 13% are located in the retroperitoneal area, and less than 1/3 of these arise from perinephric fat; and secondly the huge size (42 × 37 × 18 cm) of liposarcoma, so it can be defined giant.
Actually the surgical approach represents the only therapeutic option that can provide a concrete perspective of care considering lack of support of effective complementary therapies. An aggressive surgical attitude that includes extended resections of the extra- and intaperitoneal structures is justified, especially in tumours of large size, in order to obtain a microscopic radicality of resection margins.
Conflict of interest
All authors declare that they have not any conflict of interest.
Funding
The authors declare there are not any sponsors involvement.
Ethical approval
The authors declare that all procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008. Informed consent was obtained from the patient for being included in the study.
Consent
Authors declare that they have obtained written informed consent from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author contribution
Antonio Caizzone concept or design, data collection, data analysis or interpretation, writing the paper. Edoardo Saladino contributor.
Francesco Fleres contributor, corresponding author, translator.
Cosimo Paviglianiti contributor.
Francesco Iaropoli contributor.
Carmelo Mazzeo contributor.
Eugenio Cucinotta contributor.
Antonio Macrì study concept or design, data collection, data analysis or interpretation and reviewer.
Guarantor
Antonio Caizzone.
Edoardo Saladino.
Francesco Fleres.
Antonio Macrì.
References
- 1.Leão P., Vilaça S., Oliveira M., Falcão J. Giant recurrent retroperitoneal liposarcoma initially presenting as inguinal hernia: Review of literature. Int. J. Surg. Case Rep. 2012;3(November 22 (3)):103–106. doi: 10.1016/j.ijscr.2011.03.009. Epub 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lewis J.J., Leung D., Woodruff J.M., Brennan M.F. Retroperitoneal soft-tissue sarcoma: analysis of 500 patients treated and followed at a single institution. Ann. Surg. 1998;228(3):355–365. doi: 10.1097/00000658-199809000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hashimoto Y., Hatakeyama S., Tachiwada T. Surgical treatment of a giant liposarcoma in a Japanese man. Adv. Urol. 2010;2010 doi: 10.1155/2010/943073. Article ID 943073 3 pages. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McCallum O.J., Burke J.J., 2nd, Childs A.J. Retroperitoneal liposarcoma weighing over one hundred pound with review of the literature. Gynecol. Oncol. 2006;103(September 26 (3)):1152–1154. doi: 10.1016/j.ygyno.2006.08.005. Epub 2006. [DOI] [PubMed] [Google Scholar]
- 5.Yol S., Tavli S., Tavli L. Retroperitoneal and scrotal giant liposarcoma: report of a case. Surg. Today. 1998;28(3):339–342. doi: 10.1007/s005950050136. [DOI] [PubMed] [Google Scholar]
- 6.Herrera-Gomez A., Ortega-Gutierrez C., Betancourt A.M., Luna-Ortiz K. Giant retroperitoneal liposarcoma. World J. Surg. Oncol. 2008;6:115. doi: 10.1186/1477-7819-6-115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Martínez León M.I., Martos Forniels J.A., Arranz Salas I.M., Díaz Martí T. Liposarcoma of the perirenal cell. Arch. Esp. Urol. 2003 Nov;56(9):1050–1054. [PubMed] [Google Scholar]
- 8.Crago A.M., Singer S. Clinical and molecular approaches to well differentiated and dedifferentiated liposarcoma. Curr. Opin. Oncol. 2011;23(4):373–378. doi: 10.1097/CCO.0b013e32834796e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fletcher C., Unni K., Mertens F. Pathology and genetics of tumors of soft tissue and bone. In: Kleihues P., editor. World Health Organization Classification of Tumors. Lyon: International Agency for Research on Cancer Press; 2002. p. 427. [Google Scholar]
- 10.Dalal K.M., Kattan M.W., Antonescu C.R., Brennan M.F., Singer S. Subtype specific prognostic nomogram for patients with primary liposarcoma of the retroperitoneum, extremity, or trunk. Ann. Surg. 2006;244(3):381–391. doi: 10.1097/01.sla.0000234795.98607.00. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Singer S., Antonescu C.R., Riedel E., Brennan M.F. Histologic subtype and margin of resection predict pattern of recurrence and survival for retroperitoneal liposarcoma. Ann. Surg. 2003;238(3):358–370. doi: 10.1097/01.sla.0000086542.11899.38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Neuhaus S.J., Barry P., Clark M.A. Surgical management of primary and recurrent retroperitoneal liposarcoma. Br. J. Surg. 2005;92(2):246–252. doi: 10.1002/bjs.4802. [DOI] [PubMed] [Google Scholar]
- 13.García Marín A., Martín Gil J., Sánchez Rodríguez T., Pérez Díaz M.D., Turégano Fuentes F. Giant mixed-type perirenal fat liposarcoma. Rev. Esp. Enferm. Dig. 2010 Mar;102(3):221–222. doi: 10.4321/s1130-01082010000300015. [DOI] [PubMed] [Google Scholar]
- 14.Murphey M.D., Arcara L.K., Fanburg-Smith J. From the archives of the AFIP: imaging of musculoskeletal liposarcoma with radiologic–pathologic correlation. Radiographics. 2005;25(5):1371–1395. doi: 10.1148/rg.255055106. [DOI] [PubMed] [Google Scholar]
- 15.Bonvalot S., Miceli R., Berselli M. Aggressive surgery in retroperitoneal soft tissue sarcoma carried out at high-volume centers is safe and is associated with improved local control. Ann. Surg. Oncol. 2010;17(6):1507–1514. doi: 10.1245/s10434-010-1057-5. [DOI] [PubMed] [Google Scholar]
- 16.Tseng W.W., Madewell J.E., Wei W., Somaiah N., Lazar A.J., Ghadimi M.P., Hoffman A., Pisters P.W., Lev D.C., Pollock R.E. Locoregional disease patterns in well-differentiated and dedifferentiated retroperitoneal liposarcoma: implications for the extent of resection? Ann. Surg. Oncol. 2014;21(July (7)):2136–2143. doi: 10.1245/s10434-014-3643-4. Epub 2014 April 7. [DOI] [PubMed] [Google Scholar]
- 17.Eilber F.C., Eilber F.R., Eckardt J. The impact of chemotherapy on the survival of patients with high-grade primary extremity liposarcoma. Ann. Surg. 2004;240(4):687–695. doi: 10.1097/01.sla.0000141710.74073.0d. discussion 695–687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Grasso E., Marino F., Bottalico M., Simone M. A case of myxoid liposarcoma of the retroperitoneum: a challenging tumour for diagnosis and treatment. Case Rep. Surg. 2014;2014 doi: 10.1155/2014/572805. Article ID 572805, 4 pages. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ikoma N., Torres K.E., Somaiah N., Hunt K.K., Cormier J.N., Tseng W., Lev D., Pollock R., Wang W.L., Feig B. Accuracy of Preoperative Percutaneous Biopsy for the Diagnosis of Retroperitoneal Liposarcoma Subtypes. Ann. Surg. Oncol. 2014;(October 30) doi: 10.1245/s10434-014-4210-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pawlik T.M., Pisters P.W., Mikula L. Long-term results of two prospective trials of preoperative external beam radiotherapy for localized intermediate- or high-grade retroperitoneal soft tissue sarcoma. Ann. Surg. Oncol. 2006;4(February 24):508–517. doi: 10.1245/ASO.2006.05.035. Epub 2006. [DOI] [PubMed] [Google Scholar]


