Abstract
Introduction and Objective:
Perception is the most important predictor of behavior and there is a strong relation and correlation between behavior and believes. Thus, to improve self-care behaviors of patients, it is required to fully understand their perceptions about behavior. This paper aimed to assess the prediction power of health promotion model of systolic blood pressure (SBP) as the result of self-care behavior in rural hypertensive.
Methods:
This cross-sectional study has been carried out through random multistage sampling on 671 rural patients under the coverage of health center of Ardebil city in 2013. Data were collected through reliable and valid questionnaire based on the health promotion model in eight sectors. For data analysis, Pearson correlation statistical tests, multivariate linear regression, ANOVA and independent t-test were used and for confirmatory factor analysis, SPSS 18 and AMOS 18 (SPSS Inc., Chicago, IL, USA) were used.
Results:
The results showed significant negative correlation between self-efficacy, perceived benefits, situational influences, affects related to behavior and commitment to action structures with SBP and showed a positive significant correlation between perceived barriers and SBP. Furthermore, age and body mass had direct significant relation with SBP. The age of patients showed inverse significant correlation with self-efficacy, perceived benefits, affects related to behavior, interpersonal influences and commitment and showed a direct significant correlation with perceived barriers, means that by increase of age, the perceived barriers also increased. The structures of health promotion model have in overall the prediction power of 71.4% of SBP changes.
Conclusion:
The diet perceptions of patients, the same as health promotion model, has good predictive power of SBP, especially the structures of perceived benefits and self-efficacy have inverse meaningful relation with systole blood pressure and predicted a higher percentage of this variable.
Keywords: Disease, food, high blood pressure, Pender health promotion model
INTRODUCTION
Cardiovascular disease is the main reason for more than 30% of death and mortality in the world and high blood pressure has been mentioned as one of most important risk factors.[1] High blood pressure is not only considered a risk factor for cardiovascular disease, it is also a worrying health problem, which has great effects on public health and big economic consequences[2] and is generally mentioned as the cause of 13% of world’ death.[3] The risk of blood pressure increase has been estimated 90% in lifetime[4] and more than one-third of Patients with prehypertension progress to hypertension over a period of 4 years.[5] World health organization and most scientific institutions have introduced control of high blood pressure as a cost-effective method to reduce morbidity and mortality.[6] Thus, self-care strategies have been considered as the requirements for prediction of high blood pressure and good diet has been considered as one of the corrective actions of lifestyle and one of the necessary approaches for controlling the whole processes of high blood pressure.[7] The introduced factors, as the causes of this disease, can be modified with self-care strategies.[8] The importance of self-care in blood pressure control does not need to be proved. In fact, control of blood pressure will not be possible through drug therapy in individuals without self-care.[9] Self-care is an effective way for reducing the burden of cardiovascular disease in individual and social levels.[10] However, unfortunately, the self-care status is not good at all in individuals suffering from high blood pressure and just 20% of patients accepted and acted based on the diet advices for reducing salt consumption[11] and various studies indicated wrong diet habits.[12,13] Despite the significance of self-care, no project has been done in Iran for increasing self-care.[14]
Self-care is an organized function which is done purposefully by the individual with the aim of preserving life, health, and welfare. Self-care is an outcome-oriented and objective-based behavior which is acquired under the influence of sociocultural conditions and is affected by the individuals’ values and opinions.[15] Thus, one of the effective elements on self-care behavior is the opinions and judgments of individuals. The evidences have proven the significance of opinions and believe in emergence of behavior and introduced unhealthy behaviors as the main cause of high blood pressure.[8] This is easy to believe that perceptions are among the main predictors of behavior.[16] Thus, to improve the self-care behaviors including reduction of received sodium in this group of patients it is required to fully understand their perceptions toward the related behavior.[17] However, unfortunately and surprisingly, in Iran and especially rural areas, there is little information about patients’ perceptions of this disease. Thus, in this study, to investigate the rural patients’ perceptions, the advised diet for patients with high blood pressure was used and a theoretical framework was selected. Some of the patterns including theory of programmed behavior and self-care theory (SCT) by Peters were used which had not good prediction power.[8] The considered framework for this study is the pattern of health promotion which was first proposed by Pander.[18] Pender explains this model as a framework and a guide for discovering complex psychological processes, which motivates individuals to change their behavior, and leads them to promotion of health and hygiene.[19] In addition to internal cognitive processes, this pattern investigates other effective factors on the behavior of individual including interpersonal relation and situational effects and individuals’ previous experiences concerning the behavior[19] which seems to be recommended for diet behavior of patients suffering from high blood pressure with various experiences of preserving the recommended diet.
