Abstract
Background
We examined the relation between objectively measured physical activity with accelerometry and subcutaneous adipose tissue (SAT) and visceral adipose tissue (VAT) in a community‐based sample.
Methods and Results
We evaluated 1249 participants of the Framingham Third Generation and Omni II cohorts (mean age 51.7 years, 47% women) who underwent assessment of moderate‐to‐vigorous physical activity (MVPA) with accelerometry over 5 to 7 days, and multi‐detector computed tomography for measurement of SAT and VAT volume; fat attenuation was estimated by SAT and VAT hounsfield units (HU). In women, higher levels of MVPA were associated with decreased SAT (P<0.0001) and VAT volume (P<0.0001). The average decrement in VAT per 30 minute/day increase in MVPA was −453 cm3 (95% CI −574, −331). The association was attenuated but persisted upon adjustment for BMI (−122 cm3, P=0.002). Higher levels of MVPA were associated with higher SAT HU (all P≤0.01), a marker of fat quality, even after adjustment for SAT volume. Similar findings were observed in men but the magnitude of the association was less. Sedentary time was not associated with SAT or VAT volume or quality in men or women.
Conclusions
MVPA was associated with less VAT and SAT and better fat quality.
Keywords: accelerometry, physical activity, visceral adipose tissue
Introduction
Obesity risk is nearly cut in half in adults who participate in regular moderate‐intensity physical activity compared with inactive adults.1 Importantly, physically active adults across all weight categories (normal, overweight, and obese) have lower risk for adverse outcomes.2 Physical activity reduces risk of abdominal obesity known to be strongly associated with cardiometabolic risk.3 Higher levels of self‐reported physical activity are associated with lower visceral adipose tissue (VAT) in both younger and older women4 and with both VAT and subcutaneous adipose tissue (SAT) in men and women.5–6 Importantly, randomized trials have demonstrated reductions in visceral fat with moderate amounts of aerobic exercise.7–8
Many prior reports are limited by use of self‐reported physical activity obtained by questionnaire, which can be hampered by recall bias as well as the inability to accurately quantify physical activity levels.9 Advances in technology permit objective measurement of physical activity with accelerometers. Compared with accelerometer‐measured physical activity, participants self‐report more vigorous physical activity and less sedentary time.10 In a large nationally representative sample, increased physical activity measured with accelerometry was associated with decreased body mass index and waist circumference.11 Little is known about the relation of accelerometer‐measured physical activity duration and intensity and VAT and SAT. In a small study of inactive men and women, physical activity occurring through activities of daily living was not associated with abdominal obesity but sporadic moderate to vigorous physical activity measured with accelerometry was negatively associated with VAT.12
Cellular characteristics of adipose tissue such as adipocyte size and lipid content,13 inflammatory response,14 and reduced oxygenation15 have been associated with adverse metabolic risk in animal models and humans. A noninvasive measure of fat quality defined with computed tomography imaging Hounsfield Units (HU) in humans has been previously associated with metabolic risk factors,16 subclinical atherosclerosis,17 and mortality18 independent of fat volume. The relation of physical activity to fat quality has not been well studied.
The aim of the present study was to examine the relation between objectively measured physical activity using accelerometry and both SAT and VAT volumes and quality assessed by multidetector CT scan in a large community‐based sample of middle‐aged men and women. We hypothesized that men and women with higher levels of moderate‐to‐vigorous intensity physical activity (MVPA) would have lower levels of SAT and VAT volumes and further that MVPA performed in bouts of at least 10 minutes would be associated with lower levels of SAT and VAT. Furthermore, we hypothesized that higher levels of MVPA would be associated with improved measures of VAT and SAT quality.
Methods
Study Sample
The 4095 Framingham Heart Study Third Generation Cohort (Gen 3) participants were enrolled and attended their first research examination from 2002 to 2005.19 Details of the design and recruitment procedures of the Gen 3 cohort have been previously published. Because the Framingham cohorts are predominantly white of European ancestry, a racially and ethnically diverse sample (Omni) was drawn from Framingham, Massachusetts and the surrounding towns to reflect the current diversity. At the time of the Gen 3 recruitment, the 410 participants in Omni sample II (Omni II) were recruited. At each research examination participants undergo a medical history interview, laboratory testing, and noninvasive vascular testing. At the second examination of the Gen 3 and Omni II participants from 2008 to 2011, participants were invited to wear an actical accelerometer. Of 3732 participants attending the exam, 2915 participants had accelerometry data available that passed quality control checks. Participants were excluded if they were not part of the Framingham Multi‐detector CT Study or had missing SAT or VAT data (n=1589), or missing covariate data (n=3). We additionally excluded 74 participants with 4 or fewer valid days of accelerometry wear time. Our final study sample included 1249 participants (1133 Gen 3 participants and 116 Omni II participants). Participants excluded from the study were younger and were more likely to be current smokers (See Table S3 for detailed characteristics of the excluded sample). The median time between physical activity assessment and the Multi‐detector CT scan was within 1 month (lower quartile −0.03 months, upper quartile 3.9 months). The Institutional Review Board at Boston Medical Center approved this study and all participants provided written informed consent.
Physical Activity by Accelerometry
Physical activity was recorded using an omnidirectional Actical accelerometer (Philips Respironics, Bend, OR) as previously described.20 Briefly, at the time of their routine research examination participants were asked to wear the Actical device home on a waist‐worn belt for 8 days to achieve a full 7 days of wear time. Activity was recorded as “counts” summed over 30‐second epochs. Participants were blinded to activity counts while wearing the actical monitor. After return of the actical device, the data was downloaded by clinic staff and processed using Kinesoft software (Kinesoft, Saskatchewan, Canada) that included routine quality control checks. A valid day was defined as a minimum of 10 hours of wear time and accelerometer data files were used for this study if there were a minimum of 5 valid wear days.
