Abstract
Background
Medical mistrust is salient among African American women, given historic and contemporary racism within medical settings. Mistrust may influence satisfaction among navigated women by affecting women's perceptions of their health‐care self‐efficacy and their providers' roles in follow‐up of abnormal test results.
Objectives
To (i) examine whether general medical mistrust and health‐care self‐efficacy predict satisfaction with mammography services and (ii) test the mediating effects of health‐related self‐efficacy.
Design
The current study is a part of a randomized controlled patient navigation trial for medically underserved women who had received a physician referral to obtain a mammogram in three community hospitals in Chicago, IL. After consent, 671 African American women with no history of cancer completed questionnaires concerning medical mistrust and received navigation services. After their mammography appointment, women completed health‐care self‐efficacy and patient satisfaction questionnaires.
Results
Women with lower medical mistrust and greater perceived self‐efficacy reported greater satisfaction with care. Medical mistrust was directly and indirectly related to patient satisfaction through self‐efficacy.
Conclusions
Preliminary findings suggest future programmes designed to increase health‐care self‐efficacy may improve patient satisfaction among African American women with high levels of medical mistrust. Our findings add to a growing body of literature indicating the importance of self‐efficacy and active participation in health care, especially among the underserved.
Keywords: mammogram, medical mistrust, patient navigation, patient satisfaction, self‐efficacy
Introduction
Patient navigation is a well‐documented strategy towards the mitigation of racial/ethnic and socio‐economic disparities in access to early detection, diagnosis, treatment and survivorship of cancer.1, 2, 3, 4 Patient navigators serve multiple roles throughout the breast cancer care continuum, including care management (e.g. logistic and financial assistance), mediation of provider–patient interactions, as well as patient education and counselling (e.g. self‐efficacy, trust).5 Determining which of these roles is important for medically underserved patients to optimize existing navigation programmes.
The importance of patient satisfaction among navigated women
Recent efforts have sought to gain consensus and identify metrics towards realizing the promise of navigation to these ends, identified primary outcomes of the National Cancer Institute‐supported Patient Navigation Research Program include: (i) timeliness of diagnosis (i.e. receipt of screening and diagnostic mammography); (ii) timeliness of cancer treatment; (iii) patient satisfaction and quality of life and (iv) cost‐effectiveness analysis.2, 6 The majority of interventions have focused on the first two outcomes. Systematic and qualitative reviews have indicated that recipients of navigation are more likely to have timely adherence to recommended breast cancer screening, diagnostic procedures and treatment.4, 5 However, relatively less research has focused on perceived quality of care and patient satisfaction. Further investigation concerning predictors of patient satisfaction among navigated women is warranted, as satisfaction has been tied to patient health status, quality of life and adherence to recommended care.7 Furthermore, satisfaction has been incorporated into quality assessment and accreditation reports; these data can serve as evidence to inform organizational policy decisions on continuation and adaptation of services.8
Navigated women report particularly high levels of satisfaction with breast health care, including navigation pertaining to mammography appointments.9, 10, 11, 12 Notably, studies have had relatively low proportion of ethnic minority women.9, 10, 12 Available studies suggest racial/ethnic differences in satisfaction exist among navigated women, wherein minority women report lower satisfaction than non‐Hispanic White counterparts.13, 14 Furthermore, there has been some suggestion that the impact of navigation on satisfaction may differ across ethnic groups.13 Identifying predictors of patient satisfaction within different underserved and marginalized populations, including African Americans, is integral to inform policy decisions to adapt existing patient navigation programmes for this population. The current study examines the importance of medical trust and self‐efficacy in existing navigation training programmes to promote timely follow‐up mammography among African American women.