This model is one of the most comprehensive and predictive patterns of health promotion behaviors, which provides theoretical framework for discovering effective factors on health promoting behavior. It has been considered as a framework for explaining the lifestyle behaviors promoting health.[20] The health promotion model includes three groups of factors, individual characteristics and experiences including two structures: (1) Previous related behaviors and personal factors, (2) behavior specific cognitions and affect which are indicative of the main and most important behavioral motivation and outcomes of behavior.[20] The structures of this pattern include self-efficacy, perceived benefits and barriers, affects related to behavior, interpersonal influences, situational influences, commitment toward the behavior, preferences and immediate competitors.[19] According to our information, no study has investigated the patients’ perceptions and prediction of the variable of behavior based on health promotion pattern in this disease in Iran and other countries. We assume that, as this pattern is a proper predictor for behaviors like use of auditory protection devices[21] and physical activity;[22,23] it has good power for prediction of patients with high blood pressure. However, the patients’ behavior has not been considered in this study and the result of self-care behavior, which is blood pressure, has been investigated. Since, the measuring and evaluation of diet behavior is self-reporting and there is the probability of intended and unintended measurement error, the blood pressure of patients can be used as the result of self-care and precise measurement. To this end, the wide distribution of patients in various ages has been used in two controlled and uncontrolled groups. On the other hand, the investigation of the relation of structures and the result of behavior is in fact a hypothesis being tested in this paper and is also considered as innovation. Thus, in this study the relation between the structures of health promotion model and systolic blood pressures (SBPs) has been investigated in rural hypertensive patients.
METHODS
This cross-sectional study has been done in 2013; the statistical population of the study includes all rural patients suffering from high blood pressure in Ardebil city. Through simple random multistage method, 671 patients were selected and included in the study. The inclusion criteria include: Certain diagnosis of hypertension by physician, having profile in medical and health centers, not suffering from chronic side-effects and other chronic diseases, age between 35 and 60 years, having the literacy to read and write, willingness to participate in the study, not suffering from special mental and emotional diseases (concerning their medical profiles) and not needing certain diet due to any reason; and the exclusion criterion was unwillingness to continue participation in this study.
For data collection, a questionnaire was used including eight sections: (1) Demographic specification questions, (2) perceived benefits (nine questions in form of two ranges based on Likert attitude scale (completely agree, agree, disagree, and completely disagree) which are given 1–4 scores), (3) perceived barriers (ten questions in form of two ranges based on Likert attitude questionnaire (completely agree, agree, disagree, and completely disagree) which are given 1–4 scores), (4) self-efficacy (ten questions based on 10 items scale which are given score 1–10), (5) affects related to behavior (eight questions based on five-point Likert attitude scale (always, usually, often, rarely, and never) which are given scores 1–5), (6) interpersonal influences (nine questions based on 5-rank scale investigating social support of spouse, which are given score 1–5), (7) situational influences (seven 5-scale questions including always, usually, often, rarely and never) which are given scores 1–5), (8) commitment to plan (nine questions based on five points scale (always, usually, often, rarely, and never) which are given scores 1–5). The face validity of questionnaire was confirmed by eleven experts in health education and promotion, diet and physician and the content validity was confirmed by content validity ration and content validity index indices. The reliability of questionnaire was calculated through internal homogeneity and Cronbach’ Alpha and the values of these coefficients for every structure were calculated. The highest alpha was related to perceived self-efficacy (0.96), and the lowest to perceived benefits (0.85). It was 0.92, 0.86, 0.85, and 0.89 for perceived barriers, affects related to behavior, commitment to plan, interpersonal, and situational influences, respectively.
Data from patients have been collected through face-to-face interview by trained health workers of each rural health center which patients trust and preserving moral considerations, conscious contest of patients before entering the study and not inclusion of individuals specification and names in questionnaires, based on coordination with executive and scientific units of Ardebil Medical Sciences University.
Data analysis was done using SPSS-18. Pearson statistical tests were used for testing the correlation between blood pressure and quantitative variables including the mean score of the structures of the model and the age of patients. Multiple linear regressions was used for prediction of SBP and the Health Promotion Model (HPM). ANOVA and independent t-test were used for comparison of SBP in two groups and more than two groups like gender and education. Confirmatory factor analysis and the models’ path analysis were used for predictability of SBP in the studied group through AMOS-18. Generalized least square was used for investigation of the fitness of structural model. To assess the efficacy of model Chi-square goodness of fit, the ratio of Chi-square to degree of freedom, goodness of fit index (GFI), adjusted goodness of fit index (AGFI), normed fit index (NFI), comparative fit index (CFI), and the root mean square error of approximation RMSE were used which are recommended for proper fit. The ratio of Chi-square statistic to degrees of freedom should be <3, AGFI should be >0.8, NFI, CFI, GFI should be >0.9 and the root mean square errors should be <0.8.[24]
RESULTS
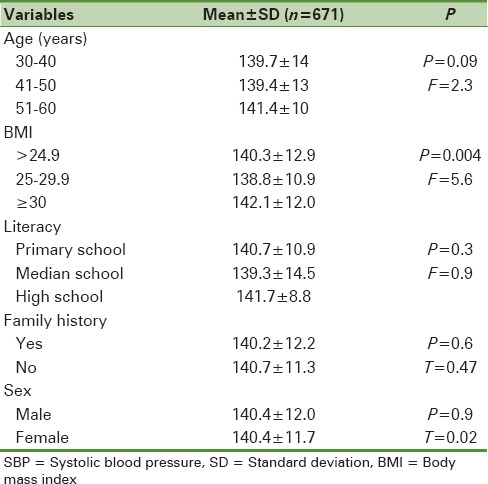
About 74.8% of respondents were female, the mean and standard deviation of patients’ age was 50.2 ± 6.4 years, and the duration of suffering from hypertension was 4.0 ± 5.9. The majority of individuals, i.e. 75.9% (509 individuals) had elementary school degree, mean BMI in samples was 29.2 [Table 1]. In this study, no significant difference was seen in the SBP between age groups, education, family experience and gender (P > 0.05), however, individuals with BMI higher than 30 had significantly higher SBP than others (P < 0.001) [Table 2].
