Abstract
Background:
According to investigations, pregnant women hypothesized that anxiety is a common factor that will improve spontaneously; they are not aware of its side effects on the fetus, baby, and pregnancy outcome, as a whole. Other studies have also not tried to design a theoretical framework based on Health Education Models (HBMs) to overcome this problem. The current study aimed at exploring the effectiveness of education on the anxiety of nulliparous women based on a HBM.
Materials and Methods:
An experimental study on 88 eligible nulliparous women (n = 44 per group), from Doroud city, was performed in 2012. The data was collected using a researcher made questionnaire. Education was conducted in three sessions tailored with HBM constructs with the help of lectures, group discussions, inquiries, Power Point presentations, and booklets. Evaluation performed using a posttest four and eight weeks after last session. The collected data were analyzed using statistical tests, including Chi-square, independent t-test, and repeated measure Analysis of Variance (ANOVA) by the significance level of 0.05.
Results:
The mean score of knowledge, perceived sensitivity, perceived severity, perceived benefits and barriers, cues to action, self efficacy, and behavior, four weeks after intervention (P < 0.001) and eight weeks after intervention (P < 0.001) were significantly more in the case group Than the control group. ANOVA with repeated measures showed a significant increase in the case group in knowledge (from 32.1 to 89.1), perceived sensitivity (from 34.8 to 91.5), perceived severity (from 31.82 to 88.48), perceived benefits (from 39.28 to 92.41), perceived barriers (from 26.93 to 88.61), cues to action (from24.65 to 92.03), self efficacy (from 29.71 to 88.75), and behavior (from 28.83 to 94.63). Changes were not significant in the control group.
Conclusion:
The effect of HBM and education on increasing knowledge and changing people's beliefs and behavior, in terms of anxiety based pregnancy, should make health planners and authorities pay more attention to these issues. Moreover, it will help in the betterment of the health of mothers and babies.
Keywords: Anxiety, education, health belief model, nulliparous women
INTRODUCTION
Pregnancy is a special experience for a woman and her family. Although, physiological changes resulting from gestation occur progressively and respectively, psychological changes do not follow this process. Psychological issues that occur in the first pregnancy include accepting the pregnancy and the maternal role, the relationship between woman and man, change of phantasm in terms of body, stresses, and fears due to pregnancy, and in short, the relationship between the mother and fetus. Therefore, a great level of social and psychological adaptation is required, and attention given to this can lead to promoting the psychological health of pregnant women and prevent family and social problems in the future.[1] Nicols and Zwelling believe that there is a direct relation between a mother's stable psychological situation during the pregnancy period and her accepting the maternal role after childbirth.[2]
Dennerstein reported that women suffer more psychological stress with regard to motherhood compared to men for fatherhood.[3] Pregnant women fear and worry about how they can fit into this new situation, and this worry causes stress that may create some of problems for them.[4] The results of several studies showed that stress disorder prevalence was more than 30%, and that reported in Iran was more than 64%.[4,5] Prenatal psychological problems have been investigated in approximately 90% of the high-income countries, while there is information for only 10% of countries in the low and moderate income category.[5] The result of a study showed that 44.8% of pregnant women have exposure to some psychological disorder.[4]
Dunkle Schetter also delineated that anxiety, depression, and stress during pregnancy can cause side-effects in the mother and fetus and lead to low birth weight of the infant, and have negative effects on the child and fetal neural development.[6] The incidence of fetal asphyxia at birth exists among anxious women, moreover, other problems that result from stress during pregnancy are, abnormal fetal heart rate patterns, low Apgar scores, increased mortality at birth, and low birth weight.[7] Intrauterine stress causes premature labor and premature infants, and is associated with a greater risk of coronary heart disease in adulthood.[8] Also there is a relationship between a mother's stress and abnormalities in fetal brain development.[9] The incidence of cleft palate and harelip is more common in infants of anxious mothers.[10]
Maternal anxiety during gestation is associated with reduced gestational age and increases the risk of premature birth.[11] A high level of pregnancy stress not only increases the risk of maternal postpartum depression and anxiety, but also leads to irritability and more crying of the baby, a more unstable condition, and even transferring to the Intensive Care Unit.[12] Furthermore, anxiety during pregnancy can lead to schizophrenia and affective disorders in the child in future.[13] A stressful event in the prenatal period not only affects the child's mental health in childhood, but is also associated with mental health problems in adulthood, which shows that it can have serious effects throughout life.[14] Severe maternal anxiety during pregnancy and after delivery imposes irreparable damage to the relationship between the mother and child and reduces her ability to play the maternal role and even reduces the production and secretion of breast milk. Anxiety during pregnancy can cause complications in the mother in various forms, including, nausea and vomiting in early pregnancy and pre-eclampsia, anxiety and negative perception toward labor and birth, unnecessary fears about childbirth and motherhood, self-medication with alcohol, or restricted activity.[15]
