Highlights
-
•
We successfully resected 6.5 cm- sized retroperitoneal cystic mass through laparoscopic approach.
-
•
Pathologic examination revealed a primary mucinous cystadenoma.
-
•
Literature review showed that male sex (p = 0.019), and solid nodules in cysts (p < 0.001) were both significantly associated with malignancy.
-
•
When confronted with a cystic mass in the retroperitoneum, a primary mucinous cystic neoplasm should be considered and complete surgical removal of the tumor without spillage is recommended.
Keywords: Primary, Retroperitoneum, Mucinous, Cystadenoma, Laparoscopy
Abstract
Introduction
Primary retroperitoneal mucinous cystic neoplasm is very rare and its histogenesis is unclear.
Presentation of case
This paper presents the case of a 31-year-old female in whom an incidentally detected retroperitoneal cystic mass, 6.5 cm in size, was successfully resected through laparoscopic approach. Pathologic examination revealed a mucinous cystadenoma. The postoperative course was uneventful, and the patient remained free of recurrence six months after surgery.
Discussion
Literature review showed that male sex (p = 0.019), and solid nodules in cysts (p < 0.001) were both significantly associated with malignancy.
Conclusion
When confronted with a cystic mass in the retroperitoneum, a primary mucinous cystic neoplasm should be considered and complete surgical removal of the tumor without spillage is recommended.
1. Introduction
Primary retroperitoneal mucinous cystic neoplasm is very rare. Although mucinous cystic neoplasm is common ovarian tumor and is grossly and microscopically similar to retroperitoneal mucinous cystic neoplasm [1], because of the limited number of reported cases, the histogenesis of primary retroperitoneal mucinous cystic neoplasm is unclear and establishing a preoperative diagnosis is very difficult. We report a case of primary retroperitoneal mucinous cystadenoma and further provide a literature review.
2. Presentation of case
A 31-year-old female was admitted due to pain in the right upper quadrant. She had an unremarkable medical history. Physical examination revealed that her BMI was in the normal range (height 163 cm, weight 50 kg) with a blood pressure of 110/60 mmHg, a pulse of 80 beats/min, and a body temperature of 36.4 C. Her abdomen was tender in the right upper quadrant but no guarding and rebound tenderness were noted. Laboratory findings including liver function test and serum tumor markers (CEA, CA125, and CA19-9) were within the normal limits. Computed tomography revealed multiple tiny gallstones with segmental gallbladder wall thickening and a 6.5 cm sized multiloculated cystic mass in the left retroperitoneal space just below the spleen (Fig 1). The preoperative diagnoses were either retroperitoneal tumor such as cystic mesothelioma, mucinous cystadenoma, or cystic lymphangioma and symptomatic gallstone with chronic cholecystitis. We proceeded to perform laparoscopic excision of the cystic mass and then cholecystectomy. The patient was placed on the operating room table in the right semi-lateral decubitus position (to a 45-degree angle to the operating table). An 11 mm trocar was inserted in the infraumbilical region and two more 5 mm trocars were inserted 3 cm below the costal margin at the left anterior axillary line and 4 cm below the xyphoid process. Laparoscopy revealed a large, well-demarcated cystic mass behind the inferior pole of the spleen that seemed to have no apparent attachment to the adjacent structures such as the pancreas, spleen, colon, and etc. The tumor was completely excised without spillage of cystic fluid. Laparoscopic cholecystectomy was then performed in the usual manner with one more 5 mm trocar 3 cm below the right costal margin at the mid-clavicular line. The mass and gallbladder were placed in a Lap-bag (Sejong Medical, Paju, Korea) and were retrieved via the umbilical port site with extension of incision upto 2 cm. The total operation time was 80 minutes. Upon gross inspection, the specimen was a thick-walled, multilocular cyst with a smooth and glistening internal surface (Fig 2). It was filled with slightly turbid, mucoid, and yellowish fluid. When microscopically examined, the lining of the cyst wall consisted of a single layer of columnar epithelium with abundant intracellular mucin and basally arranged small nuclei (Fig 3). Ovarian-like mesenchymal stroma was not seen. There was also no evidence of a malignant or borderline lesion, and the final diagnosis was thus primary retroperitoneal mucinous cystadenoma. The postoperative course was uneventful and the patient was discharged on postoperative day 5. During the six month follow-up period, the patient remained completely free of symptoms and without evidence of recurrence.