Table 1.
Socio-demographic characteristics of the study sample
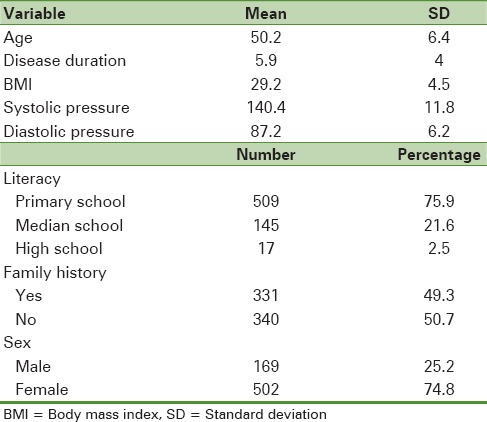
Table 2.
Mean of SBP based on demographic characteristics
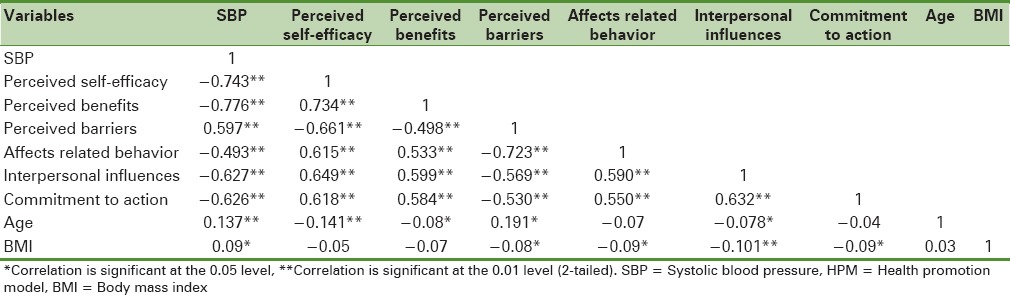
The mean and standard deviation of perceived benefits concerning dietary behavior was 29.1 ± 4.5, perceived barriers was 23.6 ± 7.7, self-efficacy was 23.9 ± 45.8, situational influences was 27.5 ± 6.2, interpersonal influences was 25.9 ± 6.1, commitment to plan was 33.5 ± 6.8, affects related to behavior was 29.1 ± 6.8. The results showed significant negative correlation between self-efficacy, perceived benefits, situational influences, affects related to behavior and commitment to action structures with SBP and showed a positive significant correlation between perceived barriers and SBP.
Furthermore, age and body mass index showed direct significant relation with SBP. In this study, the age of patients shows inverse correlation with self-efficacy, perceived benefits, affects related to behavior; commitment and interpersonal influences and a direct significant correlation with perceived barriers, meaning that increase of age increase the perceived barriers [Table 3].
Table 3.
Pearson correlation coefficient between HPM constructs and SBP
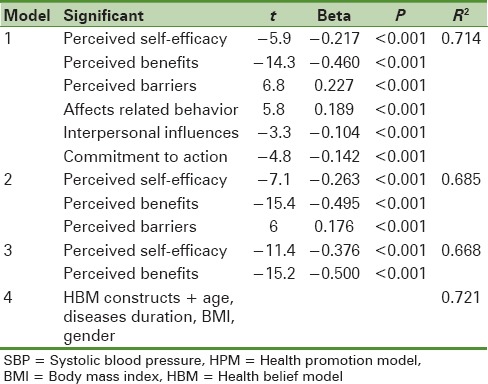
In this study, the results obtained from multiple linear regression showed that the structures of health promotion model have collectively been able to predict 71.4% of changes in SBP and by exclusion of commitment, interpersonal influences and affects related to behavior, this ability was 68.5%. In third model, the self-efficacy and perceived benefits had the prediction power of 66.8% of variation of target variable. By adding all structures and demographic variables such as age, diseases duration, body mass index and gender in regression model, the power of 72.1% was shown [Table 4].
