Abstract
Background
The US Department of State estimates that there are between 4 and 27 million individuals worldwide in some form of modern slavery. Recent studies have demonstrated that 28% to 50% of trafficking victims in the United States encountered health care professionals while in captivity, but were not identified and recognized. This study aimed to determine whether an educational presentation increased emergency department (ED) providers' recognition of human trafficking (HT) victims and knowledge of resources to manage cases of HT.
Methods
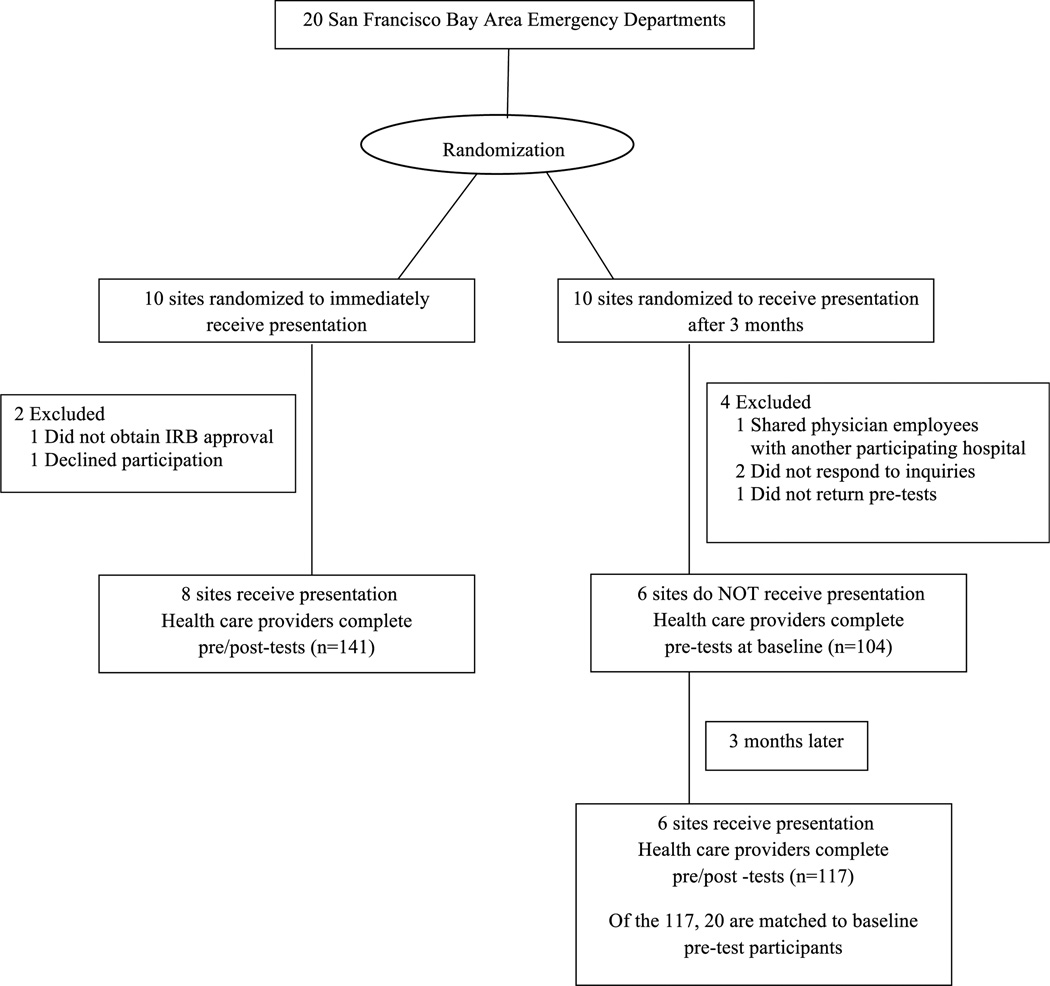
The 20 largest San Francisco Bay Area EDs were randomized into intervention (10 EDs) or delayed intervention comparison groups (10 EDs) to receive a standardized educational presentation containing the following: background about HT, relevance of HT to health care, clinical signs in potential victims, and referral options for potential victims. Participants in the delayed intervention group completed a pretest in the period the immediate intervention group received the educational presentation, and all participants were assessed immediately before (pretest) and after (posttest) the intervention. The intervention effect was tested by comparing the pre–post change in the intervention group to the change in 2 pretests in the delayed intervention group adjusted for the effect of clustering within EDs. The 4 primary outcomes were importance of knowledge of HT to the participant's profession (5-point Likert scale), self-rated knowledge of HT (5-point Likert scale), knowledge of who to call for potential HT victims (yes/no), and suspecting that a patient was a victim of HT (yes/no).