Mothers who have experienced dissatisfaction and unpleasant feelings of pregnancy during their gestation, do not have the preparation and necessary consent to keep the baby and to deal with the pregnancy issues. In fact, an unwanted pregnancy causes higher levels of anxiety and depression.[16] A close relationship between the mental health and physical health, in terms of pregnancy, shows the necessity of using a process for achieving good mental and physical health. The importance of mental health in this period extends to the fact that researchers believe that many problems of adulthood originate from poor conditions during the fetus and childhood periods. Thus, particular attention given to the mother's mental health during pregnancy can be a tool to prevent problems in adulthood.[1] The notion that being unaware of the facts of pregnancy and labor can lead to anxiety and fear cannot be exactly exempted. The greater the knowledge of the mother about these facts, the lesser her psychological problems will be.[17]
The World Health Organization maintains that education is a key component of prenatal care. Prenatal care is a proper opportunity to investigate, prevent, and treat the emotional distress of pregnant women. Belief and practice about preventive behaviors can play an important role in developing appropriate intervention programs. The Health Belief Model is an essential and exact pattern that is used to determine the relationship between health beliefs and behavior,[18] and is also the most important model that is used in the development and design of prevention programs. According to this model, a person's decision and motivation to cultivate a particular behavior included items such as, Person's perception of being at risk (perceived susceptibility) and its seriousness (perceived severity), belief in the perceived action of usefulness to reduce the risk of illness, and understanding of the health benefits (perceived benefits) due to obstacles and moderating factors such as demographic and psychosocial variables (awareness). Cues to action also facilitate healthy behaviors.[19] This model generally focuses on changing one's convictions and believes that changes in behavior can lead to changes in beliefs.[20] Therefore, healthcare providers must influence individual beliefs for improving their health,[21] as based on the implemented exploration, pregnant women have treated anxiety as a natural problem and are not aware of its harmful effects, or they are unable to correct it. Moreover, because they are not provided the required information on common prenatal care and also because of the lack of similar model base studies in this regard, in Iran, we are trying to reveal the importance of this issue so that timely intervention can be implemented. The aim of this study is to consider the effect of educational intervention by HBM constructs on the anxiety of nulliparous women.
MATERIALS AND METHODS
The experimental (interventional) survey was performed using a randomized comparison group, with a pre test and post test conducted. The explored population was made up of nulliparous pregnant women attending public health clinics in the Doroud city, which has seven health centers. As the all parts of the city were similar in terms of socioeconomical status and according to the study design, two centers were randomly selected. In the next step, the experimental and control groups were also selected based on the two mentioned groups, randomly. The inclusion criteria included: The first pregnancy, first trimester of pregnancy (from diagnosis of pregnancy to 12 weeks of gestation), singleton pregnancies, not having had abortions or infertility history, willingness to participate in the study, no drugs, no disease, not having high-risk pregnancy, not having a history of mental disease or referring a psychiatrist, and not having a history of depression before pregnancy. The exclusion criteria included: Unwanted pregnancy, specific mental illness, abortion risk, not attending training sessions, and large and sudden emotional damage during the intervention period. The sample size was at least 88 (44 in each group) women, based on similar studies[11,14] Data were collected based on a researcher-made questionnaire. To assess questionnaire validity, health education and the midwifery specialist's points of view were considered and the validity was confirmed by adding or removing some of the questions. In terms of reliability, the questionnaire was delivered to 30 nulliparous women, who were not included in the study. Following that, the Cronbach's alpha test was used to check the reliability of the knowledge and the HBM constructs section of the questionnaire. With this method, it was 93 and 83.7%, respectively. Regarding behavior questions, the Kuder Richardson method was used to assess reliability, and with 78.8%, this section of reliability also was confirmed. Therefore, the questionnaire reliability was confirmed. The questionnaire consisted of two parts. The first part included demographic questions such as age, education level, economic status, and employment status. The second section had questions about knowledge, constructs of HBM, and behavior. The knowledge section consisted of 22 questions that were designed as ‘yes’, ‘no,’ and ‘do not know’. The questions were graded in the following manner, they scored 1, 2, and 3 for ‘no’, ‘I don’t know,’ and ‘yes’, respectively. The model constructs included nine questions about perceived susceptibility, 10 questions about perceived severity, 12 questions in terms of perceived benefits, 12 questions on perceived barriers, six questions about self- efficacy, and finally five questions were with respect to cues to action. Questions about model constructs were graded based on the Likert scale (disagree = 1, somewhat disagree = 2, somewhat agree = 3, and agree = 4).
