Abstract
Brief interventions aimed at reducing alcohol use among youth may interrupt a possible developmental progression to more serious substance use if they can also affect the use of other illicit drugs. This meta-analysis examined the findings of recent research on the effects of brief alcohol interventions for adolescents and young adults on both alcohol and illicit drug use. Eligible studies were those using randomized or controlled quasi-experimental designs to examine the effects of brief alcohol interventions on illicit drug use outcomes among youth. A comprehensive literature search identified 30 eligible study samples that, on average, included participants age 17, with 57% male participants and 56% White youth. Three-level random-effects meta-analyses were used to estimate mean effect sizes and explore variability in effects. Overall, brief interventions targeting both alcohol and other drugs were effective in reducing both of these substances. However, the brief interventions that targeted only alcohol had no significant secondary effects on untargeted illicit drug use. The evidence from current research, therefore, shows modest beneficial effects on outcomes that are targeted by brief interventions for youth, but does not show that those effects generalize to untargeted illicit drug use outcomes.
Keywords: alcohol use, brief intervention, drug use, meta-analysis, systematic review
INTRODUCTION
Alcohol and illicit drug use are often initiated during the critical developmental periods of adolescence and early adulthood. In 2012, an estimated 15% of 12–20 year olds reported binge drinking in the past month (five or more drinks on the same occasion) and 4% could be classified as heavy drinkers (five or more drinks on the same occasion for five or more days) (SAMHSA 2013). Further, among youth aged 12–17, 7.2% used marijuana and 9.5% used some illicit substance in the past month; for young adults aged 18–25, an estimated 18.7% used marijuana and 21.3% used some illicit substance in the past month (SAMHSA 2013). Heavy alcohol and other illicit drug use by youth has been linked to numerous detrimental consequences, including academic problems, cognitive or neurological impairments, delinquent or criminal behavior, injuries, and risky sexual behaviors (e.g., Khan et al. 2012; Squeglia et al. 2009). Earlier ages of substance use initiation are also associated with higher likelihoods of subsequent substance use disorder diagnoses (SAMHSA 2013).
Adolescence is, therefore, a sensitive developmental period for interventions aimed at preventing the initiation of alcohol and other drug use, or interrupting the progression to clinical levels of substance use disorders in adulthood. One body of such approaches consists of brief interventions, defined broadly as interventions providing motivations and/or skills to promote behavior change in a relatively circumscribed time, typically between one to five sessions (CSAT 1999). Effective variants of brief interventions are especially attractive because of their brevity and ability to offer a cost- and time-efficient way to address a major public health issue (Fleming et al. 2000, 2002; Neighbors et al. 2010). Although some brief interventions for youth may only target a particular illicit drug (e.g., Stein et al. 2011; Walters et al. 2012), most target alcohol by itself or in combination with other drugs. The emphasis on alcohol is not surprising given the high prevalence of alcohol use among youth (SAMHSA 2013) and the fact that alcohol consumption is one of the top risk factors for global disease burden (World Health Organization 2009). Moreover, there are numerous settings (e.g., pediatric or school health clinics, juvenile diversion programs, emergency rooms) in which interventions targeting alcohol may be more appropriate or feasible to implement with youth (Winters et al. 2014).
Although evidence suggests that brief interventions can be effective in reducing alcohol consumption, it is unclear whether those with a focus on alcohol can also affect other risky substance use behaviors such as marijuana, cocaine, or other drug use. Given the scarce resources available for early intervention efforts, it is important to understand whether brief alcohol interventions might be simultaneously effective for a range of drug use outcomes. The current study sought to address this question by synthesizing findings from empirical studies identified in a larger systematic review of brief alcohol interventions for youth.
