Abstract
Introduction Obstructive sleep apnea syndrome affects up to 4% of middle-aged men and 2% of adult women. It is associated with obesity.
Objective The objective of this article is to review the literature to determine which factors best correlate with treatment success in patients with obstructive sleep apnea syndrome treated with a mandibular repositioning appliance.
Data Synthesis A search was performed of the PubMed, Cochrane, Lilacs, Scielo, and Web of Science databases of articles published from January 1988 to January 2012. Two review authors independently collected data and assessed trial quality. Sixty-nine articles were selected from PubMed and 1 from Cochrane library. Of these, 42 were excluded based on the title and abstract, and 27 were retrieved for complete reading. A total of 13 articles and 1 systematic review were considered eligible for further review and inclusion in this study: 6 studies evaluated anthropomorphic and physiologic factors, 3 articles addressed cephalometric and anatomic factors, and 4 studies evaluated variables related to mandibular repositioning appliance design and activation. All the studies evaluated had low to moderate methodologic quality and were not able to support evidence on prediction of treatment success.
Conclusion Based on this systematic review on obstructive sleep apnea syndrome treatment, it remains unclear which predictive factors can be used with confidence to select patients suitable for treatment with a mandibular repositioning appliance.
Keywords: systematic review, sleep apnea syndrome, obstructive sleep apnea syndrome
Introduction
According to the American Academy of Sleep Medicine Task Force, obstructive sleep apnea is the complete interruption of airflow to the airway for at least 10 seconds. If the anatomical obstacle or the functional change leads to complete prevention of the inspiratory flow, the patient experiences oxygen desaturation and microarousals, which is defined as hypopnea.1 2
Obstructive sleep apnea syndrome (OSAS) affects up to 4% of middle-aged men and 2% of adult women. Its prevalence increases with age until approximately the seventh and eighth decades of life; it is more frequent in men and postmenopausal women. The prevalence of OSAS, defined by Apnea-Hypopnea Index (AHI) frequency and the presence of hypersomnolence, has been estimated to range from 1.2 to 7.5%.3 It is strongly associated with obesity, and there is also evidence of a hereditary component of OSAS.4 5 6 7
OSAS has become a concern in clinical practice because of its prevalence and because it is a potential risk factor for neurologic diseases such as cerebrovascular accidents, cardiovascular hypertension, acute myocardial infarction, and congestive heart failure, in addition to obesity and metabolic syndrome. However, it remains underdiagnosed.1 2 8 9 10
There are many treatment options for OSAS, including positive airway pressure therapy, oral appliances, and surgery. Oral appliances may be used in patients with mild to moderate OSAS and in those with more severe disease who are unable to tolerate continuous positive airway pressure therapy.11 Thus, the objective of this article is to review the literature to determine which factors best correlate with treatment success in patients with OSAS treated with a mandibular repositioning appliance (MRA).
Review of Literature
MRAs, originally derived from functional dental appliances, are used during sleep to advance the mandible and thus prevent the collapse of oropharynx tissues and tongue base, thereby reducing events of upper airway obstruction. Because they are simple and portable, do not use electricity, and are relatively low cost, they are considered an alternative to the treatment of OSAS. MRAs present favorable results quickly.1 2 3 4 5 6 7 8 9 10 11 12 13
The clinical diagnosis of OSAS is confirmed by polysomnography (PSG), which assesses the parameters of quality, architecture, and sleep continuity; nasal/oral airflow; qualitative and quantitative measure of respiratory effort; oxyhemoglobin saturation; electrocardiogram; and position of the body during sleep.1 12 14
The PSG quantifies respiratory events per hour of sleep, and AHI confirms the diagnosis. This index is the number of times the air passage is blocked (apnea) or reduced (hypopnea) over 10 seconds each hour of sleep. An AHI of 5 to 15 events per hour is defined as mild apnea; 16 to 30, moderate apnea; and severe apnea, more than 30.5 12
According to anthropometric and physiologic predictors, OSAS is a common disease in the middle-aged population, in general affecting both males and females.2 Postmenopausal women may have OSAS as frequently as men. Obesity is a known risk factor directly related to OSAS.13 Obese individuals with OSAS have a higher fat volume and increase in cervical soft tissue structures on the airway, causing a reduction in size and alterations in the function of the respiratory muscles, promoting airflow obstruction.8 9 10
The respiratory problems associated with OSAS result from different anatomical and pathophysiological changes, which make it difficult to establish a single treatment that covers all cases. One conventional treatment is the MRA, which generally requires 4 weeks of adaptation to the device followed by 2 to 3 months of stepwise mandibular advancement (titration of the device) to maximize the acceptance of the appliance. A mandibular advancement of 50 to 75% of the maximum voluntary protrusion of the individual has been associated with favorable treatment results.11 12 13 The main difficulty is to achieve an adequate mandibular advancement without causing discomfort to the patient during the first night of use.
