Highlights
-
•
Gastrointestinal stromal tumors (GIST) are solid tumors.
-
•
Atypical presentations in form a cystic lesion have been rarely reported.
-
•
A duodenal GIST masquerading as a cystic lesion has never been reported.
-
•
First report a case of a large duodenal cyst that finally, turned out to be a GIST.
-
•
Successfully managed by local resection avoiding a pancreaticoduodenectomy.
Keywords: Gastrointestinal tumor, Cystic degeneration, Duodenal cyst, Duodenal diverticulum, Pyloric exclusion
Abstract
Introduction
Gastrointestinal stromal tumors (GIST) are solid tumors. A duodenal GIST masquerading as a cystic lesion has never been reported. We report a large duodenal cyst that finally turned out to be a GIST and was managed without a pancreaticoduodenectomy (PD).
Presentation of case
A 55 year old lady presented with painful lump in epigastrium. A CT scan revealed a large exophytic cystic lesion from the duodenum with a small solid component. An endoscopy showed a polypoid lesion in the second part of the duodenum adjacent to what looked like a diverticulum. A sleeve duodenal resection, duodeno-duodenostomy and pyloric exclusion was done. The histopathology was duodenal GIST.
Discussion
This case posed diagnostic difficulty as it was thought to be either a duplication cyst or a diverticulum of duodenum. The odd point was the small solid component in it. We considered the possibility of a malignancy arising in these settings, which is has been occasionally reported. To our surprise, it turned out to be a GIST. An extensive literature search yielded only four reports that have reported cystic GISTS, all arising from the stomach or pancreas where they have been mistaken for pseudocysts or even a mucinous cystadenocarcinoma of the pancreas. This is the first report of a cystic GIST arising from the duodenum.
Conclusion
GISTS can present as a predominantly cystic lesion and needs to be considered in the differential diagnosis of cystic lesions of the duodenum. Local resection is an attractive option in select cases and avoids a PD.
1. Introduction
Cystic lesions arising from the duodenum as such are an uncommon finding. These could be congenital or acquired. The commonest cystic lesion of the duodenum is a duodenal diverticulum. Then there are others like duplication cysts, choledochocoele, intramural pseudocysts, cystic dystrophy of the duodenal wall and pseudodiverticulum [1]. The clinical setting along with a cross section imaging usually clinches the diagnosis. We report a large cystic lesion arising from the duodenum, which ultimately turned out to be a gastrointestinal stromal tumor (GIST). To the best of our knowledge, a duodenal GIST presenting as a cystic lesion has never been reported. We discuss the therapeutic options in such lesions which could be challenging because of the complex pancreaticoduodenal anatomy coupled with the fear of the potent pancreatico-biliary secretions in the unfortunate occurrence of an anastomotic leak.
2. Presentation of case
A 55 year old lady presented with complaints of pain and lump in epigastric region of 3 months’ duration. She denied any history suggestive of gastric outlet obstruction, jaundice, gastrointestinal bleeding or constitutional symptoms. She had no past surgeries and had no comorbidities. On examination, there was a large lump in the epigastric and right hypochondrial regions extending into the right lumbar region. The lump was firm in consistency and had restricted mobility. A CT scan of the abdomen was done which showed a well defined exophytic cystic lesion measuring 15 × 8 × 10 cm arising from the second and the third part of the duodenum (Fig. 1A and B). A small solid component in the region of its origin from the duodenum with luminal compromise was also appreciated. An upper GI endoscopy was ordered which showed a polypoid lesion in distal part of the second part of the duodenum adjacent to what looked like a diverticulum (Fig. 1C). An endoscopic biopsy was attempted but was unsuccessful despite attempts with a pediatric scope due to the lesion being at an odd angle. A preoperative diagnosis of a duodenal diverticulum with a possibility of a malignancy arising out of it was made. The patient was taken up for laparotomy with a tentative plan for a pancreaticoduodenectomy (PD). Per-operatively, she was found to have a 15 × 10 cm cystic lesion with a small solid component arising from the third part of the duodenum (Fig. 2A–D).
Fig. 1.
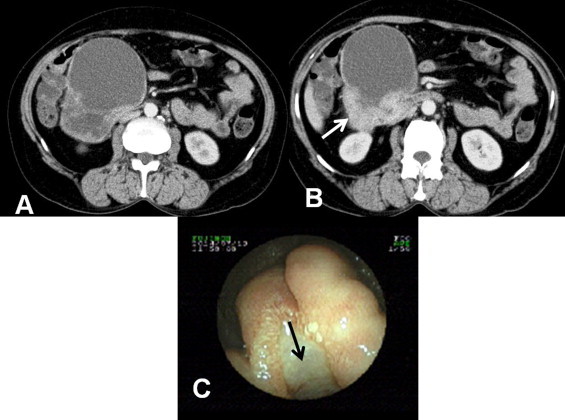
A and B. Axial sections of the CT scan showing a large cystic lesion in relation to the duodenum with a focal solid component (white arrow). C. Endoscopic view of the duodenum showing polypoid lesion in distal part of the second part of the duodenum adjacent to what looked like a diverticulum (black arrow).