Medical mistrust and patient satisfaction
Interpersonal factors, and provider–patient relationships specifically, are major predictors of patient satisfaction in the cancer care context.8 Trust in the healthcare system has important implications for satisfaction and may be particularly relevant for African Americans, who live in the context of historic and contemporary forms of racism in medical settings.15, 16, 17, 18 The unique and severe forms of racism African Americans experience, including segregated health‐care systems and overt interpersonal racism by providers, can contribute to elevated levels of medical mistrust and sub‐optimal adherence as well as lower satisfaction and quality of life.3, 17, 19, 20, 21, 22, 23, 24 The medical mistrust observed among African Americans can be considered a consequence of collective disempowerment and marginalization as well as daily exposure to implicit and explicit interpersonal and systemic forms of racism.22, 25 Medical mistrust with the health‐care system in general has been associated with anxiety, depression and perceived lower quality care among African American patients with breast cancer,24, 26 but little is known about its role in the context of early detection practices and diagnostic procedures (i.e. mammography).
Navigation services provide an opportunity to address disparities in breast health‐care use resulting from medical mistrust.3 Navigators have been thought to increase trust among patients and positive outcomes, as they are perceived to be conduits between patient communities and the health‐care industry. Nonetheless, little research has documented the general level of medical mistrust among navigated women, nor assessed the effect of medical mistrust on patient satisfaction with mammography services. Such research may serve to inform decisions concerning the importance of facilitating self‐efficacy in navigation services, especially among populations with high levels of medical mistrust.
A conceptual model of medical mistrust and patient satisfaction
Identifying psychological processes and mechanisms in associations between mistrust and satisfaction has important implications for refinement of existing navigator roles. For example, medical mistrust may impact patient preferences and perceptions concerning their own and their providers' roles in seeking care including mammography, which in turn may influence satisfaction with care. Figure 1 depicts a potential conceptual model to understand the potential mediating roles of perceptions about roles and subsequent decision‐making patterns in the relationship between medical mistrust and patient satisfaction. This framework offers a conceptualization to understand how greater medical mistrust may translate into lower patient satisfaction. Our conceptual model is adapted from the theoretical framework developed by Pascoe and Richman,27 wherein anticipation and perceptions of discrimination (e.g. medical mistrust) may influence subsequent health outcomes through psychological, behavioural and physiological mediating factors. We hypothesize that medical mistrust is related to patient satisfaction through general perceptions about the roles of patient and care provider, which in turn influence patient perceptions and actions during specific instances of care.28 Women with greater medical mistrust may perceive themselves as less able to engage with providers (e.g. lower health‐care self‐efficacy, shared decision‐making preferences). Lower general perceived decision‐making ability in medical settings may influence patient actions and perceptions of received care, including cancer screening and diagnostic appointments. Specifically, lower health‐care self‐efficacy and shared decision‐making preferences may result in lower participation in care and subsequently comprehension of procedures and information provided during health‐related interactions.29, 30 Lower levels of shared decision‐making practices and patient comprehension may be associated with lower patient satisfaction.28, 30, 31, 32, 33 The current study provides a preliminary test of this framework and examines the mediating effect of health‐care self‐efficacy in the relationship between medical mistrust and patient satisfaction.
Figure 1.
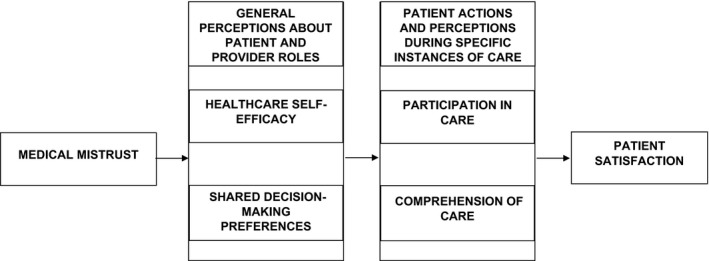
Conceptual model.
The current study defines health‐care self‐efficacy as the patient's perceived ability to obtain, understand, and act on information in medical settings.23, 34 Through this lens, women with higher levels of medical mistrust in general may perceive themselves less able to acquire, understand, and act on health information. Simultaneously, women with higher levels of health‐care self‐efficacy may have greater satisfaction with care. Consequently, higher levels of medical mistrust may result in lower satisfaction, in part, because of lower health‐care self‐efficacy. In addition to case management and informational support, another component of navigation services is patient empowerment and facilitating self‐efficacy and medical advocacy.3, 35 This component may be particularly relevant for patients with higher levels of medical mistrust. If navigated, women with high levels of general medical mistrust report lower satisfaction with mammography services due to lower perceived general health‐care self‐efficacy, recommended modifications to navigation services may include assessing patients' medical mistrust and emphasizing educational components concerning patient empowerment to increase self‐efficacy among patients with documented high levels of medical mistrust.
