Abstract
Metaplastic breast cancer is a rare malignancy in the breast. Neurofibromatosis Type 1 is an autosomal dominant multisystem disorder associated with multiple neoplasms such as optic gliomas and peripheral nerve sheath tumors. The association of breast cancer with neurofibromatosis is very rare. We present a case of a metaplastic breast cancer in a patient with Type 1 neurofibromatosis. The patient presented with a palpable mass in her left breast with suspicious findings on mammogram and ultrasound. Ultrasound-guided percutaneous biopsy showed metaplastic breast carcinoma with metastasis to an axillary lymph node. This is the third case report in the English literature to show metaplastic breast carcinoma in a patient with Type 1 neurofibromatosis. In this report we review recent literature and discuss the association between these two entities.
Keywords: Breast imaging, metaplastic breast carcinoma, neurofibromatosis
INTRODUCTION

Metaplastic breast cancer is a rare entity, with an incidence of less than 0.1-0.5% of all breast malignancies.[1] Neurofibromatosis Type 1 (NF1) is an autosomal dominant multisystem disorder affecting 1 in 3500 people.[2] It is associated with multiple neoplasms such as optic gliomas and peripheral nerve sheath tumors, but is rarely associated with breast cancer.[3] A study by Sharif et al., has shown that women with a history of NF1 have a fivefold increased risk of breast cancer.[4] So far, only two cases of metaplastic carcinoma in patients with NF1 have been described in the English literature.[5,6] We present a case of metaplastic breast cancer with keratinizing squamous histology in a patient with history of NF1. The imaging findings of metaplastic breast carcinoma and the association between metaplastic breast cancer and neurofibromatosis are reviewed and discussed.
CASE REPORT
A 46-year-old female with history of NF1 presented with a new self-discovered left breast mass. Her cutaneous neurofibroma was diagnosed after removal of two of her skin lesions with one on her ankle and the other one on her shoulder. No other neoplasm was found so far. She had no previous mammograms. The patient reported that her father had neurofibromatosis, but there was no family history of breast cancer. Approximately 8 cm large mass was palpated in the central left breast on physical examination. The skin was edematous with slight erythema.
Mammogram showed a large, centrally located left breast mass associated with microcalcifications measuring 10 × 10 × 9 cm [Figure 1]. The skin lesions (neurofibromas) were indicated by the circular-shaped radiopaque skin markers consistent with patient's known neurofibromatosis. Ultrasound of the subareolar left breast showed a large circumscribed mass, with central necrosis and irregular peripheral solid components [Figure 2]. An enlarged left axillary lymph node was also identified, measuring about 1.6 × 0.8 × 1.4 cm [Figure 3]. The lesion was classified as Breast Imaging Reporting and Data System (BI-RADS) 4. Ultrasound-guided core biopsy was performed on the breast mass and axillary lymph node. Pathologic examination of the breast mass showed metaplastic breast carcinoma with keratinizing squamous histology [Figure 4]. The neoplastic cells overexpressed human epidermal growth factor receptor 2 (HER2) (3+) and were negative for estrogen receptor (ER) and progesterone receptor (PR). Pathology of the axillary node revealed metastatic metaplastic breast carcinoma. Breast magnetic resonance imaging (MRI) was then performed, which demonstrated a large heterogeneous mass with low T1 and high T2 signals and nodular peripheral rim enhancement [Figure 5]. The small enhancing nodules (neurofibromas) on the skin were consistent with the patient's known neurofibromatosis [Figure 5]. Computed Tomography (CT) of chest, abdomen and pelvis as well as bone scan studies demonstrated no distal metastasis or other disease related to NF1 except numerous cutaneous neurofibromas throughout the body. The staging method used was American Joint Committee on Cancer (AJCC) 7th Edition, and this showed a clinical stage IIIA.
Figure 1.
