Abstract
We performed a 2-year follow-up survey of 523 patients with peripheral nerve injuries caused by the earthquake in Wenchuan, Sichuan Province, China. Nerve injuries were classified into three types: type I injuries were nerve transection injuries, type II injuries were nerve compression injuries, and type III injuries displayed no direct neurological dysfunction due to trauma. In this study, 31 patients had type I injuries involving 41 nerves, 419 had type II injuries involving 823 nerves, and 73 had type III injuries involving 150 nerves. Twenty-two patients had open transection nerve injury. The restoration of peripheral nerve function after different treatments was evaluated. Surgical decompression favorably affected nerve recovery. Physiotherapy was effective for type I and type II nerve injuries, but not substantially for type III nerve injury. Pharmacotherapy had little effect on type II or type III nerve injuries. Targeted decompression surgery and physiotherapy contributed to the effective treatment of nerve transection and compression injuries. The Louisiana State University Health Sciences Center score for nerve injury severity declined with increasing duration of being trapped. In the first year after treatment, the Louisiana State University Health Sciences Center score for grades 3 to 5 nerve injury increased by 28.2% to 81.8%. If scores were still poor (0 or 1) after a 1-year period of treatment, further treatment was not effective.
Keywords: nerve regeneration, earthquake, peripheral nerve injury, LSUHSC score, compartment syndrome, surgery therapy, physiotherapy, nerve decompression, neural regeneration
Introduction
In recent years, large earthquakes have occurred frequently all over the world (Briggs, 2006; Gautschi et al., 2008; Bayard, 2010; McCunn et al., 2010; Normile, 2011). Earthquakes cause a large number of casualties with their catastrophic force. On May 12, 2008, an earthquake of 8.0-magnitude occurred in Wenchuan, Sichuan Province, China. By May 25, 2008, 68,712 people had died, 374,640 were wounded, and 17,042 were reported missing. On January 12, 2010, a 7.3-magnitude earthquake occurred in Haiti. About 222,000 people died and 196,000 people were wounded. On March 11, 2011, a 9.0-magnitude earthquake and associated tsunami occurred in Japan. By March 25, 8,928 people had died and 12,664 were reported missing.
Focusing on the on-site rescue of earthquake victims, all nations have invested a great deal of staff and resources and have formed various rescue systems (Benson et al., 1996; Crippen, 2001; Peleg et al., 2002; Owens et al., 2005; Sever et al., 2006; Baker, 2007). We participated in the on-site rescue for the earthquake in Wenchuan and saw a large number of patients with peripheral nerve injuries. During the emergency rescue process, these patients did not receive the same on-site care as those with fractures, crush syndrome, head trauma, or injuries to the abdominal organs (Oda et al., 1997; Peek-Asa et al., 1998; Macintyre et al., 2006; Sever et al., 2006; Chen et al., 2009; Salimi et al., 2009; Chunguang et al., 2010; Gu et al., 2010; Li et al., 2010; Shi et al., 2010). However, a long period of time after the earthquake, many patients continued to experience serious peripheral nerve dysfunction, which was accompanied by severe peripheral neuralgia. Subsequently, following the earthquake, priorities shifted, and these patients received less attention than they received at the earthquake rescue site.
While these nerve injuries are not life-threatening, they can affect the long-term quality of life. Studies that have investigated nerve injury resulting from earthquakes have concluded that peripheral nerve injuries are common in disasters such as earthquakes (Yoshida et al., 1999; Uzun et al., 2005; Ahrari et al., 2006). However, because of the limited case numbers, the data have not been systematically analyzed. This paper describes our analysis of nerve injuries due to the earthquake in Wenchuan.
Subjects and Methods
Case acquisition
Mianzhu prefecture, Sichuan Province, China was one of the hardest-hit regions of the earthquake. The hospitals in Mianzhu prefecture were the most important emergency treatment centers for those affected by the Wenchuan earthquake and the only rehabilitation centers available afterward. We surveyed patients in the emergency treatment centers in the surrounding areas of Mianzhu. From weeks 5 to 16 after the earthquake, we collected data on cases of injury due to the earthquake in Mianzhu prefecture. Data were collected for 8,626 patients with confirmed earthquake injuries. This study was approved by the Medical Ethics Committees of the Chinese PLA General Hospital. All patients gave their written informed consent to participate in this study.
Clinical types of nerve injury
Based on the specific on-site nerve damage and injury observed, and in reference to other surveys (Uzun et al., 2005; Ahrari et al., 2006; Uzun et al., 2006), we classified the peripheral nerve injuries into three major types based on the Louisiana State University Health Sciences Center (LSUHSC) score, as follows:
Type I: Nerve transection injuries, a complete severing of nerve continuity.
