Abstract
Background:
Malignant transformation of craniopharyngiomas is quite rare, and the etiology of transformation remains unclear. The prognosis of malignantly transformed craniopharyngiomas is very poor.
Case Description:
A 36-year-old male had five craniotomies, five transsphenoidal surgeries, and two radiation treatments until 31 years of age after diagnosis of craniopharyngioma at 12 years of age. All serial pathological findings indicated adamantinomatous craniopharyngioma including those of a surgery performed for tumor regrowth at 31 years of age. However, when the tumor recurred approximately 5 years later, the pathological findings showed squamous metaplasia. The patient received CyberKnife surgery, but the tumor rapidly regrew within 4 months. The tumor was resected with the cavernous sinus via a dual approach: Transcranial and transsphenoidal surgery with an extracranial-intracranial bypass using the radial artery. Pathologic examination of a surgical specimen showed that it consisted primarily of squamous cells; the lamina propria was collapsed, and the tumor cells had enlarged nuclei and clarification of the nucleolus. The tumor was ultimately diagnosed as malignant transformation of craniopharyngioma. After surgery, he received combination chemotherapy (docetaxel, cisplatin, and fluorouracil). The tumor has been well controlled for more than 12 months.
Conclusion:
Serial pathological changes of the craniopharyngioma and a review of the 20 cases reported in the literature suggest that radiation of the squamous epithelial cell component of the craniopharyngioma led to malignant transformation via squamous metaplasia. We recommend aggressive surgical removal of craniopharyngiomas and avoidance of radiotherapy if possible.
Keywords: Craniopharyngioma, malignant transformation, squamous metaplasia, TPF chemotherapy
INTRODUCTION
Craniopharyngioma was first described in 1904 by Erdheim et al.[10] The term “craniopharyngioma”—introduced in 1932 by Cushing et al.[9]—refers to a benign epithelial tumor arising from the remnants of epithelial tissue in improperly formed pituitary glands or the craniopharyngeal duct remnants.[14,18] Craniopharyngioma accounts for 5–10% and 1.2–4.6% of adolescent and adult brain tumors, respectively.[5]
Malignant transformation of craniopharyngiomas is quite rare, with little information being available. It has been suggested that radiation and multiple surgeries are the inducing factors but the etiology of transformation remains unclear. We report a case of craniopharyngioma with malignant transformation and analyze the pathological transition.
CASE REPORT
The clinical course and corresponding figures are shown in Figure 1. A 36-year-old male had five craniotomies and five transsphenoidal surgeries between the ages of 12, when adamantinomatous craniopharyngioma was first diagnosed. He also received local irradiation at 15 years of age. When he was 31 years old, tumor regrowth occurred in the left cavernous sinus [Figure 2a]. We removed this lesion [Figure 2b], which appeared to be an adamantinomatous craniopharyngioma, and performed gamma-knife surgery (GKS) because of frequent cyst formations. When the patient was 36 years and 3 months of age, the tumor recurred in the cavernous sinus and surrounded the left optic nerve [Figure 2c]. Transsphenoidal biopsy was performed; the pathological findings showed squamous metaplasia, and CyberKnife surgery was performed on the residual lesion [Figure 2d]. However, the residual tumor regrew rapidly in the irradiated area during the next 4 months [Figure 2e and f], suggesting malignant transformation of the tumor. The patient was then readmitted to our department. Neurological findings at admission were blindness in his left eye and multiple complete nerve palsies of the oculomotor, trochlear, and abducens nerves on his left side. Because tumor invasion had spread into the cavernous sinus involving the carotid artery, we used a dual approach to resect the tumor, carotid artery, and cavernous sinus: Transcranial and transsphenoidal surgeries with an extracranial-intracranial (EC-IC) bypass using the radial artery. The postoperative course was uneventful, and the tumor was completely removed [Figure 3a–d].
Figure 1.
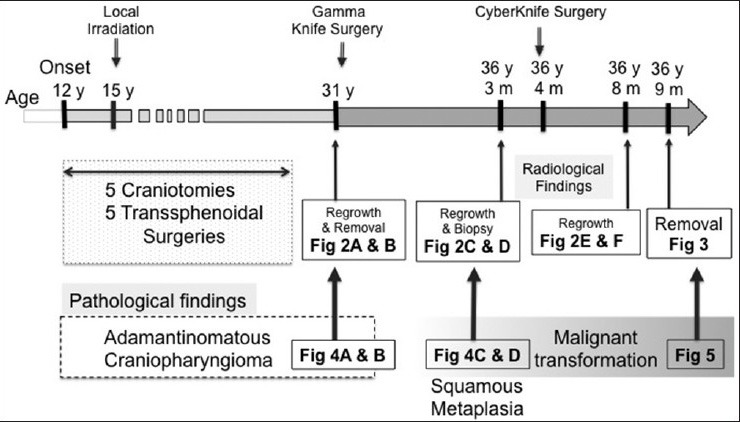
Diagram showing the clinical course of the tumor including surgical procedures and pathological findings
Figure 2.