Fig. 1.

Abdominal computed tomography shows a 6.5 cm sized multiloculated cystic mass in left retroprertoneal space just below spleen.
Fig. 2.

Glossly it shows a 6.5 × 5.5 × 0.4 cm unilocular cyst with smooth inner surface containing yellowish viscous fluid.
Fig. 3.
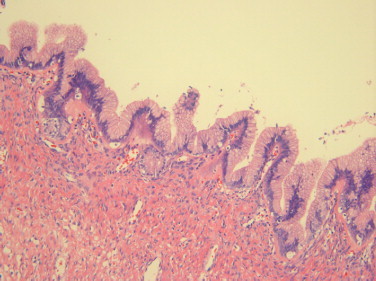
Multilocular cyst lined by a single layer of tall columnar cells. The stroma consisted of fibrocollagenous tissue with no pancreatic or ovarian components (H&E, ×200).
3. Discussion
Primary retroperitoneal mucinous cystic neoplasm is a rare cystic lesion for which only single case reports [1–32] and small series [33–36] have been published. This neoplasm shares a histological similarity to ovarian mucinous cystic neoplasm but can arise at any location in the retroperitoneum without attachment to the ovary [1].
The histogenesis of primary retroperitoneal mucinous cystic neoplasm remains unclear; however, four main theories have been proposed to explain its potential origin. First, these tumors may arise from teratoma, in which the columnar epithelium has overridden all other components to survive as the single cell component [1,2]. Another possibility is that they arise from ectopic ovarian tissue because they have resemblances to ovarian mucinous cystadenomas, which may explain why they occur mainly in women [3]. Until now only two cases of primary retroperitoneal mucinous cystic neoplasm in men have been reported in the literature [12,13]. However, ovarian remnants have not been identified in the wall of the cysts [4,5]. A third theory is that they arise from remnants of the embryonal urogenital apparatus [6–8]. However, the most plausible theory is that mucinous cystic neoplasm arises from invaginations of the peritoneal mesothelium, with subsequent endocervical metaplasia [1,2]. To support this theory, in these neoplasms the immunohistochemical staining for estrogen or progesterone is negative and there has been no gut-like muscle found in the pathologic specimens.
We performed a literature review using Medline searching from 1970 to 2013, and including the present study, a total of 56 cases [1–37] of primary mucinous cystic neoplasm of the retroperitoneum were identified and reviewed in terms of their clinicopathologic characteristics. Among these 56 cases, 54 cases were women and only two cases [12,13] were men. The median age of the patients was 39 years with wide range from 14 to 85 years. The size of the reported tumors ranged from 5 cm to 30 cm (median 12 cm). Most patients (n = 24, 51.1%) complained of abdominal mass. However, 14 patients (29.8%) complained of abdominal pain and 9 cases (19.1%) were detected incidentally. Postoperative pathology showed 31 cases (55.4%) of cystadenoma, 10 cases (17.9%) of moderate dysplasia, and 15 cases (26.8%) of cystadenocarcinoma. Both of the two male patients had cystadenocarcinoma and 9 (60.0%) of the 15 cystadenocarcinomas showed solid nodules in cysts on the preoperative images and in the gross specimen. Univariate analyses showed that male sex (p = 0.019), and solid nodules in cysts (p < 0.001) were both significantly associated with malignancy. In multivariate analysis, the presence of solid nodules in the cysts was the only significant predictive factor of malignancy (p < 0.001). In most cases of cystadenocarcinoma, the prognosis seemed to be not so bad. Among the 15 cystadenocarcinoma cases, follow-up data was available for 10 cases. In two of these cases, patient death occurred five months after surgery because of recurrence. Three patients were alive with disease for a median 26 months. The other remaining 5 cases were alive without recurrence or metastases for a median 58 months of follow-up period. Data on adjuvant treatment was not available in all carcinoma cases.
Although some authors have proposed that early diagnosis is important because primary mucinous cystic neoplasm of the retroperitoneum has the potential to develop a phased progression toward malignancy [10], correct preoperative diagnosis is considered extremely difficult due to a lack of pathognomonic clinical features. Effective and noninvasive diagnostic measures have not yet been established and the condition is often overlooked in differential diagnosis for cystic lymphangiomas, mesenteric cysts, cystic mesothelioma, lymphocele, cystic teratoma or hydatid cysts and etc. However, the presence of septas within a multi loculated cyst is suggestive of either cystic lymphangioma or of mesothelial cyst and the presence of a fat component within the predominant liquid component would also suggest cystic teratoma.