BRIEF ALCOHOL INTERVENTIONS
Although there is no universal definition of a brief intervention, they typically consist of one to five sessions delivered by an interventionist such as a physician, nurse, or psychologist (CSAT 1999). By definition, brief interventions are short in contact time, but can vary in structure, targets, delivery personnel, media communication, underpinning theory, and intervention philosophy (Heather 1995). Brief interventions are most often based on the principles of cognitive behavioral therapy, motivational enhancement therapy (Miller and Rollnick 1991), and/or the transtheoretical model of behavior change (Prochaska and DiClemente 2005), which emphasize the importance of stimulating participants’ abilities, capacities, and motivations to self-evaluate and self-regulate their behaviors. Because brief interventions are typically not intended to provide a full treatment regimen for youth with alcohol use disorders, they can be used as universal, selective, or indicated prevention strategies (CSAT 1999).
Brief interventions often include multiple therapeutic components designed to provide skills or enhance motivations for behavior change. These therapeutic components might include baseline assessments used to generate personalized feedback comparing participants’ substance use with salient reference groups (e.g., same gender, same age peers). Other activities often include goal-setting exercises (e.g., establishing target consumption levels), decisional balance exercises (e.g., listing pros and cons of substance use), discussion of moderation strategies (e.g., tips for alternating alcoholic drinks with water), and basic provision of information (e.g., how to calculate blood alcohol concentration, money spent on substances). Brief interventions that simultaneously target alcohol and other illicit drugs (i.e., “multi-targeted” interventions) may use various combinations of these therapeutic components, some of which might focus explicitly on alcohol (e.g., calculating blood alcohol concentration levels), on other drugs (e.g., listing pros and cons of marijuana use), or on alcohol and drugs together (e.g., calculating money spent on any substance). Regardless of whether these therapeutic components target alcohol or other illicit drugs, their ultimate aim is to provide skills and bolster motivations to change risky behaviors.
Although brief interventions often include multiple therapeutic components (e.g., personalized feedback combined with decisional balance and goal-setting exercise), some intervention components may be more developmentally appropriate for youth than others. For instance, the dual systems model of adolescent risk-taking (Steinberg 2010) highlights adolescents’ susceptibility to risky behaviors stemming from asynchrony in the development of brain systems that respond to incentives versus those that regulate cognitive control and response inhibition (Somerville et al. 2010). Given adolescents’ heightened reward sensitization and inhibited impulse control, intervention components that address peer-related stimuli and/or bolster cognitive control over urges may be particularly effective during this developmental stage (Albert et al. 2013; Wetherill and Tapert 2013).
Secondary effects of brief interventions
Ample evidence shows that brief interventions that target alcohol use can be effective in reducing alcohol consumption among adolescents and young adults (Tanner-Smith and Lipsey 2014). It is unclear, however, whether brief alcohol interventions can, at the same time, also affect other risky substance use behaviors, e.g., marijuana, cocaine, or other illicit drug use. One way this could occur is through participants’ generalization of the alcohol message to other substances. For instance, the motivations and skills for behavior change induced by an alcohol-related goal-setting exercise might seamlessly generalize to other drug use: setting the goal “Next week I will reduce the number of days I drink from five to three” may stimulate youth to also set the goal “Next week I will reduce the number of days I smoke marijuana from five to three.” Alcohol and drug use co-occur during adolescence and early adulthood (SAMHSA 2013), and share a range of common risk and protective factors related to peer-related stimuli and poor impulse control (e.g., Beyers et al. 2004; Clark and Winters 2002). As such, youth receiving brief alcohol-focused interventions might generalize skills and behavior change techniques to other co-occurring risk behaviors. Given the limited resources available for prevention and early intervention efforts, it is important to understand whether brief interventions that target the widespread problem of alcohol use among adolescents and young adults might simultaneously be effective for other drug use outcomes. Such generalization or spillover effects would clearly be desirable to program implementers for improving the health and well-being of youth.
For multi-targeted brief interventions (i.e., those that that simultaneously target alcohol and other illicit drugs), it is important to understand not only whether they can be effective in reducing both alcohol and drug use, but also whether such multi-targeting diminishes effects on alcohol outcomes. Broadening the focus of the brief intervention might detract from the alcohol emphasis and compromise the effectiveness of the intervention for reducing alcohol use. That would be an undesirable side effect of a multi-targeted brief intervention in contexts where alcohol use was the primary concern in the target population.