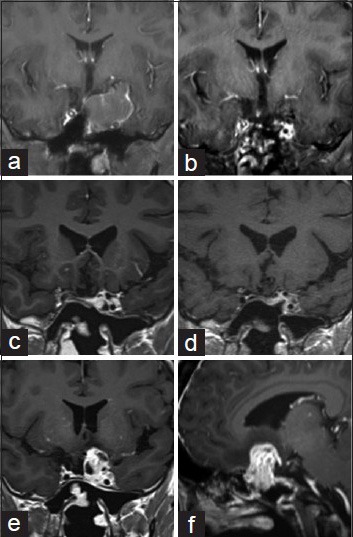
Successive gadolinium-enhanced magnetic resonance images (MRIs) showing the clinical course of the craniopharyngioma during a 6-year period. (a) Tumor regrowth in the left cavernous sinus at 31 years of age. (b) MRI after removal of the lesion and gamma knife surgery. (c) Tumor regrowth at 36 years and 3 months of age. The tumor grew around the left optic nerve. (d) MRI after transsphenoidal biopsy. (e, f) MRIs at 31 years and 8 months of age. Tumor size increased drastically, and the tumor invaded the cavernous sinus and the internal carotid artery
Figure 3.
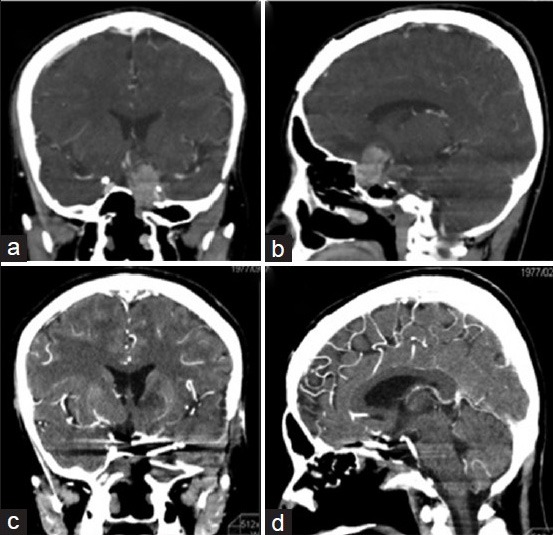
Computed tomography scans with contrast enhancement before (a and b) and after (c and d) the operation of transcranial and transsphenoidal dual surgeries with an extracranial-intracranial bypass. The tumor was totally removed
Serial pathological changes are shown in Figures 4 and 5. In the specimen taken at 31 years of age, the tumor was covered with prickle cells, and a single layer of nonatypical basal cells and cholesterin crystals were present in the interstitial tissue Internal layer of stellate cells in loose connective matrix was found [Figure 4a and b]. Similar findings had been reported in all serial pathologic examinations before 31 years of age, and the tumor was diagnosed as an adamantinomatous craniopharyngioma. The specimen taken at 36 years and 3 months of age showed densely packed squamous cells and stratification of basal cells with an atypical appearance characteristic of squamous metaplasia. The features of adamantinomatous craniopharyngioma were no longer apparent [Figure 4c, d].
Figure 4.
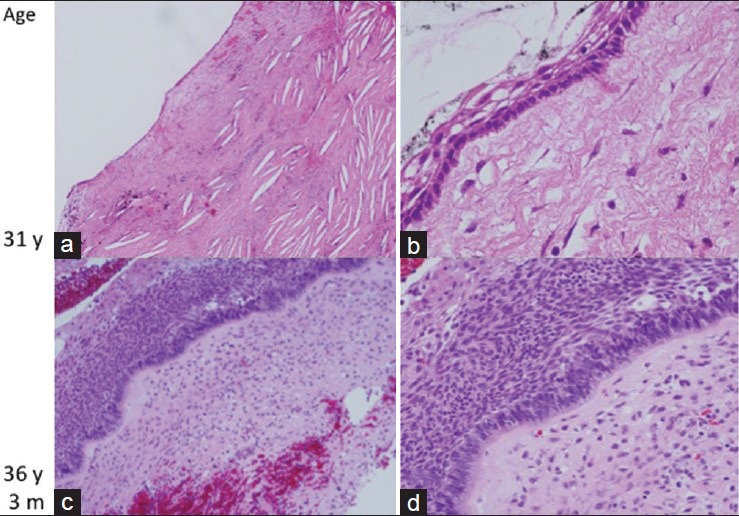
Pathological findings. (a and b) Histopathology at 31 years of age. The tumor is covered with prickle cells, and a single layer of nonatypical basal cells and cholesterin crystals is present in the interstitial tissue. The diagnosis was adamantinomatous craniopharyngioma. (c and d) Histopathology at 36 years and 3 months of age. Densely packed squamous cells and stratification of basal cells with an atypical appearance are seen. The features of adamantinomatous type craniopharyngioma are no longer apparent. (c–d) Hematoxylin and eosin staining at the original magnification
Figure 5.