Fig. 2.
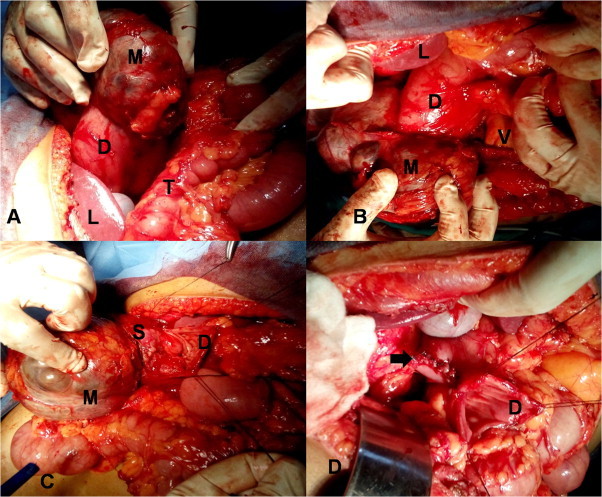
Operative photographs. A and B. Showing a 15 × 10 cm cystic lesion arising from the third part of duodenum. C. After duodenotomy, showing the small solid component. D. Following excision, duodenoduodenostomy being done. D: duodenum; M: cystic mass, S: solid component of the cystic lesion; V: superior mesenteric vessels; L: liver; T: transverse colon.
A mobilization of the cyst, sleeve duodenal resection along with duodeno-duodenostomy and pyloric exclusion was done. Additionally, a retrograde tube duodenostomy and feeding jejunostomy was done (Fig. 3A and B). She had an uneventful postoperative recovery. On gross examination, the cut section revealed a cystic lesion with a focal solid component of 3 cm.
Fig. 3.
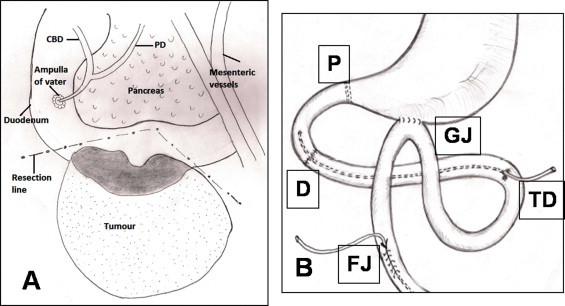
A. Line diagram showing the final surgery. B. Wide local excision of the tumor. Duodeno-duodenostomy (D), pyloric exclusion (P), gastrojejunostomy (GJ), retrograde tube duodenostomy (TD) and feeding jejunostomy (FJ).
Microscopically, a well circumscribed sub-mucosal nodular lesion (Fig 4A) with intersecting fascicles (Fig. 4B) which stained positive for CD 34 and CD 117 with a mitotic Count < 3/50HPF (Fig. 4C) was seen. A final histological diagnosis was GIST of low malignant potential arising from duodenum was made. She has now completed 6 months’ of follow-up and remains disease free.
Fig. 4.
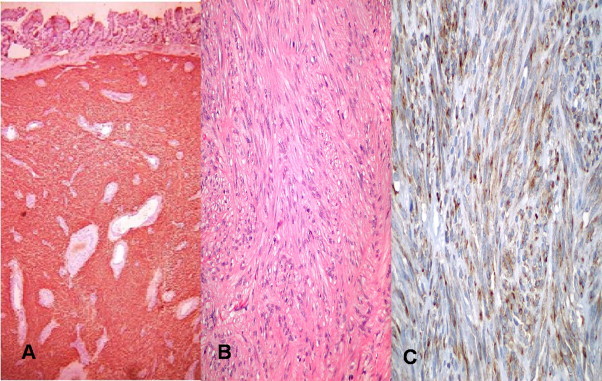
Photomicrographs showing. A. Well circumscribed sub-mucosal nodular lesion with Intersecting fascicles (H&E, 4×). B. Pleomorphic elongated cells with cigar shaped nuclei and eosinophilic cytoplasm with mitotic count < 3/50HPF (H&E, 40×). C. Tumor cells highlighted by the CD117 (c-Kit) Immunohistochemical stain (40×).
3. Discussion
This case posed diagnostic difficulty both, in terms of organ of origin as well as its nature. As a large cystic lesion arising from the duodenum, it was thought to be either a duplication cyst or a diverticulum. The odd point was the small solid component in it. We considered the possibility of a malignancy arising in these settings, which is has been occasionally reported [2,3]. To our surprise, it ultimately turned out to be a GIST.