Findings
There were 258 study participants from 14 EDs; 141 from 8 EDs in the intervention group and 117 from 7 EDs in the delayed intervention comparison group, of which 20 served as the delayed intervention comparison group. Participants in the intervention group reported greater increases in their level of knowledge about HT versus those in the delayed intervention comparison group (1.42 vs −0.15; adjusted difference = 1.57 [95% confidence interval, 1.02–2.12]; P < 0.001). Pretest ratings of the importance of knowledge about HT to the participant's profession were high in both groups and there was no intervention effect (0.31 vs 0.55; −0.24 [−0.90–0.42], P = 0.49). Knowing who to call for potential HT victims increased from 7.2% to 59% in the intervention group and was unchanged (15%) in the delayed intervention comparison group (61.4% [28.5%–94.4%]; P < 0.01). The proportion of participants who suspected their patient was a victim of HT increased from 17% to 38% in the intervention group and remained unchanged (10%) in the delayed intervention comparison group (20.9 [8.6%– 33.1%]; P < 0.01).
Interpretation
A brief educational intervention increased ED provider knowledge and self-reported recognition of HT victims.
Keywords: human trafficking, public health, women's health, slavery, social justice
The US Department of State estimates that there are between 4 and 27 million individuals worldwide in some form of modern slavery such as forced labor, bonded labor, forced child labor, or sexual servitude.1 Prevalence estimates of human trafficking (HT) vary widely due to the covert nature of this criminal activity, but HT victims have been identified in cities, suburbs, and rural areas in all 50 states and in Washington, DC.2 In the United States, runaways and youth in the juvenile justice system are at particularly high risk.3–7 Human trafficking persists despite the abolition of slavery in the United States in 18658 and efforts to combat trafficking by the United Nations9 because it is profitable. Worldwide revenues are estimated at $9.5 to $32 billion dollars annually.10,11
Human trafficking has long been recognized as an important issue in the legal, law enforcement, and social service disciplines. However, HT is also an important health care issue12–15 as health care professionals are important for recognizing, caring for, and referring trafficking victims.3,6,12,16–20 Trafficking victims experience a range of physical and psychological health problems resulting from the risks to health involved with trafficking,3,4,12–23 including dangerous workplace conditions, physical and emotional abuse, inhumane living conditions, poor sanitation, inadequate nutrition, and delay in seeking medical care.
Health care professionals play a potentially important but currently largely unrealized role in victim identification and rescue.3,6,12,19 Recent studies have demonstrated that 28% to 50%of trafficking victims in the United States encountered health care professionals while in captivity, but were not identified and recognized.12,21 Indeed, health care providers are among the few professionals likely to encounter these victims while in captivity,3 with emergency department (ED) providers in a unique position to identify and assist HT victims.20
Although ED providers are trained to recognize victims of child abuse and intimate partner violence, they are not routinely educated about the recognition of common health problems of HT victims.7,12,24 A recent study examined the experience of ED personnel with trafficking victims and found that although 29% thought it was a problem in their ED population, only 13% felt confident or very confident that they could identify a HT victim, and less than 3% had ever had any training on recognizing HT victims.24
No prior study has looked prospectively at the effects of educating health care professionals about HT.