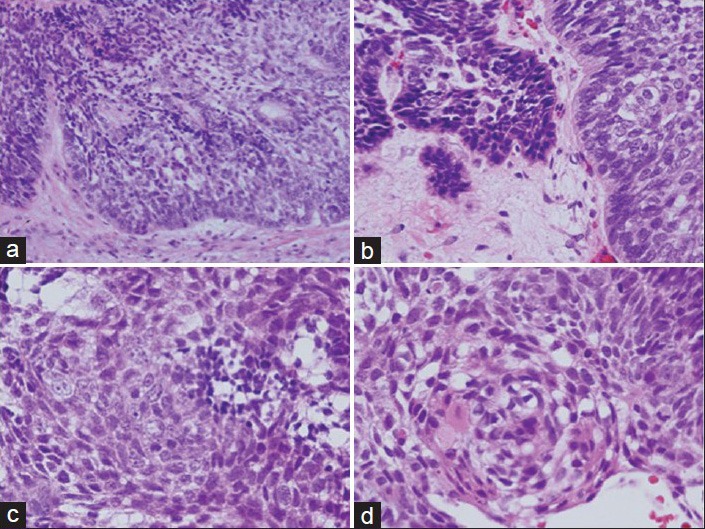
Pathological findings of a specimen from the transcranial and transsphenoidal dual surgeries at 36 years and 9 months of age. (a) The number of squamous cells has increased. (b) The lamina propria has collapsed, and infiltration of atypical cells is seen. (c) Tumor cells have enlarged nuclei and clarification of the nucleolus. (d) Parakeratosis and intercellular bridges are present in the tissue. Hematoxylin and eosin staining at the original magnification
A specimen from the transcranial and transsphenoidal dual surgeries consisted chiefly of squamous cells [Figure 5]. The lamina propria was collapsed, and infiltration of atypical cells was observed in interstitial tissue. Tumor cells had enlarged nuclei and clarification of the nucleolus. Parakeratosis and intercellular bridges were also present in the tissue, which resembled squamous cell carcinoma (SCC). As shown in immunohistochemistry, the abundance of p40 (a specific marker of squamous cells) and p53 (the indicator of malignancy) progressively increased between the ages of 31 and 36 years and 9 months [Figure 6]. On the basis of these findings, the case was ultimately diagnosed as malignant transformation of craniopharyngioma.
Figure 6.
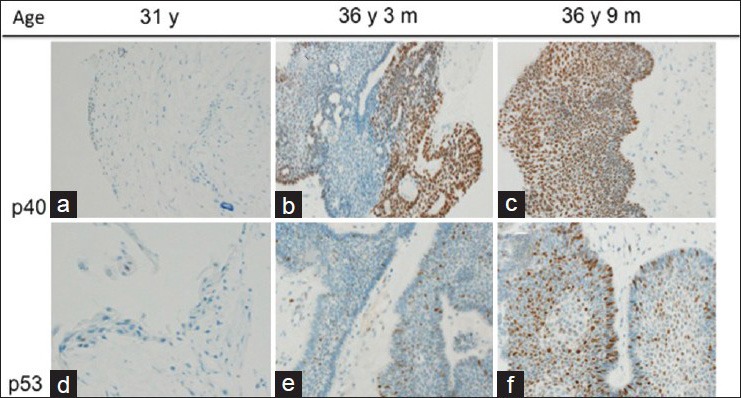
Immunohistochemistry of p40 (a–c) and p53 (d–f). The specimens were obtained at 31 years of age (A, D), 36 years and 3 months of age (b and e), and 36 years and 9 months of age (after the transcranial and transsphenoidal dual surgeries)
After the transcranial and transsphenoidal dual surgeries, the patient received chemotherapy[25] consisting of docetaxel (75 mg per body surface squared), cisplatin (100 mg per body surface squared), and fluorouracil (1000 mg per body surface squared) (TPF chemotherapy). The tumor has been well controlled for more than 12 months after surgery.