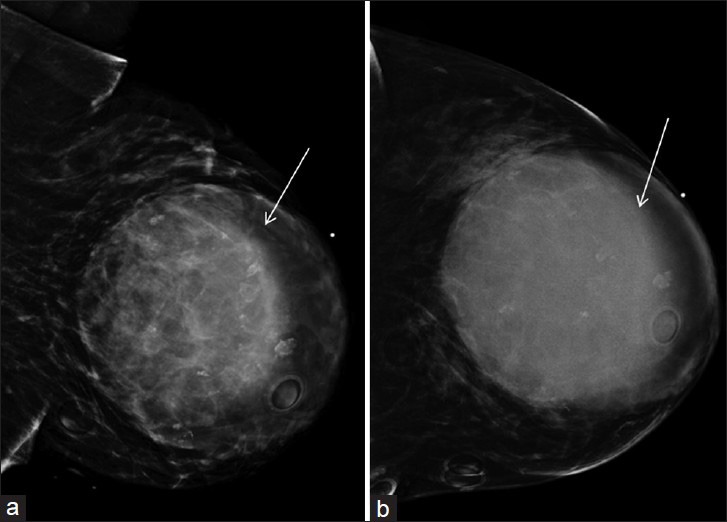
46-year-old female with history of neurofibromatosis Type 1 presented with left breast mass diagnosed as metaplastic breast carcinoma. Mediolateral (a) oblique and (b) craniocaudal views of left breast mammogram demonstrate a large, relatively circumscribed mass (arrows) adjacent to a dot-shaped radiopaque skin marker to indicate the palpable area in the central left breast. It measured approximately 10 × 10 × 9 cm. Circular-shaped radiopaque skin markers were placed to indicate the skin lesions (neurofibromas) which are consistent with patient's known neurofibromatosis.
Figure 2.
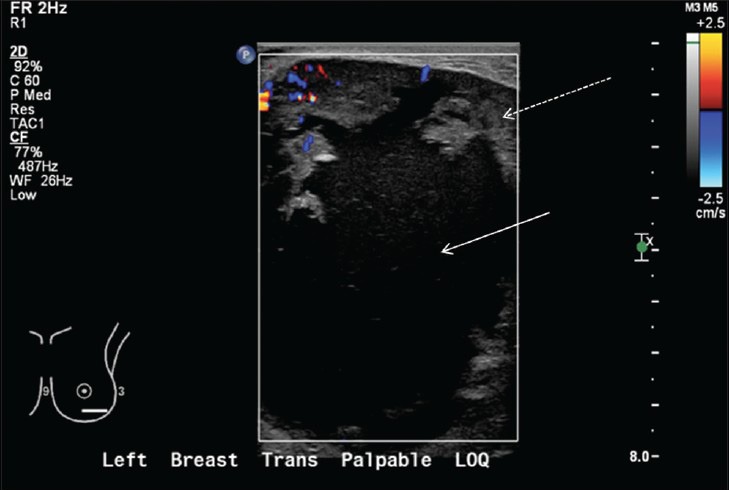
46-year-old female with history of neurofibromatosis Type 1 presented with left breast mass diagnosed as metaplastic breast carcinoma. Targeted breast ultrasound on the palpable area in the central left breast demonstrates a large heterogeneous mass with central necrosis (solid arrow) and peripheral irregular solid components (dashed arrow) with Doppler flow.
Figure 3.
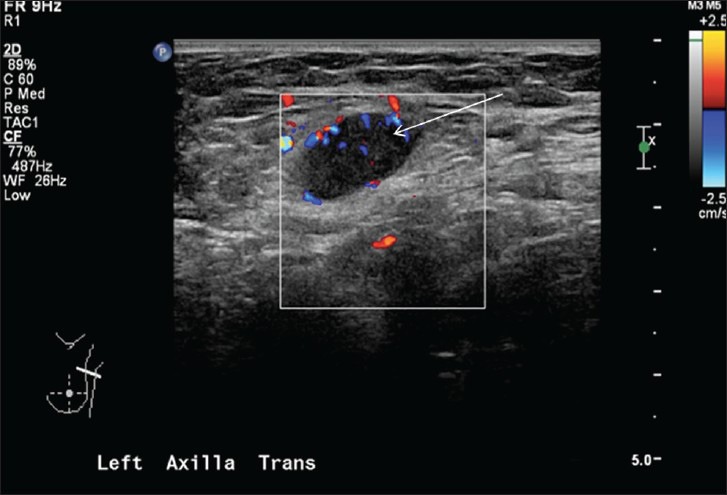
46-year-old female with history of neurofibromatosis Type 1 presented with left breast mass diagnosed as metaplastic breast carcinoma. Ultrasound of the left axilla showed an enlarged axillary lymph node (arrow) with eccentric thickened cortex.