Minimal data are available concerning the treatment of primary retroperitoneal MCN; however, treatment similar to that of its ovarian analog has been considered reasonable. Traditionally, exploratory laparotomy with complete enucleation of the cyst with no spillage is usually indicated for both diagnosis and treatment. The advancement of laparoscopic surgery offers surgeons a useful way of removing retroperitoneal cystic lesions, with further advantages including less postoperative pain, lower morbidity, shorter hospitalization, and an earlier recovery [8,24]. Laparoscopic removal should be avoided if the pathology of the tumor is still unknown or suspected as malignancy because there was one case report [37] of peritoneal seeding after laparoscopic removal including aspiration procedure. Adjuvant treatment after resection of retroperitoneal cystadenocarcinoma is not established because of its rarity. However, if the malignant cyst ruptures or invasive foci are microscopically noted, adjuvant therapy with cisplatinum-based chemotherapy or radiation, or a combination of both, may be performed as in the ovarian counterpart [37].
4. Conclusion
In conclusion, when confronted with a cystic mass in the retroperitoneum, a primary mucinous cystic neoplasm should be considered and complete surgical removal of the tumor without spillage is recommended. In cases in which the patiet is male or there are solid nodules visible in the cysts on preoperative imaging, the possibility of mucinous cystic carcinoma should be kept in mind.
Conflict of interest
There are no any conflict of interest.
Funding
There are no sources of funding for my research.
Consent
I obtained written and signed consent to publish the case report from the patient.
Author contribution
As a 1st author and corresponding author, Seung Eun Lee contributed to all the parts of this article.
Hyung Chul Oh contributed to study design and data collections.
Yong-Gum Park contributed to data analysis and writing.
Yoo Shin Choi contributed to writing and revision.
Mi Kyung Kim contributed to data collections and writing.
References
- 1.Subramony C., Habibpour S., Hashimoto L.A. Retroperitoneal mucinous cystadenoma. Arch. Pathol. Lab. Med. 2001;125:691–694. doi: 10.5858/2001-125-0691-RMC. [DOI] [PubMed] [Google Scholar]
- 2.Navin P., Meshkat B., McHugh S., Beegan C., Leen E., Prins H., Aly S. Primary retroperitoneal mucinous cystadenoma – a case study and review of the literature. Int. J. Surg. Case Rep. 2012;3:486–488. doi: 10.1016/j.ijscr.2012.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tapper E.B., Shrewsberry A.B., Oprea G., Majmudar B. A unique benign mucinous cystadenoma of the retroperitoneum: a case report and review of the literature. Arch. Gynecol. Obstet. 2010;281:167–169. doi: 10.1007/s00404-009-1118-9. [DOI] [PubMed] [Google Scholar]
- 4.Del Gobbo A., Bimbatti M., Ferrero S. A case report of mesenteric mucinous cystoadenoma with review of the literature. BMC Gastroenterol. 2010;10:105. doi: 10.1186/1471-230X-10-105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rifki Jai S., Bouffetal R., Chehab F., Khaiz D., Bouzidi A. Primary retroperitoneal mucinous cystadenoma. Arch. Gynecol. Obstet. 2009;280:479–483. doi: 10.1007/s00404-008-0925-8. [DOI] [PubMed] [Google Scholar]
- 6.Abedalthagafi M., Jackson P.G., Ozdemirli M. Primary retroperitoneal mucinous cystadenoma. Saudi Med. J. 2009;30:146–149. [PubMed] [Google Scholar]