Type II: Nerve compression injuries, with nerve continuity being present, but with a history of direct peripheral nerve injury.
Type III: No direct neurological dysfunction due to trauma. No limb fractures, dislocations or localized soft tissue wounds, but nerve injuries in certain innervated areas (Figure 1).
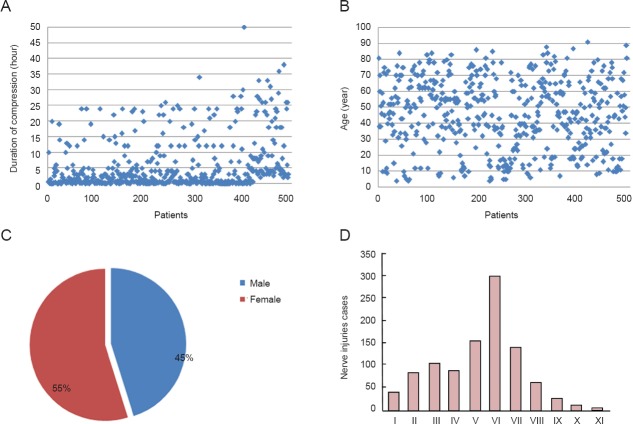
Figure 1.
Results of screening earthquake-caused nerve injuries in victims of the 2008 Wenchuan earthquake.
Patients were examined between weeks 5 and 16 after the earthquake. Subjects with positive results were given a diagnosis of nerve injury. EMG: Electromyography; NCV: nerve conduction velocity.
Survey of patients
Experienced clinicians performed physical examinations to determine the nature of the peripheral nerve injury. We analyzed and graded the injuries according to the LSUHSC Nerve Grading System (Kim et al., 2007). All patients underwent electromyography, and a database of nerve injuries was constructed. Then, patients were surveyed to determine the context of the earthquake injury, including the injury location, soft tissue condition at the time of injury, time between the injury and rescue, and treatment (surgery, physical therapy, and vitamin B12). The follow-up was 1 to 2 years after the initial information collection.
Statistical analysis
The Chi-square test was used for data analysis. Correlations were analyzed with Spearman correlation coefficient (rho, ρ). A P level of < 0.05 was considered statistically significant.
Results
Incidence of nerve injury
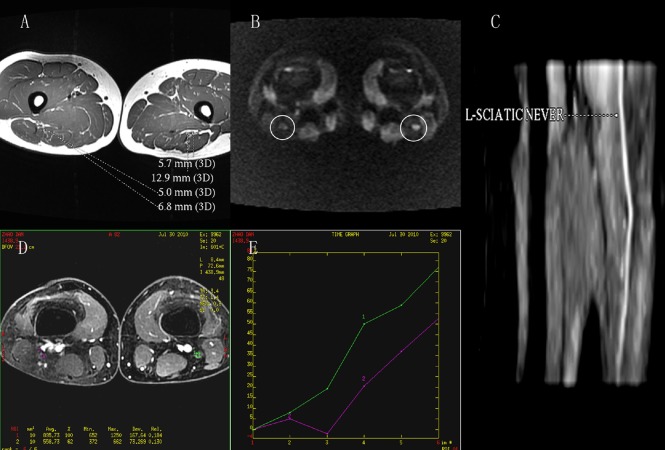
We surveyed 8,626 patients with confirmed earthquake injuries, and of these 571 had peripheral nerve injuries (including 257 males, 45%). At 2 years, 12% of the patients were lost to follow-up. We obtained continuous data for 503 patients, and their nerve injury characteristics are shown in Table 1 and Figure 2. Among these patients, 31 had type I injuries involving 41 nerves, 419 had type II injuries involving 823 nerves, and 73 had type III injuries involving 150 nerves.
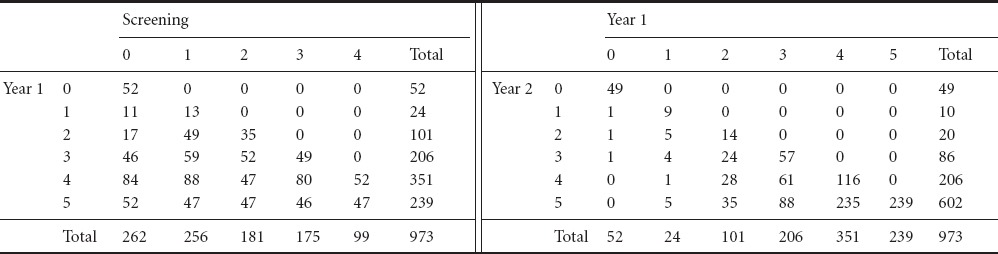
Table 1.