Behavior assessment consisted of five questions that were designed as, ‘yes’ and ‘no’, in a way that, the scores were ‘1’ and ‘2’ for ‘no’ and ‘yes’, respectively. We referred to selected clinics after getting permission of the Deputy of Research of the University, and after describing the aims of the study, the pre-test questionnaires were distributed among the samples. Moreover; guidance on how to fill out the questionnaire was given, and also a researcher was present at the time of filling the questionnaire and questions of the samples were answered as well. Education intervention was implemented in three training sessions (one hour each) in the experimental group. In the first session, after becoming familiar with each other, pregnancy anxiety was defined and the educational goals of the class and the importance of anxiety in pregnancy, symptoms of anxiety, and its effect on the mind and body of pregnant women were discussed. In the second session, the effect of anxiety on pregnancy and its outcome and its effects on the mother and fetus were discussed and the participants were made aware of the benefits and barriers, thus reducing anxiety during pregnancy in the experimental group. Finally, after explanation by the trainer, they were achieved to correct and acceptable results. The third session of the education program included the role of communication in reducing anxiety, the role of exercise and healthy nutrition in reducing anxiety, role of people, especially their husband and family, in reducing stress, and some methods to reduce anxiety and enhance their efficacy. Education was conducted by using lectures, group discussions, question and answer sessions, Power Point presentations, and training manuals. Evaluation was executed via post tests, twice, four and eight weeks after the last training session. After completion of the training sessions, training manuals were given to members of the control group. The collected data were entered into the SPSS (Ver. 20) software and analyzed using the chi-square, Mann-Whitney, and independent t-tests, and repeated measure ANOVA, at the significance level of less than 0.05. It was notable that before the first session, all the participants were asked to complete the consent form.
RESULTS
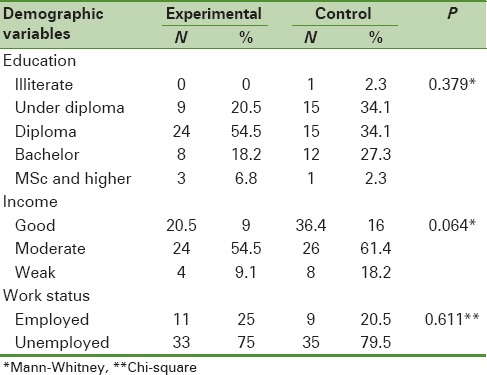
It was found that the mean age of the samples in the experimental group was 24.63 years and the age range was 15 to 38 years. The mean age of the samples in the control group was 4.88 ± 23.47 years and the age range was 16 to 33 years. The independent t-test showed that there was no significant difference between the two groups in terms of the mean age of the samples (P = 0.26). With regard to education, in the experimental and control groups, most of them had a diploma (54.5%) and less than a diploma (34.1%), respectively. The Mann-Whitney test reported that education was not different in the two groups (P = 0.379). Regarding the employment status, in the experimental and control groups, 25 and 20.5% of the samples were employed, so the chi-square test showed that the distribution of jobs in the two groups was not statistically significant (P = 0.611). The Mann-Whitney test showed no significant difference in income levels between the two groups (P = 0.064) [Table 1].
Table 1.
Frequency distribution of demographic characteristics in the two groups
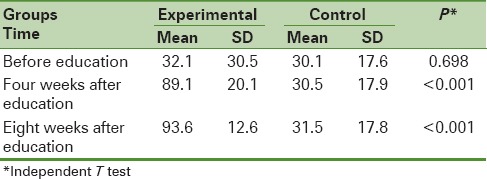
The independent t-test showed that the mean scores of knowledge, before intervention, between the two groups did not differ significantly (P = 0.829), but four weeks (P < 0.001) and eight weeks (P < 0.001) after intervention, the mean scores of knowledge in the experimental group was significantly higher than that of the control group. Repeated measure ANOVA, in the experimental group, showed that the mean scores of knowledge before the intervention and four weeks and eight weeks after the intervention were significantly different (P < 0.001), while in the control group, the mentioned status at different times were not observed (P = 0.36). The Least Significant Difference (LSD) post-hoc test showed that in the experimental group, the mean score of knowledge, four weeks after the intervention was significantly increased compared to before intervention. The latest mentioned test also showed that an average score of knowledge in the experimental group, eight weeks after the intervention, was significantly higher than before intervention (P < 0.001) [Table 2].