Current evidence on effectiveness
Since the launch of the Substance Abuse and Mental Health Service Administration’s Screening, Brief Intervention, and Referral to Treatment Initiative in 2003 (SAMHSA 2014), the body of methodologically rigorous research on the effects of brief alcohol interventions for youth has expanded. In one of the most comprehensive research syntheses to date (and the larger project from which the current meta-analysis draws), Tanner-Smith and Lipsey (2014) summarized findings from 185 research samples that examined the effects of brief alcohol interventions for youth ages 12–30. The results demonstrated that brief alcohol interventions produced significant reductions in both alcohol consumption and alcohol-related consequences among youth, with consistent effects across interventions of different duration and persisting for up to one year after the intervention. The results also indicated that some therapeutic components, notably decisional balance and goal-setting exercises, were associated with larger beneficial effects. These results were generally consistent with findings from other research syntheses (Carey et al. 2007; Carey et al. 2009; Jensen et al. 2011; Moreira et al. 2009; Tait and Hulse 2003). Prior reviews have also found that brief alcohol interventions can affect other proximal outcomes such as alcohol-related knowledge, attitudes toward drinking, normative alcohol beliefs, and intentions to reduce alcohol consumption (Scott-Sheldon et al. 2009).
Little summary evidence is available, however, about whether brief alcohol interventions can have secondary effects on other outcomes. One meta-analysis of brief alcohol interventions for adults found beneficial secondary effects on overall mortality rates (Cuijpers et al. 2004). McCambridge and Jenkins (2008), on the other hand, found no evidence of secondary effects on untargeted smoking cessation outcomes in their meta-analysis of brief alcohol interventions for adults. They concluded that brief alcohol interventions do not have effects on untargeted behaviors. Nevertheless, it would be premature to generalize this conclusion to youth or to other untargeted secondary outcomes like illicit drug use. Nor do these findings address the question of whether brief interventions that target use of other drugs as well as alcohol have effects on both. The present study attempts to address these gaps by examining whether brief alcohol interventions can have secondary effects on illicit drug use among youth, an important issue given the critical developmental considerations necessary for behavioral interventions with youth.
The Present Study
This study used meta-analytic methods to synthesize findings from research that reported the effects of brief alcohol interventions on both alcohol and other illicit drug use. Specifically, this meta-analysis addressed three research questions. First, what are the effects of brief alcohol interventions (which may or may not simultaneously target illicit drug use) on youth’s subsequent alcohol/drug use? Understanding whether brief alcohol intervention effects can generalize to secondary or untargeted outcomes has important implications for developmentally appropriate intervention programming for youth. Second, does the presence/absence of particular therapeutic intervention components (e.g., decisional balance, goal-setting exercises) moderate the effects of brief alcohol interventions? Some intervention components may be more developmentally appropriate for youth than others, and hence more effective, so it is crucial to explore which components might yield the largest beneficial effects. Finally, does intervention duration or follow-up timing moderate the effects of brief alcohol interventions? Understanding the optimal length of a brief intervention and the persistence of effects should advance knowledge about how best to affect risky substance use behavior among youth. This study does not address whether brief interventions targeting illicit drug use, but not alcohol use, are effective (see instead Burke et al. 2004; Carney and Myers 2012; Jensen et al. 2011; Smedslund et al. 2011). Rather, this study assesses whether brief alcohol interventions that explicitly target alcohol use can also lead to reductions in illicit drug use.