Accelerometer count thresholds were applied based on previously reported intensity thresholds21–22 as follows: sedentary time less than 200 counts/minute; light activity 200 to 868 counts/minute; moderate intensity activity 870 to 5070 counts/minute and >5070 counts/minute for vigorous activity, corresponding to 3 to 6 MET values for moderate intensity activity and >6 METS for vigorous activity. Total physical activity time at each intensity level was the sum of minutes at that intensity level during the time the accelerometer was worn. Bouts were defined as the sum of moderate and vigorous physical activity (MVPA) accumulated in bouts of at least 10 minutes allowing for up to a 2‐minute interruption anywhere in the bout. The interruption simulates real‐life conditions such as slowing a jog at a traffic light. Current physical activity guidelines for health recommend that adults get 150 minutes of MVPA per week with the MVPA accumulated in bouts of at least 10 minutes (http://www.health.gov/paguidelines).
Multi‐detector CT Study: Measurement of VAT and SAT Volumes and Quality
An 8‐slice multi‐detector computed tomography scan of the abdomen was obtained as previously described (LightSpeed Ultra, General Electric, Milwaukee, WI).23 Subcutaneous adipose tissue (SAT) and visceral adipose tissue (VAT) volumes (Aquarius 3D Workstation, TeraRecon Inc, San Mateo, CA), were acquired by manually tracing the abdominal muscular wall. Applying an image display window of −195 to −45 Hounsfield Units (HU) results in semi‐automatic quantification of SAT and VAT volumes. We also recorded the average HU of each fat depot.16 Lower CT attenuation (lower HU values) is a noninvasive measure of fat quality associated with adipose tissue with higher lipid content and adverse cardiometabolic risk beyond absolute adipose tissue volume.16 Interclass correlations for inter‐reader comparisons were 0.997 for SAT and 0.992 for VAT23; the intra‐class correlations were 0.99 for SAT and VAT.
Covariates/Characteristics
At the time of the routine research examination, participants were asked to report their race, education (highest degree of level of school: grades 1 to 8, grades 9 to 11, completed high school, some college but no degree, technical school certificate, associate degree, bachelor's degree, graduate or professional degree), current employment state and current occupation. Height and weight were measured by trained technicians and body mass index (BMI) was calculated as weight in kilograms divided by height in meters squared. Normal weight was defined as BMI <25 mg/kg2, overweight 25 to <30 mg/kg2 and obese ≥30 mg/kg2. A participant was considered a current smoker if he or she reported smoking at least 1 cigarette per day over the year preceding the examination. Participants reported the number of hours per day spent in sleep, sedentary, slight, moderate, and heavy activities to calculate the physical activity index.
Statistical Analysis
As prior work from our group identified sex specific differences in SAT and VAT volume associations24 all analyses were conducted stratified by sex. Sex specific Pearson correlation coefficients were calculated to assess the correlations between physical activity levels and SAT and VAT volumes and quality measured by Hounsfield units (HU). Separate multivariable linear regression models were used to examine the cross‐sectional association of each physical activity measure (MVPA, MVPA bouts, met MVPA guidelines, and sedentary time) with adipose tissue volumes and quality (dependent variables). The primary model adjusted for age, education, cohort (Gen 3/Omni II), race, and actical wear time in minutes per day. The beta estimate gives the average increment in the dependent variable (SAT, VAT, SAT HU, or VAT HU) per 30 minute/day increase in MVPA or sedentary time. The beta estimate for the dependent variable, met the guidelines, gives the average difference in SAT or VAT volume for participants who met the guidelines versus for participants not meeting the guidelines. In secondary analyses of fat volumes we additionally adjusted for VAT volume in models predicting SAT volume. Similarly, we additionally adjusted for SAT volume in models predicting VAT volume. Additionally, these models (those predicting VAT volume) were also (separately) adjusted for BMI. Models predicting VAT volume were also run by BMI category. In models evaluating fat attenuation (quality), we additionally adjusted for fat volume and BMI (separately). Finally we conducted separate models adjusting for waist circumference and waist to height ratio. All analyses were performed using SAS version 9.3 (SAS Institute, Cary, NC). P‐values<0.05 were considered statistically significant.
Results
The sample was nearly half women (47%), middle‐aged (mean age 52.0 years in women and 49.6 years in men), predominantly white, and well educated (>80% had more than a high school education) (Table 1). More men than women were employed full‐time and reported manual labor type employment. Over 90% of the sample spent ≥10 hours per day in sedentary time. On average, women recorded 24 minutes/day in MVPA while men recorded 29 minutes/day in MVPA and 42.7% of women and 55.8% of men met the guideline for MVPA (≥150 minutes/week). However, only 13.3% of women and 11.8% of men met the MVPA guidelines for activity performed in bouts of at least 10 minutes.
Table 1.