Table 2.
The mean score of knowledge of nulliparous women about pregnancy anxiety in the experimental and control groups
The independent t-test maintained that the mean score of the model constructs including perceived susceptibility, perceived severity, perceived benefits, perceived barriers, self-efficacy, and cues to action, before intervention were not very different in the two groups (P > 0.05). However, four weeks after intervention (P < 0.001) and eight weeks after intervention (P < 0.001), the mean scores of all the structures in the experimental group were significantly higher than those in the control group. Repeated measure ANOVA also showed that the mean score of model constructs in the experimental group before intervention and four and eight weeks after the intervention were different (P < 0.001), while in the control group, the mentioned condition was not different (P > 0.05). In the experimental group, the LSD post-hoc test showed that the mean score of the model constructs significantly increased four weeks after the intervention, than before the intervention, and in the study group, this test also showed that the mean score of constructs was significantly different eight weeks after the intervention compared to before the intervention (P < 0.001) [Tables 3 and 4].
Table 3.
The mean score of HBM l constructs of nulliparous women about pregnancy anxiety in the experimental and control groups
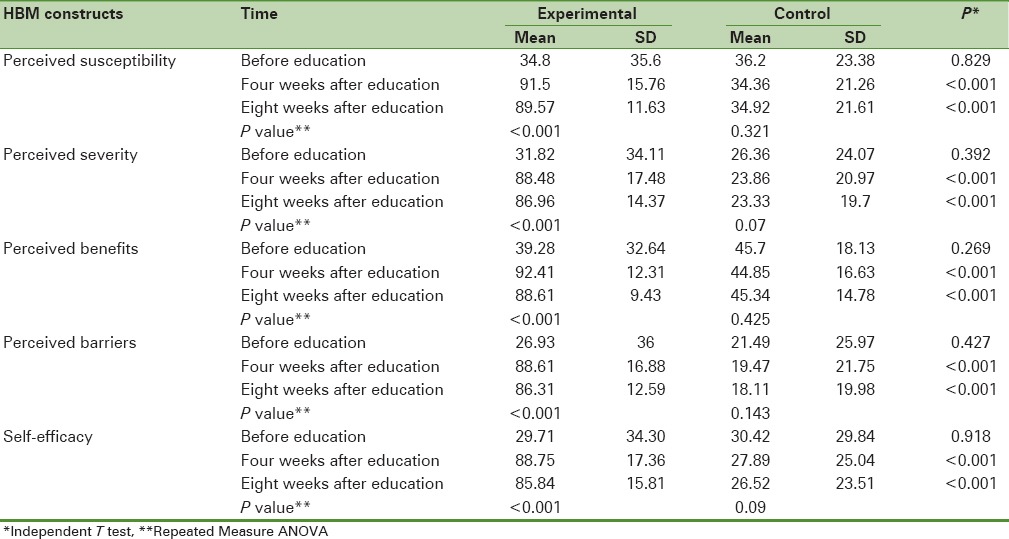
Table 4.
The mean score of cues to action and practice of nulliparous women during pregnancy anxiety in the experimental and control groups
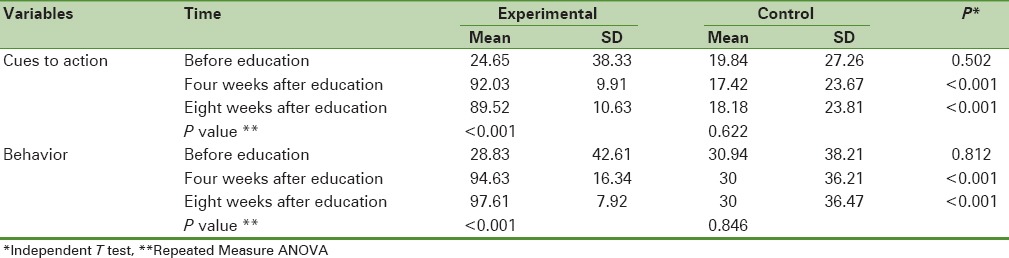
The independent t-test showed that the mean score of behavior between the two groups was not statistically different (P = 0.812), however, four weeks after intervention (P < 0.001) and eight weeks after intervention (P < 0.001), the mean score of behavior in the experimental group was significantly higher than in the control group. In the study group, repeated measure ANOVA showed that the mean scores of behavior prior to the intervention and four weeks and eight weeks after intervention were significantly different (P < 0.001), while in the control group, the mentioned condition was not seen (P > 0.05). The LSD post-hoc test showed that the mean score of behavior in the experimental group four weeks after intervention was significantly increased than before the intervention. The same test also showed that the mean score of behavior of the study group eight weeks after the intervention was different than before (P < 0.001) [Table 4].