Current study
The current study provides preliminary evidence concerning the importance of patient perceptions and confidence in active participation in care for health‐care utilization among African American women. We hypothesize that, among women who receive navigation services for mammography services, African American women with higher levels of general medical mistrust and lower levels of general health‐care self‐efficacy will report lower satisfaction with mammography services. Second, we hypothesize greater general medical mistrust may be related to lower satisfaction with mammography services indirectly through lower general self‐efficacy.
Materials and methods
Procedures
The current study is part of a 5‐year patient navigation intervention for female patients with primary care provider referrals for screening and diagnostic mammography across three community hospitals located in Chicago, Illinois (‘Patient Navigation in Medically Underserved Areas Project’). All study procedures and content were approved by the participating research institution's Institutional Review Board. Potential participants were identified from breast imaging departments' patient lists of individuals who had scheduled a screening or diagnostic mammography appointment. Study staff randomized women into standard care and navigation arms. Women who were randomized into the navigation arm subsequently interacted with one of four patient navigators who were lay community residents, but affiliated with one of the participating hospitals. Study staff with years of experience in training navigators monitored study navigators with regard to intervention fidelity and interview processes. Navigators then contacted potential participants for screening and to obtain informed consent.
Navigated women interacted at least twice with navigators, unless they missed an appointment or initiated contact. During the first interaction, women underwent screening, consent, baseline questionnaires and navigation services. Baseline questionnaires included socio‐demographic information as well as the instrument for medical mistrust. Navigators provided assistance with appointment/information verification, correcting potential systemic errors (e.g. delayed scheduling), and counselling women with regard to communication concerns (e.g. confusion about recommended mammography) and attitudes towards providers (e.g. perceived disrespect from staff). Navigators also utilized a ‘teach back’ method to ensure comprehension of upcoming appointments and to encourage patients to actively engage health‐care staff for further information. After completing their mammography appointments, women interacted with navigators a second time to complete questionnaires concerning general health‐care self‐efficacy and patient satisfaction.
The current study uses a subset of the larger study's sample (n = 671), which was identified from baseline and follow‐up survey answers using the following criteria: (i) identification as African American; (ii) randomization into the navigation arm of the larger project; (iii) no previous cancer history and (iv) completion of the patient satisfaction questionnaire. There was no age eligibility criterion for the trial.
Measures
Socio‐demographic and clinical variables
During the first interaction, age, education leveland household income data were collected. In addition, women were asked about the type of insurance they had, whether they had a medical home/regular source of care and if they had ever received a mammogram prior to study enrolment.
General medical mistrust
During the first interaction, we administered the 10‐item Health Care System Distrust Scale, which has been validated in several studies including a substantial proportion of African American participants.16 Sample items include ‘If a mistake were made in my health care, the health care system would try to hide it from me’ and ‘The health care system cares more about holding costs down than it does about doing what is needed for my health’. Response categories were on a 5‐point Likert scale, as follows: 1 = strongly disagree, 2 = strongly disagree, 3 = not sure, 4 = agree and 5 = strongly agree. Cronbach's alpha for this sample was 0.80. Summary scores were calculated such that higher scores indicated greater distrust in the health‐care system.
General health‐care self‐efficacy
During the second interaction, women completed the 12‐item Communication and Attitudinal Self‐efficacy Scale, which was developed and validated among a sample with a large proportion of African Americans.36 Sample items include ‘I know that I will be able to actively participate in decisions about my health’ and ‘It is easy for me to get health information’. Response categories were on a 5‐point Likert scale, as follows: 1 = strongly disagree, 2 = slightly disagree, 3 = slightly agree and 4 = strongly agree. Preliminary distribution of individual items suggested non‐normal distribution; given this, we recoded options to be 1 = strongly disagree/slightly disagree, 2 = slightly agree and 3 = strongly agree. Cronbach's alpha for this scale was 0.84. Summary scores were calculated such that higher scores indicated greater health‐care self‐efficacy.