Characteristics of the Study Sample
| Characteristic: Mean (SD) or % (N) | Women (N=586) | Men (N=663) |
|---|---|---|
| Age, y | 52.0 (7.1) | 49.6 (7.0) |
| BMI, kg/m2 | 27.6 (6.0) | 28.8 (4.4) |
| Normal | 40.4 (237) | 19.6 (130) |
| Overweight | 31.4 (184) | 46.9 (311) |
| Obese | 28.2 (165) | 33.5 (222) |
| Race | ||
| White, % | 93.0 (545) | 94.9 (629) |
| African American or Black, % | 3.1 (18) | 1.8 (12) |
| Asian, % | 3.2 (19) | 2.6 (17) |
| American Indian or Alaska native, % | 0.9 (5) | 1.4 (9) |
| Highest level of education | ||
| High school or less, % | 16.0 (94) | 15.5 (103) |
| Some college/Associate degree/Technical, % | 32.1 (188) | 30.2 (200) |
| College degree, % | 31.7 (186) | 33.8 (224) |
| Graduate or professional degree | 20.1 (118) | 20.5 (136) |
| Employment status | ||
| Homemaker, not working outside home | 8.6 (50) | 0.5 (3) |
| Employed full time | 56.6 (331) | 83.1 (551) |
| Employed part time | 20.7 (121) | 4.1 (27) |
| Employed, but on leave | 0.5 (3) | 0.2 (1) |
| Unemployed or laid off | 4.1 (24) | 4.2 (28) |
| Retired from usual occupation | 6.3 (37) | 5.1 (34) |
| Full‐time student | 0.3 (2) | |
| Other | 2.4 (14) | 2.5 (16) |
| Manual labor employment | 1.9 (11) | 17.6 (117) |
| Current smoking | 7.2 (42) | 9.4 (62) |
| Physical activity index | 35.7 (5.6) | 37.0 (7.8) |
| Sedentary, h/day | ||
| ≤9 | 4.8 (28) | 10.0 (66) |
| 10 | 20.1 (118) | 19.2 (127) |
| 11 | 31.6 (185) | 35.0 (232) |
| 12 | 32.4 (190) | 26.4 (175) |
| ≥13 | 11.1 (65) | 9.5 (63) |
| Light time, min/day | 126.2 (43.7) | 139.6 (53.2) |
| MVPA, min/day | 24.1 (19.6) | 28.9 (20.6) |
| Met MVPA guidelines, % | 42.7 (250) | 55.8 (370) |
| MVPA bouts, min/day | 9.4 (14.2) | 7.6 (11.5) |
| Met MVPA bouts guidelines, % | 13.3 (78) | 11.8 (78) |
| Wear time, 7 days, % | 73.4 (430) | 71.3 (473) |
| SAT, cm3 | 3710 (1785) | 2972 (1325) |
| VAT, cm3 | 1457 (978) | 2818 (1339) |
| SAT HU | −107 (5) | −105 (4) |
| VAT HU | −91 (6) | −96 (6) |
BMI indicates body mass index; HU, hounsfield unit; MVPA, moderate‐to‐vigorous physical activity; SAT, subcutaneous adipose tissue; SD, standard deviation; VAT, visceral adipose tissue.
Pearson Correlation Coefficients
MVPA and MVPA bouts were negatively correlated with SAT and VAT volume and positively correlated with SAT and VAT HU in women (all P<0.0001, Table 2). Similar associations were observed in men but the magnitude of the correlation was weaker. There was not evidence of a linear relationship between sedentary time and measures of SAT and VAT volume or quality.
Table 2.
Age‐adjusted Sex Specific Pearson Correlation Coefficients Between the Physical Activity Level and Adiposity Measures
| Women (min/day) | Men (min/day) | |||||||
|---|---|---|---|---|---|---|---|---|
| Sedentary Time | Light | MVPA | MVPA Bouts | Sedentary Time | Light | MVPA | MVPA Bouts | |
| Age, y | 0.03 | −0.18** | −0.21** | −0.11* | 0.01 | −0.15** | −0.17** | 0.04 |
| BMI, kg/m2 | 0.02 | −0.06 | −0.28** | −0.24** | −0.04 | −0.0004 | −0.06 | −0.07 |
| VAT, cm3 | 0.02 | −0.08 | −0.31** | −0.28** | −0.001 | −0.08* | −0.12** | −0.08* |
| SAT, cm3 | 0.004 | −0.05 | −0.28** | −0.24** | −0.01 | −0.07 | −0.07 | −0.05 |
| VAT HU | −0.05 | 0.05 | 0.29** | 0.25** | −0.04 | 0.06 | 0.12* | 0.11* |
| SAT HU | 0.04 | −0.02 | 0.26** | 0.25** | −0.04 | 0.05 | 0.12* | 0.10* |
BMI indicates body mass index; HU, hounsfield unit; MVPA, moderate‐to‐vigorous physical activity; SAT, subcutaneous adipose tissue; VAT, visceral adipose tissue.
*P<0.05; **P<0.001.
Association Between Physical Activity and Fat Volumes
In women, all measures of MVPA were significantly associated with decreased SAT volume (P<0.0001, Table 3). The average decrement in SAT per 30 minute/day increase in MVPA was −776 cm3 (95% CI −1003, −549). Women meeting MVPA guidelines had on average −997 cm3 (95% CI −1291, −703) less SAT volume than those not meeting MVPA guidelines. Similar findings were observed for MVPA performed in bouts. The associations between SAT volume and all measures of MVPA in women were markedly attenuated and no longer significant after adjustment for BMI and after adjustment for VAT volume (data not shown). In men, associations between MVPA and SAT volumes were much smaller and did not reach statistical significance. Sedentary time was not significantly associated with SAT in women or men.
Table 3.