Inclusion Criteria for Studies
Type of Study
We reviewed published randomized controlled trials with experimental and control group addressing the research question: which factors best correlate with treatment success in patients with obstructive sleep apnea syndrome treated with a mandibular repositioning appliance.
Type of Participants
Studies with participants of both genders, over 16 years of age, with a diagnosis of OSAS, and with more than five apneas/hypopneas per hour of sleep were included.
Type of Intervention
The treatment group included studies that reported treatment with any MRA for OSAS; the control group included studies that reported OSAS treatments using another intervention (surgical or nonsurgical) or no intervention.
Search Methods
Two reviewers independently performed an electronic search databases of PubMed, Web of Science, Cochrane Library, Lilacs, and Scielo. The terms used in the literature review were: [(sleep apnea OR sleep apnoea OR obstructive sleep apnea OR obstructive sleep apnoea OR sleep apnea syndrome OR sleep apnoea syndrome OR apneic OR apnoea OR respiratory disturbance OR sleep disorder breathing OR upper airway resistance syndrome) AND (mandibular repositioning appliance OR mandibular advancement device OR oral appliance OR mandibular device OR anterior mandibular positioner OR mandibular splint OR oral appliance therapy OR intraoral sleep apnea devices OR oral jaw-positioning appliance OR intraoral positioning appliance OR occlusal splint OR anteriorly titratable mandibular positioner OR adjustable oral appliance OR mandibular advancement splint OR mandibular protruding device OR mandibular advancing appliance OR oral jaw positioning appliance OR titratable oral appliance OR oral vestibular shield OR intraoral protrusive appliance)] AND (Randomized Clinical Trial AND English)]. The electronic search was from January 1988 to January 2012, with language restriction (English only). Two review authors conducted the electronic search independently.
Data Extraction
Primary outcomes include AHI. Secondary outcomes included other parameters of PSG, such as quality, architecture, and sleep continuity; nasal/oral airflow; quality and quantity measurement of respiratory effort; saturation of oxyhemoglobin; oxygen desaturation; body position; quality of life; and cognitive function.
Data Analysis
The selection of the studies took place in three phases. First, articles were selected from PubMed, followed by articles from other electronic databases using the search terms mentioned previously. From these and based on the information provided in the title and the abstract, examiners selected the articles to read the entire text. Then, articles in which predictive factors of MRA treatment were possibly discussed were selected.