DISCUSSION
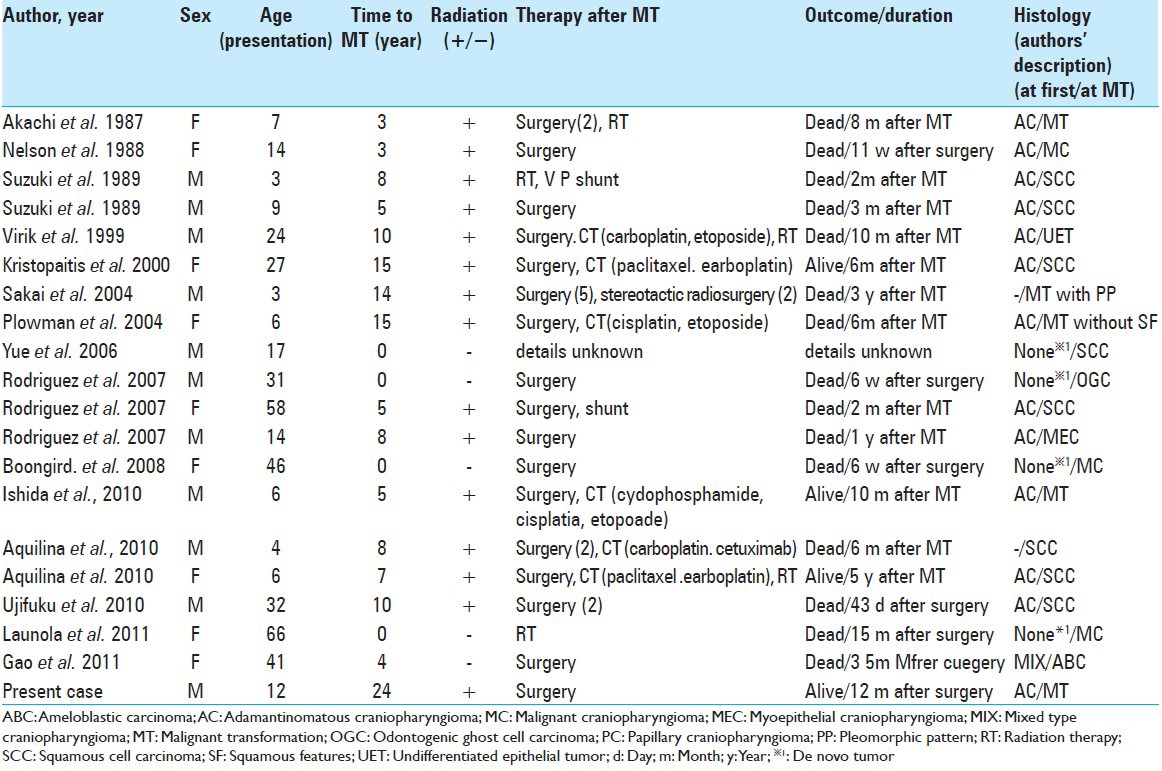
A craniopharyngioma is typically a pathologically benign tumor with no malignant features; malignant craniopharyngioma is quite rare. According to the World Health Organization (WHO) classification of tumors of the central nervous system published in 2007,[19] “malignant transformation of craniopharyngioma to squamous carcinoma after irradiation is exceptual.” To our knowledge, only 20 craniopharyngioma cases with malignant features (or transformation) have been reported [Table 1].[1,2,4,15,16,17,22,24,26,27,30,32,33,35] Excluding four de novo cases, the male to female ratio is 11:9, the mean age of onset is 21.3 years (range, 6–66 years), and the mean duration from the first operation to malignant transformation is 9 years (range, 3–24 years). Fifteen of the 20 cases (75%) had a history of radiation therapy, which suggests that radiation may be a strong inducer of malignant transformation. In our case, the patient had received two previous radiation treatments, and malignant changes occurred 4 months after CyberKnife surgery. However, de novo malignant craniopharyngiomas can occur in the absence of prior radiation,[4,17,26,35] then the etiology of the transformation remains obscure.
Table 1.
