Abstract
There are more than 50 different techniques of laparoscopic cholecystectomy (LC) available in literature mainly due to modifications by surgeons in aim to improve postoperative outcome and cosmesis. These modifications include reduction in port size and/or number than what is used in standard LC. There is no uniform nomenclature to describe these different techniques so that it is not possible to compare the outcomes of different techniques. We brief the advantages and disadvantages of each of these techniques and suggest the situation where particular technique would be useful. We also propose a nomenclature which is easy to remember and apply, so that any future comparison will be possible between the techniques.
Keywords: Laparoscopic cholecystectomy, SILS, SSLS, NOTES, 3 port laparoscopic cholecystectomy, nomenclature
INTRODUCTION
Laparoscopic cholecystectomy (LC) since its inception in 1989 has become the gold standard treatment for gall stone disease. The technique of performing LC has undergone many changes and variations. Several surgeons have tried to reduce the size and number of ports to improve cosmetic and postoperative outcomes and developed their own different versions. The most recent development in technique of LC is single incision laparoscopic surgery (SILS) or single site laparoscopic cholecystectomy (SSLC). In literature there is no uniform technique and nomenclature for this most common procedure; which makes comparison of various techniques difficult. We propose a uniform classification and nomenclature system for LC which is easy to remember and apply. The nomenclature will easily allow the comparison of different techniques in the institution and between the institutions. It will give uniformity to the description of LC. In this article, an attempt is made to describe the possible methods of performing a LC and briefs the advantages and disadvantages of each of these techniques and to identify situation where a particular technique would be used.
Standard Laparoscopic Cholecystectomy
The standard technique of performing LC is to use 4 ports. The pneumoperitoneum is achieved by either closed Veress needle technique or open technique using a blunt trocar or a Hasson's trocar. A 10 mm telescope usually a 30 degree is used at the umbilicus either infra, intra or supraumbilical depending on patient's habitus and surgeon's preference. Another 10 mm trocar is used in the epigastrium which is the main right working port for the surgeon. One 5 mm trocar in the right lumbar region is used for gallbladder fundus traction and another 5 mm trocar in the right hypochondrium is used as left hand working port for the surgeon. With left hand Hartmann's pouch is retracted and with right hand anterior and posterior dissection is done in Calot's triangle and wide window is created. Critical view of safety is of utmost importance to prevent bile duct injury. Clipping of the cystic duct and cystic artery is achieved from 10 mm epigastric port. Gallbladder extraction is generally done from either epigastric or umbilical port. This technique can be named as “10-10-5-5” or “4 ports standard LC”. “10-10-5-5” denotes 10 mm umbilical port for camera, 10 mm epigastric port for right working instrument, 5 mm right hypochondrium port for left working instrument and 5 mm right lumber port for fundal retraction respectively. Sign “denotes that port incisions are at different places, while “/” indicates that port incisions are placed at same place.
In selected patients, with difficult LC like acute cholecystitis, dense adhesion, or inadequate exposure an additional 5 mm port may require in the left hypochondrium for retraction of the duodenum or continuous suction while dissecting in the Calot's triangle. This technique can be termed as “10-10-5-5-5” or “5 port extended LC”.
Modified Laparoscopic Cholecystectomy - Is There a Need?
Recently several surgeons have been using more and more modified techniques to perform LC. The idea is to make the operation more minimally invasive and to inflict lesser postoperative pain and better cosmesis.
The modifications may be either reduced port size, i.e. from 10 mm to 5 mm or from 5 mm to 3 or 2 mm or reduced port numbers. There are various techniques of NOTES (Natural orifices transluminal endoscopic surgery) cholecystectomy like transgastric, transvaginal and transcolonic approaches are under evaluation. These NOTES technique can also be combined with laparoscopic techniques. Studies have shown advantage of these techniques in terms of better cosmesis and less pain12].