Table 4.
Multiple linear regression of HPM constructs in SBP prediction
In this study, for determining the predictability of model structures concerning blood pressure, path analysis with maximum likelihood estimation was used. Based on expressed paths by related indices presented in Table 5 (df = 1, P = 0.31) and modified indices based on scientific evidences, some paths for improvement of model's fit was asserted and the results showed that the final model [Figure 1] has good fit.
Table 5.
Structural equation modeling fitness based on the HPM constructs on SBP prediction
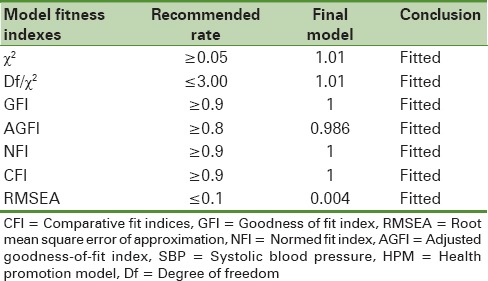
Figure 1.
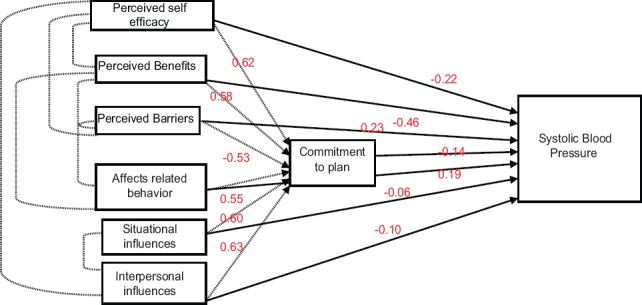
Standardized estimations based on final model
DISCUSSION
As far as we know, this is the first study on prediction of blood pressure in rural patient and its relation with perception within the framework of HPM constructs and provides important information which can be helping in designing systematic interventions in controlling the disease in target group. Change of lifestyle and self-care are the first advises for control of high blood pressure to patients[7] which are to some extent influenced by the opinions and perceptions of patients from disease, related behavior and social-cultural group.[15]
In this study, the structures of model were able to predict 71.4% of changes in SBP which can be considered a significant figure. This finding is in line with those studies which make the significance of perceptions in self-care clear, self-care affects blood pressure thus perceptions are related with the final outcome of behavior. However, it is incompatible and inconsistent with Peter study where the opinions and attitudes were not able to predict blood pressure. This finding might be due to limited sample size (206 participants) and minimum difference in blood pressure of their studied group. Furthermore, in that study, there was a mutual relation between blood pressure and self-care behavior.[8] Thus, the selection of proper number of samples with good dispersion of blood pressure in the present study leads to good fit of the model and prediction of a significant amount of target variable. It might be that other causes of the obtained result include the presence of perceived barriers and benefits, interpersonal influences and situational influences of structures in the Pender's HPM; where the pattern of planned behavior and self-care theory do not exist. In addition, the presences of these structures, which investigate the environmental situations and interpersonal influences, in addition to individual's inner perceptions have been the strength points for obtaining results.
The perceived barriers in this study have been almost high and had direct meaningful relation with blood pressure, i.e. by increase of blood pressure the perceived barriers also increase and in the model 1, it was able to predict 22% of variations of target variable. Perceived barriers are the main predictors of behavior and their significance become clear in the studies. Thus, it provides familiarization with barriers, potential awareness for change of behavior and helps in preparation for beginning and continuing the healthy behaviors. Knowledge of barriers and benefits can be effective for promotion of care and following the provided advises for prevention of cardiovascular diseases.[10] Due to lack of similar studies, those studies investigating perceived barriers of diet self-care behaviors including reduction of sodium were used. The reason is that there is direct and meaningful relation between reduction of received salt and reduction of blood pressure and consequently reduction of cardiovascular disease risk due to high blood pressure.[25,26] Moreover, the proposed strategies for sodium reduction are focused on the motivation of patients toward the behavior.[17] Furthermore, in Cornélio study lack of motivation for correcting diet behavior in this group of patients was introduced as a barrier on the way of healthy behavior.[27] From the studies which selected Pender model as their framework, 79% expressed experimental support for significance of barriers as the determiners of behavior. Barriers might be real or imaginary. They include imaginations related to inaccessibility, inappropriateness or an action being expensive or time-consuming. Barriers are usually considered as dams or personal costs due to certain behavior. Behavioral barriers lead to avoidance or reduction of health promotion behaviors.[28]
Perceived barriers have a great role in diet especially in reduction of received salt. These barriers include individuals’ unwillingness to reduce salt in food such in Newson study one-third of individuals were unwilling to reduce salt.[17] Some individuals have improper attitude toward reduction of received salt and assume that by reducing salt consumption, their physical power decreases[29] and a significant number of individuals add salt to food before knowing the test of food.[17] Thus, in some cases, just knowing the advantages of low-salt regime can help individuals reduce their salt consumption. In Smith study, reduction of salt consumption was difficult for most respondents, especially in men and they believed that salt is the flavor of food and there is no replacement for it. The more they tried to reduce their salt consumption they again used more than the allowed limit. Some other believed that despite suffering from heart disease, some foods don’t have taste without salt[30] and in Agondi study the main barrier of provided strategies for sodium reduction was unpleasant flavor of low-salt food.[26]
In this study, the interpersonal influences predicts almost 10% of systole blood pressure variation in model 1 which indicates the significance of others in showing or not showing healthy behavior. This is in line with the results of similar studies where family members’ dissatisfaction of low-salt food has been introduced as a barrier for sodium reduction.[26,31] In Aroian study the role of virtual norms, norms and cultural issues has been referred to as effective factor in patients’ behavior and it is argued that paying attention to these factors is important in design and implementation of main interventions.[32] The important point which should be said is that unfortunately, in Iran these factors are not considered and in designing country interventions and executional system, no value is given to them.