- 7.Yan S.L., Lin H., Kuo C.L., Wu H.S., Huang M.H., Lee Y.T. Primary retroperitoneal mucinous cystadenoma: report of a case and review of the literature. World J. Gastroenterol. 2008;14:5769–5772. doi: 10.3748/wjg.14.5769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ishikawa K., Hirashita T., Araki K., Kitano M., Matsuo S., Matsumata T., Kitano S. A case of retroperitoneal mucinous cystadenoma treated successfully by laparoscopic excision. Surg. Laparosc. Endosc. Percutan. Tech. 2008;18:516–519. doi: 10.1097/SLE.0b013e318174464c. [DOI] [PubMed] [Google Scholar]
- 9.Kim G.Y., Choi D.H., Lim Y.C., Ko B.K., Park S.J., Nah Y.W., Cho H.R. Retroperitoneal mucinous cystadenoma. J. Kor. Surg. Soc. 2008;75:343–346. [Google Scholar]
- 10.Kassab A., El-Bialy G., Clark J., Callen P., Powari M., Jones H. Unusual presentation of 22-kg retroperitoneal müllerian serous cystadenoma. Gynecol. Oncol. 2007;104:257–259. doi: 10.1016/j.ygyno.2006.08.055. [DOI] [PubMed] [Google Scholar]
- 11.Cottrill H.M., Roberts W.S. Primary retroperitoneal mucinous borderline tumor: a case report. Gynecol. Oncol. 2007;106:626–627. doi: 10.1016/j.ygyno.2007.04.023. [DOI] [PubMed] [Google Scholar]
- 12.Green J.M., Bruner B.C., Tang W.W., Orihuela E. Retroperitoneal mucinous cystadenocarcinoma in a man: case report and review of the literature. Urol. Oncol. 2007;25:53–55. doi: 10.1016/j.urolonc.2006.02.015. [DOI] [PubMed] [Google Scholar]
- 13.Thamboo T.P., Sim R., Tan S.Y., Yap W.M. Primary retroperitoneal mucinous cystadenocarcinoma in a male patient. J. Clin. Pathol. 2006;59:655–657. doi: 10.1136/jcp.2005.030122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lai E.C., Chung K.M., Lau W.Y. Primary retroperitoneal mucinous cystadenoma. ANZ J. Surg. 2006;76:537. doi: 10.1111/j.1445-2197.2006.03768.x. [DOI] [PubMed] [Google Scholar]
- 15.Sheen-Chen S.M., Eng H.L. Retroperitoneal mucinous cystadenoma. Dig. Dis. Sci. 2006;51:752–753. doi: 10.1007/s10620-006-3202-3. [DOI] [PubMed] [Google Scholar]
- 16.Matsubara M., Shiozawa T., Tachibana R., Hondo T., Osasda K., Kawaguchi K., Kimura K., Konishi I. Primary retroperitoneal mucinous cystadenoma of borderline malignancy: a case report and review of the literature. Int. J. Gynecol. Pathol. 2005;24:218–223. doi: 10.1097/01.pgp.0000161313.30054.1d. [DOI] [PubMed] [Google Scholar]
- 17.Min B.W., Kim J.M., Um J.W., Lee E.S., Son G.S., Kim S.J., Moon H.Y. The first case of primary retroperitoneal mucinous cystadenoma in Korea: a case report. Kor. J. Intern. Med. 2004;19:282–284. doi: 10.3904/kjim.2004.19.4.282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Arribas D., Cay A., Latorre A., Córdoba E., Martínez F., Lagos J. Retroperitoneal mucinous cystadenoma. Arch. Gynecol. Obstet. 2004;270:292–293. doi: 10.1007/s00404-003-0515-8. [DOI] [PubMed] [Google Scholar]
- 19.Tamura T., Yamataka A., Murakami T., Okada Y., Kobayashi H., Ohshiro K., Lane G.J., Miyano T. Primary mucinous cystadenoma arising from behind the posterior peritoneum of the descending colon in a child: a case report. Asian J. Surg. 2003;26:237–239. doi: 10.1016/S1015-9584(09)60313-4. [DOI] [PubMed] [Google Scholar]
- 20.Erdemoglu E., Aydogdu T., Tokyol C. Primary retro peritoneal mucinous cystadenoma. Acta Obstet. Gynecol. Scand. 2003;82:486–487. doi: 10.1034/j.1600-0412.2003.00158.x. [DOI] [PubMed] [Google Scholar]
