Highlights
-
•
Developmental abnormalities of liver including ectopic liver are rare conditions.
-
•
Although it does not usually produce any symptom clinically, it can rarely result in serious complications such as bleeding, pyloric and portal vein obstruction.
-
•
Ectopic liver has the capacity of malignant transformation to hepatocellular carcinoma that makes it essential to be removed.
-
•
The vascular anatomy of ectopic liver should be identified before the dissection of gallbladder in order to prevent hemorrhage from the liver parenchyma.
Keywords: Ectopic liver tissue, Gallbladder, Laparoscopy, Cholecystectomy, Vascular supply, ERCP
Abstract
Introduction
Developmental abnormalities of liver including ectopic liver tissue (ELT) are rare conditions. Few cases presenting ELT have been reported in literature till now. Even though the most common area seen is gallbladder, it is detected both abdominal and thoracic sites. There is a relationship between HCC and ectopic liver that necessitates the removal.
Presentation of case
A 51-year-old female was hospitalized because of abdominal pain. Gallstone and bile duct dilatation were determined during ultrasonographic (USG) evaluation. The patient was operated for cholecystectomy following a successful endoscopic retrograde cholangiopancreatography (ERCP). During operation, a mass located on gallbladder with its unique vascular support was identified and resected together with gallbladder. The mass had a separate vascular stalk arising from liver parenchyma substance and it was clipped with laparoscopic staples. The histopathological examination revealed that the mass adherent to gallbladder was ectopic liver confirming the intraoperative observation. The postoperative course of patient was uneventfull and she was discharged at the second day after the operation.
Discussion
Ectopic liver tissue is incidentally found both in abdominal and thoracic cavity. ELT can rarely be diagnosed before surgical procedures or autopsies. It can be overlooked easily by radiological techniques. Although it does not usually produce any symptom clinically, it can rarely result in serious complications such as bleeding, pyloric and portal vein obstruction. ELT also has the capacity of malignant transformation to hepatocellular carcinoma that makes it essential to be removed.
Conclusion
Although ELT is rarely seen, it should be removed when recognized in order to prevent the complications and malignant transformation.
1. Introduction
Ectopic liver tissue (ELT) is a rare condition. It differs from accessory liver in that ectopic liver tissue is not connected to the mother liver [1]. Most authors believe that it occurs due to aberrant migration during the embryological development of liver. ELT has been reported in the various body zones below and above the diaphragm [2]. The most frequent organs in the abdominal cavity are gallbladder, gastrohepatic and umbilical ligaments, omentum and stomach. Above the diaphragm, it has been reported in the pleural cavity, mediastinum, lungs and heart. Hovewer, the gallbladder seems to be most frequently affected organ in the abdominal cavity [3]. The number of reported cases of ELT is less than 100 so far [4]. Ectopic liver tissue can rarely be diagnosed before surgery because of absence of the symptoms. The reported cases are usually found incidentally during autopsy or surgery. It has been emphasized that ELT has increased the potential risk of hepatocellular carcinoma that makes the resection essential [5]. Although the vascular supply of ELT especially adherent to gallbladder was not reported in detail in literature; there are mainly three different vascular supply patterns of gallbladder associated ELT. (a) Artery arising from cystic artery. (b) Vascular pedicle (with/without its own vein) arising from liver parenchyma substance (as in our case). (c) Vascular structures embedded in a mesentery lying from the hepatic site to ELT tissue. In one study Koh and Hunt [15] reported a case of ELT on the gallbladder wall in which its artery was derived from cystic artery and bile duct drainage to cystic duct. Catani et al. reported that ectopic liver nodule seemed drizzled by an arterial branch that runs along the front part of gallbladder [4]. The identification of vascular supply desires surgical attention because it can cause uncontrollable hemorrhage, in cases with a direct vascular supply from liver substance, due to tear or rupture during gallbladder traction. We herein, report a case of ectopic liver attached to the gallbladder wall with its unique separate vascular pedicle arising from native liver. The detailed histopathological examination of ELT is essential since it is more prone to malignant transformation than native liver. So the pathologist should be noticed on this topic. The case in our report couldnot be diagnosed preoperatively and encountered incidentally during laparoscopic cholecystectomy. The histopathological diagnosis revealed cholecystitis and ectopic liver tissue located on gallbladder.