Sex Specific Multivariable‐Adjusted* Association Between Physical Activity and SAT/VAT Volumes
| Physical Activity Level | SAT | VAT | ||||||
|---|---|---|---|---|---|---|---|---|
| Women, β (95% CI) | P Value | Men, β (95% CI) | P Value | Women, β (95% CI) | P Value | Men, β (95% CI) | P Value | |
| MVPA | −776 (−1003, −549) | <0.0001 | −132 (−285, 20) | 0.09 | −453 (−574, −331) | <0.0001 | −228 (−377, −78) | 0.003 |
| +BMI | −77 (−184, 30) | 0.16 | −45 (−132, 42) | 0.31 | −122 (−200, −44) | 0.002 | −147 (−243, −52) | 0.003 |
| MVPA bouts | −871 (−1176, −566) | <0.0001 | −143 (−410, 124) | 0.29 | −524 (−688, −361) | <0.0001 | −232 (−495, 30) | 0.08 |
| +BMI | −85 (−226, 56) | 0.24 | −28 (−180, 124) | 0.72 | −151 (−254, −49) | 0.004 | −127 (−294, 41) | 0.14 |
| Met MVPA guideline | −997 (−1291, −703) | <0.0001 | −161 (−372, 50) | 0.13 | −579 (−737, −422) | <0.0001 | −337 (−544, −131) | 0.001 |
| +BMI | −71 (−209, 68) | 0.32 | −35 (−156, 85) | 0.57 | −141 (−242, −39) | 0.01 | −222 (−354, −90) | 0.001 |
| Met MVPA bout guidelines | −981 (−1405, −557) | <0.0001 | −143 (−458, 171) | 0.37 | −580 (−808, −352) | <0.0001 | −180 (−490, 129) | 0.25 |
| +BMI | −80 (−272, 113) | 0.42 | −12 (−191, 167) | 0.89 | −150 (−290, −9) | 0.04 | −59 (−257, 139) | 0.56 |
| Sedentary time | 1.1 (−77.9, 80.2) | 0.98 | 9.7 (−38.1, 57.4) | 0.69 | 9.3 (−33.3, 51.9) | 0.67 | 8.0 (−38.9, 55.0) | 0.74 |
| +BMI | −15.2 (−49.8, 19.3) | 0.39 | 26.3 (−0.8, 53.4) | 0.06 | 1.4 (−23.9, 26.8) | 0.91 | 23.3 (−6.6, 53.3) | 0.13 |
BMI indicates body mass index; CI, confidence interval; HU, hounsfield unit; MVPA, moderate‐to‐vigorous physical activity; SAT, subcutaneous adipose tissue; VAT, visceral adipose tissue.
Adjusted for age, education, cohort, race, and actical wear time; the beta estimate is the average increment in the dependent variable (SAT or VAT) per 30 minute/day increase in MVPA or sedentary time.
All measures of MVPA were significantly associated with decreased VAT volume in women (P<0.0001, Table 3). The average decrement in VAT per 30 minute/day increase in MVPA was −453 cm3 (95% CI −574, −331) and the average decrement in VAT for women meeting MVPA guidelines versus women not meeting guidelines was −579 cm3 (95% CI −737, −422). Similar associations were observed for MVPA performed in bouts. The associations between MVPA measures and VAT volume were similar in men but the magnitude of the association was less. Among women, associations between MVPA and VAT were attenuated but remained significant upon adjustment for BMI (Table 3) and for SAT volume (data not shown). Adjustment for waist circumference and waist‐to‐height ratio separately (Table S1) provide associations between MVPA and VAT that are similar to those obtained from models adjusting for BMI. Associations between meeting MVPA guidelines and VAT were consistent across all weight categories (normal, overweight, and obese) in men and women (Figure). There was increased VAT with increasing BMI category with less VAT in those meeting guidelines versus not. Sedentary time was not associated with VAT volume in men or women.
Figure 1.
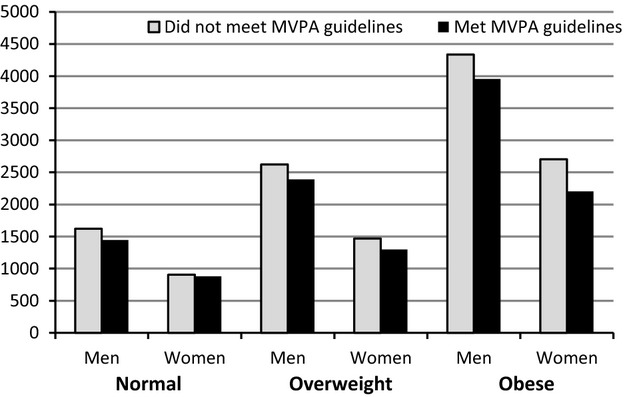
Mean* VAT volume in cm3 among men and women by BMI category. *Means are adjusted for age, education, cohort, race, and actical wear time (provided from sex‐specific regression models stratified by BMI category). BMI indicates body mass index; MVPA, moderate‐to‐vigorous physical activity; VAT, visceral adipose tissue.
Association Between Physical Activity and Fat Attenuation
MVPA measures were positively associated with SAT HU in women (all P<0.0001) and men (P≤0.01 except met MVPA bout guidelines) (Table 4). MVPA was positively associated with SAT HU consistent with less lipid‐rich adipose tissue quality. The associations were attenuated but generally remained significant after adjustment for absolute SAT volume and for BMI (separately). Adjustment for waist circumference and waist‐to‐height ratio are similar to results obtained from models adjusting for BMI (Table S2). MVPA was also positively associated with VAT HU in both women and men however upon adjusted for VAT volume the relation was no longer significant. Similarly meeting MVPA guidelines was positively associated with VAT HU. The association persisted upon adjustment for VAT volume but was attenuated and no longer significant after adjustment for BMI. Sedentary time was not associated with SAT or VAT HU.