METHOD
INCLUSION AND EXCLUSION CRITERIA
For this analysis, we used data collected from studies identified in a larger systematic review of brief alcohol interventions for adolescents and young adults (Tanner-Smith and Lipsey 2014). To be included in the larger review, primary studies had to meet the following eligibility criteria: (1) evaluate a brief intervention designed to have beneficial effects on participants’ alcohol use or alcohol-related consequences (with a primary intervention focus on alcohol); (2) have no more than five hours of total intervention contact time and no more than four weeks in duration between the first and last session; (3) use a randomized or quasi-experimental research design that included a comparison condition of no treatment, wait-list control, or some form of treatment as usual; (4) focus on youth age 11–25, or on samples of undergraduate college students no older than age 301; (5) assess the effects on at least one alcohol or alcohol related problem outcome; (6) be conducted in 1980 or later, to ensure applicability to current youth.
The meta-analysis reported here included those studies that met all the above eligibility criteria and also assessed effects on at least one illicit drug use outcome. We also included an additional group of studies that were not part of the larger parent review because they evaluated a brief intervention that targeted both alcohol and illicit drug use (i.e., they failed eligibility criterion 1 above), but met all other aforementioned eligibility criteria. Because this research involved secondary analysis of existing research documents, it was not considered human subjects research per CFR 46.102(f)(2).
SEARCH STRATEGIES
Studies were identified via the comprehensive literature search used in the parent meta-analysis that was designed to detect all relevant published and unpublished studies current through December 31, 2012. The following electronic databases were searched: CINAHL, Clinical Trials Register, Dissertation Abstracts International, ERIC, International Bibliography of the Social Sciences, NIH RePORTER, PsycARTICLES, PsycINFO, PubMed, Social Services Abstracts, Sociological Abstracts, and WorldWideScience.org. Several additional grey literature sources were searched, e.g., Australasian Medical Index, Google Scholar, Index to Theses in Great Britain and Ireland, International Clinical Trials Registry, KoreaMed, and online conference proceedings (see Tanner-Smith and Lipsey 2014 for complete details). We checked the bibliographies of all screened and eligible studies, as well as the bibliographies in prior narrative reviews and meta-analyses. We also conducted hand-searches on the table of contents from key journals in the field.
Coding Procedures
Six researchers (graduate students and master’s level research scientists) first screened all abstracts/titles to eliminate any clearly irrelevant study reports. For training purposes, each of the six screened the abstracts/titles of 500 randomly selected reports; all disagreements were discussed until 100% consensus was reached. The remaining abstracts/titles were then screened by one person with all decisions reviewed by the first author and any disagreements discussed until consensus was reached. If there was any ambiguity about the potential eligibility of a report based on the abstract, we erred on the side of inclusivity and retrieved the full text report before making the eligibility decision. We retrieved the full text for all reports that were not explicitly ineligible at the abstract screening phase. The same six researchers then screened the full text reports to make final eligibility decisions using the same procedure. Again, the first author served as a second screener for all full text eligibility decisions.
The coding of information from the eligible studies used a computer-based protocol and was conducted by six coders who participated in several weeks of initial training led by the first author and weekly coding meetings thereafter. During initial training, five studies were coded by all coders, who then convened as a group to resolve any coding discrepancies until 100% consensus was attained on all coded variables. After the training period, all coding questions were addressed in weekly meetings and decided via consensus with the group. The first author double-checked all of the coding, and resolved any further discrepancies via consensus with the first coder.
MODERATORS
Based on prior theory and research on brief intervention effectiveness for youth (e.g., CSAT 1999; Tanner-Smith and Lipsey 2014), the following intervention characteristics were explored as potential effect size moderators: presence/absence of specific alcohol- or drug-related therapeutic components (decisional balance exercise, generic education/information about use, goal-setting/contracting exercise, identifying high-risk situations, information on consequences of heavy use, information about risk factors for use disorders or related consequences, moderation strategies discussion, local/national norm referencing of use levels, and personalized feedback on use levels); length between intervention end and posttest measurement (weeks); and intervention duration (minutes).
Although not explicitly framed as effect size moderators, the following methodological characteristics were coded and used in analysis as covariate controls given that prior meta-analyses on this topic have demonstrated their importance (e.g., Carey et al. 2007; Carey et al. 2009; Jensen et al. 2011; Tanner-Smith and Lipsey 2014): study design (randomized control trial vs. quasi-experimental); attrition; whether binary data were used to estimate the effect size; whether the effect size was based on pretest adjusted data; type of control group (no treatment versus treatment as usual); and the standardized mean difference effect size measuring pretest differences in groups.