DISCUSSION
For most women, pregnancy is a joyous period, but is often considered as a stressful period with physiological and psychological changes. As women endure many changes during pregnancy and they are greatly affected by the different stresses, this period is very vital psychologically. Therefore, evidence obtained from epidemiological studies around the world shows that mood disorders in women are twice that in men, and their peak is during pregnancy and childbirth. The research conducted by Bahadoran in 2005, has presented that 20.93% of the samples have experienced moderate-to-severe stress during pregnancy.[19]
In the present study, before intervention, the mean scores of knowledge between the two groups were not statistically significant, however, four and eight weeks after intervention, the mean knowledge score was significantly higher in the experimental group than in the control group. This difference could be attributed to the formation of classes that could greatly increase awareness about anxiety in pregnant women. In the study group, the mean score of knowledge four weeks after intervention than before intervention and eight weeks after the intervention compared to four weeks after intervention showed a significant increase. This could be the result of the continuing impact of classroom instruction, providing training manuals, increased interest of pregnant women in this topic, and also increased knowledge of other sources regarding anxiety. However, the mean scores of knowledge in the control group were not significantly different in the three mentioned time periods. Prenatal care is a great opportunity to consider the stress disorders of pregnant women. A midwife or doctor, by raising the level of education and information, can play a pivotal role in the mental health and vitality of the woman and her family. Totally, family practice and obstetrician in the process of adopting pregnancy is effective and also have important impact on reducing anxiety and stress in this period. The more well-informed a woman is, the less will be her mental health problem. Fear of childbirth is fear of the unknown, furthermore; more knowledge will reduce this fear.[22] Significant knowledge improvement in the intervention group after education has also been confirmed in other studies.[21,23] Charron, in his study, showed that model constructs were significantly associated with reproductive health behaviors and metabolic control of type 1 diabetes. Interventions focused on increasing awareness and changing health beliefs can be effective in promoting positive reproductive health behaviors of adolescent girls with diabetes.[24]
In addition, our study showed that four and eight weeks after intervention, the mean perceived susceptibility scores in the survey group was significantly higher than those the control group, and this difference reflects the impact of education on promoting the perceived susceptibility of pregnant women. Most mothers in the intervention group, after intervention, understood that anxiety could be harmful to their health and fetus, it was not a trivial event, and they felt that they were at a similar risk and this finding was associated with thesimilar studies.[21,22,25] It could be stated that the continuation of their perceived susceptibility caused their attention to health care and their baby. In Tajik's study and in Khazaie Pool's survey, the increasing perceived susceptibility after education was consistent with our study results.[17,26] In this study, a low score of perceived severity reported that pregnant women did not understand the seriousness and danger of pregnancy anxiety. Using slides and a video training manual to show the seriousness and severity of the complications and to highlight some of the irreparable consequences were critical factors for promoting the perceived severity of samples, in our study. The results of the Mohebbi and Sharifirad studies were associated with our study findings in this section.[21,25]
As increasing the perceived benefits can be important in the prevention of harmful health behaviors, our course emphasized the important role of relieving anxiety, for having a healthy pregnancy and labor, having healthy growth and health of the fetus, and creating a better and pleasant relationship with the fetus, wife, and family. This could cause a substantial and significant increase in the mean score of the perceived benefits of the study group four and eight weeks after the intervention. The mean score of the perceived benefits in the experimental group, four and eight weeks after intervention was significantly higher than that in the control group, and that seemed reasonable because of the type and quality of education. Hassani et al. also showed statistically significant differences in the perceived benefits of the individuals who do breast self-exam and individuals who do not do that.[27] In terms of perceived barriers, in the present study, the majority of pregnant women knew that talking about pregnancy anxiety with husband and family was difficult and they thought that talking about it would not help to relieve the anxiety, but would increase it. Of course, most of them were afraid that they would be reprimanded by the family. They also did not know where they should go or if there was anybody to support them. In addition, their imagination about expensive and time-consuming methods of reducing anxiety, as well as other barriers could be pointed out, which the training class and manuals tried to solve. In the study group, the mean score of perceived barriers was significantly increased after intervention, but that did not happen in the control group. In the Ghaffari study, after training, a significant difference was not found between the mean scores of perceived barriers to reduce Cesarean rates. This was inconsistent with our results.