2. Presentation of case
A 51 year-old female suffering from abdominal pain was admitted to general surgery clinic. Gallstones and bile duct dilatation have been shown by abdominal ultrasonography (USG). In general evaluation, right upper quadrant tenderness and alteration of biochemical parameters were found. Her aspartate transaminase (AST), alanine transaminase (ALT), gamma glutamy transaminase (GGT), alkaline phosphatase (ALP), amylase and direct bilirubin values were as follows, respectively: 497.3 U/L (0–40), 335.5 U/L (0–41), 650 U/L (0–60), 148 U/L (35–130), 1419 U/L (30–300) and 1.11 mg/dL (0–0.2). Combining the dilated choledochus, alterations of biochemical parameters, general evaluation of the patient suggested us biliary pancreatitis and endoscopic retrograde cholangiopancreatography (ERCP) was planned. ERCP revealed mildly dilated choledochus (11–12 mm diameter) and there was no other filling defect or pathology. These findings set the diagnosis of type II sphincter of Oddi dysfunction (SOD) and sphincterotomy was applied. Following ERCP, her biochemical parameters and physical findings returned to normal and she was operated for gallstone. During laparoscopy, an ectopic tissue of liver about 2 × 1 cm was seen on the corpus of gallbladder without any connection to liver. It had its own vascular pedicle arising from liver but no biliary drainage connected to the main biliary system or cystic duct (Fig. 1). The vascular pedicle was isolated and clipped separately, and the ectopic liver mass was removed together with gallbladder (Fig. 2). The pathological evaluation of the specimen revealed the diagnosis of the ectopic liver without any malignant transformation and cholecystitis (Fig. 3a and b). The patient was discharged on the second postoperative day without any complication.
Fig. 1.
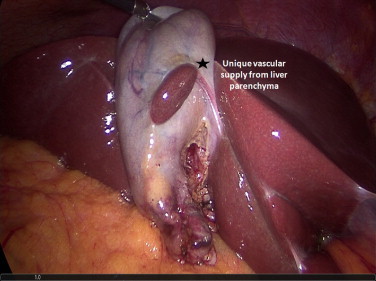
The unique vascular supply of ectopic liver from liver parenchyma.
Fig. 2.

Ectopic liver tissue on gallbladder (Postoperatively).
Fig. 3.
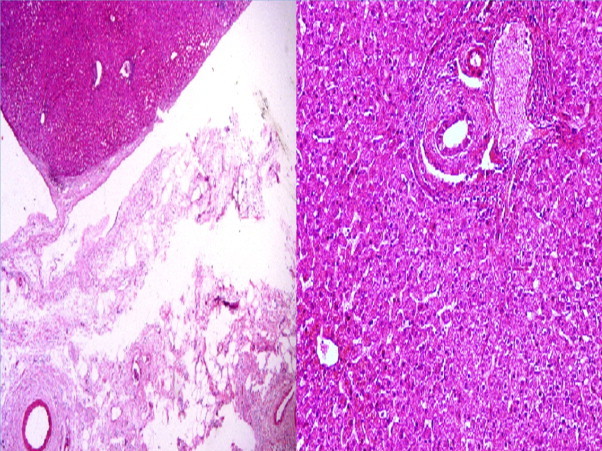
(a) The presence of ectopic liver adhered to the gallbladder wall. (x40 H&E). (b) Ectopic liver tissue containing preserved hepatic lobules with central vein, hepatic artery and bile canaliculi. (x100 H&E).