Summary of the reported 20 cases of malignant transformation of craniopharyngioma
There are no clear definitions of malignant craniopharyngiomas in previous reports. As summarized by Gao et al.,[13] the characteristics of malignant craniopharyngioma include a high proliferative index and high mitotic activity and histologic features such as destruction of the basement membrane, infiltrative growth, and coagulative necrosis. Because the present case included malignant histological findings such as large nuclei, clarification of the nucleolus, parakeratosis, and intercellular bridges, it was diagnosed as malignant craniopharyngioma. For management of suprasellar tumors with malignancy, some infrequent patterns of tumor should be considered. Chang et al.[7] reported a case of a recurrent olfactory neuroblastoma invading the brain base, in which focal components of craniopharyngioma were found. They suggest that this is an example of a neoplasm with a single origin that developed histological heterogeneity during progression rather than two distinct neoplasms developing concurrently. Naresh et al.[21] reported similar tumor and considered it as a sinonasal teratocarcinosarcoma. Nishioka et al.[23] described an odontogenic-like neoplasia as a malignant odontogenic tumor without morphological evidence of craniopharyngioma. Adamantinomatous craniopharyngioma histologically resembles some odontogenic tumors but consistently shows odontogenic epithelial differentiation in immunohistochemistry.[23,29] Our case showed the same pathological findings of benign adamantinomatous craniopharyngioma during 20 years without other pathological finding. Therefore, the tumor in our case is not considered to be a teratocarcinosarcoma or an odontogenic tumor.
Pathologically, two principal types of craniopharyngioma are recognized, adamantinomatous and squamous papillary.[11] Most of the reported cases with malignant changes in which the initial diagnosis was adamantinomatous craniopharyngioma, showed malignant squamous epithelial cell components, such as squamous carcinoma cells [Table 1]. Likewise, in our case, the features of adamantinomatous craniopharyngioma disappeared and squamous cell components materialized during malignant transformation. Our case showed squamous metaplasia with cells expressing p40, a specific squamous cell marker.[3] An important issue concerns the origin of the malignantly transformed epithelial cells. Yamada et al.[34] explained the histogenesis of craniopharyngioma as follows: The anterior wall of Rathke's pouch epithelium fails to evolve into the adenohypophysis and transforms into either enamel organs (adamantinomatous) or oral mucosa composed of nonkeratinized squamous epithelium (papillary squamous). The WHO classification of tumors of the central nervous system published in 2007[19] states that adamantinomatous craniopharyngioma is characterized by squamous epithelium disposed in cords, and thus contains “peripheral palisading epithelium,” whereas squamous papillary craniopharyngioma consists of “squamous and well-differentiated non-keratinizing epithelium."[28] Both types may transform to malignant SCC-like tumors.
Possible mechanisms of malignant tumorigenesis in our case are as follows [Figure 7]: (i) The peripheral palisading epithelium of the adamantinomatous craniopharyngioma undergoes transformation; (ii) the squamous cells of a coexisting papillary squamous craniopharyngioma (or a mixed type tumor) undergo transformation; (iii) neighboring normal epithelial cells undergo transformation; and (iv) the adamantinomatous craniopharyngioma hosts a distant metastasis (the tumor to tumor phenomenon). The first two hypotheses fit our findings, and the first is the most plausible. There was no pathological evidence of squamous papillary craniopharyngioma during the long clinical course of the tumor nor were p40-positive cells observed before squamous metaplasia arose. In addition, the possibility of collateral damage from radiation therapy (e.g., a radiation-induced malignant tumor) must be considered.[30,31] Cahan et al.[6] and Menon et al.[20] found that the latency period necessary for malignant transformation was more than 5 years after radiotherapy. In our case, the patient received GKS at 31 years of age and local irradiation at 15 years of age; both treatments are potential triggers of transformation. An otherwise benign craniopharyngioma may occasionally serve as the “recipient” in rare tumor-to-tumor metastasis situations [Figure 7d]. Fraggetta et al.[12] reported a case with metastasis of pulmonary adenocarcinoma to the craniopharyngioma. Although we did not find any other malignant tumors in our case, we must always consider the tumor-to-tumor phenomenon.
Figure 7.