Distribution (n) of injury in peripheral nerves among victims of the 2008 Wenchuan earthquake using the 5-point Louisiana State University Health Sciences Center (LSUHSC) Nerve Grading System
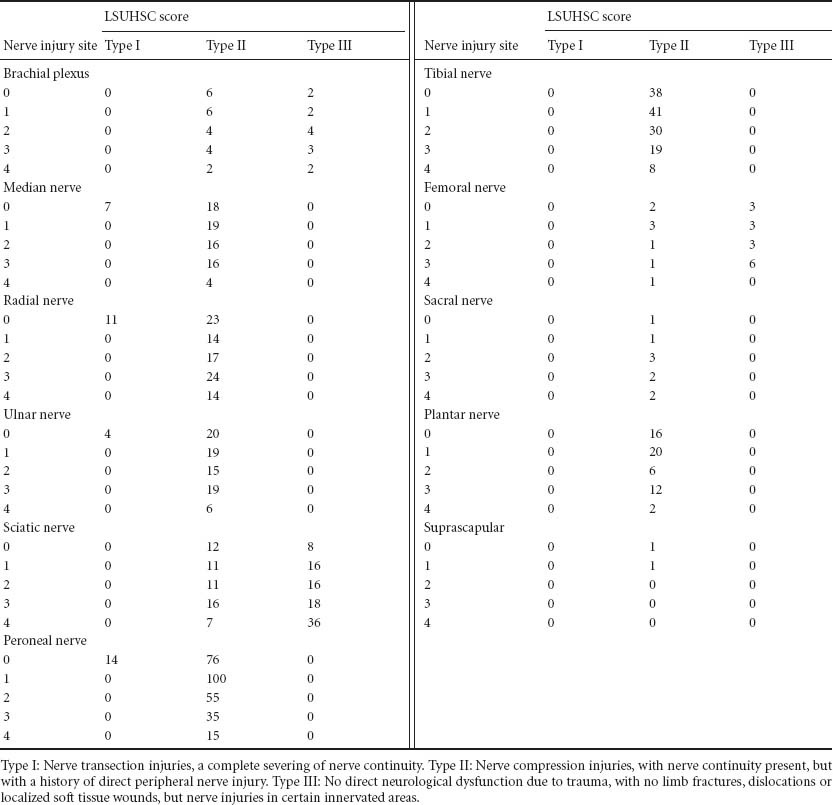
Figure 2.
Distribution of the duration of compression, patient age, gender and type of earthquake-caused injury.
(A) Duration of compression in patients with peripheral nerve injury. (B) Age of patients. (C) Gender of patients. (D) Site of peripheral nerve injury. I: Brachial plexus; II: median nerve; III: radial nerve; IV: ulnar nerve; V: sciatic nerve; VI: peroneal nerve; VII: tibial nerve; VIII: femoral nerve; IX: ssacral nerve; X: plantar nerve; XI: suprascapular.
Soft tissue lesion and nerve injury
We evaluated soft tissue injury according to the medical records of patients and the Arbeitsgemeinschaft für Osteosynthesefragen (AO) classification system for soft tissue injury (McKay et al., 1983) to determine the predictive value of the severity of closed injury on the severity of nerve injury, evaluated with the LSUHSC nerve injury scoring system. We found that closed injury was associated with LSUHSC nerve injury score (P < 0.05). Similarly, we examined whether open transection nerve injury, muscle and tissue injury or nerve and vessel injury were independent predictors of nerve injury. We found that muscle and tissue injury, as well as nerve and vessel injury, were associated with nerve injury score (P < 0.05), but had no association with open injury (P > 0.05).
For type II nerve injury, we determined whether compartment syndrome and crush injury were associated with nerve injury score and found that both factors were associated with nerve injury score (P < 0.05).
Seventy-three patients had movement disorder and sensory dysfunction in certain innervated areas when they were rescued, but these patients were not harmed directly by external mechanical forces. A few similar injuries have been described in other reports (Yoshida et al., 1999). All patients had been trapped in a passive body position for a long period of time. The hip joint of patients with sciatic nerve injury was in the flexion position when they were trapped. Overall, 38 patients were in a squatting position. Among these, the hip joint was in the flexion position and the knee joint was in the extension position for 12 patients, and three had their legs spread apart in a split position.