Perceptions and believes play a great role in health and hygiene behaviors.[33,34] In Serour study, 63% of individuals at risk of cardiovascular diseases preserved diet advices and the reported barriers include the difficulty of preparing food in two kinds, social norms and unwillingness.[35] False attitude and improper perception of hygienic information are considered as a barrier on health promotion. These discussions make clear the significance of investigating patients’ perception in the realms of these structures, effective reasons and factors on these perceptions. Moreover, it is proposed by comprehensive study of patients’ perceptions and health services providers, especially rural people, the findings of these studies to be used in medical health system for training and improvement of perceptions and to replicate these studies for updating perception of patients and their demands.
The other point extracted from this study and similar studies is that the perceived barrier is a reality in control of high blood pressure and patients realize these barriers well. It is also required to provide proper strategies for individuals’ function and improvement of their diet by getting information about the perceptions of individuals of barriers. Although paying attention to daily experiences is considered required and necessary for designing effective interventions of patients suffering from high blood pressure,[36] it seems that in fact, it has not been considered at least in designing and implementing merged protocol of centers.
In this study, the average blood pressure has no meaningful difference between men and women and different age groups. Concerning variable of gender, this is in line with Lin study where gender had not role in predication of systole blood pressure, however diastole blood pressure was meaningfully higher in men.[37] However, concerning age variable, it contradicts with our findings. The reason might be the age difference of participants of both studies, where the average age of individuals was 76 years. As far as age is considered as a factor in blood pressure variation and by increase of age, blood pressure also increases. On one hand, this contradiction has been seen in the results of studies and in foreign studies, the blood pressure has been reported higher in men[1,38] while in Iranian studies, women are reported as having higher blood pressure.[39] Thus, the social and cultural differences can be a justification for this finding. Ultimately, similar diet pattern and integrated medical and health system in rural areas with the aim of merging prevention program and blood pressure control in health and medical system of the country might lead to lack of difference in individuals’ blood pressure based on demographic variable.
In the present study, by increase of age a meaningful reduction in mean self-efficacy and perceived benefits was obtained which is in line with Miller study where age has meaningful relation with patients’ attitude.[40] The present study, the patients were not in overall in good position in various structures of model and most of them obtained scores below average. Due to the fact that no similar study was found for comparison of findings, we investigated the studies using similar concepts with pattern structures.
In this study, diet self-efficacy of patients was less than half of the achievable score and was dissatisfactory. Self-efficacy is the most common psychological concept used in management of chronic diseases.[41] The significance of self-efficacy is unavoidable in control of this disease such that in Warren study, self-efficacy had strong and direct relation with five self-care behaviors introduced for control of blood pressure.[41] Insuring that this disease is controllable and insuring of our ability to perform the recommended behavior can be effective in increase of probability of effective behavior. Thus, using techniques of self-efficacy increase should be taken into account in training these patients. It might be the case that care providers might wrongly assume that self-efficacy becomes meaningful in complex behaviors; however, the simplest behavior in this disease might be drug therapy. The studies have shown direct relation between self-efficacy and following up of regime therapy.[42]
Self-efficacy is individual's self-judgment of one's ability for organizing and performing behavior. Self-efficacy is not related to individual's skills about behavior, however, it is related to the individual's judgment about what he can do with the skills he has. Individual's perception of abilities and skills in a certain realm motives individuals to perform the behavior that the individual is skillful it.