The grading of evidence from selected studies was also performed by the same two independent reviewers according to slight modification of the criteria and classified according to sample size calculation, randomization, clear definition of the inclusion and/or exclusion criteria, follow-up completion (and reasons for withdrawal in each study group were specified), experimental and control group comparable at baseline, presence of blinding, appropriate statistical analysis, and calibration of examiners.15 16 The total score was calculated for each study and the results regarding quality were evaluated and considered, as follows: <7 points, high risk of bias (not reviewed); 7 to 10 points, moderate risk of bias; and >10 points, low risk of bias. Moreover, the strengths and weakness of all the included studies were assessed according to Cochrane Reviewers' Handbook.5
Discussion
Description of Studies
Initially, 69 articles were selected from PubMed and 2 from Cochrane Library. Of these, 30 were excluded based on the title and 12 were excluded based on the abstract, with 29 retrieved for complete reading. Then, 7 articles were excluded because of the methodological quality of the studies and 6 because the study did not address the research question. A total of 13 articles and 1 systematic review were considered eligible for further review and inclusion in this study. The article selection process is charted in Fig. 1.
Fig. 1.
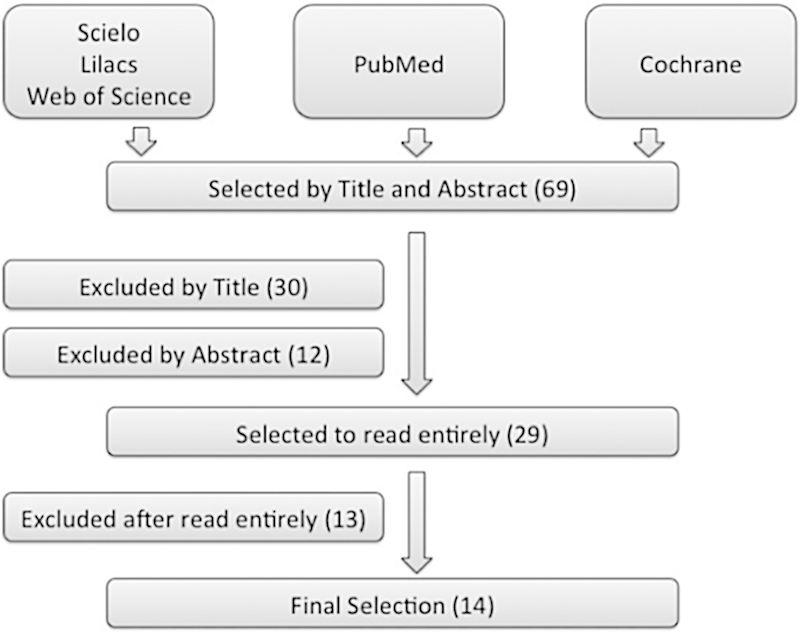
Flowchart.
There was no disagreement about study inclusion between reviewers. The most important limitation of this study is the heterogeneity of the articles, due to differences in disease severity and how the authors defined treatment success. Table 1 lists the studies reviewed by the authors in relation anthropometric and physiologic factors.16 17 18 19 20 21
Table 1. Studies in relation to anthropometric and physiologic factors.
| Author | Defined treatment success |
|---|---|
| Barnes et al17 | Mild to moderate disease severity. In patients with mild to moderate OSAS, authors found that CPAP and MRA effectively treated sleep-disorder breathing and sleepiness; however, the expected response in neurobehavioral function was incomplete. This may be due to MRA having a lesser therapeutic effect and CPAP being poorly tolerated (used less in this patient group). |
| Engelman et al18 | Mixed disease severity. Objective sleepiness, cognitive performance, and preference for treatment were not different. In patients treated with CPAP versus MRA experiencing a mild form of the syndrome (AHI < 15, n = 18), symptoms, treatment efficacy satisfaction, and subjective sleepiness were better with CPAP than MRA. These results do not support the MRA as first-line treatment for patients with OSAS. |
| Hoekema et al19 | Mixed disease severity. MRA therapy was less effective in individuals with severe disease (AHI > 30). Because these patients could be at particular risk for cardiovascular disease, primary MRA therapy appears to be supported only for those with nonsevere apnea. |
| Metha et al20 | Mixed disease severity. MRA used in this study was well tolerated, at least in the short term, and was associated with substantial subjective and objective improvements in a significant proportion of patients. These results support the use of MRA even in some of the patients with more severe forms of OSAS. |
| Tan et al21 | Mild to moderate disease severity. (1) MRA may be a suitable alternative to nasal CPAP in patients with mild to moderate OSAS; (2) larger studies on the long-term efficacy of the MRA will be required before MRA can be offered as definitive alternative to nasal CPAP; (3) MRAs were well tolerated and preferred by the majority of patients. |
| Wilhemson et al22 | Mild to moderate disease severity. Findings suggest that the MRA is useful in the treatment of mild to moderate OSAS. |
Abbreviations: AHI, apnea-hypopnea index; CPAP, continuous positive airway pressure therapy; MRA, mandibular repositioning appliance; OSAS, obstructive sleep apnea syndrome.