This study was designed to determine whether an educational presentation delivered within an existing health care venue changed ED providers' attitudes about the importance of HT to their practices, increased recognition of individuals seen who are or might have been victims of HT, and increased knowledge of resources to manage cases of HT.
METHODS
Study Design and Setting
A group randomized controlled trial examining the effectiveness of a standardized educational presentation about HT and health care using a delayed intervention comparison group was conducted in the 20 largest EDs in the San Francisco (SF) Bay Area. The study was approved by the lead university's institutional review board (IRB) as a multisite study. All sites approved the study through signed consent within the lead university's IRB. Some sites, in addition, required their own IRB approval.
Selection of Participants
The 20 hospitals with the highest number of ED discharges in the SF Bay Area comprised the study population. The California Office of Statewide Health Planning and Development public patient discharge database was used to identify EDs with the highest patient volume in 2008 in 4 SF Bay Area counties: San Francisco, Alameda, San Mateo, and Santa Clara. The Office of Statewide Health Planning and Development collects data on all inpatient discharges from more than 500 California licensed hospitals, excluding federal facilities and prison hospitals.
Between April 2011 and August 2011, EDs in the SF Bay Area were invited to participate in the trial. The EDs were randomized to either an intervention or a delayed intervention comparison group using research randomizer software, as shown in Figure 1. As part of their recruitment and for scheduling purposes, EDs were told whether they would receive the intervention immediately or if they would be delayed. The educational presentations occurred in divisional/departmental meetings or Grand Rounds already existing in these health care venues, and all present ED providers at these meetings (particularly physicians, nurses, and social workers) were invited to join the study. Participants in the institutions that received the intervention immediately took a pretest before the educational intervention and then an immediate posttest. The ED providers in the delayed intervention comparison group institutions were asked to complete the first pretest in the period when the institutions in the intervention arm received the educational presentation. Providers at these institutions took a second pretest immediately before the educational intervention followed by an immediate posttest. Identifying information for the delayed intervention comparison group participants could not be obtained due to IRB restrictions; therefore, individuals who completed the first pretest could not be recontacted and asked to complete the second pretest. Demographic data collected at both pretests (age, sex, profession, and years in practice) were used to determine which respondents in the delayed intervention comparison group completed both pretests. Data for 20 respondents matched on all 4 demographic variables. These 20 individuals comprised the delayed intervention comparison group.
FIGURE 1.
Study design.
Intervention
The intervention consisted of an educational PowerPoint presentation developed in partnership with the San Jose Police Department, a leader in the field of law enforcement and community education about HT. Content of the presentation included background about HT, including local cases; relevance of HT to health care; clinical signs to identify potential victims; and referral options for potential victims including 911, the National Human Trafficking Hotline (1-888-3737-888), and social workers. Presentations were delivered by 1 member of the San Jose Police Department and 1 physician. Due to time constraints at some hospitals, short (25 minutes in divisional/departmental meetings) and long (60 minutes in Grand Rounds) versions of the presentations were developed. Both versions contained the same content and key messages.
Methods and Measurements
An anonymous survey assessed changes in participants' attitudes, knowledge, and recognition of HT victims. The survey was developed in consultation with a research scientist familiar with survey design (M.B.), was pilot tested with 77 subjects, and then revised for clarity. Outcomes included changes to responses on 4 survey questions: (a) It is important for me to know about HT for my profession (responses on a 5-point Likert scale ranging from 1 = strongly disagree to 5 = strongly agree); (b) Please rate your level of knowledge about HT (responses on a 5-point Likert scale ranging from 1 = not at all knowledgeable to 5 = very knowledgeable); (c) I know who to call if I encounter a potential HT victim (yes/no); and (d) I have suspected that a patient of mine was a victim of HT (yes/no). Responses to questions (a) and (b) were dichotomized with the highest 2 responses in one category and the lowest 3 responses in the other.