Recovery following nerve injury
The nerve injury scores from screening patients at up to 1 year and between 1 and 2 years are given in Table 2. If scores remained poor (0 or 1) after 1 year of treatment, further treatment was not effective and the nerve scores did not improve. However, if the scores increased (4 or 5) after 1 year, further treatment was likely to be more effective and the possibility of recovery increased (Murovic, 2009a, b).
Table 2.
Louisiana State University Health Sciences Center (LSUHSC) nerve injury scores from 2008 to 2010
Infection and nerve injury recovery
Among the 22 patients with open transection injury, 13 had infections around the wound. Patients with infections had their dressings changed (Table 3). After the soft tissue was stabilized, surgery was performed. One patient underwent direct nerve anastomosis. Five patients had nerve graft repair.
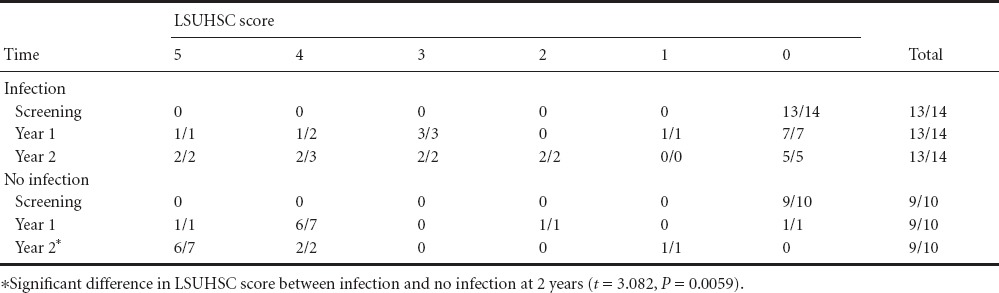
Table 3.
Number of cases and nerves (case/nerves) using the Louisiana State University Health Sciences Center (LSUHSC) nerve injury score for patients with and without infection
Calf compartment syndrome and nerve injury recovery
We studied whether calf compartment syndrome was associated with recovery from injury. We calculated the difference in LSUHSC scores during treatment and found an association between compartment syndrome and recovery (Figure 3).
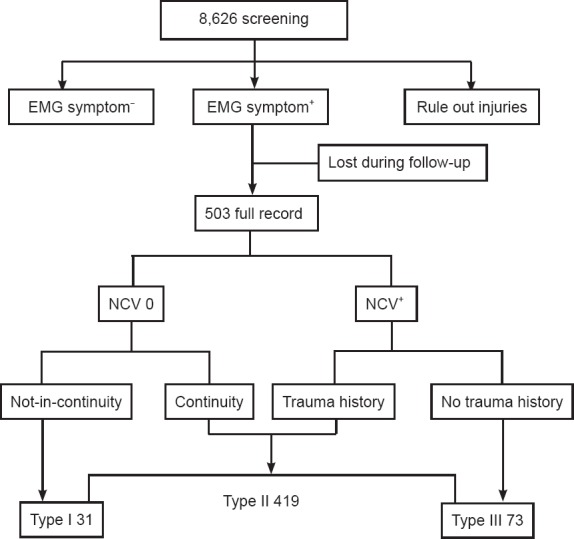
Figure 3.
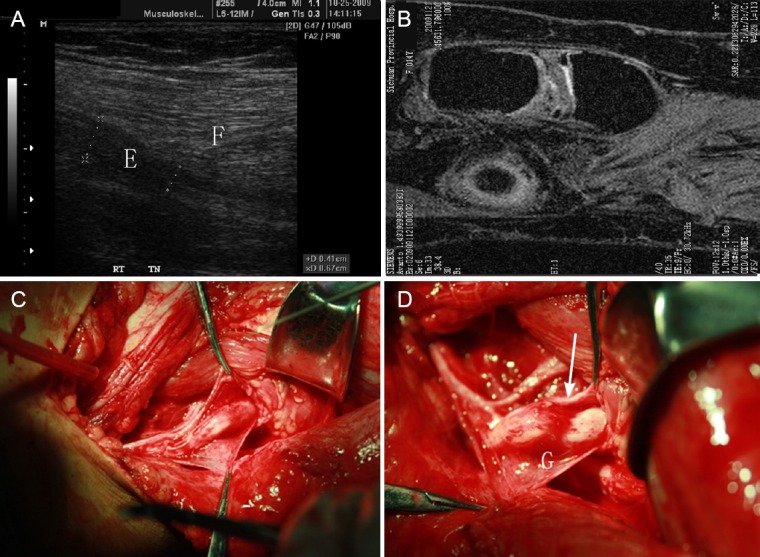
Proximal tibial nerve of one patient with earthquake-caused nerve injury.