Table 4.
Sex Specific Multivariable‐Adjusted* Association Between Physical Activity and SAT/VAT Quality
| Physical Activity | SAT HU | VAT HU | ||||||
|---|---|---|---|---|---|---|---|---|
| Women, β (95% CI) | P Value | Men, β (95% CI) | P Value | Women, β (95% CI) | P Value | Men, β (95% CI) | P Value | |
| MVPA | 1.67 (1.09, 2.24) | <0.0001 | 0.74 (0.30, 1.19) | 0.001 | 2.71 (1.90, 3.52) | <0.0001 | 1.25 (0.52, 1.97) | 0.0008 |
| +Volume | 0.60 (0.10, 1.11) | 0.02 | 0.51 (0.15, 0.87) | 0.005 | 0.11 (−0.32, 0.54) | 0.62 | 0.27 (−0.07, 0.62) | 0.12 |
| +BMI | 0.86 (0.31, 1.42) | 0.002 | 0.59 (0.20, 0.99) | 0.003 | 0.87 (0.23, 1.50) | 0.008 | 0.92 (0.37, 1.47) | 0.001 |
| MVPA bouts | 2.22 (1.45, 2.98) | <0.0001 | 1.08 (0.29, 1.86) | 0.007 | 3.10 (2.02, 4.19) | <0.0001 | 1.61 (0.34, 2.89) | 0.013 |
| +Volume | 1.03 (0.36, 1.69) | 0.0025 | 0.83 (0.20, 1.45) | 0.01 | 0.09 (−0.48, 0.66) | 0.75 | 0.62 (0.02, 1.22) | 0.04 |
| +BMI | 1.31 (0.59, 2.03) | 0.0004 | 0.88 (0.19, 1.57) | 0.01 | 1.02 (0.18, 1.86) | 0.017 | 1.18 (0.21, 2.14) | 0.017 |
| Met MVPA guideline | 1.76 (1.00, 2.51) | <0.0001 | 0.99 (0.38, 1.61) | 0.0017 | 3.62 (2.57, 4.67) | <0.0001 | 1.85 (0.85, 2.85) | 0.0003 |
| +Volume | 0.36 (−0.30, 1.02) | 0.28 | 0.71 (0.22, 1.21) | 0.005 | 0.31 (−0.25, 0.87) | 0.27 | 0.41 (−0.07, 0.89) | 0.10 |
| +BMI | 0.66 (−0.06, 1.38) | 0.07 | 0.78 (0.24, 1.33) | 0.005 | 1.19 (0.37, 2.02) | 0.0046 | 1.37 (0.61, 2.13) | 0.0004 |
| Met MVPA bout guidelines | 2.92 (1.86, 3.98) | <0.0001 | 0.71 (−0.22, 1.63) | 0.135 | 3.73 (2.22, 5.24) | <0.0001 | 0.96 (−0.54, 2.47) | 0.21 |
| +Volume | 1.57 (0.67, 2.48) | 0.0007 | 0.45 (−0.29, 1.19) | 0.23 | 0.41 (−0.37, 1.18) | 0.30 | 0.19 (−0.52, 0.90) | 0.60 |
| +BMI | 1.88 (0.89, 2.86) | 0.0002 | 0.48 (−0.33, 1.30) | 0.25 | 1.33 (0.19, 2.48) | 0.02 | 0.46 (−0.68, 1.60) | 0.43 |
| Sedentary time | 0.10 (−0.10, 0.30) | 0.32 | −0.12 (−0.26, 0.02) | 0.09 | −0.14 (−0.43, 0.14) | 0.32 | −0.12 (−0.35, 0.11) | 0.31 |
| +Volume | 0.10 (−0.06, 0.27) | 0.22 | −0.11 (−0.22, 0.01) | 0.06 | −0.09 (−0.23, 0.05) | 0.20 | −0.08 (−0.19, 0.02) | 0.13 |
| +BMI | 0.12 (−0.06, 0.30) | 0.18 | −0.15 (−0.27, −0.03) | 0.016 | −0.10 (−0.31, 0.11) | 0.35 | −0.18 (−0.35, −0.01) | 0.04 |
BMI indicates body mass index; CI, confidence interval; HU, hounsfield unit; MVPA, moderate to vigorous physical activity; SAT, subcutaneous adipose tissue; VAT, visceral adipose tissue; Volume, SAT volume for SAT HU models; VAT volume for VAT HU models.
Adjusted for age, education, cohort, race, and actical wear time; the beta estimate is the average increment in the dependent variable (SAT HU, or VAT HU) per 30 minute/day increase in MVPA or sedentary time.
Discussion
In our large community‐based sample of middle‐aged men and women, several important findings regarding the association between physical activity levels and adipose tissue volumes and quality were observed. First, MVPA performed in both bouts and non‐bouts was associated with lower SAT and VAT volumes in women. In men, MVPA was associated with lower VAT volumes. The magnitude of the associations between MVPA and the adipose tissue depots were greater in women than men. Second, with respect to fat quality, MVPA was positively associated with SAT attenuation in both women and men. Physical activity intensity levels were not associated with VAT attenuation. Third, sedentary time was not associated with adipose tissue volumes or quality in men or women.