No randomized controlled trials addressing cephalometric and anatomical factors were found to be included in this review. Factors related to MRA (titratable, vertical dimension, and amount of advance), anthropometric and physiologic factors and MRA (titratable, vertical dimension and amount of advance), and the study founded in Cochrane Systematic Review are shown in Table 2.5 23 24 25 26 27 28 29
Table 2. Factors related to MRA, anthropometric and physiologic factors, and the study found in Cochrane Systematic Review.
| Factors related to MRA only | Anthropometric and physiologic factors and MRA | Cochrane Systematic Review | |||
|---|---|---|---|---|---|
| Author | Description | Author | Description | Author | Description |
| Araab et al23 | In patients with mild to moderate condition titratable during PSG, the authors found no differences in excessive daytime sleepiness improvements (MRA x nCPAP). This would indicate that the larger improvements in AHI in the nCPAP group are not clinically relevant. nCPAP patients may show more problems in accepting nCPAP than MRA patients. | Gagnodoaux et al26 | Titrated MRA is an effective therapy in moderately sleepy and overweight patients with OSAS. Although less effective than CPAP, successfully titrated MRA was very effective at reducing the AHI and was associated with a higher reported compliance. Both treatments improved functional outcomes to a similar degree. One night of titration of MRA had a low negative predictive value for treatment success. | Lim et al5 | The review found 16 studies that met the inclusion criteria, comparing treatment with oral appliances. The authors suggest that future research should recruit patient with more severe symptoms, to establish whether the response to therapy differs between subgroups. |
| Araab et al24 | No clinically relevant difference was found between MRA and nCPAP in the treatment of mild/moderate OSA when both treatment modalities are titrated objectively; | Petri et al27 | MRA had significantly beneficial effects on OSA, including cure in some cases of severe OSA. Protrusion of the mandible is essential for the effect. MRA had no placebo effect and may be a good alternative to CPAP. | ||
| Pitsis et al25 | The amount of bite opening induced by MRA does not have a significant impact on treatment efficacy but does have an impact on patient acceptance. | Tegelberg et al28 | MRA recommended for patients of mild to moderate OSAS but recommended to not start the treatment by more than 50% of mandibular advancement. | ||
| Walker-Engstron et al29 | MRA could be an alternative treatment for some patients with severe OSAS. | ||||
Abbreviations: AHI, apnea-hypopnea index; CPAP, continuous positive airway pressure therapy; MRA, mandibular repositioning appliance; nCPAP, nasal continuous positive airway pressure therapy; OSAS, obstructive sleep apnea syndrome; PSG, polysomnography.
Summary of Evidence
MRAs are widely prescribed for the treatment of OSAS both as primary therapy and as an alternative for patients who are unable to tolerate continuous positive airway pressure therapy. Although significant progress has been made in demonstrating the efficacy of MRA for OSAS, numerous methodologic weaknesses in published studies bring uncertainty about the role of this therapy in the routine management of OSAS. Until the mid to late 1990s, the majority of studies on the use of MRA in OSAS were short term, not controlled, small, and retrospective. More recently, the quality of MRA clinical research has become more rigorous.20
This review identified 13 randomized controlled trials with low or moderate methodologic quality involving participants with varied degrees of OSAS severity and 1 systematic review. However, the evidence to support the ability to predict treatment outcome and hence to preselect suitable candidates for this treatment option still remains in its early stages of development.