Figure 4.
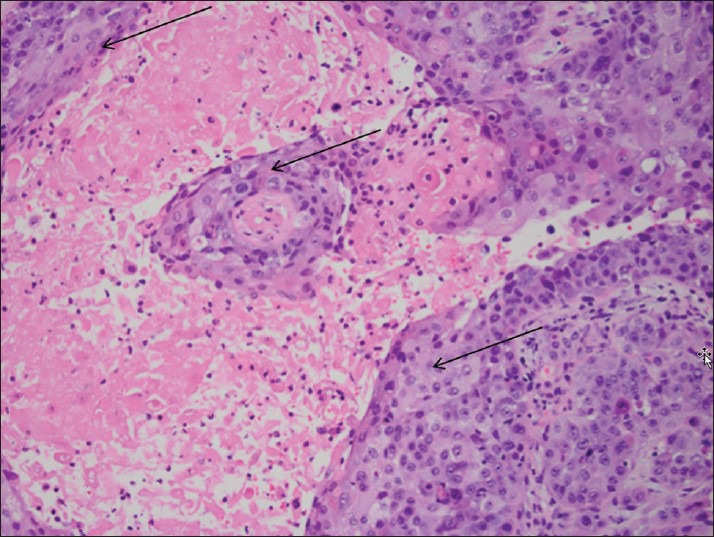
46-year-old female with history of neurofibromatosis Type 1 presented with left breast mass diagnosed as metaplastic breast carcinoma. Microscopic examination of the core biopsy (hematoxylin and eosin stain, ×200) reveals solid sheets of neoplastic cells with squamous differentiation (arrows), diagnostic of metaplastic breast carcinoma with keratinizing squamous histology.
Figure 5.
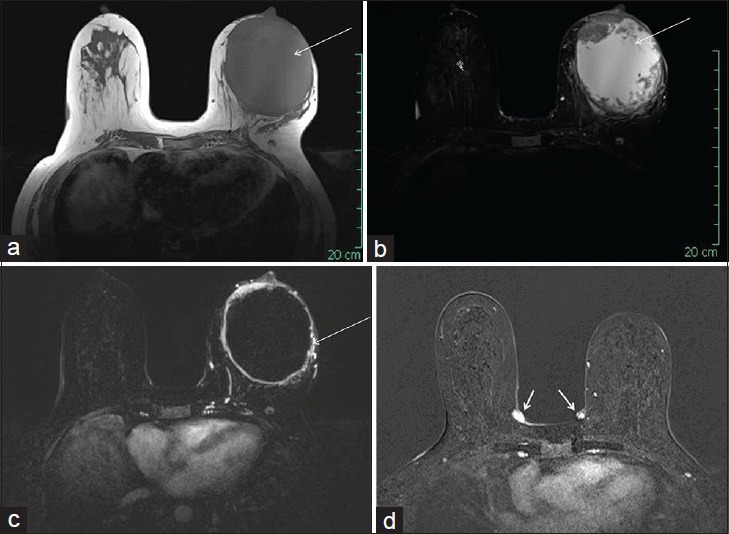
46-year-old female with history of neurofibromatosis Type 1 presented with left breast mass diagnosed as metaplastic breast carcinoma. Breast MRI with (a) T1-weighted, (b) short tau inversion recovery (STIR), and (c and d) subtraction post-contrast images demonstrate a large mass (long arrows) in the central left breast with low T1 (a), high T2 (b), and rim-like enhancement (c). Small enhancing nodules (neurofibromas) (short arrows) are also noted at the skin of the left breast, consistent with patient's known neurofibromatosis (d).
Breast MRI, performed after the patient completed 8 cycles of neoadjuvant chemotherapy, demonstrated significantly decreased tumor size, peripheral rim enhancement [Figure 6], and axillary lymphadenopathy. The patient then underwent a left mastectomy and sentinel lymph node biopsy. Pathologic analysis of the mastectomy specimen demonstrated a minute focus of residual viable metaplastic carcinoma (0.03 cm) in a 6.1 cm necrotic tumor bed with near-complete response. Micrometastatic metaplastic carcinoma was noted in one of five sentinel lymph nodes. The patient subsequently underwent radiation therapy and Herceptin treatment. One year later, a prophylactic right skin-sparing mastectomy was performed due to her elevated breast cancer risk with NF1. At follow-up 12 months after the initial diagnosis, the patient is without evidence of recurrent disease or distant metastasis.