Moderate‐to‐Vigorous Physical Activity
In a nationally representative sample, objectively measured MVPA with accelerometry was associated with decreased odds of obesity with even small differences in MVPA (5 to 10 minutes/day) associated with large differences in obesity risk.25 The strength of the association between objectively measured MVPA and lower BMI and smaller waist circumference is stronger for MVPA performed in bouts versus non‐bouts likely because bout minutes are performed at a higher intensity level than non‐bout minutes.11 However, for weight gain prevention all physical activity performed at higher intensity is beneficial suggesting that every minute counts.26
Data examining regional adipose tissue depots and objectively measured MVPA are sparse and suggest physical activity may influence adipose tissue depots differently in men and women.27 One small weight loss study noted that among men light activity was inversely associated with VAT while in women total active time was inversely associated with VAT.27 In normal weight Japanese women (n=42), very brief bouts of non‐exercise physical activity was associated with lower VAT.28 Sporadic MVPA was negatively associated with VAT in a sample of inactive men and women.12 Our study extends this knowledge with a large middle‐aged community‐based sample demonstrating that MVPA performed in both bouts and non‐bouts is associated with decreased VAT in both women and men but with a larger effect in women. Further the association is observed across all BMI categories (normal, overweight, and obese). VAT is a metabolically active fat depot associated with higher levels of metabolic risk factors24 including insulin resistance.29 Hence, interventions to decrease VAT may improve metabolic risk. For overweight and obese persons, a moderate amount of aerobic exercise was associated with lower measures of visceral fat and improved measures of insulin resistance.7
In both men and women in our sample, MVPA is associated positively with SAT quality (higher CT attenuation) even after accounting for SAT volume and BMI. This finding is important because lower CT attenuation of SAT is associated with adverse cardiometabolic risk16 and all‐cause mortality, non‐cardiovascular disease mortality, and cancer mortality.18 Therefore, physical activity time and intensity may not only improve adipose tissue volumes but also improve qualitative indices of the fat depots that provide further insights into metabolic risk.
Sedentary Time
There have been global trends demonstrating increasing time spent in sedentary behaviors.30 Consistent with other population‐based samples, the vast majority of accelerometer time in our sample was sedentary (>90% of the sample spent ≥10 hours/day in sedentary time). Using data from NHANES, a nationally representative community‐based sample, men and women age 40 to 59 years spent a mean of 509 (SD 124) and 498 (SD 147) minutes/day in sedentary time respectively.31 This is somewhat less than our sample however sedentary time was defined as <100 counts/minute in that study whereas in our study sedentary time was defined as <200 counts/minute likely resulting in the greater amount of time spent in sedentary behavior in our sample. In older Icelandic men and women32 and women participating in the Women's Health Study33 about 10 hours/day on average was spent in sedentary time. Sedentary time has been linked to a number of adverse cardiometabolic health outcomes34–35 including increased mortality risk36 even after accounting for MVPA. The mechanisms driving the health risks associated with sedentary time remain to be determined but may be related in part to associations with regional fat depots.37
Data are conflicting with respect to the association between sedentary time and VAT. In adult men and women who reported sedentary behavior at baseline and at 6‐year follow‐up, there was no association between baseline sedentary behavior or change in sedentary behavior and longitudinal change in VAT.38 One small study suggests a positive association between accelerometer‐derived sedentary time and VAT among women only27 whereas a second small study did not find an association in women or men.12 In our large community‐based sample we did not observe an association between sedentary time and VAT or SAT or measures of adipose tissue quality. To date, it is not clear that accumulation of VAT is a factor linking sedentary behavior to cardiometabolic risk.
Several potential limitations of this study merit comment. Our study was cross‐sectional and therefore we cannot infer causality. Our sample was primarily white and thus our findings may not be generalizable to other race/ethnic groups. Given the modest size of the non‐white participants we were not able to conduct an investigation in each race/ethnic group. The accelerometer captures activity and does not distinguish purposeful leisure time physical activity and occupational physical activity. High levels of occupational activity are associated with lower likelihood of being obese.1 Employment patterns (prevalence of full vs part‐time work) and prevalence of manual type of labor differed between men and women in our sample. It is unclear if differences in occupational activity may have contributed to sex differences in the associations detected. Trends in no leisure‐time activity have improved in the general population and are not different in men and women.39 However, the type, duration, and intensity of physical activity may differ between men and women. We did not correct for multiple comparisons as there are correlations among the fat measures, therefore we consider our findings hypothesis generating.
Conclusions
In our large community‐based sample of middle‐aged men and women, MVPA was associated with lower SAT and VAT volumes in women and lower VAT volume in men. MVPA was also associated with improved SAT quality defined by fat attenuation. Promoting interventions to increase physical activity time and intensity in the community may have a positive impact on the adipose tissue depots associated with the greatest cardiometabolic risk.
Sources of Funding
The National Heart, Lung and Blood Institute's Framingham Heart Study is supported by contract N01‐HC‐25195. The accelerometry study was supported by R01AG047645.
Disclosures
Alison Pedley is an employee of Merck and Co, Inc. Dr Massaro, Dr Murabito, and Dr Vasan received support from N01‐HC‐25195 to oversee collection, quality control, and analyses of the accelerometry data. Dr. Vasan received additional support from R01AG047645.