Predictors of Response to the MRA
The reviewed studies identified a range of anthropomorphic, physiologic, and PSG variables associated with better treatment outcome. Practice parameters developed by the American Academy of Sleep Medicine recommend the use of MRAs only for those patients with mild OSAS or those who refuse or cannot tolerate continuous positive airway pressure therapy. Several studies support this conclusion. However, there is growing evidence supporting an expansion of use of MRAs in more severe forms of OSA, provided that patients are followed cautiously and objective verification of outcome is monitored. The pretreatment AHI, which reflects disease severity, has been suggested as a possible indicator of treatment effect in OSAS patients, with generally higher index levels suggesting treatment failure.20 30 31 32 33 The positive effect of the dental appliance was also independent of whether the predominant obstruction was in the oropharynx, the hypopharynx, or both.
Some evidence indicates that moderate to severe OSAS is closely associated with obesity and indicates that the dental appliance is an effective treatment in obese patients.29 34
Further work is required to determine the most effective design and vertical dimension opening of MRAs as a predictor of treatment success. The majority of the studies have compared devices of different design.20 25 35 36
The differences in results may be due to differences in the study design, in the way the MRA was titrated, in the baseline characteristics of the studies participants (e.g., the severity of OSA), in the primary outcome variable chosen, or in the specifics of the appliances and devices used. At least in part this uncertainty is related to how treatment success is defined and what factors can be clinically used as predictors of success.37 38 39 40 41
The results of this review justify well-designed, large-scale, randomized controlled trials to assess the effectiveness of MRA treatment.
Conclusion
This review of the published literature suggests that it is unclear which factors can be used with confidence to select patients suitable for OSAS treatment with MRAs. We are only able to make some assertions:
Implications of this review for clinical practice: In the absence of clear predictors of MRA success, it would seem critical to monitor all subjects who have had an MRA fitted with a further overnight sleep study to make sure that the appliance provides satisfactory control of the disease.
Implication of this review for research: Although significant progress has been reported in proving the efficacy of MRA for OSAS, the ability to predict treatment outcome and hence to preselect suitable candidates for this treatment still remains in its early stages. The review of these clinical trials suggests that there is need to conduct more randomized control trials comparing MRA with not only other treatments as controls but also placebo controls. Numerous methodologic weaknesses in published studies bring uncertainty about the role of this therapy in the routine management of OSAS.
References
- 1.Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. The Report of an American Academy of Sleep Medicine Task Force. Sleep. 1999;22(5):667–689. [PubMed] [Google Scholar]