[23] The decision with regard to choosing the method of delivery could be caused by a stronger influence of friends and family rather than anxiety. Laleh Hassani's study showed that there was no significant difference in the perceived barriers of people who performed breast self-exam and those who did not perform that, which was relevant to our survey.[27] In the present study, the mean score of self-efficacy of the intervention group was increased from 29.71 to 88.75 (P < 0.05), which was statistically significant. Before the intervention, the baseline self-efficacy scores between the two groups did not differ significantly and were low in both groups. A majority of pregnant women found that they were not able to overcome anxiety and were not able to learn, and also doubted that they would be able to talk to their family and their husband on the related issue. However, after four and eight weeks of intervention, the mean score of the efficacy in the study group was significantly higher than that in the control. Group discussion was used in the self-efficacy sessions – by this method, all the participants were able to explain their views on the factors that caused prenatal anxiety. The Bastani study showed that the educational program both increased the efficacy and reduced the anxiety of nulliparous women,[28] which was in accordance with our findings. Results of the Mohebbi study were also consistent with our survey.[21]
According to our survey, four and eight weeks after intervention, the mean score of cues to action in the study group was significantly higher than that in the control group, which indicated education and effects of the training manual. Cues to action can be strong predictors of health behavior, because using training manuals and husband's participation in this field has led to a significant increase in the mean score of cues to action. In the education manual provided to pregnant women some parts point out the husband's role in making the women relax and relieving their anxiety during pregnancy and the strategies are also outlined, and the results indicate its effectiveness. Couple cooperation can be considered as an external cue to action, which relieves anxiety in pregnant women and increases the effectiveness of education classes, as well as, continues healthy behaviors in families. The study by Rahimi and colleagues have recommended that mass media can be applied to increase knowledge and healthy habits in pregnant women, in terms of exercise. Nejadsadeghi and Askerinejad have also reported that using mass media is an important and effective tool for pregnant women.[29,30,31]
In terms of behavior, four and eight weeks after intervention, the mean score of behavior was significantly higher in the study group, as compared to the control. After education, a majority of women expressed that they would attempt to remove their anxiety by talking about it with their husbands and families and ask a counselor to help them. In the Rahimikian survey, a comparison of the two groups showed that the mean scores of behavior were significantly higher after training.[32] Sharifirad's study represented that the average scores of behavior in the experimental group were significantly increased after intervention than before prior to that,[33] which was consistent with our survey. However, in Tarshizi's study, no difference was observed in the behavior of the test group after training, which was not in accordance with our study. It seems that various factors were effective in changing behavior in this group, except for education, including an appropriate economical condition to consume dairy and essential supplements.[34] In Lagampan's study, behavior of the two groups had a significant difference – it was higher in the study group, which was consistent with our study.[35]
CONCLUSION
The results of this study indicated the positive effect of educational intervention based on the Health Belief Model with regard to knowledge, perceived susceptibility, perceived severity, perceived benefits, perceived barriers, self-efficacy, cues to action, and pregnant women's attitude toward anxiety. The results show the importance of control of anxiety during pregnancy. Furthermore, as there are limited interventional and theory-based studies that can relieve anxiety during pregnancy and lead to pregnant performance improvement, it is recommended that researchers across the country design special training programs to reduce anxiety during pregnancy, until they lead to a developed standardized training program model for reducing anxiety during pregnancy in the country.
LIMITATIONS
The lack of a concurrent presence of the husbands of pregnant women in the training classes was caused by shortage of teaching space. It is suggested that in the further research, the concurrent presence of both husband and wife must noted, due to the important role that husbands can play for relieving anxiety in pregnant women. Due to the lack of similar studies in terms of pregnancy anxiety when using the Health Belief Model, the scholars inevitably used other studies in the discussion that measured the impact of education on other topics based on the Health Belief Model. It is notable that, in this study we did not assess the anxiety score in women, which could be considered as a limitation.