3. Discussion
Ectopic liver tissue is a very rare entity. The first data goes back to 1920’s [4,6]. Even though the exact incidence of ELT is unknown, two big series studied on this topic reported three cases (0.05%) at autopsy including 5500 cases and twelve cases (0.6%) during laparoscopy among 1802 cases related to gallbladder [7,8]. In the present report our patient was the only case (0.1%) of ELT among 932 cholecystectomy cases in three years period. Hovewer, we consider that the real incidence of ELT is an overlooked problem, since it is a neglected diagnosis because of absence of symptoms and lack of awareness. In symptomatic cases the main problem is usually due to torsion, necrosis, rupture, malignant transformation and the problems related to compression by mass effect. Although, the most common localization of ELT is gallbladder, it is seen both in intraabdominal and intra thoracic cavity. It was found in spleen, umbilicus, vena cava, and also in heart and lung [9–12]. Hepatobiliary system originates from foregut in the fourth week during embryological period. ELT results from aberrant migration of the liver proper in the period of embryologic development [5]. The diagnosis of ELT without surgery or autopsy is difficult by means of radiological studies. ELT is probably not recognized by radiologist due to rarity of the condition and the lack of awareness. It can be seen as a soft tissue mass on CT or US imaging [13]. The percutaneous biopsy is not recommended because of the risk of malignancy and bleeding [6]. In the present case, although gallstone was recognized in the patient, ELT couldnot be diagnosed by radiology preoperatively. Although, there is relationship between ELT attached to gallbladder and biliary disease, such as cholelithiasis and acute or chronic cholecystitis, it is probably due to the fact that the ectopic liver has been diagnosed during operation related to gallstone [14,15]. We also observed the ELT during cholecystectomy performed for chronic cholecystitis.
ELT usually has a normal histology of the liver i.e., normal portal structure, regular lobules and central vein. Even though the possible reason is not clear the risk of hepatocellular carcinoma has increased in patients with ELT, it is likely that biliary drainage is insufficient and/or blood supply is reduced in the ectopic liver tissue [6,16]. There are various articles about the relationship between the ELT and hepatocellular carcinoma. Arakawa et al. [17] reported that there were 21 HCC cases related to ELT and emphasized that only six cases (27%) had cirrhosis in the main liver. Interestingly, patients who had ELT on gallbladder were less susceptible to HCC development as compared to other localizations outside the gallbladder. This study, revealed that only one of 42 ELT localized on the gallbladder was diagnosed as malignant [17]. The optimal surgical strategy for the patients who had cancer of ELT is complete resection of ELT and the attached organ [18]. In our case, there was no malign transformation in the pathologic examination. Although, there are several reports in literature defining the ELT, the vascular support is often undefined. It is clinically important to define the ELT and vascular supply before the dissection of gallbladder from the liver bad because undue traction of gallbladder during the removal may result in rupture or tear of vascular structure derived directly from the liver substance eventually leading to severe bleeding. The vascular peduncle usually originates from liver substance directly or cystic artery. It sometimes may be embedded in a mesentery lying from the hepatic site to EL tissue [6]. In this circumstances, following the Callot’s triangle dissection, the vascular peduncles or mesentery should be isolated and clipped separately before the gallbladder dissection.
4. Conclusion
Ectopic liver tissue is a rare condition. The diagnosis is unusual before surgery. ELT should be operated not only for serious complications but also for the malignancy potential. The vascular pedicle should be identified and secured in suitable cases in order to decrease the hemorrhagic complications.
Conflict of interest
Authors declared no conflict of interest.
Funding
None.
Ethical approval
A written informed consent was obtained from the patient before the preparation of manuscript.