- 2.Berry R B, Budhiraja R, Gottlieb D J. et al. Rules for scoring respiratory events in sleep: update of the 2007 AASM Manual for the Scoring of Sleep and Associated Events. J Clin Sleep Med. 2012;8(5):597–619. doi: 10.5664/jcsm.2172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tufik S, Santos-Silva R, Taddei J A, Bittencourt L RA. Obstructive sleep apnea syndrome in the Sao Paulo Epidemiologic Sleep Study. Sleep Med. 2010;11(5):441–446. doi: 10.1016/j.sleep.2009.10.005. [DOI] [PubMed] [Google Scholar]
- 4.Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S. The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med. 1993;328(17):1230–1235. doi: 10.1056/NEJM199304293281704. [DOI] [PubMed] [Google Scholar]
- 5.Lim J, Lasserson T J, Fleetham J, Wright J. Oral appliances for obstructive sleep apnoea. Cochrane Database Syst Rev. 2006;(1):CD004435. doi: 10.1002/14651858.CD004435.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sateia M J. Neuropsychological impairment and quality of life in obstructive sleep apnea. Clin Chest Med. 2003;24(2):249–259. doi: 10.1016/s0272-5231(03)00014-5. [DOI] [PubMed] [Google Scholar]
- 7.Alchanatis M, Zias N, Deligiorgis N, Amfilochiou A, Dionellis G, Orphanidou D. Sleep apnea-related cognitive deficits and intelligence: an implication of cognitive reserve theory. J Sleep Res. 2005;14(1):69–75. doi: 10.1111/j.1365-2869.2004.00436.x. [DOI] [PubMed] [Google Scholar]
- 8.Shahar E, Whitney C W, Redline S. et al. Sleep-disordered breathing and cardiovascular disease: cross-sectional results of the Sleep Heart Health Study. Am J Respir Crit Care Med. 2001;163(1):19–25. doi: 10.1164/ajrccm.163.1.2001008. [DOI] [PubMed] [Google Scholar]
- 9.Marin J M, Carrizo S J, Vicente E, Agusti A GN. Long-term cardiovascular outcomes in men with obstructive sleep apnoea-hypopnoea with or without treatment with continuous positive airway pressure: an observational study. Lancet. 2005;365(9464):1046–1053. doi: 10.1016/S0140-6736(05)71141-7. [DOI] [PubMed] [Google Scholar]
- 10.Marshall N S, Wong K K, Liu P Y, Cullen S R, Knuiman M W, Grunstein R R. Sleep apnea as an independent risk factor for all-cause mortality: the Busselton Health Study. Sleep. 2008;31(8):1079–1085. [PMC free article] [PubMed] [Google Scholar]
- 11.Freedman N. Treatment of obstructive sleep apnea syndrome. Clin Chest Med. 2010;31(2):187–201. doi: 10.1016/j.ccm.2010.02.012. [DOI] [PubMed] [Google Scholar]
- 12.American Academy of Sleep Medicine . Westchester, IL, USA: American Academy of Sleep Medicine; 2005. International Classification of Sleep Disorders: Diagnostic and Coding Manual (ICSD-2). 2nd ed. [Google Scholar]
- 13.Chaves Junior C M, Dal-Fabbro C, de Bruin V MS, Tufik S, Bittencourt L RA. Brazilian consensus of snoring and sleep apnea—aspects of interest for orthodontists. Dental Press J Orthod. 2011;16:e1–e10. [Google Scholar]
- 14.Lacasse Y, Bureau M P, Sériès F. A new standardised and self-administered quality of life questionnaire specific to obstructive sleep apnoea. Thorax. 2004;59(6):494–499. doi: 10.1136/thx.2003.011205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Esposito M, Worthington H V, Coulthard P. In search of truth: the role of systematic reviews and meta-analyses for assessing the effectiveness of rehabilitation with oral implants. Clin Implant Dent Relat Res. 2001;3(2):62–78. doi: 10.1111/j.1708-8208.2001.tb00234.x. [DOI] [PubMed] [Google Scholar]
- 16.Roccuzzo M Bunino M Needleman I Sanz M Periodontal plastic surgery for treatment of localized gingival recessions: a systematic review J Clin Periodontol 20022903178–194., discussion 195–196 [DOI] [PubMed] [Google Scholar]