The feeling of being skillful in performing an action is more likely to motivate and encourage the individual to perform it than the times when the individual feels as being inefficient. 86% of the studies testing health promotion model supported the significance of self-efficacy as a determining factor of health promotion.[43] Self-efficacy could be obtained from previous successful experiences, observing other's success, other's encouragement and individual's physiologic states.[44]
At the end, what was found in this study is that patients have little perceptions of diet behavior related to high blood pressure. In fact, what becomes clear from patients’ responses to some questions about the perceived benefits and barriers like high cost and time consuming of preserving diet, avoidance of favorable foods and the need to cook different foods for healthy diet is that they have improper perceptions in some realms and areas. However, this is not a new finding and different studies have frequently referred to the improper perceptions of patients. For example, in Petrella study about 60% of individuals did not consider high pressure as a disease or health problem and about 59% did not regard themselves as suffering from blood pressure.[45] However, this issue is not related only to patient and considering the patient as the only guilty person might not be good understanding of improper perceptions of individuals and their condition. The reason is that studies have shown that health care providers are required to renew their perceptions of disease[6] and relying on these results, the service providing system and heath care providers might be considered as guilty for wrong perceptions of patients.
The present study is based on the study done in Canada where most caregivers have not new information of the advices for disease and give wrong answers to the basic questions about it.[6] However, the surprising point is that in common medical and health system of the study, no action has been taken for understanding the perceptions of patients and social workers of health center as the individuals having the first and most contact with this group. Thus, the significance of this study is that, it is one of the first studies investigating the perceptions and their predictability power of the result of self-care behavior, which is blood pressure. Thus, we recommend carrying out wider studies on different ethnicities in various countries and cultures to use behavior therapy of these patients in addition to drug therapy so control of this disease might be satisfactory.
The limitations of present study is its being cross-sectional which make it almost difficult to determine its causal relation and failure to investigate the immediate preferences and competitors and hence it is recommended to consider this structure beside other structures concerning the role of desires and temptations in diet self-care. Furthermore, it is recommended to use behavioral change theories for investigations that are used in some studies for increase of predictability of theories.[46] On contrary, path analysis by desired number of samples along with standard devices is considered as the strength of the study. Furthermore, the other strength of this study is that it is done on rural patients suffering from high blood pressure that according to our knowledge, few studies have been done on.
CONCLUSION
Patients’ dietary perceptions in form of HPM constructs had proper predictability of SBP. Especially, the structures of perceived benefits and self-efficacy have significant inverse relation with SBP and a higher percentage of changes predicted by this variable. This pattern can be used in care providing system as an instrument for measuring patients’ perceptions and in designing the interventions for improving self-care and health promoting behaviors.
Footnotes
Source of Support: Ardabil University of Medical Sciences
Conflict of Interest: None declared
REFERENCES
- 1.Rampal L, Rampal S, Azhar MZ, Rahman AR. Prevalence, awareness, treatment and control of hypertension in Malaysia: A national study of 16,440 subjects. Public Health. 2008;122:11–8. doi: 10.1016/j.puhe.2007.05.008. [DOI] [PubMed] [Google Scholar]
- 2.Echouffo-Tcheugui JB, Batty GD, Kivimäki M, Kengne AP. Risk models to predict hypertension: A systematic review. PLoS One. 2013;8:e67370. doi: 10.1371/journal.pone.0067370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mendis S, Puska P, Norrving B. Geneva: World Health Organization; 2011. Global Atlas on Cardiovascular Disease Prevention and Control. [Google Scholar]
- 4.Vasan RS, Beiser A, Seshadri S, Larson MG, Kannel WB, D’Agostino RB, et al. Residual lifetime risk for developing hypertension in middle-aged women and men: The Framingham Heart Study. JAMA. 2002;287:1003–10. doi: 10.1001/jama.287.8.1003. [DOI] [PubMed] [Google Scholar]