Figure 6.
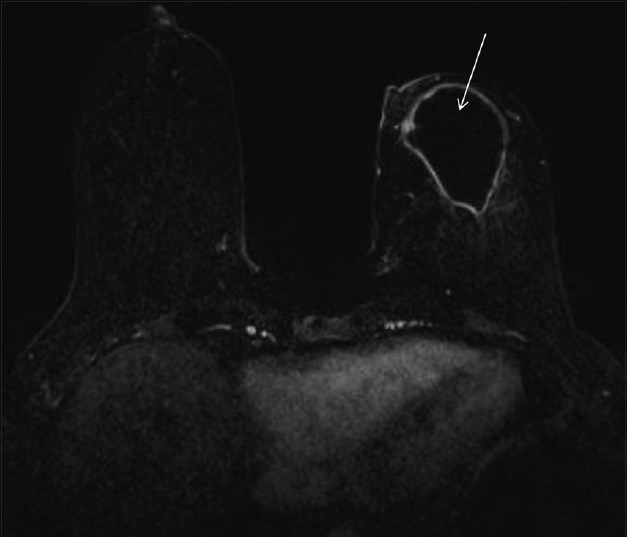
46-year-old female with history of neurofibromatosis Type 1 presented with left breast mass diagnosed as metaplastic breast carcinoma. Breast MRI status post chemotherapy with subtraction post-contrast image shows significantly decreased size and rim enhancement of the mass (arrow) in the left breast.
DISCUSSION
Metaplastic breast carcinoma is a subtype of breast carcinoma that exhibits a non-glandular growth pattern.[1] The non-glandular histology can be epithelial (e.g. squamous as in our case) or mesenchymal (e.g. spindled, sarcomatous, chondroid, or osseous).[7,8] Metaplastic carcinoma is challenging on core biopsy for pathologists due to its non-glandular histology. The differential diagnosis often includes sarcoma, melanoma, malignant phyllodes tumor, and squamous cell carcinoma depending on the particular histology. The tumor tends to be greater than 3 cm at presentation, which is usually in Stage II or III. Lymph node involvement is less common with the rate of involvement ranging from 13% to 54%. These tumors tend to have a lower expression of ER, PR, and HER2 compared to invasive ductal carcinoma and more often occur in women older than 50 years.[8] This is in contrast to our case, in which the patient was 46 years old, premenopausal, and HER2 positive.
On mammography, this entity tends to be more circumscribed than typical invasive ductal carcinoma, although occasionally may demonstrate ill-defined or spiculated margins.[8] Microcalcifications are overall less common than in invasive ductal carcinoma.[8] On sonography, they may be round or lobular shaped, circumscribed to ill-defined masses. Overall, they display more benign features than invasive ductal carcinoma.[8] On MRI, metaplastic breast carcinoma tends to have high T2 signal, thought to be due to mucoid contents and/or necrosis.[8] The most common pattern on post-contrast images is heterogeneous enhancement, with the second most common pattern being rim-like enhancement such as the tumor in our case.[8]
The treatment option for metaplastic breast carcinoma is determined by the stage of the tumor.[9] As these lesions tend to be large at detection, they are usually treated with a combination of surgery, chemotherapy, and radiation, as in our case.[9] The prognosis of metaplastic breast carcinoma is generally considered worse than that of other breast cancers.[7,9]
Neurofibromatosis is an autosomal dominant disease, with mutations in the Neurofibromin 1 gene, which is located in chromosome band 17q II.2 and encodes the protein neurofibromin, a tumor suppressor and a negative regulator of the rat sarcoma (ras) signal transduction pathway.[2] A variety of neoplasms have been reported in patients with NF1, including cutaneous neurofibroma, plexiform fibromas, optic gliomas, astrocytomas, and pheochromocytomas. The association with breast cancer is very rare.[3] A few recent studies have suggested that there may be an increased risk of breast cancer in patients with NF1.[4] The breast cancer gene 1 (BRCA1) is located on the long arm of chromosome 17.[10] Although Güran and Safali have suggested a possible interaction between these two genes,[10] the link between the two genes is not quite clear yet and more studies are needed to address it. In our case, BRCA testing was not performed on the patient probably due to the fact that no other family member presented with breast cancer.