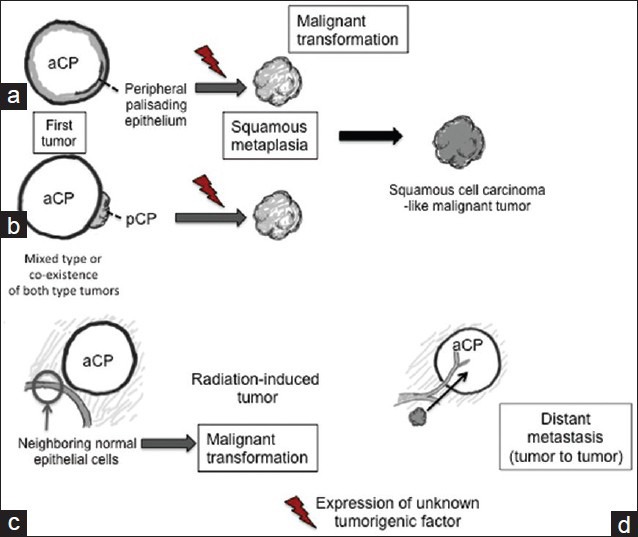
Diagram of the possible mechanisms of craniopharyngioma transformation. (a) The peripheral palisading epithelium of an adamantinomatous craniopharyngioma (aCP) undergoes transformation. (b) The squamous cells of a coexisting papillary squamous craniopharyngioma (pCP) or a mixed-type tumor undergo transformation. (c) Neighboring normal epithelial cells undergo transformation. (d) A distant metastasis invades an aCP
The prognosis of malignantly transformed craniopharyngioma is very poor [Table 1]. After diagnosis of malignant transformation, surgical resection, additional radiation, and chemotherapy have been administered. Although none of these treatments individually resulted in long-term survival, the combination of surgical resection and chemotherapy is now considered the best treatment. All chemotherapies for malignant craniopharyngioma included platinum, and three of six (50%) patients receiving combination therapy are still alive at present. For these reasons, we administered TPF chemotherapy[25] to our patient, but its long-term effect is unknown.
It is unclear whether radical surgery is better than other types of surgery for resection of craniopharyngiomas. Although mortality and morbidity rates after radical surgery for tumors surrounding the cavernous sinus are relatively high, Couldwell et al.[8] recommend radical resection of such tumors in the following situations: (i) Benign tumors recur despite all reasonable medical and radiation therapies, including stereotactic radiosurgery and fractionated radiation; (ii) as a salvage therapy for malignant tumors for which no other therapy is reasonable; and (iii) the patient is in an acceptable neurologic and general physiologic condition for attempts to extend survival. Because our patient had complete paresis of all nerves related to the cavernous sinus, we performed a radical tumor resection including the cavernous sinus using both transcranial and transsphenoidal techniques and an EC-IC bypass. The surgery completely removed the tumor, and there has been no tumor regrowth. It is now 12 months after surgery, and our patient has not manifested any new neurological deficits. The management of malignant transformation of craniopharyngioma is currently unclear and controversial in terms of how best to remove the tumor and which type of chemotherapy is the most effective. Because radiation may be a strong inducer of malignant transformation, we suggest that radical removal of the craniopharyngioma and avoidance of radiation therapy may be the best options.
ACKNOWLEDGMENTS
The authors thank Ms. Keiko Suematsu for technical assistance. This work was supported by Grants-in-Aid for Scientific Research from the Ministry of Education, Sports, Science, and Culture of Japan. There are no conflicts of interest. The authors would like to thank Editage (www.editage.jp) for English language editing.
Footnotes
Available FREE in open access from: http://www.surgicalneurologyint.com/text.asp?2015/6/1/50/154274
Contributor Information
Tetsuya Negoto, Email: emptydoughnut@gmail.com.
Kiyohiko Sakata, Email: kiyo@med.kurume-u.ac.jp.
Takachika Aoki, Email: takachi@med.kurume-u.ac.jp.
Kimihiko Orito, Email: orito_kimihiko@kurume-u.ac.jp.
Shinji Nakashima, Email: nakashima_shinji@med.kurume-u.ac.jp.
Masaru Hirohata, Email: hiroha@med.kurume-u.ac.jp.
Yasuo Sugita, Email: sugita_yasuo@med.kurume-u.ac.jp.
Motohiro Morioka, Email: mmorioka@med.kurume-u.ac.jp.