GISTs originate from the interstitial cells of Cajal and thus to start with, are confined to the submucosa and muscularis propria. As they grow, they protrude exophytically and larger growing ones can undergo cystic changes due to liquefaction and hemorrhage. But it is extremely rare for them to present a largely cystic lesion with only a thin rim of viable tumor, which may occur in a rapidly growing GIST.
An extensive literature search yielded only four case reports that have reported cystic GISTS, all arising from the stomach or pancreas where they have been mistaken for pseudocysts or even a mucinous cystadenocarcinoma of the pancreas [4–7]. This is the first report of a cystic GIST arising from the duodenum. A preoperative diagnosis could have been clinched, but unfortunately the lesion was negotiable only by a pediatric endoscope and attempts to biopsy it failed.
We took up the patient for surgery with a tentative plan for a PD. As we started mobilizing the cystic lesion from the transverse colon and mesocolon and the retroperitoneum, safeguarding the mesenteric vessels, we realized that it was arising from the third part of the duodenum and at its site of origin we could feel a solid component. A duodenotomy was made between stay sutures to assess the extent of involvement. The tumor was well away from the ampulla of Vater and involved about half the circumference of the dilated duodenum.
The management decision in duodenal GISTS depends mainly on three factors: (1) the location, especially its relation to the sphincter of Oddi, (2) the extent of involvement of the duodenal wall, and (3) the pancreatic involvement if any. The options are between a PD or a local resection, which could be in the form of a wedge resection and primary closure for small tumors, wedge resection and duodeno-jejunotosmy for a larger tumor or segmental resection and duodeno-duodenostomy or duodeno-jejunostomy with stapling off of the distal duodenum for tumors that involve a large portion of the duodenal wall [8,9]. We did a wedge resection encompassing a margin of normal wall and reconstruction was in the form of a duodeno-duodenostomy. Due to a large suture line and keeping in mind the catastrophic consequences of a leak, we decided to add a pylorus exclusion to protect the anastomosis.
4. Conclusion
Our case highlights the fact that large, rapidly growing GISTS can present as a predominantly cystic lesion and needs to be considered in the differential diagnosis of cystic lesions of the duodenum. These can be challenging in terms of diagnosis and management. Local resection is an attractive option in cases without pancreatic/ampullary involvement and avoids a PD.
Conflicts of interest
None declared.
Funding
None.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Acknowledgement
None.
References
- 1.C. Ruivo, C. Antunes, M.A. Goncalves, et al., Cystic lesions of the pancreatic-duodenal region: a Pictoral review. Poster session presented at: European Congress of Radiology. (2012) doi:10.1594/ecr2012/C-1828.
- 2.Seeliger B., Piardi T., Marzano E. Duodenal duplication cyst: a potentially malignant disease. Ann. Surg. Oncol. 2012;19:3753–3754. doi: 10.1245/s10434-012-2502-4. [DOI] [PubMed] [Google Scholar]
- 3.Furukawa M., Izumi S., Tsukuda K. Duodenal carcinoma from a duodenal diverticulum mimicking pancreatic carcinoma. Acta Med. Okayama. 2012;66:423–427. doi: 10.18926/AMO/48967. [DOI] [PubMed] [Google Scholar]
- 4.Naitoh I., Okayama Y., Hirai M. Exophytic pedunculated gastrointestinal stromal tumor with remarkable cystic change. J. Gastroenterol. 2003;38:1181–1184. doi: 10.1007/s00535-003-1228-2. [DOI] [PubMed] [Google Scholar]
- 5.Pauser U., Hinz S., Merz H., Feller A.C. Gastrointestinal stromal tumors with pseudocystic change mimicking a pancreatic tumor: two case reports. J. Med. Case Rep. 2009;3:7592. doi: 10.1186/1752-1947-3-7592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pugh J.L., Jie T., Bhattacharyya A.K. Pedunculated gastrointestinal stromal tumor (GIST) of the stomach presenting as pancreatic mucinous cystadenocarcinoma: a case report. J. Clin. Exp. Pathol. 2013;3:135. [Google Scholar]
- 7.Ding G., Yang J., Cheng S. A rare case of rapid growth of exophytic gastrointestinal stromal tumor of the stomach. Dig. Dis. Sci. 2005;50:820–823. doi: 10.1007/s10620-005-2646-1. [DOI] [PubMed] [Google Scholar]
- 8.Hoeppner J., Kulemann B., Marjanovic G. Limited resection for duodenal gastrointestinal stromal tumors: surgical management and clinical outcome. World J. Gastrointest. Surg. 2013;5:16–21. doi: 10.4240/wjgs.v5.i2.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Beham A., Schaefer I.M., Cameron S. Duodenal GIST: a single center experience. Int. J. Colorectal. Dis. 2013;28:581–590. doi: 10.1007/s00384-012-1432-8. [DOI] [PMC free article] [PubMed] [Google Scholar]