The survey was administered to participants in person before the intervention presentation and at the conclusion of the presentation. The survey data were entered by research assistants (A.T., M.J.) and data were checked for accuracy by reviewing 25% of the surveys (A.G., S.L., K.C.).
Analysis
The data were summarized using the median and range for continuous measures and counts and proportions for categorical measures. Subject characteristics for both groups were compared using the 2-sample t test for normally distributed measures, the Wilcoxon rank sum test for nonnormally distributed measures, and the χ2 test or Fisher exact test for categorical variables and were not adjusted for the within-ED correlation. Primary analyses included 141 participants from 8 EDs in the intervention group and 20 participants from 4 EDs in the delayed intervention comparison group. Paired differences were calculated for each participant in the intervention (posttest minus pretest) and delayed intervention comparison (second pretest minus first pretest) groups. The intervention effect was assessed by comparing these differences adjusted for the effect of clustering within EDs. The small number of EDs in this study precluded our using linear mixed models or generalized estimating equations. Instead, we used extensions of the 2-sample t test for continuous outcomes and a normal-theory approximation to McNemar test for binary outcomes; to account for the within-ED correlation, we estimated the intraclass correlation coefficient (ICC) and calculated the variance inflation factor (IF) for each outcome, which in turn was used to calculate confidence intervals and test statistics.25,26
Negative estimates of the ICC were attributed to sampling error as the true ICC was assumed to be greater or equal to 0; in such cases, the ICC was set to 0.005 to calculate the IF. Continuous outcomes that were dichotomized were considered to be secondary outcomes. Secondary analyses included all 258 participants from 14 EDs. The change from posttest to pretest was evaluated using extensions of the paired t test for continuous outcomes and McNemar test for binary outcomes adjusted for the within-ED correlation using the IF as described previously.25,26 Sensitivity analyses were undertaken to compare the intervention effect for the shorter (25-minute) and longer (60-minute) intervention and to assess the intervention effect among the subsample of ED physicians. P values less than 0.05 were considered to be statistically significant and no adjustments were made for multiple comparisons. We used SAS version 9.2 for the analyses (SAS Institute Inc, Cary, NC).
Role of the Funding Source
Funding for this research was generously provided by the Community Partnerships Department at Lucile Packard Children's Hospital to Drs Chamberlain and Grace. The members of the San Jose Police Department (Detectives Dotzler and Martinez and Lt. Vanek) were funded in part by a grant from the US Department of Justice Grant/Bureau of Justice Assistance, #2011-VT-BX-K006.
RESULTS
Characteristics of Study Subjects
A total of 258 participants received the presentation; 141 subjects in the immediate intervention group and 117 in the delayed intervention comparison group. Of the 117 participants in the delayed intervention comparison group, 20 had also completed the first pretest and comprise the delayed intervention comparison group for the primary analyses. Participants were in their 30s (delayed intervention comparison group median age 33 years [range, 27–85 y]; intervention group median age 37 years [range, 25–65 y]), approximately equally divided by sex (delayed intervention comparison group 45% men; intervention group 56% men), and most often emergency medicine physicians (Table 1). Participant characteristics were similar for the intervention and delayed intervention comparison groups, although the intervention group included more nonphysicians than the delayed intervention comparison group.
TABLE 1.