Patient satisfaction with mammography services
During the second interaction, the Patient Satisfaction with Cancer‐Related Care is an instrument developed by investigators from the ten‐site National Cancer Institute Patient Navigation Research Program.2, 7 This instrument was developed to assess satisfaction throughout the breast cancer care continuum. The content of all items is general and can be applied to different types of breast cancer care, from screening mammography to breast cancer treatment. Sample items include ‘My questions were answered to my satisfaction’ and ‘I received all the services I needed’. Response categories included: 1 = strongly disagree, 2 = disagree, 3 = undecided, 4 = agree and 5 = strongly agree. Cronbach's alpha for the overall instrument for this sample was 0.93. Summary scores were calculated such that higher scores indicated greater satisfaction with follow‐up care.
Statistical analysis
Descriptive statistics were reported concerning participants' baseline socio‐demographic and clinical variables. Pearson's correlations and analyses of variance (anovas) were conducted to identify potential covariates. Next, we conducted a linear regression model to examine the relative effects of general medical mistrust and general health‐care self‐efficacy on patient satisfaction with mammography services. Finally, we conducted mediation analyses, using the bootstrapping Preachers and Hayes method.37 This method is a non‐parametric resampling procedure that involves data sampling multiple times (5000 for this study) and generating a sampling distribution. We calculated 95% confidence intervals of the effect of significant predictors of satisfaction through general health‐care self‐efficacy (A*B or mediated effect). We also conducted the conventional Sobel's test to test the mediation model.38
Results
Table 1 summarizes socio‐demographic, clinical and main study variables for our sample (n = 671). As there were very few missing cases (<1%), we used case deletions to accommodate them. This is considered a simplistic and adequate method for data sets with a limited amount of missing data.39 Bivariate analyses showed that age was negatively correlated with patient satisfaction with mammography services, Pearson's r = −0.13, P = 0.001 and general medical mistrust, Pearson's r = 0.09, P = 0.02. Other associations were not statistically significant. Given this, age was included as a covariate in all subsequent analyses.
Table 1.
Characteristics of study sample (n = 671)
| Variable | Range | M (SE) |
|---|---|---|
| Age | 58.77 (0.47) | |
| Educationa | 1–7 | 4.35 (0.06) |
| Incomeb | 1–6 | 4.17 (0.07) |
| General medical mistrustc | 14–44 | 25.84 (0.21) |
| General health‐care self‐efficacyd | 11–46 | 31.60 (0.16) |
| Patient satisfactionc | 34–140 | 111.11 (0.52) |
| n (%) | |
|---|---|
| % Private insurance | 540 (78) |
| % Regular source of care | 677 (97) |
| % Lifetime history of mammography | 670 (97) |
1 = 8th grade or less, 2 = some high school, 3 = high school diploma/GED, 4 = some college/vocational training, 5 = associate's degree, 6 = college degree and 7 = graduate/professional degree.
1 = <$10 000, 2 = $10–19 999, 3 = $20–29 999, 4 = $30–39 999, 5 = $40–49 999, 6 = $50 000<.
1 = strongly disagree to 5 = strongly agree.
1 = strongly disagree to 4 = strongly agree.
A multivariable linear regression model was conducted to examine associations of general medical mistrust and health‐care self‐efficacy on patient satisfaction with mammography services, controlling for age. General medical mistrust was negatively related to patient satisfaction with mammography services, B = −0.52, 95% CI [−0.69, −0.34], P < 0.0001. Women with high levels of general perceived self‐efficacy, B = 0.46, 95% CI [0.29, 0.64], P < 0.0001.