REFERENCES
- 1.Akachi K, Takahashi H, Ishijima B, Nakamura Y, Oda M, Takizawa T, et al. Malignant changes in a craniopharyngioma. No Shinkei Geka. 1987;15:843–8. [PubMed] [Google Scholar]
- 2.Aquilina K, Merchant TE, Rodriguez-Galindo C, Ellison DW, Sanford RA, Boop FA. Malignant transformation of irradiated craniopharyngioma in children: Report of 2 cases. J Neurosurg Pediatr. 2010;5:155–61. doi: 10.3171/2009.9.PEDS09257. [DOI] [PubMed] [Google Scholar]
- 3.Bishop JA, Teruya-Feldstein J, Westra WH, Pelosi G, Travis WD, Rekhtman N. p40 (ΔNp63) is superior to p63 for the diagnosis of pulmonary squamous cell carcinoma. Mod Pathol. 2012;25:405–15. doi: 10.1038/modpathol.2011.173. [DOI] [PubMed] [Google Scholar]
- 4.Boongird A, Laothamatas J, Larbcharoensub N, Phudhichareonrat S. Malignant craniopharyngioma; Case report and review of the literature. Neuropathology. 2009;29:591–6. doi: 10.1111/j.1440-1789.2008.00986.x. [DOI] [PubMed] [Google Scholar]
- 5.Bunin GR, Surawicz TS, Witman PA, Preston-Martin S, Davis F, Bruner JM. Descriptive epidemiology of craniopharyngioma. J Neurosurg. 1998;89:547–51. doi: 10.3171/jns.1998.89.4.0547. [DOI] [PubMed] [Google Scholar]
- 6.Cahan WG, Woodard HQ. Sarcoma arising in irradiated bone; Report of 11 cases. Cancer. 1948;1:3–29. doi: 10.1002/1097-0142(194805)1:1<3::aid-cncr2820010103>3.0.co;2-7. [DOI] [PubMed] [Google Scholar]
- 7.Chang KC, Jin YT, Chen RM, Su LJ. Mixed olfactory neuroblastoma and craniopharyngioma: An unusual pathological finding. Histopathology. 1997;30:378–82. doi: 10.1046/j.1365-2559.1997.d01-615.x. [DOI] [PubMed] [Google Scholar]
- 8.Couldwell WT, MacDonald JD, Taussky P. Complete Resection of the cavernous sinus-indications and technique. World Neurosurg. 2014;82:1264–1270. doi: 10.1016/j.wneu.2013.08.026. [DOI] [PubMed] [Google Scholar]
- 9.Cushing H. springfield, illinois: 1932. The craniopharyngiomas. In: Intracranial tumors. Notes upon a series of two thousand verified cases with surgical mortality percentages pertaining thereto; pp. 93–8. [Google Scholar]
- 10.Erdheim J. Ueber hypophysengangsgeschwulste und hirncholesteratome. Akad Wiss Wien. 1904;113:537–726. [Google Scholar]
- 11.Fernandez-Miranda JC, Gardner PA, Snyderman CH, Devaney KO, Strojan P, Suárez C, et al. Craniopharyngioma: A pathologic, clinical, and surgical review. Head Neck. 2012;34:1036–44. doi: 10.1002/hed.21771. [DOI] [PubMed] [Google Scholar]
- 12.Fraggetta F, Galia A, Grasso G, D’Arrigo C, Cristaudo C, Giangaspero F. Pulmonary adenocarcinoma metastatic to pituitary craniopharyngioma. J Clin Pathol. 2000;53:946–7. doi: 10.1136/jcp.53.12.946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gao S, Shi X, Wang Y, Qian H, Liu C. Malignant transformation of craniopharyngioma: Case report and review of the literature. J Neurooncol. 2011;103:719–25. doi: 10.1007/s11060-010-0407-2. [DOI] [PubMed] [Google Scholar]
- 14.Garnett MR, Puget S, Grill J, Sainte-Rose C. Craniopharyngioma. Orphanet J Rare Dis. 2007;10:2–18. doi: 10.1186/1750-1172-2-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ishida M, Hotta M, Tsukamura A, Taga T, Kato H, Ohta S, et al. Malignant transformation in craniopharyngioma after radiation therapy: A case report and review of the literature. Clin Neuropathol. 2010;29:2–8. doi: 10.5414/npp29002. [DOI] [PubMed] [Google Scholar]
- 16.Kristopaitis T, Thomas C, Petruzzelli GJ, Lee JM. Malignant craniopharyngioma. Arch Pathol Lab Med. 2000;124:1356–60. doi: 10.5858/2000-124-1356-MC. [DOI] [PubMed] [Google Scholar]
- 17.Lauriola L, Doglietto F, Novello M, Signorelli F, Montano N, Pallini R, et al. De novo malignant craniopharyngioma: Case report and literature review. J Neurooncol. 2011;103:381–6. doi: 10.1007/s11060-010-0382-7. [DOI] [PubMed] [Google Scholar]
- 18.Lindholm J, Nielsen EH. Craniopharyngioma: Historical notes. Pituitary. 2009;12:352–9. doi: 10.1007/s11102-008-0165-8. [DOI] [PubMed] [Google Scholar]