- 5.Vasan RS, Larson MG, Leip EP, Kannel WB, Levy D. Assessment of frequency of progression to hypertension in non-hypertensive participants in the Framingham Heart Study: A cohort study. Lancet. 2001;358:1682–6. doi: 10.1016/S0140-6736(01)06710-1. [DOI] [PubMed] [Google Scholar]
- 6.Allu SO, Bellerive J, Walker RL, Campbell NR. Hypertension: Are you and your patients up to date? Can J Cardiol. 2010;26:261–4. doi: 10.1016/s0828-282x(10)70381-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr, et al. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003;42:1206–52. doi: 10.1161/01.HYP.0000107251.49515.c2. [DOI] [PubMed] [Google Scholar]
- 8.Peters RM, Templin TN. Theory of planned behavior, self-care motivation, and blood pressure self-care. Res Theory Nurs Pract. 2010;24:172–86. doi: 10.1891/1541-6577.24.3.172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dickey RA, Janick JJ. Lifestyle modifications in the prevention and treatment of hypertension. Endocr Pract. 2001;7:392–9. doi: 10.4158/EP.7.5.392. [DOI] [PubMed] [Google Scholar]
- 10.Tol A, Shojaeizadeh D, Eshraghian MR, Mohebbi B. Determination of perceived barriers and benefits of adopting health-promoting behaviors in cardiovascular diseases prevention: Application of preventative behavior model. J Tehran Univ Paramed Sch. 2012;6:204–14. [Google Scholar]
- 11.Warren-Findlow J, Seymour RB. Prevalence rates of hypertension self-care activities among African Americans. J Natl Med Assoc. 2011;103:503–12. doi: 10.1016/s0027-9684(15)30365-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sakamaki R, Toyama K, Amamoto R, Liu CJ, Shinfuku N. Nutritional knowledge, food habits and health attitude of Chinese university students - A cross sectional study. Nutr J. 2005;4:4. doi: 10.1186/1475-2891-4-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pirouznia M. The association between nutrition knowledge and eating behavior in male and female adolescents in the US. Int J Food Sci Nutr. 2001;52:127–32. doi: 10.1080/713671772. [DOI] [PubMed] [Google Scholar]
- 14.Sadeghi M, Shiri M, Roohafza H, Rakhshani F, Sepanlou S, Sarrafzadegan N. Developing an appropriate model for self-care of hypertensive patients: First experience from EMRO. ARYA Atheroscler. 2013;9:232–40. [PMC free article] [PubMed] [Google Scholar]
- 15.Orem D. 6th ed. St. Louis: Mosby; 2001. Nursing Concepts of Practice. [Google Scholar]
- 16.Krauss J. Attitudes and the prediction of behavior: A meta-analysis of the empirical literature. Pers Soc Psychol Bull. 1995;21:58–75. [Google Scholar]
- 17.Newson RS, Elmadfa I, Biro G, Cheng Y, Prakash V, Rust P, et al. Barriers for progress in salt reduction in the general population. An international study. Appetite. 2013;71:22–31. doi: 10.1016/j.appet.2013.07.003. [DOI] [PubMed] [Google Scholar]
- 18.Marriner T, Raile AM. 5th ed. St Louis: Mosby; 2005. Nursing Theorists and Their Work. [Google Scholar]
- 19.Pender NJ, Murdaugh CL, Parsons MA. 6th ed. Boston, MA: Pearson; 2011. Health Promotion in Nursing Practice. [Google Scholar]
- 20.Chamberlain B. Health promotion in nursing practice. Clin Nurse Spec. 2007;21:130. [Google Scholar]
- 21.Ronis DL, Hong O, Lusk SL. Comparison of the original and revised structures of the Health Promotion Model in predicting construction workers’ use of hearing protection. Res Nurs Health. 2006;29:3–17. doi: 10.1002/nur.20111. [DOI] [PubMed] [Google Scholar]
- 22.Walker SN, Pullen CH, Hertzog M, Boeckner L, Hageman PA. Determinants of older rural women's activity and eating. West J Nurs Res. 2006;28:449–68. doi: 10.1177/0193945906286613. [DOI] [PubMed] [Google Scholar]
- 23.Choi M. Yongin, Korea: Korean Nurses Association; 2000. Health promotion and physiological effects of exercise. Paper Presented at the Inservise Education Workshop. [Google Scholar]
- 24.Zendehdel M, Paim L. Predicting consumer attitude to use on-line shopping: Context of Malaysia. Life Sci J. 2013;10:497–501. [Google Scholar]
- 25.Elliott P, Walker LL, Little MP, Blair-West JR, Shade RE, Lee DR, et al. Change in salt intake affects blood pressure of chimpanzees: Implications for human populations. Circulation. 2007;116:1563–8. doi: 10.1161/CIRCULATIONAHA.106.675579. [DOI] [PubMed] [Google Scholar]
- 26.Agondi Rde F, Gallani MC, Cornélio ME, Rodrigues RC. Analysis of action plans and coping plans for reducing salt consumption among women with hypertension. Rev Lat Am Enfermagem. 2012;20:486–94. doi: 10.1590/s0104-11692012000300009. [DOI] [PubMed] [Google Scholar]
- 27.Cornélio ME, Gallani MC, Godin G, Rodrigues RC, Mendes RD, Nadruz Junior W. Development and reliability of an instrument to measure psychosocial determinants of salt consumption among hypertensive patients. Rev Lat Am Enfermagem. 2009;17:701–7. doi: 10.1590/s0104-11692009000500017. [DOI] [PubMed] [Google Scholar]