It is extremely vital that while performing a modified LC, the standard established principles of LC should not be violated. It is not worth to perform a modified LC with reduced ports with a presumable advantage of better cosmesis, compromising the vision and increasing the risk of bile duct injury for the patient. Thus modified LC should only be performed by experienced surgeons in selected group of patients. The decision to perform a modified LC is generally proceeded after placing the telescope through first trocar and evaluating the area of interest. It is important to understand that during the performance of modified LC if any difficulty is encountered, it is imperative to add an additional trocar timely as required or convert to standard LC rather than risking the patient to injury.
Terminology in Literature
More than 50 technical combinations are possible for performing LC. It is imperative that advantages and disadvantages of each of these techniques are known and a uniform nomenclature is derived to document the technique used in a particular given case. Each LC is different and an appropriate technique would be needed in particular given case. Comparison of different techniques is possible only if a standard nomenclature is accepted and adhered to.
In literature, various terms like minilaparoscopy, microlaparoscopy, miniendoscopic or microendoscopic surgery have been used where smaller ports are used.[3] Gagner and Garcia-Ruiz used the word needloscopic surgery where 2-3 mm diameter instruments were used.[3] Minilaparoscopic cholecystectomy term was used when two instruments of 2 mm size were used in a study.[4] Microlaparoscopic cholecystectomy was referred when use of 5 mm umbilical camera and rest all 3 mm instruments where used in a study by McCormack et al.[5] Santoro et al., described the word miniendoscopic surgery where 5 mm or less diameter instruments were used.[6] So presently there is no uniform nomenclature in the literature. Several combinations of reduced port size and port numbers are possible in LC.
Reduced Port (size) Laparoscopic Cholecystectomy
The commonest modification used today is to reduce the size of epigastric trocar from 10 mm to 5 mm to reduce the pain and improve the cosmesis. This technique can be called “10-5-5-5” and can be performed for most LC today [Figure 1a]. This requires bipolar coagulation of the cystic artery, 5 mm clip applicator for clipping (we prefer the 5 mm haemolock) of the cystic duct or ligation of cystic duct with a free silk suture and an additional double ligation with an endoloop after dividing the cystic duct especially for wide cystic duct needing double ligature. At the end of the procedure the gall bladder is placed in an endobag and then 5 mm telescope is used from the epigastric port to extract the gallbladder from the umbilical port. Another variant of this technique called “5-10-5-5”, in which 5 mm telescope is used at the umbilicus and a 10 mm epigastric trocar is used for standard clip ligature of the cystic duct and epigastric extraction of the gallbladder.
Figure 1.
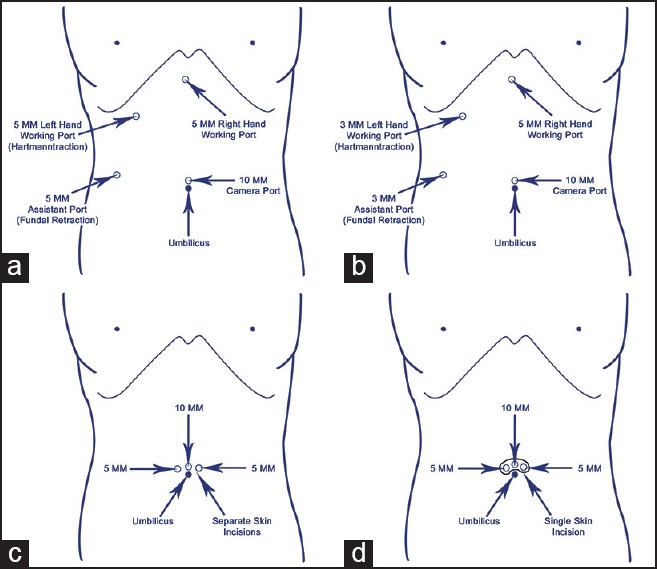
(a) 10-5-5-5 (b) 10-5-3-3 (c) 10/5/5, this can be used with or without suture fundal traction. Note the separate skin incision in single site laparoscopic surgery (d) 10/5/5, this can be used with or without suture fundal traction. Note the same skin incision for all three ports which is marked by underline
This same operation can be further being done using two 3 mm retraction trocars in the right abdomen for many straight forward LC. This technique is called “10-5-3-3” or “5-10-3-3” which needs two 3 mm trocars and two 3 mm graspers [Figure 1b]. This technique is very useful technique for pediatric population as well. For children, 5-5-3-3 technique is sufficient for most patients and gallbladder is extracted by enlarging umbilical port to 7-8 mm, thus avoiding a 10 mm scar.