STATISTICAL METHODS
Effect size metric
The outcomes of interest were measured with standardized mean difference effect sizes (Hedges’ g; Hedges 1981), coded so that positive effect sizes represent better outcomes (e.g., less drug use, higher abstinence). We used the Cox transformation outlined by Sánchez-Meca and colleagues (2003) to transform effect sizes and standard errors for any binary outcomes. Effect size and sample size outliers (defined as three interquartile ranges beyond the upper/lower fences of the distributions) were Winsorized to less extreme values to prevent distortion of the meta-analysis results (Lipsey and Wilson 2001).
Because effect sizes can be influenced by the methodological characteristics of the studies, all analyses used method-adjusted effect sizes that held effect sizes at the following values: randomized study design, binary data not used to estimate effect size, effect size adjusted for pretest differences, no-treatment control condition, no pretest differences, and average level of attrition. This was done by predicting the effect sizes from only these variables, retaining the residuals, and adding each residual to the constant from the prediction model corresponding to the selected values on the covariates (see Tanner-Smith and Lipsey 2014 for the estimation model). This conservative technique ensures that any variance in effect sizes associated with differences in method between studies is removed from the analysis of the influence of substantive variables on those effect sizes.
Missing data
When primary studies failed to include enough statistical information to estimate effect sizes, we contacted the study authors for that information. If the authors were unresponsive or unable to provide the requested effect size data, we dropped those studies from the analysis. There was a small amount of missing data for two of the study characteristics (attrition; pretest effect sizes) used in the method-adjustment procedure described above. For these variables, we imputed missing data using an expectation-maximization algorithm (Allison 2002) so that all cases could be included within any given analysis (see Tanner-Smith and Lipsey 2014).
Analytic strategies
Most studies reported multiple measures of alcohol consumption (e.g., frequency of consumption, quantity consumed, blood alcohol concentration), and/or multiple measures of illicit drug use. We therefore used a three-level random-effects meta-analysis approach to model the dependent effect sizes (Cheung 2014b; Konstantopoulos 2011; Van den Noortgate et al. 2013), where primary study participants (Level 1) provide multiple effect size estimates (Level 2), which are nested within studies (Level 3). The three-level meta-analyses were estimated using the metasem package in R (Cheung 2014a, 2014b). The three-level meta-analytic model can be written as:
where yij is the ith effect size in the jth study; β0 is the average population effect; u(2)ij and u(3)j are the Level 2 and Level 3 random effects such that Var(u(2)ij) = τ2L2 and Var(u(3)j) = τ2L3 are the within-study and between-study variance components; and eij is the residual for the ith effect size in the jth study. This model can then be extended to include a study level covariate xj, where:
These three-level meta-regression models were used to summarize the overall effects of brief alcohol interventions on illicit drug use and alcohol use, and the potential moderating effects of intervention components, duration, and follow-up timing.