- 28.Blais K, Hayes J, Kozier B. 6th ed. Upper Saddle River, NJ: Prentice Hal; 2010. Professional Nursing Practice: Concepts and Perspectives. [Google Scholar]
- 29.Zhang J, Xu AQ, Ma JX, Shi XM, Guo XL, Engelgau M, et al. Dietary sodium intake: Knowledge, attitudes and practices in Shandong Province, China, 2011. PLoS One. 2013;8:e58973. doi: 10.1371/journal.pone.0058973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Smith SL, Quandt SA, Arcury TA, Wetmore LK, Bell RA, Vitolins MZ. Aging and eating in the rural, southern United States: Beliefs about salt and its effect on health. Soc Sci Med. 2006;62:189–98. doi: 10.1016/j.socscimed.2005.05.009. [DOI] [PubMed] [Google Scholar]
- 31.de Brito-Ashurst I, Perry L, Sanders TA, Thomas JE, Yaqoob MM, Dobbie H. Barriers and facilitators of dietary sodium restriction amongst Bangladeshi chronic kidney disease patients. J Hum Nutr Diet. 2011;24:86–95. doi: 10.1111/j.1365-277X.2010.01129.x. [DOI] [PubMed] [Google Scholar]
- 32.Aroian KJ, Peters RM, Rudner N, Waser L. Hypertension prevention beliefs of Hispanics. J Transcult Nurs. 2012;23:134–42. doi: 10.1177/1043659611433871. [DOI] [PubMed] [Google Scholar]
- 33.Lukoschek P. African Americans’ beliefs and attitudes regarding hypertension and its treatment: A qualitative study. J Health Care Poor Underserved. 2003;14:566–87. doi: 10.1353/hpu.2010.0690. [DOI] [PubMed] [Google Scholar]
- 34.Ford CD, Kim MJ, Dancy BL. Perceptions of hypertension and contributing personal and environmental factors among rural Southern African American women. Ethn Dis. 2009;19:407–13. [PMC free article] [PubMed] [Google Scholar]
- 35.Serour M, Alqhenaei H, Al-Saqabi S, Mustafa AR, Ben-Nakhi A. Cultural factors and patients’ adherence to lifestyle measures. Br J Gen Pract. 2007;57:291–5. [PMC free article] [PubMed] [Google Scholar]
- 36.Bokhour BG, Cohn ES, Cortés DE, Solomon JL, Fix GM, Elwy AR, et al. The role of patients’ explanatory models and daily-lived experience in hypertension self-management. J Gen Intern Med. 2012;27:1626–34. doi: 10.1007/s11606-012-2141-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lin CY, Chen PC, Kuo HK, Lin LY, Lin JW, Hwang JJ. Effects of obesity, physical activity, and cardiorespiratory fitness on blood pressure, inflammation, and insulin resistance in the National Health and Nutrition Survey 1999-2002. Nutrition, metabolism, and cardiovascular diseases: NMCD. 2010 Dec 20;10:713–9. doi: 10.1016/j.numecd.2009.06.005. [DOI] [PubMed] [Google Scholar]
- 38.Mohan V, Deepa M, Farooq S, Datta M, Deepa R. Prevalence, awareness and control of hypertension in Chennai – The Chennai urban rural epidemiology study (CURES-52) J Assoc Physicians India. 2007;55:326–32. [PubMed] [Google Scholar]
- 39.Fakhrzadeh H, Nouri M, Pourebrahim R, Ghotbi S, Hashmat R, Bastanhagh MH. Prevalence of hypertension and risk factors at 25-64aged in population research center, Tehran Medical University. Iran J Diabetes Lipid Disord. 2003;3(1):43–9. [Google Scholar]
- 40.Miller NH, Berra K, Long J. Hypertension 2008 – Awareness, understanding, and treatment of previously diagnosed hypertension in baby boomers and seniors: A survey conducted by Harris interactive on behalf of the preventive cardiovascular nurses association. J Clin Hypertens (Greenwich) 2010;12:328–34. doi: 10.1111/j.1751-7176.2010.00267.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Warren-Findlow J, Seymour RB, Brunner Huber LR. The association between self-efficacy and hypertension self-care activities among African American adults. J Community Health. 2012;37:15–24. doi: 10.1007/s10900-011-9410-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Breaux-Shropshire TL, Brown KC, Pryor ER, Maples EH. Relationship of blood pressure self-monitoring, medication adherence, self-efficacy, stage of change, and blood pressure control among municipal workers with hypertension. Workplace Health Saf. 2012;60:303–11. doi: 10.3928/21650799-20120625-04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Chrisrensen A, WJ, Benotsch E, Lawton W. Perceived health competence, health locus of control, and patient adherence in renal dialysis. Cognit Ther Res. 1996;20:411–21. [Google Scholar]
- 44.Mohamadian H, Eftekhar-Ardebili H, Rahimi A, Taghdisi MH, Shojaiezade D. Evaluation of Pender's health promotion model for predicting adolescent girls’ quality of life. J Sch Public Health Inst Public Health Res. 2011;8:1–14. [Google Scholar]
- 45.Petrella RJ, Campbell NR. Awareness and misconception of hypertension in Canada: Results of a national survey. Can J Cardiol. 2005;21:589–93. [PubMed] [Google Scholar]
- 46.Baranowski T, Cullen KW, Nicklas T, Thompson D, Baranowski J. Are current health behavioral change models helpful in guiding prevention of weight gain efforts? Obes Res. 2003;11(Suppl):23S–43. doi: 10.1038/oby.2003.222. [DOI] [PubMed] [Google Scholar]