Mediation models
We conducted a mediation analysis to assess the indirect effect of general medical mistrust on patient satisfaction with mammography services through general health‐care self‐efficacy, after adjusting for age. We found evidence of significant partial mediation, adjusted R 2 = 0.11, mediated effect = −0.07, 95% CI [−0.13, −0.02] (Fig. 2). Results were similar when a Sobel test was conducted, Z = 3.07, P = 0.002. Altogether, one factor contributing to the lower levels of patient satisfaction with mammography services among navigated women who had higher levels of general medical mistrust was lower general health‐care self‐efficacy.
Figure 2.
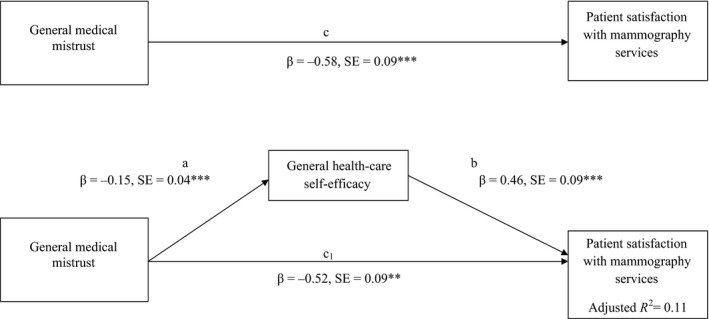
Mediation model of the relationship of general medical mistrust and patient satisfaction with mammography services (n = 665), after adjusting for age. All coefficients represent unstandardized regression coefficients. **P < 0.01. ***P < 0.001.
Discussion
Patient navigation is a strategy that was developed to aid medically underserved women, including low‐income racial/ethnic minorities.1 To date, much research has explored the effectiveness of navigation on timeliness in receipt of recommended procedures; less work has examined patient satisfaction and contributing factors.4, 5 Existing work has suggested variation across race/ethnicity and the need to explore determinants of satisfaction within racial/ethnic groups. The current study provides important contributions to existing literature with regard to patient satisfaction with mammography services among African American women receiving navigation services. One implication from our work is the potential for navigation services to improve satisfaction with mammography services and other breast health care for this traditionally marginalized population, by continuing to provide support to facilitate health‐care self‐efficacy among women with high levels of mistrust, which seems to mitigate the effect of mistrust.
Our work contributes to a substantial body of literature that has indicated the importance of addressing medical mistrust among African Americans to improve patient satisfaction and adherence.3, 17, 19, 20, 23, 24 The current study suggests that the impact of mistrust is relevant for interventions aiming to mitigate health care and health disparities. African American women with high levels of medical mistrust reported less satisfaction with navigation care with mammography services. Such findings suggest a need to continue to strengthen ties between medically underserved communities and health‐care institutions. Importantly, we used lay navigators who were affiliated with hospitals. Women with elevated levels of medical mistrust may respond differently to navigators, based on their status as a community member as opposed to health‐care professional (e.g. nurse navigator) and their affiliation with hospitals. Future work concerning the influence of medical mistrust on the impact of navigation should examine these potential differences and explore how different navigator models may be more effective in building self‐efficacy among different populations varying in medical mistrust. Nevertheless, patient navigation is an excellent potential tool with which partnerships may be fostered and trust may be built. Future qualitative research on patient and health‐care provider perspectives is warranted to determine how and why navigators may best facilitate relationships.
Our work further aligns with extant literature concerning self‐efficacy and patient satisfaction. Women who indicated greater health‐care self‐efficacy also reported more satisfaction with mammography services. Our work suggests that general medical mistrust may directly influence satisfaction with specialty care and mammography services in particular, but also may also influence satisfaction through impacting patient perceptions of their own abilities and roles within care (health‐care self‐efficacy). Our work provides evidence towards the theory of Pascoe and Richman27 as well as contributes to a growing body of literature concerned with the role of psychological factors and perceptions in patient–provider interactions and receipt of care.