(A) Ultrasound image of the proximal tibial nerve of one patient with earthquake-caused nerve injury. A well-localized indentation is shown in the tibial nerve (E) directly beneath the fibromuscular soleal sling (F). (B) MRI image of the fibromuscular soleal sling and tibial nerve. (C) Surgery of the nerve. Proximal is to the left and distal is to the right. The curved line highlights the fibromuscular soleal sling. (D) Same patient with the tibial nerve injury underwent neurolysis and fibromuscular sling retraction (G: Location of compression on the tibial nerve by the fibromuscular sling). Arrow points to the discrete, well-localized indentation in the tibial nerve beneath the fibromuscular soleal sling, which is suggestive of pathologic compression of the tibial nerve.
Positional nerve injury recovery analysis: a typical case
During the second year, all of the type III patients showed full recovery, except for one female 19-year-old patient, who had been trapped under the earthquake rubble for 38 hours with hip flexion and knee extension. This patient underwent ultrasonography, MRI and electromyography. At the end of year 2, her whole sciatic nerve had thickened, because of injury to the entire nerve and all branches. Imaging showed the internal blood supply was greater on the injured than the opposite side, and electromyography revealed persistent left sciatic nerve injury (Figure 4).
Figure 4.
MRI results of type III sciatic nerve injury.
The patient, female, 19 years old, had been trapped under the earthquake rubble for 38 hours with hip flexion and knee extension. (A) Injured left sciatic nerve shows larger diameter than the right nerve (12.9 mm × 5.7 mm vs. 6.8 mm × 5.0 mm) on the axial T1-weighted MRI image. (B) Left sciatic nerve shows hyperintense signals and the right sciatic nerve shows isointense signals on axial diffusion-weighted MRI image. (C) A large part of the left sciatic nerve demonstrating hyperintense signals and thickness on reconstructed diffusion-weighted MRI image. (D, E) After contrast media administration, the left sciatic nerve shows greater enhancement than the right (77% vs. 53%).
Therapeutic intervention and recovery from nerve injury
Physiotherapy and pharmacotherapy
Neurologic recovery was evaluated by calculating the difference in LSUHSC scores between 2008 and 2010. Recovery was considered an ordinal categorical variable. In all, 229 patients received physiotherapy. Physiotherapy was effective for recovery for type I and type II (P = 0.034 and P = 0.001), but not type III nerve injury (P = 0.511). A total of 346 patients received pharmacotherapy (vitamin B12, 500 μg/day, for about 12 weeks). Recovery significantly differed with and without pharmacotherapy for recovery for type I injury (P = 0.003). For patients with type II nerve injury, pharmacotherapy was negatively correlated with recovery (ρ = −0.076). For type III nerve injury, pharmacotherapy was not effective (P > 0.05).
Surgery and compartment incision decompression
In total, 262 nerves were surgically operated on and 186 nerves were rehabilitated. Surgery was weakly correlated with nerve rehabilitation (ρ = 0.092). Cutting open the compartment for decompression affected nerve recovery. In the first year, 75% of nerves (27 nerves) with a screening score of 0 that did not undergo nerve decompression did not improve, and only 33.3% of nerves with a score of 0 (five nerves) that underwent decompression did not improve. Similarly, nerves with a screening score of 2 or 3 having undergone nerve decompression improved more than those not having undergone decompression. In the second year, all nerves with an LSUHSC screening score of 0 showed no recovery, but nerves with higher initial scores that underwent decompression improved more than those that did not undergo decompression.
During follow-up, some patients with calf compartment syndrome showed a delay in tibial nerve recovery (Figure 3). Physical examination revealed some patients with Tinel's sign for irritated nerves in the upper part of the calf. Ultrasonography and MRI revealed signs of nerve compression where the tibial nerve passes through the tendinous arch of the soleus muscle (Figure 3). Six patients underwent incision of the tendinous arch for decompression, for better recovery.
Discussion
Our analysis of a large number of cases showed that earthquake compression injuries were mostly caused by direct nerve compression, resulting in deformation of the nerve. Injury in this group of patients could be at any location in the nerve and could be due to direct compression on the local nerve by a foreign object or to the compression or twisting of the nerve by a fractured bone. Other than the localized compression injuries caused by direct nerve compression, we also found many patients at the earthquake site who suffered from crush syndrome and compartment syndrome. These patients experienced a diffuse external mechanical force directly on the nerves, causing a wide range of nerve injuries.