Participant Characteristics for the Comparison (n = 20) and Intervention (n = 141) Groups
| Comparison | Intervention | P | |
|---|---|---|---|
| Age, median (range), y | 33 (27–85) | 37 (25–65) | 0.50 |
| Male sex, n (%) | 9 (45.0) | 76 (55.9) | 0.36 |
| Profession, n (%) | 0.008 | ||
| Physician—emergency medicine | 12 (60.0) | 88 (63.3) | |
| Physician—other | 8 (40.0) | 15 (10.8) | |
| Nurse | 0 (0) | 6 (4.3) | |
| Social worker | 0 (0) | 6 (4.3) | |
| Medical student | 0 (0) | 8 (5.8) | |
| Other | 0 (0) | 16 (11.5) | |
| Years seeing patients, median (range) | 8 (3–44) | 12 (0–40) | 0.53 |
Main Results
Initial ratings about the importance of knowledge about HT to the participant's profession were high in both groups, and the intervention effect was not significant (adjusted mean difference = −0.24, 95% confidence interval, [−0.90 to 0.42], P = 0.49) (Table 2). However, changes in responses for the other 3 outcomes were significantly more favorable among participants in the intervention group than the delayed intervention comparison group (P < 0.01). Self-rated knowledge increased by an average of 1.42 points in the intervention group versus −0.15 points in the delayed intervention comparison group (1.57 [1.02–2.12], P < 0.001); similarly, the proportion of participants who rated themselves as knowledgeable/very knowledgeable increased from 7.2% to 59.0% in the intervention group and was unchanged (15.0%) in the delayed intervention comparison group.
TABLE 2.
Adjusted Intervention Effect
| Comparison Group (n = 20) |
Intervention Group (n = 141) |
Adjusted Intervention Effect† | |||||
|---|---|---|---|---|---|---|---|
| ICC* | Pretest 1 | Pretest 2 | Pretest | Posttest | Difference (95% CI) | P | |
| It is important for me to know about HT for my profession | |||||||
| Score [out of 5; mean (SD)] | 0.0377 | 3.70 (0.80) | 4.25 (0.64) | 4.18 (0.91) | 4.49 (0.94) | −0.24 (−0.90 to 0.42) | 0.49 |
| % Agree/strongly agree | 0.1814 | 60.0% | 90.0% | 78.4% | 90.7% | −17.8% (−56.8% to 21.3%) | 0.40 |
| Self-rated level of knowledge about HT | |||||||
| Score [out of 5; mean (SD)] | −0.0102 | 2.30 (1.13) | 2.15 (1.23) | 2.21 (0.91) | 3.63 (0.75) | 1.57 (1.02–2.12) | <0.001 |
| % Knowledgeable/very knowledgeable | −0.0031 | 15.0% | 15.0% | 7.2% | 59.0% | 51.8% (35.1%–68.5%) | <0.001 |
| I know who to call if I encounter a potential HT victim | 0.0806 | 20.0% | 35.0% | 23.6% | 100.0% | 61.4% (28.5%–94.4%) | 0.005 |
| I have suspected that a patient of mine was a victim of HT | 0.0782 | 10.0% | 10.0% | 17.2% | 38.1% | 20.9% (8.6%–33.1%) | 0.003 |
Estimated ICC < 0 were set equal to 0.005 to calculate the variance inflation factor (IF).
The intervention effect was tested by comparing the post-pre change in the intervention group to change from the second to the first pretest in the comparison group, adjusted for the effect of clustering within EDs.
CI indicates confidence interval.
Knowledge of who to call if they encountered a potential victim increased more in the intervention group (from 24% to 100%) than the delayed intervention comparison group (from 20% to 35%): (61.4% [28.5%–94.4%], P = 0.005). Additionally, the proportion of participants in the intervention group who suspected that a patient was a victim of HT doubled (from 17% to 38%), whereas the delayed intervention comparison group remained at 10% (20.9% [8.6%–33.1%], P = 0.003) (Table 2).
In secondary analyses, the change from pretest to posttest was examined using all available data (n = 258) from the delayed intervention comparison (n = 117) and intervention (n = 141) groups. The pattern of results was similar to those observed in the primary analyses (Table 3). However, although posttest scores were not significantly higher for the importance of knowledge about HT to the participant's profession, the proportion who agreed or strongly agreed that knowing about HT was important to their profession were significantly higher on the posttest (91.7% vs 79.2%; 12.5% [4.7%–24.5%], P = 0.05). Self-rated level of knowledge of HT increased by 1.39 points on average [0.84–1.93], P < 0.001. At the pretest, approximately 1 in 4 participants reported knowing who to call when encountering a potential HT victim, whereas nearly all participants at the posttest reported knowing who to call (25.8% vs 98.8%). The proportion of participants who reported suspecting that a patient was a potential victim of HT was twice as high after the presentation than before the presentation (34.8% vs 16.5%, P < 0.001) (Table 3).