Notably, we did not test all of the associations posited in our conceptual model. Future work is necessary to explore how patient perceptions and trust in the health‐care industry impact their perspectives on patient and provider roles and subsequent satisfaction and utilization patterns. For example, future research may benefit from using validated instruments of shared decision‐making preferences or the preference to have providers and patients collaborate together in decisions concerning care. African Americans have been suggested to be less likely to prefer shared decisions in general.40 Qualitative work by Peek and colleagues have highlighted that preference for doctors to decide care may be a consequence of medical mistrust and internalized racism among African Americans.31 Simultaneously, shared decision‐making preferences have been associated with greater information exchange among patients–providers, adherence, and satisfaction in breast health care and other medical settings.31, 32 Altogether, future research is needed to test whether shared decision‐making preferences serve as another mediator in the relationship between medical mistrust and patient satisfaction. Studies are also necessary to incorporate patient actions with regard to decisions about and comprehension of care and test multiple components of our model. This research would help to develop targeted interventions to mitigate mistrust and promote satisfaction and adherence to recommended care, depending on patients' needs.
Limitations
The current study has several limitations. First, while the larger intervention study is a randomized controlled trial, the current study draws from a subsample of women who received the intervention, which may impact generalizability. Second, the mediator and outcome variables were measured during the same time‐point, which influences our ability to make causal inferences. Third, the current study focused on the experiences of African American women, given the well‐documented and extensive disparities in receipt of breast cancer‐related care (mammography, diagnostic procedures and treatment) and subsequent cancer outcomes. Other work is, however, necessary to explore whether relationships between medical mistrust, self‐efficacy and satisfaction are paralleled in other medically underserved populations. Finally, research is warranted to examine the role of navigation in these relationships; future studies should examine associations of medical mistrust, health‐care self‐efficacy and satisfaction with care across women who have and have not received navigation services.
Conclusions
The current study found several important factors pertaining to patient satisfaction among a group of African American women who were received navigation services to obtain mammograms. African American women with greater levels of general medical mistrust reported lower satisfaction with mammography services. Simultaneously, women with greater general health‐care self‐efficacy reported greater satisfaction with mammography services. In line with existing theory by Pascoe and Richman27 and our conceptual model (Fig. 1), findings suggested that one contributing factor to the association between medical mistrust and patient satisfaction was health‐care self‐efficacy, wherein women with higher levels of general medical mistrust experience lower general perceived health‐care self‐efficacy and subsequent lower satisfaction with mammography services. Our work coincides with existing literature and furthermore adds much needed information concerning potential mechanisms to target to improve existing programs dedicated to the reduction and elimination of health disparities and to increase quality of care for traditionally underserved populations with high levels of medical mistrust.
Research and practice implications to improve patients' perceived self‐efficacy and action in care
Instilling trust and promoting self‐efficacy are major roles of many navigator programs. Our data suggest that these programs may consider measuring levels of medical trust to determine the level of emphasis that should be placed on promoting self‐efficacy to improve African American women's satisfaction with mammography and other breast health care. Health‐care providers may also address these needs, either as navigators or in their primary roles during administration of care. Building trust with African American patients may result in greater satisfaction with cancer‐related care, including mammography. Also, targeted patient advocacy and empowerment strategies for African American women with high levels of medical trust may help to improve satisfaction. Such efforts to increase patients' perceived confidence and self‐efficacy in obtaining, understanding and acting on health information may help to reduce the influence of trust on satisfaction.
Sources of funding
The current project was funded by multiple National Institutes of Health/National Cancer Institute grants (P50CA106743, P50CA148143, R25CA92408).
Disclosure Statement
The authors have no conflicts to disclose.
Acknowledgements
The authors thank Dr. Beti Thompson, Dr. Richard Campbell, Heather Pauls and Ganga Vijayasiri for data support and constructive feedback.