Using electromyographic, ultrasound and MRI examinations, we found that three factors were involved in nerve injuries. First, the diffuse force directly impacted nerve bundles. Second, a large portion of soft tissue injuries caused damage to the nerve vascular bed, affecting blood supply to the nerve. Third, because of extensive compression, numerous scars formed within and around nerves, further aggravating the nerve injury and affecting nerve functional recovery. Trauma and other factors can cause the tendinous arch of the soleus muscle to compress the tibial nerve (Drees et al., 2002; Williams et al., 2009). Mastaglia (2000) reported nine patients with tibial nerves compressed by the tendinous arch of the soleus. Compartment syndrome associated with the earthquake exhibited similar features (Yoshida et al., 1999; Drees et al., 2002).
Nerve injury without direct trauma is a special class of injury. After reviewing the literature, we found that a few similar injuries have been described unsystematically in different reports (Yoshida et al., 1999). For example, for the Hanshin-Awaji earthquake in Japan, Takeshi reported some patients with orthostatic nerve injuries (Yoshida et al., 1999). Patients with this type of nerve injury normally do not have direct injury or soft tissue or bone tissue injury where nerves are located. However, further investigation showed that patients normally had a longer period in a passive body position. The analysis of patient body positions and injured nerves showed that sciatic nerve injuries occurred most often in patients trapped in a squatting position. The sciatic nerve is in the hip extensor side. When the hip joint bends, the sciatic nerve comes under tension. The femoral nerve is in the hip flexor side. When the hip joint is in hyperextension, the femoral nerve is under tension. When the patients were trapped in a squatting position, the sciatic nerve was under tension, and the femoral nerve was relaxed. The tensed state of the sciatic nerve resulted in injury when it persisted for a long period of time, and the relaxed femoral nerve did not have any abnormality. This type of relationship between injury and body position was observed in all of the nerve injuries without direct trauma; the injured nerves differed only because the position of joint hyperextension or flexion varied.
Further analysis suggested that the injuries were related to the duration of entrapment. We used ordered logistic regression (Long, 1997) and found a significant association between the length of time being trapped and the LSUHSC nerve injury score. The severity of injury could also be related to the degree of stretch. We found that the hip joint of most patients with sciatic nerve injuries was in the flexion position and the knee joint was in the flexion position. However, in some patients, the hip joint was in the flexion position and the knee joint was in the hyperextension position. When the hip joint is flexed, the sciatic nerve is stretched, but if the knee is flexed at the joint, the intensity of stretching can be alleviated to some extent, so the nerve is relatively thicker in the sciatic nerve segment. In addition to hip joint flexion, these patients also had knee joint hyperextension. When trapped for the same or a shorter period of time, the nerve injuries in these patients were more severe than in the other patients.
Among the 22 patients with open transection injury, 13 had infections around the wound. Nerve repair of transection injuries by nerve anastomosis resulted in significantly poorer outcome than other similar nerve injuries. Infection and on-site anastomosis are key determinants of outcome. We think that for this type of nerve transection injury, immediate anastomosis on-site or at frontline emergency treatment centers may not be the best option. Therefore, we propose that, when conditions permit, the damage should first be carefully determined and secondary anastomosis subsequently conducted.
Data were collected 4 weeks after the earthquake and mainly covered information for patients treated in the core area of the earthquake aid center. However, for many affected individuals, the nerve injury was not life-threatening, so those with minor injuries would not seek health care in our aid center. In addition, some had fully recovered before they were approached. Therefore, our data on nerve injury after the earthquake are incomplete. Also, because of the complexities of injury types and locations caused by the earthquake, the observation and analysis of nerve recovery was limited using current methods for statistical analysis.
Earthquake-induced nerve injury may not be life-threatening, but it can affect the long-term quality of life. Effective treatment depends on careful observation and targeted interventions. Closed soft tissue injury was significantly associated with severity of nerve injury, as were compartment and crush syndrome. The position of entrapment was an important factor in the nerve injury. The severity of positional nerve injury was related to the duration of entrapment. The rehabilitation of nerve injuries mainly took place during the first year. Decompression and physiotherapy were effective for neurological recovery. Pharmacotherapy was not effective.
Footnotes
Conflicts of interest: None declared.