TABLE 3.
Comparisons of Pretest and Posttest Scores for all Participants (n = 258)
| Pretest | Posttest | Adjusted Difference* | P | |
|---|---|---|---|---|
| It is important for me to know about HT for my profession | ||||
| Score [out of 5; mean (SD)] | 4.18 (0.89) | 4.54 (0.88) | 0.35 (−0.28 to 0.99) | 0.30 |
| % Agree/strongly agree | 79.2% | 91.7% | 12.5% (4.7%–24.5%) | 0.05 |
| Self-rated level of knowledge about HT | ||||
| Score [out of 5; mean (SD)] | 2.23 (1.01) | 3.62 (0.75) | 1.39 (0.84–1.93) | <0.001 |
| % Knowledgeable/very knowledgeable | 8.8% | 60.9% | 52.1% (45.2%–59.0%) | <0.001 |
| I know who to call if I encounter a potential HT victim | 25.8% | 98.8% | 72.9% (63.5%–82.3%) | <0.001 |
| I have suspected that a patient of mine was a victim of HT | 16.5% | 34.8% | 18.3% (9.1%–27.4%) | <0.001 |
Paired differences between the posttest and pretest, adjusted for the effect of clustering within EDs.
Sensitivity analyses comparing the intervention effect for the shorter (25-minute) and longer (60-minute) intervention showed that the intervention effect was not significantly associated with the length of the intervention (results not shown). The results of additional sensitivity analyses that assessed the intervention effect among the subsample of ED physicians were consistent with the primary findings (results not shown).
DISCUSSION
The results of this study show promise for quickly increasing ED providers' knowledge and awareness about victims of HT. A short, single-session educational presentation statistically significantly increased knowledge about HT and what to do about a potential victim compared to a delayed intervention comparison group. Importantly, this short intervention also sensitized providers to the signs and symptoms of possible victims and produced a statistically significant shift in the percentage of providers in the intervention as compared to those in the delayed intervention comparison group who suspected a victim of HT among their patients. Interestingly, the low percentage of suspected victims of HT before the intervention and the continued low percentage in the delayed intervention comparison group over both pretests is consistent with the reported low levels of identification of victims by medical providers.12,21 The doubling of recognition of possible victims in the intervention as compared to the delayed intervention comparison group medical providers suggests that education may be able to improve identification of HT victims.
Given the potential importance of health care providers in the recognition, care, and referral of victims of HT, a number of recommendations for mandatory education of health care professionals about HT have been proposed. In Illinois and Chicago, recommendations designating physicians as first responders have been made.27,28 The Illinois State Medical Society has also encouraged the American Medical Association to adopt a similar policy and to develop a medical school curriculum on HT.28 To our knowledge, this study is the first to provide evidence that such training could positively impact health care providers' knowledge about and identification of trafficking victims. Importantly, data suggest that physicians in training want to learn about HT. A large survey of Canadian medical students showed that 85% felt it was important or very important to learn about the identification and health needs of trafficked persons.29
The effective use of existing venues within medical care settings to improve knowledge about and recognition of HT is critical if medical providers are to function as effective first responders given the increasing demands on providers. It seems from these data that Grand Rounds and divisional/departmental meetings may be underused to transmit knowledge about this important social issue. Physicians often cite time as a barrier30 in obtaining additional education about social issues. Thus, using existing meetings for education on trafficking and other relevant societal challenges may allow physicians to learn about important topics they might not otherwise have the time to independently explore.