The occurrence of metaplastic breast cancer with NF1 is extremely rare. Only two cases have been reported so far in the English literature.[5,6] Our case is the third case report of metaplastic breast cancer in an NF1 patient. Since it is difficult to address the association of a particular subtype such as metaplastic breast cancer with NF1 from this single case, further studies on the molecular mechanisms and association of breast cancer, including metaplastic breast cancer, with neurofibromatosis are needed. In addition, awareness of the increased risk of breast cancer in patients with neurofibromatosis with close surveillance, prevention, and management is recommended.
CONCLUSION
Metaplastic breast cancer is a rare form of breast malignancy. The occurrence of metaplastic breast cancer in a patient with NF1 is extremely rare. Further exploration of the role of Neurofibromin 1 gene in the oncogenesis of breast cancer, including metaplastic breast cancer, is needed. Close surveillance for breast cancer in patients with neurofibromatosis is warranted.
Footnotes
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2015/5/1/17/154102
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Lai HW, Tseng LM, Chang TW, Kuo YL, Hsieh CM, Chen ST, et al. The prognostic significance of metaplastic carcinoma of the breast (MCB)-a case controlled comparison study with infiltrating ductal carcinoma. Breast. 2013;22:968–73. doi: 10.1016/j.breast.2013.05.010. [DOI] [PubMed] [Google Scholar]
- 2.Boyd KP, Korf BR, Theos A. Neurofibromatosis type 1. J Am Acad Dermatol. 2009;61:1–16. doi: 10.1016/j.jaad.2008.12.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Salemis NS, Nakos G, Sambaziotis D, Gourgiotis S. Breast cancer associated with type 1 neurofibromatosis. Breast Cancer. 2010;17:306–9. doi: 10.1007/s12282-009-0119-7. [DOI] [PubMed] [Google Scholar]
- 4.Sharif S, Moran A, Huson SM, Iddenden R, Shenton A, Howard E, et al. Women with neurofibromatosis 1 are at a moderately increased risk of developing breast cancer and should be considered for early screening. J Med Genet. 2007;44:481–4. doi: 10.1136/jmg.2007.049346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Natsiopoulos I, Chatzichristou A, Stratis I, Skordalaki A, Makrantonakis N. Metaplastic breast carcinoma in a patient with Von Recklinghausen's disease. Clin Breast Cancer. 2007;7:573–5. doi: 10.3816/CBC.2007.n.015. [DOI] [PubMed] [Google Scholar]
- 6.Vivas AP, Bomfin LE, Pinto CA, Nicolau UR, Alves FA. Oral metastasis of metaplastic breast carcinoma in a patient with neurofibromatosis 1. Case Rep Oncol Med 2014. 2014 doi: 10.1155/2014/719061. 719061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Beatty JD, Atwood M, Tickman R, Reiner M. Metaplastic breast cancer: Clinical significance. Am J Surg. 2006;191:657–64. doi: 10.1016/j.amjsurg.2006.01.038. [DOI] [PubMed] [Google Scholar]
- 8.Choi BB, Shu KS. Metaplastic carcinoma of the breast: Multimodality imaging and histopathologic assessment. Acta Radiol. 2012;53:5–11. doi: 10.1258/ar.2011.110341. [DOI] [PubMed] [Google Scholar]
- 9.Hu Q, Chen WX, Zhong SL, Li J, Luo Z, Tang JH, et al. Current progress in the treatment of metaplastic breast carcinoma. Asian Pac J Cancer Prev. 2013;14:6221–5. doi: 10.7314/apjcp.2013.14.11.6221. [DOI] [PubMed] [Google Scholar]
- 10.Güran S, Safali M. A case of neurofibromatosis and breast cancer: Loss of heterozygosity of NF1 in breast cancer. Cancer Genet Cytogenet. 2005;156:86–8. doi: 10.1016/j.cancergencyto.2004.04.019. [DOI] [PubMed] [Google Scholar]