References
- King GA, Fitzhugh EC, Bassett DR, Jr, McLaughlin JE, Strath SJ, Swartz AM, Thompson DL. Relationship of leisure‐time physical activity and occupational activity to the prevalence of obesity. Int J Obes Relat Metab Disord. 2001; 25:606-612. [DOI] [PubMed] [Google Scholar]
- Li TY, Rana JS, Manson JE, Willett WC, Stampfer MJ, Colditz GA, Rexrode KM, Hu FB. Obesity as compared with physical activity in predicting risk of coronary heart disease in women. Circulation. 2006; 113:499-506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steeves JA, Bassett DR, Jr, Thompson DL, Fitzhugh EC. Relationships of occupational and non‐occupational physical activity to abdominal obesity. Int J Obes (Lond). 2012; 36:100-106. [DOI] [PubMed] [Google Scholar]
- Demerath EW, Rogers NL, Reed D, Lee M, Choh AC, Siervogel RM, Chumlea WC, Towne B, Czerwinski SA. Significant associations of age, menopausal status and lifestyle factors with visceral adiposity in African‐American and European‐American women. Ann Hum Biol. 2011; 38:247-256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hairston KG, Vitolins MZ, Norris JM, Anderson AM, Hanley AJ, Wagenknecht LE. Lifestyle factors and 5‐year abdominal fat accumulation in a minority cohort: the IRAS family study. Obesity. 2012; 20:421-427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molenaar EA, Massaro JM, Jacques PF, Pou KM, Ellison RC, Hoffmann U, Pencina K, Shadwick SD, Vasan RS, O'Donnell CJ, Fox CS. Association of lifestyle factors with abdominal subcutaneous and visceral adiposity: the Framingham Heart Study. Diabetes Care. 2009; 32:505-510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slentz CA, Bateman LA, Willis LH, Shields AT, Tanner CJ, Piner LW, Hawk VH, Muehlbauer MJ, Samsa GP, Nelson RC, Huffman KM, Bales CW, Houmard JA, Kraus WE. Effects of aerobic vs. resistance training on visceral and liver fat stores, liver enzymes, and insulin resistance by HOMA in overweight adults from STRRIDE AT/RT. Am J Physiol Endocrinol Metab. 2011; 301:E1033-E1039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ismail I, Keating SE, Baker MK, Johnson NA. A systematic review and meta‐analysis of the effect of aerobic vs. resistance exercise training on visceral fat. Obes Rev. 2012; 13:68-91. [DOI] [PubMed] [Google Scholar]
- Prince SA, Adamo KB, Hamel ME, Hardt J, Connor Gorber S, Tremblay M. A comparison of direct versus self‐report measures for assessing physical activity in adults: a systematic review. Int J Behav Nutr Phys Act. 2008; 5:56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dyrstad SM, Hansen BH, Holme IM, Anderssen SA. Comparison of self‐reported versus accelerometer‐measured physical activity. Med Sci Sports Exerc. 2014; 46:99-106. [DOI] [PubMed] [Google Scholar]
- Strath SJ, Holleman RG, Ronis DL, Swartz AM, Richardson CR. Objective physical activity accumulation in bouts and nonbouts and relation to markers of obesity in US adults. Prev Chronic Dis. 2008; 5:A131. [PMC free article] [PubMed] [Google Scholar]
- McGuire KA, Ross R. Incidental physical activity and sedentary behavior are not associated with abdominal adipose tissue in inactive adults. Obesity. 2012; 20:576-582. [DOI] [PubMed] [Google Scholar]
- Weyer C, Foley JE, Bogardus C, Tataranni PA, Pratley RE. Enlarged subcutaneous abdominal adipocyte size, but not obesity itself, predicts type II diabetes independent of insulin resistance. Diabetologia. 2000; 43:1498-1506. [DOI] [PubMed] [Google Scholar]
- Gauvreau D, Gupta A, Fisette A, Tom FQ, Cianflone K. Deficiency of c5l2 increases macrophage infiltration and alters adipose tissue function in mice. PLoS One. 2013; 8:e60795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pasarica M, Sereda OR, Redman LM, Albarado DC, Hymel DT, Roan LE, Rood JC, Burk DH, Smith SR. Reduced adipose tissue oxygenation in human obesity: evidence for rarefaction, macrophage chemotaxis, and inflammation without an angiogenic response. Diabetes. 2009; 58:718-725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenquist KJ, Pedley A, Massaro JM, Therkelsen KE, Murabito JM, Hoffmann U, Fox CS. Visceral and subcutaneous fat quality and cardiometabolic risk. JACC Cardiovasc Imaging. 2013; 6:762-771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alvey NJ, Pedley A, Rosenquist KJ, Massaro JM, O'Donnell CJ, Hoffmann U, Fox CS. Association of fat density with subclinical atherosclerosis. J Am Heart Assoc. 2014; 3:e00078810.1161/JAHA.114.000788 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenquist KJ, Massaro JM, Pedley A, Long MT, Kreger BE, Vasan RS, Murabito JM, Hoffmann U, Fox CS. Fat quality and incident cardiovascular disease, all‐cause mortality and cancer mortality. J Clin Endocrinol Metab. 2015; 100:227-234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Splansky GL, Corey D, Yang Q, Atwood LD, Cupples LA, Benjamin EJ, D'Agostino RB, Sr, Fox CS, Larson MG, Murabito JM, O'Donnell CJ, Vasan RS, Wolf PA, Levy D. The third generation cohort of the National Heart, Lung, and Blood Institute's Framingham Heart Study: design, recruitment, and initial examination. Am J Epidemiol. 2007; 165:1328-1335. [DOI] [PubMed] [Google Scholar]