Limitations
As with all data, these have certain limitations. Hospital administrators knew whether they had been randomized to immediate or delayed intervention, possibly introducing some bias. All data are self-report and are subject to reporting biases. Because identifying information for the delayed intervention participants could not be obtained due to IRB restrictions, the individuals who completed the first pretest could not be recontacted and asked to complete the second pretest. Thus, the number of individuals in the delayed intervention comparison group who could be identified as having completed both the first and second pretests is small and may not be representative. This study was conducted in Northern California, a multicultural setting with high levels of immigration and incidence of HT, potentially contributing to increased awareness of the topic before the intervention. It may be the case that the intervention has an even larger impact on physicians practicing in other regions of the United States where there is less awareness of HT. Finally, the time between pretests for the delayed intervention comparison group was considerably longer than the time between the pretests and posttests for the intervention participants, allowing more time for the delayed intervention comparison group participants to potentially be exposed to information on HT, which may have resulted in an underestimation of the effect of the intervention. We anticipate that the impact on the findings, which would have resulted in bias toward the null, was trivial. Regardless of the limitations, these data show a considerable impact of the educational presentation on ED providers' knowledge and recognition of HT.
In summary, HT is an important but underrecognized health issue. A brief educational intervention shows considerable promise for changing health care providers' knowledge and self-reported recognition of HT victims. Within health care settings, Grand Rounds and divisional/departmental meetings seem to be effective venues for educational interventions on important social issues such as HT.
Acknowledgments
Funding for this research was generously provided by the Community Partnerships Department at Lucile Packard Children's Hospital to Drs Chamberlain and Grace. The members of the San Jose Police Department (Detectives Dotzler and Martinez and Lt Vanek) were funded in part by a grant from the US Department of Justice Grant/Bureau of Justice Assistance, #2011-VT-BX-K006.
Footnotes
Disclosure: The authors declare no conflict of interest.
REFERENCES
- 1.U.S. Department of State. Trafficking in Persons Report: June 2007. 2007 Pub. No. 11407, [Google Scholar]
- 2.Polaris Project. [Accessed July 7, 2013];Human Trafficking—The Victims. Polaris Project Web site. Available at: http://www.polarisproject.org/human-trafficking/overview/the-victims.
- 3.Barrows J, Finger R. Human trafficking and the healthcare professional. South Med J. 2008;101:521–524. doi: 10.1097/SMJ.0b013e31816c017d. [DOI] [PubMed] [Google Scholar]
- 4.Hodge DR. Sexual trafficking in the United States: a domestic problem with transnational dimensions. Soc Work. 2008;53:143–152. doi: 10.1093/sw/53.2.143. [DOI] [PubMed] [Google Scholar]
- 5.Anoshiravani A. Personal communication re: human trafficking in the juvenile justice system. San Francisco: 2012. May, [Google Scholar]
- 6.Isaac R, Solak J, Giardino A. Health care providers' training needs related to human trafficking: maximizing the opportunity to effectively screen and intervene. J Appl Res Child. 2011;2 [Google Scholar]
- 7.Ring M, Brantley N. Commercial sexual exploitation of children. Adolescent Health Working Group Ninth Annual Provider Gathering; 2012 April 27; San Francisco, CA. [Google Scholar]
- 8.United States Constitution: Amendment XIII. 1865 [Google Scholar]
- 9.United Nations General Assembly. Protocol to Prevent, Suppress and Punish Trafficking in Persons, Especially Women and Children, supplementing the United Nations Convention against Transnational Organized Crime. [Accessed September 19, 2012];2000 Available at: http://www.unhcr.org/refworld/docid/4720706c0.html. [Google Scholar]