We propose that it should be named as “minilaparoscopic cholecystectomy” if only one 10 mm port and rest all 5 mm or one 5 mm and other less than 5 mm ports have been used, while it should be named as “microlaparoscopic cholecystectomy” if only one 10 mm and rest all 2-3 mm ports have been used. If one 10 mm port, one 5 mm and rest 2 to 3 mm ports have been used then also it should be called minilaparoscopic cholecystectomy.
Reduced Port (number) Laparoscopic Cholecystectomy
Initial attempts were made by surgeons to reduce the port numbers from 4 to 3 for performing standard LC. However, the vision achieved with 3 ports is quite different than with 4 ports and thus a majority of surgeons till practice standard 4 ports LC, while a few practice 3 port LC and they get away with it in most cases. We feel that there is no major advantage in reducing one 5 mm right lumbar port as it neither reduces pain nor alters the postoperative recovery and it is cosmetically not superior to the traditional standard 4 port LC. There is still a possibility that in a few selected patients with a short gallbladder and a floppy liver, one may achieve a good vision of the Calot's triangle with just one 5 mm retraction of the Hartmann's pouch. There are studies showed advantage of 3 ports LC over 4 ports LC in terms of less pain,[2] shorter hospital stay[2] and fewer surgical scars.[7] Thus in few selected patients; 3 port LC is possible without endangering patient's safety. This operation would be named as “10-10-5” or “3 port modified LC”.
Another technique of performing a 3 port LC is to use a suture for fundal traction (SF), so that without compromising the vision of the calots triangle a 3 port LC can be performed. The traction suture can be inserted from the right lower chest wall taking care it does not penetrate the pleura or the lung in the right anterior or midaxillary line with a straight needle inserted percutaneously or by a free thread inserted into the abdomen and withdrawn by a prolene loop inserted through a standard 18 G needle or an epidural needle [Figure 2]. The only risk factor for this technique is occasional minor bile leak from the fundal suture especially if it cuts across the gallbladder wall. Thus, it is preferable to take a figure of eight suture and apply only gentle adequate traction on the fundus. With these precautions, this technique is an excellent technique to perform a 3 port LC and this technique is labeled as “10-10-5-SF”. Other modification using smaller size trocars can be “10-5-3-SF”.
Figure 2.
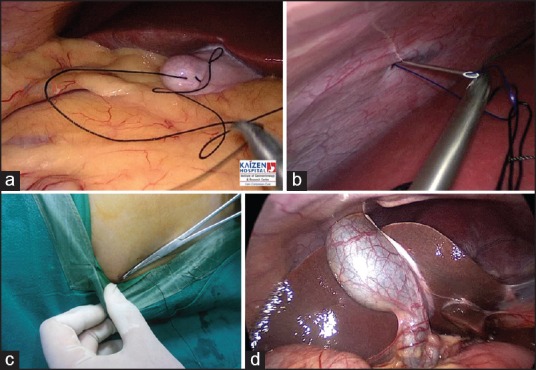
(a) Figure of eight suture over the fundus of gall bladder (b) Suture of fundus going out via a prolene loop made using 18 F spinal needle (c) Suture fundus traction applied at right side of lower chest using a hemostat artery forceps (d) Exposure with suture fundal traction
There can be several techniques of performing a reduced port size along with reduced port numbers in LC.