- 21.Tangjitgamol S., Manusirivithaya S., Sheanakul C., Leelahakorn S., Thawaramara T., Kaewpila N. Retroperitoneal mucinous cystadenocarcinoma: a case report and review of literature. Int. J. Gynecol. Cancer. 2002;12:403–408. doi: 10.1046/j.1525-1438.2002.01120.x. [DOI] [PubMed] [Google Scholar]
- 22.Balat O., Aydin A., Sirikci A., Kutlar I., Aksoy F. Huge primary mucinous cystadenoma of the retroperitoneum mimicking a left ovarian tumor. Eur. J. Gynaecol. Oncol. 2001;22:454–455. [PubMed] [Google Scholar]
- 23.Kehagias D.T., Karvounis E.E., Fotopoulos A., Gouliamos A.D. Retroperitoneal mucinous cystadenoma. Eur. J. Obstet. Gynecol. Reprod. Biol. 1999;82:213–235. doi: 10.1016/s0301-2115(98)00254-1. [DOI] [PubMed] [Google Scholar]
- 24.Chen J.S., Lee W.J., Chang Y.J., Wu M.Z., Chiu K.M. Laparoscopic resection of a primary retroperitoneal mucinous cystadenoma: report of a case. Surg. Today. 1998;28:343–355. doi: 10.1007/s005950050137. [DOI] [PubMed] [Google Scholar]
- 25.Yunoki Y., Oshima Y., Murakami I., Takeuchi H., Yasui Y., Tanakaya K., Konaga E. Primary retroperitoneal mucinous cystadenoma. Acta Obstet. Gynecol. Scand. 1998;77:357–358. [PubMed] [Google Scholar]
- 26.Ginsburg G., Fraser J., Saltzman B. Retroperitoneal mucinous cystadenoma presenting as a renal cyst. J. Urol. 1997;158:2232. doi: 10.1016/s0022-5347(01)68209-0. [DOI] [PubMed] [Google Scholar]
- 27.Bortolozzi G., Grasso A., Zasso B. Mucinous cystadenoma of the retroperitoneum: A case report and review. Eur. J. Gynaecol. Oncol. 1995;16:65–68. [PubMed] [Google Scholar]
- 28.Gotoh K., Konaga E., Arata A., Takeuchi H., Mano S. A case of primary retroperitoneal mucinous cystadenocarcinoma. Acta Med. Okayama. 1992;46:49–52. doi: 10.18926/AMO/32679. [DOI] [PubMed] [Google Scholar]
- 29.Park U., Han K.C., Chang H.K., Hur M.H. A primary mucinous cystoadenocarcinoma of the retroperitoneum. Gynecol. Oncol. 1991;42:64–67. doi: 10.1016/0090-8258(91)90232-t. [DOI] [PubMed] [Google Scholar]
- 30.Pennell T.C., Gusdon J.P., Jr. Retroperitoneal mucinous cystadenoma. Am. J. Obstet. Gynecol. 1989;160:1229–1231. doi: 10.1016/0002-9378(89)90201-9. [DOI] [PubMed] [Google Scholar]
- 31.Banerjee R., Gough J. Cystic mucinous tumours of the mesentery and retroperitoneum: report of three cases. Histopathology. 1988;12:527–532. doi: 10.1111/j.1365-2559.1988.tb01972.x. [DOI] [PubMed] [Google Scholar]
- 32.Williams P.P., Gall S.A., Prem K.A. Ectopic mucinous cystadenoma. A case report. Obstet. Gynecol. 1971;38:831–837. [PubMed] [Google Scholar]
- 33.Roma A.A., Malpica A. Primary retroperitoneal mucinous tumors: a clinicopathologic study of 18 cases. Am. J. Surg. Pathol. 2009;33:526–533. doi: 10.1097/PAS.0b013e3181909018. [DOI] [PubMed] [Google Scholar]
- 34.Isse K., Harada K., Suzuki Y., Ishiguro K., Sasaki M., Kajiura S., Nakanuma Y. Retroperitoneal mucinous cystadenoma: report of two cases and review of the literature. Pathol. Int. 2004;54:132–138. doi: 10.1111/j.1440-1827.2004.01595.x. [DOI] [PubMed] [Google Scholar]
- 35.Motoyama T., Chida T., Fujiwara T., Watanabe H. Mucinous cystic tumor of the retroperitoneum. A report of two cases. Acta Cytol. 1994;38:261–266. [PubMed] [Google Scholar]
- 36.Rothacker D., Knolle J., Stiller D., Borchard F. Primary retroperitoneal mucinous cystadenomas with gastric epithelial differentiation. Pathol. Res. Pract. 1993;189:1195–1204. doi: 10.1016/S0344-0338(11)80844-7. [DOI] [PubMed] [Google Scholar]
- 37.Song D.E., Kim M., Shin K.K., Yu E., Cho K.J. Primary mucinous cystic neoplasm of the retroperitoneum – a report of three cases. Kor. J. Pathol. 2003;37:204–209. [Google Scholar]