This article was derived from the MSc thesis of Health Education of the Isfahan University of Medical Science No. 391320.
Footnotes
Source of Support: Isfahan University of Medical Sciences
Conflict of Interest: No coflicts of interest exist between the authors
REFERENCES
- 1.Moein Z. Tehran: Cultural Affairs and Prevention Publication; 2001. Mental health of mothers during pregnancy. [Google Scholar]
- 2.Nicols F, Zwelling E. Philadelphia: W. B Saunders Co; 1997. Maternal and newborn nursing. [Google Scholar]
- 3.Dennerstein L, Estebri J, Mors K. Tehran: Boshra Publication; 2003. Women's Health (Psychosocial aspects and mental health) [Google Scholar]
- 4.Mardanihamule M, Ebrahimi E. Mental Health Status of Pregnant Women Referring to Shahinshahr Health Care Centers. Bouyeh journal Gorgan Univ Med Sci. 2010;7:27–33. [Google Scholar]
- 5.Alipour Z, Lamyian M, Hajizadeh E. Anxiety during Pregnancy: A Risk Factor for Neonatal Physical outcome. J Urmia Nurs Midwifery Fac. 2011;9:30–8. [Google Scholar]
- 6.Dunkel Schetter C, Tanner L. Anxiety, depression and stress in pregnancy: Implications for mothers, children, research, and practice. Curr Opin Psychiatry. 2012;25:141–8. doi: 10.1097/YCO.0b013e3283503680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Babanazari L, Kafi SM. Comparative study of anxiety in relation to different periods of pregnancy, marital satisfaction and demographic factors. Iranian Journal of Psychiatry and Clinical Psychology. 2008;14:206–13. [Google Scholar]
- 8.Shayeghian Z, Rasolzadeh Tabatabaey SK, Seddighilooye E. Effect of Maternal Anxiety during Third Trimester on Pregnancy Outcomes and Infants’ Mental Health. Journal of Faculty of Nursing and Midwifery. 2009;14:57–64. [Google Scholar]
- 9.Ghazavi H, Ahadi M, Aghasi Yazdi Z, Behzadmehr A. Anxiety in pregnancy. J Raze Behzistan. 2008;17:19–21. [Google Scholar]
- 10.Nasiri AF, Salmalian H, Hajiahmadi M, Ahmadi AM. Association between Prenatal Anxiety and Spontaneous Preterm Birth. J Babol Univ Med Sci. 2009;11:42–8. [Google Scholar]
- 11.Toosi M, Akbarzadeh M, Zare N, Sharif F. Effects of attachment behaviors education on anxiety and attachment of mother to baby at first pregnancy. J Fac Nurs Midwifery. 2011;17:69–79. [Google Scholar]
- 12.Bazrafshan MR, Ghorbani Z. The Effect of slow stroke back massages on anxiety among primigravid women. J Fac Nurs Midwifery. 2010;16:34–40. [Google Scholar]
- 13.Shahidi LH, Moghimian M, Tavakkoli Zadeh J. The comparison of depression in wanted and unwanted pregnancies. J Gonabad Univ Med Sci Health Serv. 2002;8:90–5. [Google Scholar]
- 14.Motevally E, Faizi Z, Ganji T, Haghani H. Effect of watching childbirth by videotape on anxiety level of primigravid mothers. Iran J Nurs. 2003;15-16:100–4. [Google Scholar]
- 15.Glance K, Marcus F, Barbara L. Health behavior and health education (Theory, Research, Operation) In: Forough S, editor. Tehran: Ladan Publication; 1997. pp. 68–84. [Google Scholar]
- 16.Khazaie PM, Ebadiazar F, Solhi M, Asadilari M, Abdi N. Study in the effect of education through Health Belief Model on the perceptions of girl Students in primary school about breakfast and snack in Noshahr-2007. Toloo e Behdasht. 2008;7:51–63. [Persian] [Google Scholar]
- 17.Shojaezadeh D, Mehrabbaic A, Mahmoodi M, Salehi L. To evaluate of efficacy of education based on Health Belief Model on knowledge, attitude and practice among women with low socioeconomic status regarding osteoporosis prevention. Iran J Epidemiol. 2011;7:30–7. [Google Scholar]
- 18.Ebadi Fard Azar F, Solhi M, Zohoor AR, Hosseini AM. The effect of Health Belief Model on promoting preventive behaviors of osteoporosis among rural women of Malayer. J Qazvin Univ Med Sci Health Serv. 2012;16:58–64. [Google Scholar]