- 10.Belser P. Forced Labor and Human Trafficking: Estimating the Profits. Geneva: International Labour Office; 2005. [Google Scholar]
- 11.U.S. Department of State. Trafficking in Persons Report: June 2004. 2004 Pub. No. 11150. [Google Scholar]
- 12.Family Violence Prevention Fund. Turning Pain Into Power: Trafficking Survivors' Perspectives on Early Intervention Strategies. San Francisco, CA: Family Violence Prevention Fund; 2005. [Google Scholar]
- 13.Gajic-Veljanoski O, Stewart DE. Women trafficked into prostitution: determinants, human rights and health needs. Transcult Psychiatry. 2007;44:338–358. doi: 10.1177/1363461507081635. [DOI] [PubMed] [Google Scholar]
- 14.Gushulak BD, MacPherson DW. Health issues associated with the smuggling and trafficking of migrants. J Immigr Health. 2000;2:67–78. doi: 10.1023/A:1009581817682. [DOI] [PubMed] [Google Scholar]
- 15.Trafficking in women is a health issue. Lancet. 2006;367:1954. doi: 10.1016/S0140-6736(06)68856-9. [DOI] [PubMed] [Google Scholar]
- 16.Crane PM, Morena M. Human trafficking: what is the role of the health care provider? J Appl Res Child. 2011;2:1–27. [Google Scholar]
- 17.Dovydaitis T. Human trafficking: the role of the health care provider. J Midwifery Womens Health. 2010;55:462–467. doi: 10.1016/j.jmwh.2009.12.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Caring for Trafficked Persons: Guidance for Health Providers. Geneva: International Organization for Migration; 2009. International Organization for Migration, United Nations Global Initiative to Fight Human Trafficking, and London School of Hygiene and Tropical Medicine. [Google Scholar]
- 19.Kul S, Galvin JR, Morales O. Responding to human trafficking in Connecticut: a guide for health-care providers. Conn Med. 2007;71:495–497. [PubMed] [Google Scholar]
- 20.Patel RB, Ahn R, Burke TF. Human trafficking in the emergency department. West J Emerg Med. 2010;11:402–404. [PMC free article] [PubMed] [Google Scholar]
- 21.Baldwin SB, Eisenman DP, Sayles JN, et al. Identification of human trafficking victims in health care settings. Health Hum Rights. 2011;13:1–12. [PubMed] [Google Scholar]
- 22.Beyrer C. Global child trafficking. Lancet. 2004;364:16–17. doi: 10.1016/S0140-6736(04)17624-1. [DOI] [PubMed] [Google Scholar]
- 23.Zimmerman C, Hossain M, Yun K. Stolen Smiles: A Summary Report on the Physical and Psychological Health Consequences of Women and Adolescents Trafficked in Europe. London: London School of Hygiene and Tropical Medicine; 2006. [Google Scholar]
- 24.Chisolm-Straker M, Richardson L. Assessment of emergency department provider knowledge about human trafficking victims in the ED. Society for Academic Emergency Medicine Annual Meeting; 2007; Chicago. [Google Scholar]
- 25.Donner A, Klar N. Design and Analysis of Cluster Randomization Trials. London: Arnold; 2000. [DOI] [PubMed] [Google Scholar]
- 26.Yang Z, Sun X, Hardin JW. Confidence intervals for the difference of marginal probabilities in clustered matched-pair binary data. Pharm Stat. 2012;11:386–393. doi: 10.1002/pst.1523. [DOI] [PubMed] [Google Scholar]
- 27.Human Trafficking in California: Final Report. California Attorney General's Office; 2007. California Alliance to Combat Slavery and Trafficking Task Force. [Google Scholar]
- 28.Anderson T. Educating Medical Providers as First-Line Responders to Stop Human Trafficking. Illinois State Medical Society House of Delegates, Resolution 19. [Accessed July 17, 2012];2012 Available at http://www.isms.org/hod/2012res/Pages/res19.aspx. [Google Scholar]
- 29.Wong JC, Hong J, Leung P, et al. Human trafficking: an evaluation of Canadian medical students' awareness and attitudes. Educ Health (Abingdon) 2011;24:1–10. [PubMed] [Google Scholar]
- 30.Stafford S, Sedlak T, Fok MC, et al. Evaluation of resident attitudes and self-reported competencies in health advocacy. BMC Med Educ. 2010;10:82. doi: 10.1186/1472-6920-10-82. [DOI] [PMC free article] [PubMed] [Google Scholar]