- 17.Barnes M, McEvoy R D, Banks S. et al. Efficacy of positive airway pressure and oral appliance in mild to moderate obstructive sleep apnea. Am J Respir Crit Care Med. 2004;170(6):656–664. doi: 10.1164/rccm.200311-1571OC. [DOI] [PubMed] [Google Scholar]
- 18.Engleman H M, McDonald J P, Graham D. et al. Randomized crossover trial of two treatments for sleep apnea/hypopnea syndrome: continuous positive airway pressure and mandibular repositioning splint. Am J Respir Crit Care Med. 2002;166(6):855–859. doi: 10.1164/rccm.2109023. [DOI] [PubMed] [Google Scholar]
- 19.Hoekema A, Stegenga B, Wijkstra P J, van der Hoeven J H, Meinesz A F, de Bont L GM. Obstructive sleep apnea therapy. J Dent Res. 2008;87(9):882–887. doi: 10.1177/154405910808700917. [DOI] [PubMed] [Google Scholar]
- 20.Mehta A, Qian J, Petocz P, Darendeliler M A, Cistulli P A. A randomized, controlled study of a mandibular advancement splint for obstructive sleep apnea. Am J Respir Crit Care Med. 2001;163(6):1457–1461. doi: 10.1164/ajrccm.163.6.2004213. [DOI] [PubMed] [Google Scholar]
- 21.Tan Y K, L'Estrange P R, Luo Y-M. et al. Mandibular advancement splints and continuous positive airway pressure in patients with obstructive sleep apnoea: a randomized cross-over trial. Eur J Orthod. 2002;24(3):239–249. doi: 10.1093/ejo/24.3.239. [DOI] [PubMed] [Google Scholar]
- 22.Wilhelmsson B, Tegelberg A, Walker-Engström M L. et al. A prospective randomized study of a dental appliance compared with uvulopalatopharyngoplasty in the treatment of obstructive sleep apnoea. Acta Otolaryngol. 1999;119(4):503–509. doi: 10.1080/00016489950181071. [DOI] [PubMed] [Google Scholar]
- 23.Aarab G, Lobbezoo F, Hamburger H L, Naeije M. Oral appliance therapy versus nasal continuous positive airway pressure in obstructive sleep apnea: a randomized, placebo-controlled trial. Respiration. 2011;81(5):411–419. doi: 10.1159/000319595. [DOI] [PubMed] [Google Scholar]
- 24.Aarab G, Lobbezoo F, Heymans M W, Hamburger H L, Naeije M. Long-term follow-up of a randomized controlled trial of oral appliance therapy in obstructive sleep apnea. Respiration. 2011;82(2):162–168. doi: 10.1159/000324580. [DOI] [PubMed] [Google Scholar]
- 25.Pitsis A J, Darendeliler M A, Gotsopoulos H, Petocz P, Cistulli P A. Effect of vertical dimension on efficacy of oral appliance therapy in obstructive sleep apnea. Am J Respir Crit Care Med. 2002;166(6):860–864. doi: 10.1164/rccm.200204-342OC. [DOI] [PubMed] [Google Scholar]
- 26.Gagnadoux F, Fleury B, Vielle B. et al. Titrated mandibular advancement versus positive airway pressure for sleep apnoea. Eur Respir J. 2009;34(4):914–920. doi: 10.1183/09031936.00148208. [DOI] [PubMed] [Google Scholar]
- 27.Petri N, Svanholt P, Solow B, Wildschiødtz G, Winkel P. Mandibular advancement appliance for obstructive sleep apnoea: results of a randomised placebo controlled trial using parallel group design. J Sleep Res. 2008;17(2):221–229. doi: 10.1111/j.1365-2869.2008.00645.x. [DOI] [PubMed] [Google Scholar]
- 28.Tegelberg A, Walker-Engström M L, Vestling O, Wilhelmsson B. Two different degrees of mandibular advancement with a dental appliance in treatment of patients with mild to moderate obstructive sleep apnea. Acta Odontol Scand. 2003;61(6):356–362. doi: 10.1080/00016350310007130. [DOI] [PubMed] [Google Scholar]