- Glazer NL, Lyass A, Esliger DW, Blease SJ, Freedson PS, Massaro JM, Murabito JM, Vasan RS. Sustained and shorter bouts of physical activity are related to cardiovascular health. Med Sci Sports Exerc. 2013; 45:109-115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crouter SE, Bassett DR., Jr A new 2‐regression model for the actical accelerometer. Br J Sports Med. 2008; 42:217-224. [DOI] [PubMed] [Google Scholar]
- Heil DP. Predicting activity energy expenditure using the actical activity monitor. Res Q Exerc Sport. 2006; 77:64-80. [DOI] [PubMed] [Google Scholar]
- Maurovich‐Horvat P, Massaro J, Fox CS, Moselewski F, O'Donnell CJ, Hoffmann U. Comparison of anthropometric, area‐ and volume‐based assessment of abdominal subcutaneous and visceral adipose tissue volumes using multi‐detector computed tomography. Int J Obes (Lond). 2007; 31:500-506. [DOI] [PubMed] [Google Scholar]
- Fox CS, Massaro JM, Hoffmann U, Pou KM, Maurovich‐Horvat P, Liu CY, Vasan RS, Murabito JM, Meigs JB, Cupples LA, D'Agostino RB, Sr, O'Donnell CJ. Abdominal visceral and subcutaneous adipose tissue compartments: association with metabolic risk factors in the Framingham Heart Study. Circulation. 2007; 116:39-48. [DOI] [PubMed] [Google Scholar]
- Maher CA, Mire E, Harrington DM, Staiano AE, Katzmarzyk PT. The independent and combined associations of physical activity and sedentary behavior with obesity in adults: NHANES 2003‐06. Obesity. 2013; 21:E730-E737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fan JX, Brown BB, Hanson H, Kowaleski‐Jones L, Smith KR, Zick CD. Moderate to vigorous physical activity and weight outcomes: does every minute count? Am J Health Promot. 2013; 28:41-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith HA, Storti KL, Arena V, Kriska AM, Gabriel KK, Sutton‐Tyrrell K, Hames KC, Conroy MB. Associations between accelerometer‐derived physical activity and regional adiposity in young men and women. Obesity. 2013; 21:1299-1305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ayabe M, Kumahara H, Morimura K, Sakane N, Ishii K, Tanaka H. Accumulation of short bouts of non‐exercise daily physical activity is associated with lower visceral fat in Japanese female adults. Int J Sports Med. 2013; 34:62-67. [DOI] [PubMed] [Google Scholar]
- Preis SR, Massaro JM, Robins SJ, Hoffmann U, Vasan RS, Irlbeck T, Meigs JB, Sutherland P, D'Agostino RB, Sr, O'Donnell CJ, Fox CS. Abdominal subcutaneous and visceral adipose tissue and insulin resistance in the Framingham Heart Study. Obesity. 2010; 18:2191-2198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ng SW, Popkin BM. Time use and physical activity: a shift away from movement across the globe. Obes Rev. 2012; 13:659-680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin KR, Koster A, Murphy RA, Van Domelen DR, Hung MY, Brychta RJ, Chen KY, Harris TB. Changes in daily activity patterns with age in U.S. men and women: National Health and Nutrition Examination Survey 2003‐04 and 2005‐06. J Am Geriatr Soc. 2014; 62:1263-1271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arnardottir NY, Koster A, Van Domelen DR, Brychta RJ, Caserotti P, Eiriksdottir G, Sverrisdottir JE, Launer LJ, Gudnason V, Johannsson E, Harris TB, Chen KY, Sveinsson T. Objective measurements of daily physical activity patterns and sedentary behaviour in older adults: age, gene/environment susceptibility‐Reykjavik study. Age Ageing. 2013; 42:222-229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiroma EJ, Freedson PS, Trost SG, Lee IM. Patterns of accelerometer‐assessed sedentary behavior in older women. JAMA. 2013; 310:2562-2563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bankoski A, Harris TB, McClain JJ, Brychta RJ, Caserotti P, Chen KY, Berrigan D, Troiano RP, Koster A. Sedentary activity associated with metabolic syndrome independent of physical activity. Diabetes Care. 2011; 34:497-503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henson J, Yates T, Biddle SJ, Edwardson CL, Khunti K, Wilmot EG, Gray LJ, Gorely T, Nimmo MA, Davies MJ. Associations of objectively measured sedentary behaviour and physical activity with markers of cardiometabolic health. Diabetologia. 2013; 56:1012-1020. [DOI] [PubMed] [Google Scholar]
- Koster A, Caserotti P, Patel KV, Matthews CE, Berrigan D, Van Domelen DR, Brychta RJ, Chen KY, Harris TB. Association of sedentary time with mortality independent of moderate to vigorous physical activity. PLoS One. 2012; 7:e37696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larsen BA, Allison MA, Kang E, Saad S, Laughlin GA, Araneta MR, Barrett‐Connor E, Wassel CL. Associations of physical activity and sedentary behavior with regional fat deposition. Med Sci Sports Exerc. 2014; 21:529-536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saunders TJ, Tremblay MS, Despres JP, Bouchard C, Tremblay A, Chaput JP. Sedentary behaviour, visceral fat accumulation and cardiometabolic risk in adults: a 6‐year longitudinal study from the Quebec Family Study. PLoS One. 2013; 8:e54225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Trends in leisure‐time physical inactivity by age, sex, and race/ethnicity–United States, 1994–2004. MMWR Morb Mortal Wkly Rep. 2005; 54:991-994. [PubMed] [Google Scholar]