One can use a 5 mm umbilical telescope and a 10 mm epigastric trocar with a 5 mm retraction trocar in the right abdomen with or without suture traction of gallbladder fundus. This technique is labeled as “5-10-5” or “5-10-5-SF”. With this technique, one can use the standard 10 mm clip applicators for cystic duct and artery clipping and extract the gallbladder from the epigastric port without need of changing the telescope as the entire procedure is done with a 5 mm telescope. To perform this procedure safely, a 3 chip or HD camera, a xenon light source and a flat panel monitor is advisable to achieve a good vision from a 5 mm telescope. This technique of 5-10-5 has little rationale as 10 mm epigastric port presumably causes more pain and avoiding a 10 mm incision in umbilicus has no cosmetic advantage.
One can also use microlaparoscopic instruments, i.e. 3 mm or 2 mm instruments for performing reduced port (number) LC. These techniques can be labeled as “10-5-3” or “10-5-3-SF”. These techniques are eminently possible without a compromise of the vision or dissection. For performing a pure microlaparoscopic cholecystectomy with “10-3-3” or “10-3-3-SF” technique one needs good quality 3 mm instruments especially dissectors, suction as well as 3 mm telescope for extraction of gallbladder from the 10 mm umbilical port. As adequate clip application is not achievable with the currently available 3 mm clip applicator, only intracorporeal ligation of cystic duct is possible with this technique. The alternative is use of 10 mm clip applicator with 3 mm telescope.
Recently two ports LC has become possible by using two traction sutures; one on the fundus of gall bladder (SF) and another on the Hartmann's pouch (SH). With this technique in selected straightforward cases; a two port LC is possible. For anterior as well as posterior dissection of the Calot's triangle, a double suture swinging traction of the Hartmann's can be employed with one suture extracted from the epigastric port and one from the right lumbar port. Thus with traction on the right lumbar suture, anterior dissection of Calot's triangle is possible, while with an epigastric suture traction posterior dissection is possible. Certainly, the quality of traction and countertraction will not be as same as with instrument as the traction are more or less fixed in axis rather than variable and have a fixed direction of traction. Thus, some amount of difficulty and learning curve is expected with this technique. Those different techniques would be “10-10-SF-SH”, “10-5-SF-SH” or “5-10-SF-SH”. These could also be performed with microlaparoscopy instruments or with single port technique at the umbilicus. These techniques can be 10-3-SF-SH or 3-10-SF-SH. It is noteworthy that at least one trocar has to be 10 mm to extract the gallbladder.
Single Site Laparoscopic Cholecystectomy (SSLC) or Trans-umbilical Single Site Surgery (TUSS)
In the last 3 to 4 years, a great amount of interest has been developed in the single incision laparoscopic surgery (SILS) through the umbilicus. SSLC means when all ports are placed at single site; here it is practically in or around umbilicus. SSLC includes single skin and sheath incision or single skin and separate sheath incisions or separate skin and sheath incisions but at the same site. This can be achieved using a single skin and sheath incision; and one of the port devices such as SILS port (Covedien), Tri port or Quad port (Olympus) or X cone (Storz) through the single incision. However, this incision typically requires a larger skin incision (at least 20 mm) then that needs in standard LC. In routine LC, most of the gallbladders can be extracted through a 10 mm trocar incision, however sometimes require extension of the incision from 10 mm to 15 to 20 mm for thick walled gallbladder containing large stones. In single incision LC using one of these ports, at least a 20 mm incision is required for all cases. In the authors view, this is unacceptable as there is evidence that larger the sheath incision at the umbilicus, more are the chances of incisional hernia. Many techniques of single incision or single port LC has been described in the literature, although at present there is no single standard technique of performing SSLC.