- 29.Walker-Engström M L, Ringqvist I, Vestling O, Wilhelmsson B, Tegelberg A. A prospective randomized study comparing two different degrees of mandibular advancement with a dental appliance in treatment of severe obstructive sleep apnea. Sleep Breath. 2003;7(3):119–130. doi: 10.1007/s11325-003-0119-3. [DOI] [PubMed] [Google Scholar]
- 30.Schmidt-Nowara W, Lowe A, Wiegand L, Cartwright R, Perez-Guerra F, Menn S. Oral appliances for the treatment of snoring and obstructive sleep apnea: a review. Sleep. 1995;18(6):501–510. doi: 10.1093/sleep/18.6.501. [DOI] [PubMed] [Google Scholar]
- 31.O'Sullivan R A, Hillman D R, Mateljan R, Pantin C, Finucane K E. Mandibular advancement splint: an appliance to treat snoring and obstructive sleep apnea. Am J Respir Crit Care Med. 1995;151(1):194–198. doi: 10.1164/ajrccm.151.1.7812552. [DOI] [PubMed] [Google Scholar]
- 32.Lowe A Fleetham J Ryan F Mathews B Effects of a mandibular repositioning appliance used in the treatment of obstructive sleep apnea on tongue muscle activity Prog Clin Biol Res 1990345395–404., discussion 405 [PubMed] [Google Scholar]
- 33.Eveloff S E, Rosenberg C L, Carlisle C C, Millman R P. Efficacy of a Herbst mandibular advancement device in obstructive sleep apnea. Am J Respir Crit Care Med. 1994;149(4 Pt 1):905–909. doi: 10.1164/ajrccm.149.4.8143054. [DOI] [PubMed] [Google Scholar]
- 34.Millman R P, Rosenberg C L, Carlisle C C, Kramer N R, Kahn D M, Bonitati A E. The efficacy of oral appliances in the treatment of persistent sleep apnea after uvulopalatopharyngoplasty. Chest. 1998;113(4):992–996. doi: 10.1378/chest.113.4.992. [DOI] [PubMed] [Google Scholar]
- 35.Bloch K E, Iseli A, Zhang J N. et al. A randomized, controlled crossover trial of two oral appliances for sleep apnea treatment. Am J Respir Crit Care Med. 2000;162(1):246–251. doi: 10.1164/ajrccm.162.1.9908112. [DOI] [PubMed] [Google Scholar]
- 36.Rose E C, Staats R, Lehner M, Jonas I E. Cephalometric analysis in patients with obstructive sleep apnea. Part I: diagnostic value. J Orofac Orthop. 2002;63(2):143–153. doi: 10.1007/s00056-002-0057-x. [DOI] [PubMed] [Google Scholar]
- 37.Ferguson K A, Cartwright R, Rogers R, Schmidt-Nowara W. Oral appliances for snoring and obstructive sleep apnea: a review. Sleep. 2006;29(2):244–262. doi: 10.1093/sleep/29.2.244. [DOI] [PubMed] [Google Scholar]
- 38.Liu Y, Lowe A A, Fleetham J A, Park Y-C. Cephalometric and physiologic predictors of the efficacy of an adjustable oral appliance for treating obstructive sleep apnea. Am J Orthod Dentofacial Orthop. 2001;120(6):639–647. doi: 10.1067/mod.2001.118782. [DOI] [PubMed] [Google Scholar]
- 39.Marklund M, Stenlund H, Franklin K A. Mandibular advancement devices in 630 men and women with obstructive sleep apnea and snoring: tolerability and predictors of treatment success. Chest. 2004;125(4):1270–1278. doi: 10.1378/chest.125.4.1270. [DOI] [PubMed] [Google Scholar]
- 40.Randerath W J, Heise M, Hinz R, Ruehle K H. An individually adjustable oral appliance vs continuous positive airway pressure in mild-to-moderate obstructive sleep apnea syndrome. Chest. 2002;122(2):569–575. doi: 10.1378/chest.122.2.569. [DOI] [PubMed] [Google Scholar]
- 41.Ahrens A, McGrath C, Hägg U. Subjective efficacy of oral appliance design features in the management of obstructive sleep apnea: a systematic review. Am J Orthod Dentofacial Orthop. 2010;138(5):559–576. doi: 10.1016/j.ajodo.2010.01.030. [DOI] [PubMed] [Google Scholar]