- 19.Louis DN, Ohgaki H, Wiestler OD, Cavenee WK, Burger PC, Jouvet A, et al. The 2007 WHO classification of tumours of the central nervous system. Acta Neuropathol. 2007;114:97–109. doi: 10.1007/s00401-007-0243-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Menon GI, Nair S, Rajesh BJ, Rao BR, Radhakrishnan VV. Malignant astrocytoma following radiotherapy for craniopharyngioma. J Cancer Res Ther. 2007;3:50–2. doi: 10.4103/0973-1482.31974. [DOI] [PubMed] [Google Scholar]
- 21.Naresh KN, Pai SA. Foci resembling olfactory neuroblastoma and craniopharyngioma are seen in sinonasal teratocarcinosarcomas. Histopathology. 1998;32:84. doi: 10.1046/j.1365-2559.1998.0241a.x. [DOI] [PubMed] [Google Scholar]
- 22.Nelson GA, Bastian FO, Schlitt M, White RL. Malignant transformation in craniopharyngioma. Neurosurgery. 1988;22:427–9. doi: 10.1227/00006123-198802000-00029. [DOI] [PubMed] [Google Scholar]
- 23.Nishioka H, Shibuya M, Izawa H, Ikeda Y. Primary suprasellar malignant tumor with odontogenic features: Case report. Neurosurgery. 2009;65:E380–2. doi: 10.1227/01.NEU.0000349923.24247.D1. [DOI] [PubMed] [Google Scholar]
- 24.Plowman PN, Besser GM, Shipley J, Summersgill B, Geddes J, Afshar F. Dramatic response of malignant craniopharyngioma to cisplatin-based chemotherapy. Should craniopharyngioma be considered as a suprasellar ‘germ cell’ tumour? Br J Neurosurg. 2004;18:500–5. doi: 10.1080/02688690400012400. [DOI] [PubMed] [Google Scholar]
- 25.Posner MR, Hershock DM, Blajman CR, Mickiewicz E, Winquist E, Gorbounova V, et al. Cisplatin and fluorouracil alone or with docetaxel in head and neck cancer. N Engl J Med. 2007;357:1705–15. doi: 10.1056/NEJMoa070956. [DOI] [PubMed] [Google Scholar]
- 26.Rodriguez FJ, Scheithauer BW, Tsunoda S, Kovacs K, Vidal S, Piepgras DG. The spectrum of malignancy in craniopharyngioma. Am J Surg Pathol. 2007;31:1020–8. doi: 10.1097/PAS.0b013e31802d8a96. [DOI] [PubMed] [Google Scholar]
- 27.Sakai K, Tanaka Y, Hongo K, Tada T, Shigeta H, Kobayashi S. Treatment of craniopharyngiomas in children. No Shinkei Geka. 2004;32:345–53. [PubMed] [Google Scholar]
- 28.Sarah JL, Olfar A. Pathology and pathogenesis of craniopharyngioma. Pituitary. 2013;16:9–17. doi: 10.1007/s11102-012-0418-4. [DOI] [PubMed] [Google Scholar]
- 29.Sekine S, Takata T, Shibata T, Mori M, Morishita Y, Noguchi M, et al. Expression of enamel proteins and LEF1 in adamantinomatous craniopharyngioma: Evidence for its odontogenic epithelial differentiation. Histopathology. 2004;45:573–9. doi: 10.1111/j.1365-2559.2004.02029.x. [DOI] [PubMed] [Google Scholar]
- 30.Suzuki F, Konuma I, Matsumoto M, Aoki M, Hayakawa I. Craniopharyngioma with malignant transformation—A report of two cases. Gan No Rinsho. 1989;35:723–8. [PubMed] [Google Scholar]
- 31.Tanaka S1, Nishio S, Morioka T, Fukui M, Kitamura K, Hikita K. Radiation-induced osteosarcoma of the sphenoid bone. Neurosurgery. 1989;25:640–3. doi: 10.1097/00006123-198910000-00021. [DOI] [PubMed] [Google Scholar]
- 32.Ujifuku K, Matsuo T, Takeshita T, Hayashi Y, Hayashi K, Kitagawa N, et al. Malignant transformation of craniopharyngioma associated with moyamoya syndrome. Neurol Med Chir (Tokyo) 2010;50:599–603. doi: 10.2176/nmc.50.599. [DOI] [PubMed] [Google Scholar]
- 33.Virik K, Turner J, Garrick R, Sheehy JP. Malignant transformation of craniopharyngioma. J Clin Neurosci. 1999;6:527–30. doi: 10.1016/s0967-5868(99)90019-x. [DOI] [PubMed] [Google Scholar]
- 34.Yamada H, Haratake J, Narasaki T, Oda T. Embrtonal Craniopharyngioma. Case report of the morphogenesis of a craniopharyngioma. Cancer. 1995;75:2971–7. doi: 10.1002/1097-0142(19950615)75:12<2971::aid-cncr2820751227>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- 35.Yue Y, Da JP. Malignant transformation of craniopharyngioma: A case report. Zhonghua Bing Li Xue Za Zhi. 2006;35:439. [PubMed] [Google Scholar]