Copyedited by Patel B, Norman C, Yu J, Yang Y, Li CH, Song LP, Zhao M
References
- Ahrari MN, Zangiabadi N, Asadi A, Sarafi Nejad A. Prevalence and distribution of peripheral nerve injuries in victims of Bam earthquake. Electromyogr Clin Neurophysiol. 2006;46:59–62. [PubMed] [Google Scholar]
- Baker MS. Creating order from chaos: part I: triage, initial care, and tactical considerations in mass casualty and disaster response. Mil Med. 2007;172:232–236. doi: 10.7205/milmed.172.3.232. [DOI] [PubMed] [Google Scholar]
- Bayard D. Haiti earthquake relief, phase two--long-term needs and local resources. New Engl J Med. 2010;362:1858–1861. doi: 10.1056/NEJMp1003839. [DOI] [PubMed] [Google Scholar]
- Benson M, Koenig KL, Schultz CH. Disaster triage: START, then SAVE--a new method of dynamic triage for victims of a catastrophic earthquake. Prehosp Disaster Med. 1996;11:117–124. doi: 10.1017/s1049023x0004276x. [DOI] [PubMed] [Google Scholar]
- Briggs SM. Earthquakes. Surg Clin N Am. 2006;86:537–544. doi: 10.1016/j.suc.2006.02.003. [DOI] [PubMed] [Google Scholar]
- Chen TW, Yang ZG, Wang QL, Dong ZH, Yu JQ, Zhuang ZP, Hou CL, Li ZL. Crush extremity fractures associated with the 2008 Sichuan earthquake: anatomic sites, numbers and statuses evaluated with digital radiography and multidetector computed tomography. Skeletal Radiol. 2009;38:1089–1097. doi: 10.1007/s00256-009-0743-5. [DOI] [PubMed] [Google Scholar]
- Chunguang Z, Rigao C, Fuguo H, Chongqi T, Yueming S, Guanglin W, Hui Z, Fuxing P, Yan K, Peng L, Ping F, Ye T. Characteristics of crush syndrome caused by prolonged limb compression longer than 24 h in the Sichuan earthquake. Emerg Med J. 2010;27:627–630. doi: 10.1136/emj.2008.070961. [DOI] [PubMed] [Google Scholar]
- Crippen D. The World Trade Center attack. Similarities to the 1988 earthquake in Armenia: time to teach the public life-supporting first aid? Crit Care. 2001;5:312–314. doi: 10.1186/cc1058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drees C, Wilbourn AJ, Stevens GH. Main trunk tibial neuropathies. Neurology. 2002;59:1082–1084. doi: 10.1212/wnl.59.7.1082. [DOI] [PubMed] [Google Scholar]
- Gautschi OP, Cadosch D, Rajan G, Zellweger R. Earthquakes and trauma: review of triage and injury-specific, immediate care. Prehosp Disaster Med. 2008;23:195–201. doi: 10.1017/s1049023x00005847. [DOI] [PubMed] [Google Scholar]
- Gu J, Yang W, Cheng J, Yang T, Qu Y, Kuang Y, Huang H, Yang L, He W, Min L. Temporal and spatial characteristics and treatment strategies of traumatic brain injury in Wenchuan earthquake. Emerg Med J. 2010;27:216–219. doi: 10.1136/emj.2008.065342. [DOI] [PubMed] [Google Scholar]
- Kim DH, Kline DG, Midha R, Murovic JA. Philadelphia: W.B. Saunders Co; 2007. Kline and Hudson's Nerve Injuries: Operative Results for Major Nerve Injuries, Entrapments and Tumors. [Google Scholar]
- Li R, Wang H, Xiao J, Yang X, Guo L, Lu Q, Tang W, Long J, Liu L, Li X, Tian W. Maxillofacial injuries in the Wenchuan earthquake. J Trauma. 2010;69:1481–1485. doi: 10.1097/TA.0b013e3181d76564. [DOI] [PubMed] [Google Scholar]
- Long JS. London: SAGE Publications Ltd; 1997. Regression Models for Categorical and Limited Dependent Variables. [Google Scholar]
- Macintyre AG, Barbera JA, Smith ER. Surviving collapsed structure entrapment after earthquakes: a “time-to-rescue” analysis. Prehosp Disaster Med. 2006;21:4–17. doi: 10.1017/s1049023x00003253. [DOI] [PubMed] [Google Scholar]
- Mastaglia FL. Tibial nerve entrapment in the popliteal fossa. Muscle Nerve. 2000;23:1883–1886. doi: 10.1002/1097-4598(200012)23:12<1883::aid-mus15>3.0.co;2-4. [DOI] [PubMed] [Google Scholar]