More and more surgeons are utilizing standard trocars and standard instruments for performing SSLC. This can be performed from a single skin incision or multiple small skin incision in and around the umbilicus. Some surgeons use special pre-curved instruments introduced either through short plastic trocars or directly without the trocars or through the special ports used for this surgery. Some modifications are needed for instrumentation while performing single site surgery to avoid clashing of instruments and trocars. One should use trocars of differing lengths, only one trocar with gas outlet and use telescope of long length preferable with a straight light cable connection like Endo eye (Olympus) or a T connector (Storz). No more than 3 instruments are advisable at the umbilicus as it is difficult to handle them. In case of difficulty, an additional trocar of 3 mm or 5 mm may be used in the epigastrium if needed for dissection or in the right lumbar region if needed for retraction of the gallbladder. SF or SH can be used in SSLC. Thus several combinations of SSLC would be “10/5/5/5; 10/5/3/3; 5/5/3/3; 10/5/5-SF; 10/5/5-SH; 5/5/5-SF; 5/5/5-SH; 5/5/3-SF; 5/5/3-SH; 5/3/3-SF; 5/3/3-SH; 10/5-SF-SH; 5/5-SF-SH” (note: slash sign “/” is used for SSLC where ports are placed at the same site and underline indicates placement of multiple ports through same incision) [Figure 1c and 1d]. It appears that out of all techniques 5/5/5-SF appears to be good one. It employs a 15 mm skin incision into the umbilicus through which three 5 mm ports are introduced and SF is used for fundal traction. Using a 5 mm telescope and two 5 mm instruments out of which one can be a curved grasper, dissection of calots triangle is performed. In case of difficulty additional 3 mm or 5 mm trocars are placed for retraction or dissection. Different surgeons have different techniques of performing SSLC which is still under evaluation as benefits of these techniques are not proven by randomized trials.
Hybrid Laparoscopic Cholecystectomy
To obviate the disadvantages of single site surgery and to get the advantages of triangular dissection of standard multiport LC, we have developed a hybrid technique of traditional multiport surgery and single site surgery. In this hybrid technique three trocars are placed into the umbilicus whereas; one trocar which is the active dissection trocar is placed into the epigastrium lower down and more on the left side. This trocar is placed under direct vision of the first trocar and then the other two 5 mm trocars are also placed under direct vision with the telescope from this trocar. With this technique “10/5/5-5” or “5/5/5-5”, advantages of both single incision and multiport are gained and the surgery can be expeditiously completed. Though this is strictly not a single site surgery, as one of the trocars is away from the umbilicus, pain is minimal and cosmetic appearance is also good. For appendectomy our technique is to have two trocars into the umbilicus and one 5 mm trocar in the suprapubic hairline. Thus this technique 10/5-5 or 5/5-5 gives an excellent cosmetic result and can be performed with the same ease as a standard multiport surgery without increasing the operating times or compromising the safety of the patient. We have published a Hybrid single site laparoscopic restorative proctocolectomy and ileal pouch with additional trocars at the ileostomy site and the drain site from the beginning to complete the procedure almost as smoothly as a standard multiport surgery.[8] This technique can also be used as bridge to single site surgery while a surgeon is in a learning curve from multiport laparoscopic surgery to single site surgery.
NOTES Cholecystectomy
Earliest NOTES cholecystectomy in humans was reported in 2006 and 2007.[9,10] However; still the technique is in its infancy and is essentially performed under a strict protocol. Various techniques which have been used are transvaginal, transgastric or transcolonic. In either of these techniques, at least one 3 mm or 5 mm port is placed in the umbilicus as an initial guide to puncture the peritoneum and at the end to assist in closure of the defect.
The transvaginal technique uses a long angle telescope 45° or even a flexible endoscope. The umbilical trocar would also assist in retraction or dissection. The final extraction is through the vaginal port which then sutured. The major limitations are in terms of instrumentations, ethical dilemmas in using vagina, the risk of sepsis and dyspareunia in the long term. An injury to rectum during vaginal puncture has been reported and is a cause for concern.