References
- 1. Freeman HP. Patient navigation: a community based strategy to reduce cancer disparities. Journal of Urban Health, 2006; 83: 139–141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Freund KM, Battaglia TA, Calhoun E et al National cancer institute patient navigation research program. Cancer, 2008; 113: 3391–3399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Natale‐Pereira A, Enard KR, Nevarez L, Jones LA. The role of patient navigators in eliminating disparities. Cancer, 2011; 117: 3543–3552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Wells KJ, Battaglia TA, Dudley DJ et al Patient navigation: state of the art or is it science? Cancer, 2008; 113: 1999–2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Robinson‐White S, Conroy B, Slavish KH, Rosenzweig M. Patient navigation in breast cancer: a systematic review. Cancer Nursing, 2010; 33: 127–140. [DOI] [PubMed] [Google Scholar]
- 6. Esparza A, Calhoun E. Measuring the impact and potential of patient navigation. Cancer, 2011; S15: 3535–3536. [DOI] [PubMed] [Google Scholar]
- 7. Jean‐Pierre P, Fiscella K, Freund KM et al Structural and reliability analysis of a patient satisfaction with cancer‐related care measure: a multisite patient navigation research program study. Cancer, 2011; 117: 854–861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Lis CG, Rodeghier M, Gupta D. Distribution and determinants of patient satisfaction in oncology: a review of the literature. Patient Satisfaction and Adherence, 2009; 3: 287–304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Campbell C, Craig J, Eggert J, Bailey‐Dorton C. Implementing and measuring the impact of patient navigation at a comprehensive community cancer center. Oncology Nursing Forum, 2010; 37: 61–69. [DOI] [PubMed] [Google Scholar]
- 10. Cavanagh MF, Lane DS, Messina CR, Anderson JC. Clinical case management and navigation for colonoscopy screening in an academic medical center. Cancer, 2013; 119: 2894–2904. [DOI] [PubMed] [Google Scholar]
- 11. Ferrante J, Chen P‐H, Kim S. The effect of patient navigation on time to diagnosis, anxiety, and satisfaction in urban minority women with abnormal mammograms: a randomized controlled trial. Journal of Urban Health, 2007; 85: 114–125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Hook A, Ware L, Siler B, Packard A. Breast cancer navigation and patient satisfaction: exploring a community‐based patient navigation model in a rural setting. Oncology Nursing Forum, 2012; 39: 379–386. [DOI] [PubMed] [Google Scholar]
- 13. Fiscella K, Whitley K, Hendren S et al Patient navigation for breast and colorectal cancer treatment: a randomized trial. Cancer Epidemiology, Biomarkers, & Prevention, 2012; 2012: 1673–1681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Jean‐Pierre P, Winters PC, Clark J et al Do better‐rated navigators improve patient satisfaction with cancer‐related care? Journal of Cancer Education, 2013; 28: 527–534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Adegbembo AO, Tomar SL, Logan HL. Perception of racism explains the difference between Blacks' and Whites' level of healthcare trust. Ethnicity & Disease, 2006; 16: 792–798. [PubMed] [Google Scholar]
- 16. Armstrong K, Rose A, Peters N, Long JA, McMurphy S, Shea JA. Distrust of the health care system and self‐reported health in the United States. Journal of General Internal Medicine, 2006; 21: 292–297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Boulware LE, Cooper LA, Ratner LE, LaVeist TA, Powe NR. Race and trust in the health care system. Public Health Reports, 2003; 118: 358–365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Kennedy BR, Mathis CC, Woods AK. African Americans and their distrust of the health care system: healthcare for diverse populations. Journal of Cultural Diversity, 2007; 14: 56–60. [PubMed] [Google Scholar]
- 19. Bogart LM, Bird ST, Walt LC, Delahanty DL, Figler JL. Association of stereotypes about physicians to health care satisfaction, help‐seeking behavior, and adherence to treatment. Social Science & Medicine, 2004; 58: 1049–1058. [DOI] [PubMed] [Google Scholar]
- 20. Katapodi MC, Pierce PF, Facione NC. Distrust, predisposition to use health services and breast cancer screening: results from a multicultural community‐based survey. International Journal of Nursing Studies, 2010; 47: 975–983. [DOI] [PubMed] [Google Scholar]