- McCunn M, Ashburn MA, Floyd TF, Schwab CW, Harrington P, Hanson CW, Sarani B, Mehta S, Speck RM, Fleisher LA. An organized, comprehensive, and security-enabled strategic response to the Haiti earthquake: a description of pre-deployment readiness preparation and preliminary experience from an academic anesthesiology department with no preexisting international disaster response program. Anesth Analg. 2010;111:1438–1444. doi: 10.1213/ANE.0b013e3181f42fd3. [DOI] [PubMed] [Google Scholar]
- McKay D, Schofield N, Whiteley P. London: Frances Printers; 1983. Data Analysis and the Social Sciences. [Google Scholar]
- Murovic JA. Upper-extremity peripheral nerve injuries: a Louisiana State University Health Sciences Center literature review with comparison of the operative outcomes of 1837 Louisiana State University Health Sciences Center median, radial, and ulnar nerve lesions. Neurosurgery. 2009a;65:A11–17. doi: 10.1227/01.NEU.0000339130.90379.89. [DOI] [PubMed] [Google Scholar]
- Murovic JA. Lower-extremity peripheral nerve injuries: a Louisiana State University Health Sciences Center literature review with comparison of the operative outcomes of 806 Louisiana State University Health Sciences Center sciatic, common peroneal, and tibial nerve lesions. Neurosurgery. 2009b;65:A18–23. doi: 10.1227/01.NEU.0000339123.74649.BE. [DOI] [PubMed] [Google Scholar]
- Normile D. Japan disaster. Devastating earthquake defied expectations. Science. 2011;331:1375–1376. doi: 10.1126/science.331.6023.1375. [DOI] [PubMed] [Google Scholar]
- Oda J, Tanaka H, Yoshioka T, Iwai A, Yamamura H, Ishikawa K, Matsuoka T, Kuwagata Y, Hiraide A, Shimazu T, Sugimoto H. Analysis of 372 patients with crush syndrome caused by the Hanshin-Awaji earthquake. J Trauma. 1997;42:470–476. doi: 10.1097/00005373-199703000-00015. [DOI] [PubMed] [Google Scholar]
- Owens PJ, Forgione A, Briggs S. Challenges of international disaster relief: use of a deployable rapid assembly shelter and surgical hospital. Disaster Manag Response. 2005;3:11–16. doi: 10.1016/j.dmr.2004.10.004. [DOI] [PubMed] [Google Scholar]
- Peek-Asa C, Kraus JF, Bourque LB, Vimalachandra D, Yu J, Abrams J. Fatal and hospitalized injuries resulting from the 1994 Northridge earthquake. Int J Epidemiol. 1998;27:459–465. doi: 10.1093/ije/27.3.459. [DOI] [PubMed] [Google Scholar]
- Peleg K, Reuveni H, Stein M. Earthquake disasters--lessons to be learned. Isr Med Assoc J. 2002;4:361–365. [PubMed] [Google Scholar]
- Salimi J, Abbasi M, Khaji A, Zargar M. Analysis of 274 patients with extremity injuries caused by the Bam earthquake. Chin J Traumatol. 2009;12:10–13. [PubMed] [Google Scholar]
- Sever MS, Vanholder R, Lameire N. Management of crush-related injuries after disasters. New Engl J Med. 2006;354:1052–1063. doi: 10.1056/NEJMra054329. [DOI] [PubMed] [Google Scholar]
- Shi YK, Wang LL, Lin YD, Pei FX, Kang YM. Challenges for rear hospital care of Wenchuan earthquake casualties: experience from West China Hospital. Chin J Traumatol. 2010;13:131–136. [PubMed] [Google Scholar]
- Uzun N, Savrun FK, Kiziltan ME. Electrophysiologic evaluation of peripheral nerve injuries in children following the Marmara earthquake. J Child Neurol. 2005;20:207–212. doi: 10.1177/08830738050200030701. [DOI] [PubMed] [Google Scholar]
- Uzun N, Tanriverdi T, Savrun FK, Kiziltan ME, Sahin R, Hanimoglu H, Hanci M. Traumatic peripheral nerve injuries: demographic and electrophysiologic findings of 802 patients from a developing country. J Clin Neuromuscul Dis. 2006;7:97–103. doi: 10.1097/01.cnd.0000203641.38887.63. [DOI] [PubMed] [Google Scholar]
- Williams EH, Williams CG, Rosson GD, Dellon LA. Anatomic site for proximal tibial nerve compression: a cadaver study. Ann Plas Surg. 2009;62:322–325. doi: 10.1097/SAP.0b013e31817e9d81. 381. [DOI] [PubMed] [Google Scholar]
- Yoshida T, Tada K, Uemura K, Yonenobu K. Peripheral nerve palsies in victims of the Hanshin-Awaji earthquake. Clin Orthop Relat Res. 1999:208–217. [PubMed] [Google Scholar]