References
- 1.Collan Y., Hakkiluoto A., Hästbacka J. Ectopic liver. Ann. Chir. Gynaecol. 1978;1:27–29. [PubMed] [Google Scholar]
- 2.Zwaenepoel T., Dierickx D., Laleman W., Sciot R. Ectopic liver tissue in two distinct anatomical regions: a case report. Acta Gastro-Enterol. Belgica. 2014;1:68–70. [PubMed] [Google Scholar]
- 3.Arslan Y., Altintoprak F., Serin K.R., Kivilcim T., Yalkin O., Ozkan O.V. Rare entity: ectopic liver tissue in the wall of the gallbladder – a case report. World J. Clin. Cases. 2014;12:924–926. doi: 10.12998/wjcc.v2.i12.924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Catani M., De Milito R., Romagnoli F., Mingazzini P., Silvestri V., Usai V. Ectopic liver nodules: a rare finding during cholecystectomy. G. Chir. 2011;5:255–258. [PubMed] [Google Scholar]
- 5.Lundy J., Johnson E., Edwards K., Rivera D. Laparoscopic management of gallbladder-associated ectopic liver. JSLS. 2005;4:485–487. [PMC free article] [PubMed] [Google Scholar]
- 6.Martinez C.A., de Resende H.C., Jr, Rodrigues M.R., Sato D.T., Brunialti C.V., Palma R.T. Gallbladder-associated ectopic liver: a rare finding during a laparoscopic cholecystectomy. Int. J. Surg. Case Rep. 2013;3:312–315. doi: 10.1016/j.ijscr.2013.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tejada E., Danielson C. Ectopic or heterotopic liver (choristoma) associated with the gallbladder. Arch. Pathol. Lab. Med. 1989;113:950–952. [PubMed] [Google Scholar]
- 8.Sato S., Watanabe M., Nagasawa S., Niigaki M., Sakai S., Akagi S. Laparoscopic observations of congenital anomalies of the liver. Gastrointest. Endosc. 1998;47:136–140. doi: 10.1016/s0016-5107(98)70345-1. [DOI] [PubMed] [Google Scholar]
- 9.Park W.H., Choi S.O., Lee S.S., Randolph J.G. Ectopic umbilical liver in conjunction with biliary atresia: uncommon association. J. Pediatr. Surg. 1991;2:219–222. doi: 10.1016/0022-3468(91)90917-i. [DOI] [PubMed] [Google Scholar]
- 10.Morris M.W., Helling T.S., Creswell L.L., Jordan B., Mitchell M.E. Ectopic liver masquerading as a floating intracaval mass. J.Vasc. Surg. 2012;6:1759–1760. doi: 10.1016/j.jvs.2011.12.064. [DOI] [PubMed] [Google Scholar]
- 11.Xu L., Jeudy J., Burke A.P. Ectopic hepatic tissue presenting as right atrial mass. Hum. Pathol. 2012;6:958–960. doi: 10.1016/j.humpath.2011.10.004. [DOI] [PubMed] [Google Scholar]
- 12.Iber T., Rintala R. Intrapulmonary ectopic liver. J. Pediatr. Surg. 1999;9:1425–1426. doi: 10.1016/s0022-3468(99)90028-3. [DOI] [PubMed] [Google Scholar]
- 13.Hamdani S.D., Baron R.L. Ectopic liver simulating a mass in the gallbladder wall: imaging findings. AJR Am. J. Roentgenol. 1994;3:647–648. doi: 10.2214/ajr.162.3.8109514. [DOI] [PubMed] [Google Scholar]
- 14.Caygill C.P., Gatenby P.A. Ectopic liver and hepatocarcinogenesis. Eur. J. Gastroenterol. Hepatol. 2004;8:727–729. doi: 10.1097/01.meg.0000131037.92864.df. [DOI] [PubMed] [Google Scholar]
- 15.Koh C.E., Hunt R. Ectopic liver encountered during laparoscopic cholecystectomy. Asian J. Surg. 2007;3:227–229. doi: 10.1016/S1015-9584(08)60028-7. [DOI] [PubMed] [Google Scholar]
- 16.Leone N., De Paolis P., Carrera M., Carucci P., Musso A., David E. Ectopic liver and hepatocarcinogenesis: report of three cases with four years’ follow-up. Eur. J. Gastroenterol. Hepatol. 2004;8:731–735. doi: 10.1097/01.meg.0000131044.05434.f7. [DOI] [PubMed] [Google Scholar]
- 17.Arakawa M., Kimura Y., Sakata K., Kubo Y., Fukushima T., Okuda K. Propensity of ectopic liver to hepatocarcinogenesis: case reports and a review of the literature. Hepatology. 1999;29:57–61. doi: 10.1002/hep.510290144. [DOI] [PubMed] [Google Scholar]
- 18.Beltran M.A., Barria C., Pujado B., Barrera R., Mendez P., Pozo C. Hepatic heterototopic tissue on the gallbladder wall: an incidental finding with pathological potential. J. Gastrointest. Liver Dis. 2007;3:347–349. [PubMed] [Google Scholar]