The transgastric and the transcolonic techniques are fraught with instrumentation issues in terms of access device and the closure devices. They use the flexible endoscope to perform the surgery with a double channel endoscope for at least two instruments. However this is not a stable platform and the vision and light travels with the same instrument arm, which is major limitation of this platform. Future innovation, technologies and robotics may obviate these limitations. At present NOTES cholecystectomy is under evaluation and not routinely performed, so we have not included this procedure in our proposed nomenclature.
Summary of the Proposed Nomenclature
There is no uniform nomenclature for different techniques of LC, which leads to lot of confusion and incorrect and incomplete usage of terms to describe the procedure [Table 1]. Thus, we propose a simple nomenclature based on size and number of ports used and whether it is a single incision or multiport. Use of suture fundal or Hartmann's traction is abbreviated by SF or SH. The nomenclature 10-5-5-5 easily describes that 10 mm umbilical port has been used for telescope, a 5 mm epigastric trocar has been used and two 5 mm retraction ports have been used to perform LC. Similarly 10-5-3-SF means a 10 mm telescope, a 5 mm working port, a 3 mm Hartmann's retraction and suture traction for fundus has been used. For single site (“/”) umbilical surgery nomenclature is 10/5/5-SF. If the skin incision is the same this is labeled as 10/5/5-SF. Similarly if skin incision is same for two trocars but separate for the third one it is denoted as 10/5/5-SF.
Table 1.
Summary of the nomenclature system
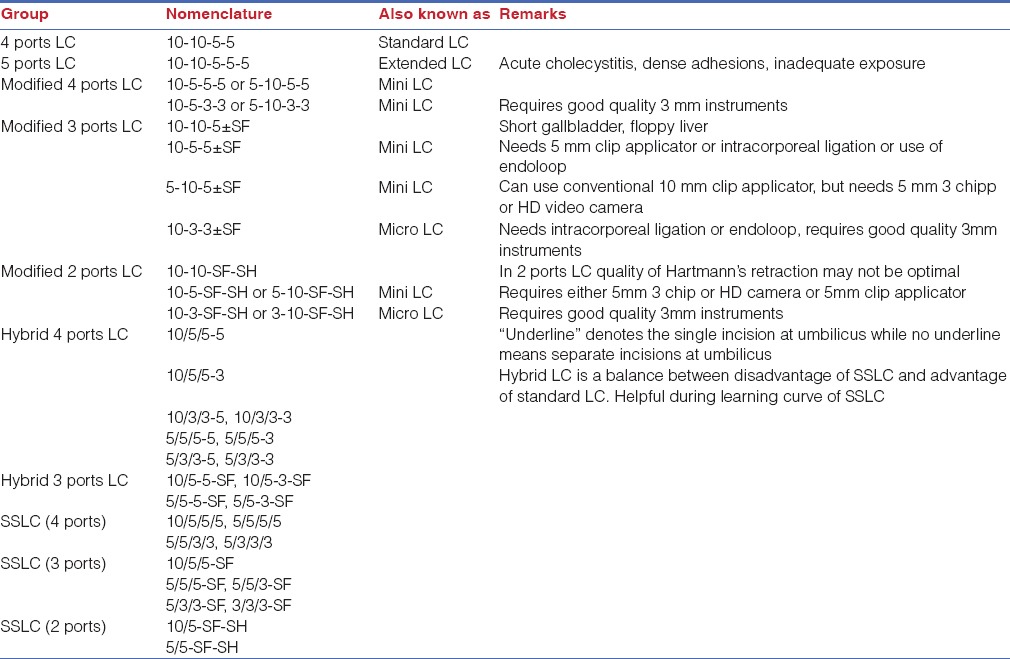
The proposed nomenclature is easy to remember and use and can be recorded on the computer as well in electronic medical records. Later comparison of different techniques within a center or between centers would be possible. All conversions would also be recorded in patient file.