- 21. LaVeist TA, Isaac LA, WIlliams KP. Mistrust of the health care organizations is associated with underutilization of health services. Health Services Research, 2009; 44: 2093–2105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. LaVeist TA, Nickerson KJ, Bowie JV. Attitudes about racism, medical mistrust, and satisfaction with care among African American and white cardiac patients. Medical Care Research and Review, 2000; 57: 146–161. [DOI] [PubMed] [Google Scholar]
- 23. Maly RC, Stein JA, Umezawa Y, Leake B, Douglas Anglen M. Racial/ethnic differences in breast cancer outcomes among older patients: effects of physician communication and patient empowerment. Health Psychology, 2008; 27: 728–736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Sheppard VB, Harper FWK, Davis K, Hirpa F, Makambi K. The importance of contextual factors and age in association with anxiety and depression in black breast cancer patients. Psycho‐Oncology, 2014; 23: 143–150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Dovidio JF, Penner LA, Norton TL, Gaertner SL, Shelton JN. Disparities and distrust: the implications of psychological processes for understanding racial disparities in health and health care. Social Science & Medicine, 2008; 67: 478–486. [DOI] [PubMed] [Google Scholar]
- 26. Masi CM, Gehlert S. Perceptions of breast cancer treatment among African‐American women and men: implications for interventions. Journal of General Internal Medicine, 2008; 24: 408–414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Pascoe EA, Richman LS. Perceived discrimination and health: a meta‐analytic review. Psychological Bulletin, 2009; 135: 531–554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Coulter A, Ellins J. Effectiveness of strategies for informing, educating, and involving patients. BMJ, 2007; 335: 24–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Cameron K, Ross E, Clayman M, Bergeon A, Federman A, Bailey S, et al Measuring patients' self‐efficacy in understanding and using prescription medication. Patient Education & Counseling, 2010; 80: 372–376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Donovan‐Kicken E, Mackert M, Guinn T, Tollison A, Breckinridge B, Pont S. Health literacy, self‐efficacy, and patients' assessments of medical disclosure and consent documentation. Health Communication, 2012; 27: 581–590. [DOI] [PubMed] [Google Scholar]
- 31. Peek ME, Odoms‐Young A, Quin MT, Gorawara‐Bhat R, Wilson SC, Chin MH. Race and shared decision‐making perspectives of African Americans with diabetes. Social Science & Medicine, 2010; 71: 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Polacek GNL, Romas MC, Ferrer RL. Breast cancer disparities and decision‐making among US women. Patient Education and Counseling, 2007; 65: 158–165. [DOI] [PubMed] [Google Scholar]
- 33. Golin C, DiMatteo M, Gelberg L. The role of patient participation in the doctor visit: Implications for adherence to diabetes care. Diabetes Care, 1996; 19: 1153–1164. [DOI] [PubMed] [Google Scholar]
- 34. Baker TA, O'Connor ML, Roker R, Krok JL. Satisfaction with pain treatment in older cancer patients: Identifying variants of discrimination, trust, communication, and self‐efficacy. Journal of Hospice & Palliative Nursing, 2013; 15: 455–463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Steinberg ML, Fremont A, Khan DC, Huang D, Knapp H, Karaman D, et al Lay patient navigator program implementation for equal access to cancer care and clinical trials. Cancer, 2006; 11: 2669–2677. [DOI] [PubMed] [Google Scholar]
- 36. Wolf M, Chang C, Davis T, Makoul G. Development and validation of the communication and attitudinal self‐efficacy scale for cancer (CASE‐cancer). Patient Education and Counseling, 2005; 57: 333–341. [DOI] [PubMed] [Google Scholar]
- 37. Hayes A, Preacher K. Quantifying and testing indirect effects in simple mediation models when the constituent paths are nonlinear. Multivariate Behavioral Research, 2010; 45: 627–660. [DOI] [PubMed] [Google Scholar]
- 38. Sobel ME. Direct and indirect effects in linear structural equation models. Sociological Methods & Research, 1987; 16: 155–176. [Google Scholar]
- 39. Schafer J, Graham J. Missing data: our view of the state of the art. Psychological Methods, 2002; 7: 147–177. Epub 2002/07/02. [PubMed] [Google Scholar]
- 40. Levinson W, Kao A, Kuby A, Thisted RA. Not all patients want to participate in decision making: a national study of public preferences. Journal of General Internal Medicine, 2005; 20: 531–535. [DOI] [PMC free article] [PubMed] [Google Scholar]