- 19.Bahadoran P, Mohamadalibeygi N. Stress and anxiety during pregnancy. J Nurs Midwifery Res. 2005;27:18–23. [Google Scholar]
- 20.Nasiri M. Tehran: Boshra publication; 2000. Pregnancy and Childbirth Mental Health. [Google Scholar]
- 21.Mohebi M. Effect of nutrition education program on the recommended weight gain in during pregnancy application of Health Belief Model: A randomaized cilinical trial. J Qom Univ Med Sci. 2012;6:23–30. [Google Scholar]
- 22.Ghaffari M, Sharifirad GH, Akbari Z, Khorsandi M, Hassanzadeh A. Health belief model-Based education and reduction of cesarean among pregnant women: An interventional study. Health Syst Res. 2011;7:200–8. [Google Scholar]
- 23.Charron-Prochownik D, Sereika SM, Becker D, Jacober S, Mansfield J, White NH, et al. Reproductive health beliefs and behaviors in teens with diabetes: Application of the Expanded Health Belief Model. Pediatr Diabetes. 2001;2:30–9. doi: 10.1046/j.1399-543x.2001.00000.x. [DOI] [PubMed] [Google Scholar]
- 24.Ebadifardazar F, Solhi M, Pakpurhajiagha A, Yekaninejad MS. The impact of health education through Health Belief Model (H.B.M) on mother's perceptions about obesity children obese male student in elementary schools (17th district, Tehran City) J Health Adm. 2006;8:7–14. [Google Scholar]
- 25.Sharifirad GH, Hazavehie SM, Mohebi S, Rahimi MA, Hasanzadeh A. The effect of educational program based on Health Belief Model (HBM) on the foot care by type II diabetic patients. Iran J Endocrinol Metab. 2006;8:231–9. [Google Scholar]
- 26.Tajik R, Shamsi M, Mohamadbeigi A. Knowledge, attitude and behavior of mothers in the arbitrary use of drugs in Arak. Payesh. J Iran Inst Health Sci Res. 2011;10:197–204. [Google Scholar]
- 27.Hassani L, Aghamolaei T, Tavafian SS. Exercise self-efficacy, exercise perceived benefits and barriers among students in Hormozgan University of Medical Sciences. Iran J Epidemiol. 2009;4:9–15. [Google Scholar]
- 28.Bastani F, Heidarnia AR, Vafaei M, KazemNejad A, Kashanian M. The effect of relaxation training based on self-efficacy theory on mental health of pregnant women. Iran J Psychiatry Clin Psychol. 2006;12:109–116. [Google Scholar]
- 29.Rahimi S, Sayed RE. Reproductive health beliefs and behaviors in teens with diabetes. Iran Nurs Period. 2004;17:6–10. [Google Scholar]
- 30.Nejadsadeghi E, Taghdisi MH. Evaluation of pregnant women in the field of urinary tract infection according to the components of Health Belief Model. J Jahrom Med School. 2011;8:36–42. [Google Scholar]
- 31.Askernejad M, Bakhshi H. Analysis of awareness, attitude and actions of pregnant women of Rafsanjan towards the importance of care taking during pregnancy in the year 2000. Rafsanjan Med Sci Univ Mag. 2002;1:1–7. [Google Scholar]
- 32.Rahimikian F, Mirmohamadali M, Mehran A, Aboozari K, Salmaanibarough N. Effect of education designed based on Health Belief Model on choosing delivery mode. J Fac Nurs Midwifery. 2009;14:25–32. [Google Scholar]
- 33.Sharifirad GH, Hazavei MM, Hasan- Zadeh A, Danesh-Amouz A. The effect of health education based on Health Belief Model on preventive actions of smoking in grade one, middle school students. Arak Med Univ J. 2007;10:79–86. [Google Scholar]
- 34.Torshizi L, Anoosheh M, Ghofranipour F, Ahmadi F, Houshyar-Rad A. The effect of education based on Health Belief Model on preventive factors of osteoporosis among postmenopausal women. Iran J Nurs. 2009;22:71–82. [Google Scholar]
- 35.Lagampan S, Lapvongwatana P, Tharapan C, Nonthikorn J. Health Belief Model teaching program for thalassemia education in high school students. Chula Med J. 2004;48:723–35. [Google Scholar]