The disadvantage of this classification is that it does not give exact idea about the site of port, for example right hand working port may be used in epigastrium in midline or more on left side of the midline. In same way assistant's port may be used anywhere in left lumber region. But we feel that this is not much relevant in term of purpose of this classification. Another shortcoming of this nomenclature is in case of incidental cholecystectomy where the cholecystectomy may be done using the ports of main surgery.
Application of the Nomenclature to Other Laparoscopic Procedure
The similar nomenclature can be applied to other standard laparoscopic procedures. We are planning to standardize the similar nomenclature for other laparocopic procedures in our future publications.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Pan MX, Jiang ZS, Cheng Y, Xu XP, Zhang Z, Qin JS, et al. Single-incision vs three-port laparoscopic cholecystectomy: Prospective randomized study. World J Gastroenterol. 2013;19:394–8. doi: 10.3748/wjg.v19.i3.394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Azawi DA, Houssein N, Rayis AB, McMahon D, Hehir DJ. Three-port versus four-port laparoscopic cholecystectomy in acute and chronic cholecystitis. BMC Surg. 2007;7:1–6. doi: 10.1186/1471-2482-7-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Piskun G, Rajpal S. Transumbilical laparoscopic cholecystectomy utilizes no incisions outside the umbilicus. J Laparoendosc Adv Surg Tech A. 1999;9:361–4. doi: 10.1089/lap.1999.9.361. [DOI] [PubMed] [Google Scholar]
- 4.Novitsky YW, Kercher KW, Czerniach DR, Kaban GK, Khera S, Gallagher-Dorval KA, et al. Advantages of mini-laparoscopic vs conventional laparoscopic cholecystectomy: Results of a prospective randomized trial. Arch Surg. 2005;140:1178–83. doi: 10.1001/archsurg.140.12.1178. [DOI] [PubMed] [Google Scholar]
- 5.McCormack D, Saldinger P, Cocieru A, House S, Zuccala K. Micro-laparoscopic cholecystectomy: An alternative to single-port surgery. J Gastrointest Surg. 2011;15:758–61. doi: 10.1007/s11605-011-1438-5. [DOI] [PubMed] [Google Scholar]
- 6.Santoro E, Agresta F, Veltri S, Mulieri G, Bedin N, Mulieri M. Minilaparoscopic colorectal resection: A preliminary experience and an outcomes comparison with classical laparoscopic colon procedures. Surg Endosc. 2008;22:1248–54. doi: 10.1007/s00464-007-9601-5. [DOI] [PubMed] [Google Scholar]
- 7.Kumar M, Agrawal CS, Gupta RK. Three-Port versus standard four-port laparoscopic cholecystectomy: A randomized controlled clinical trial in a community-based teaching hospital in eastern Nepal. JSLS. 2007;11:358–62. [PMC free article] [PubMed] [Google Scholar]
- 8.Nagpal AP, Soni H, Haribhakti S. Hybrid single-incision laparoscopic restorative proctocolectomy with ileal pouch anal anastomosis for ulcerative colitis. Indian J Surg. 2010;72:400–3. doi: 10.1007/s12262-010-0125-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zorron R, Filgueiras M, Maggioni LC, Pombo L, Lopes GC, Lacerda AO. NOTES transvaginal cholecystectomy: report of the first case. Surg Innov. 2007;14:279–83. doi: 10.1177/1553350607311090. [DOI] [PubMed] [Google Scholar]
- 10.Marescaux J, Dallemagne B, Perretta S, Wattiez A, Mutter D, Coumaros D. Surgery without scars: Report of transluminal cholecystectomy in a human being. Arch Surg. 2007;142:823–6. doi: 10.1001/archsurg.142.9.823. [DOI] [PubMed] [Google Scholar]