RESULTS
LITERATURE SEARCH
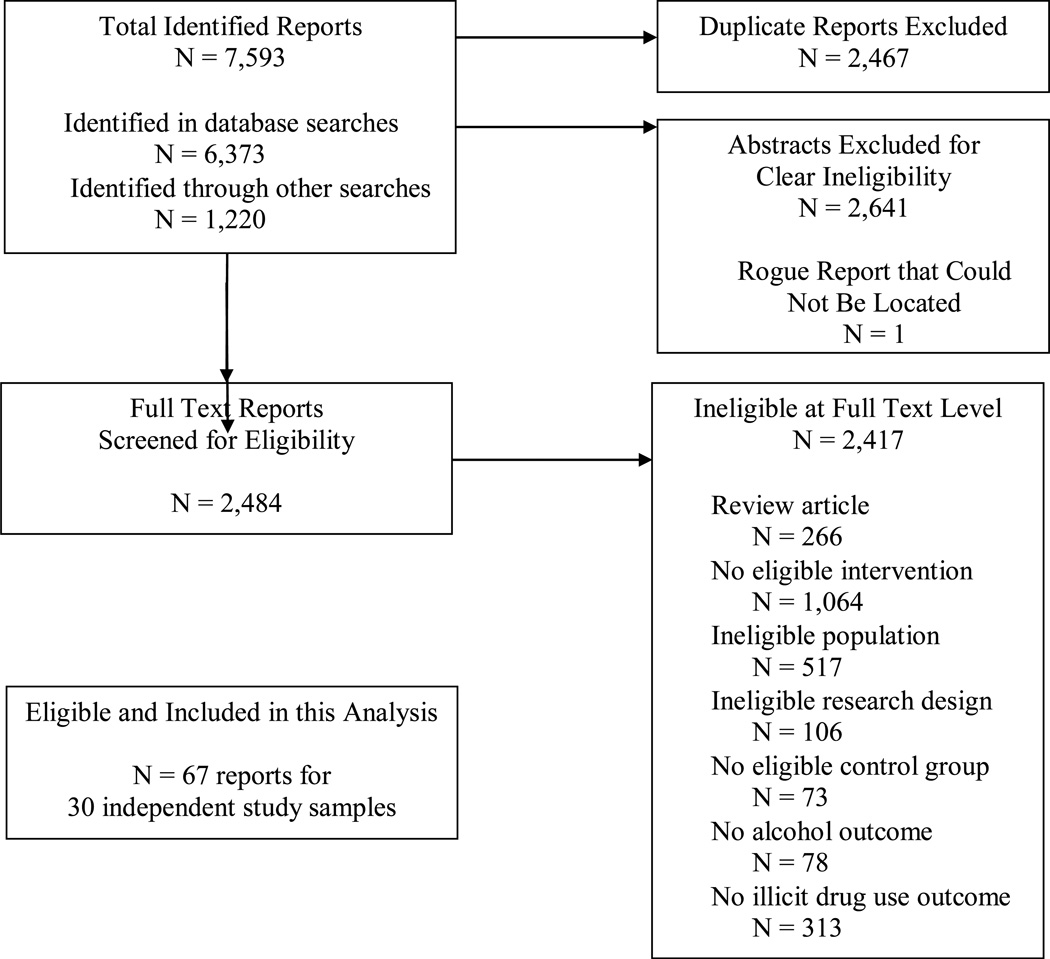
In the larger parent systematic review, 7,593 reports were identified in the literature search, 2,467 of which were duplicates and dropped from consideration, and 2,641 that were screened as ineligible at the abstract phase (see Figure 1). Of the 2,484 articles retrieved in full text format, 2,417 were deemed ineligible for the current study. Thus, this meta-analysis synthesizes findings from 30 study samples reported in 67 documents (see online Appendix A for references to reports from eligible studies that provided effect size data). Seven of the eligible studies involved brief interventions that primarily targeted alcohol consumption, and 23 involved brief interventions that targeted both alcohol and other drug use.
FIG. 1.
STUDY IDENTIFICATION FLOW DIAGRAM
STUDY CHARACTERISTICS
Table 1 presents descriptive characteristics of the studies included in the meta-analysis, shown separately for the 7 alcohol only targeted interventions and the 23 multi-targeted (alcohol and other drug) interventions. The majority of studies were conducted in the United States, were published in peer-reviewed journals, were randomized controlled trials, had low attrition rates, and reported effects approximately 6-months after the end of the intervention. The most common intervention modality was motivational interviewing/motivational enhancement therapy (MET), although a few studies used a combination of MET and cognitive behavioral therapy, feedback only, or generic psycho-education. Most interventions were conducted in high school or university settings and were delivered individually with the participant and provider. The average number of sessions in which the interventions were delivered was one and the average contact time per session was 50 minutes (alcohol targeted) or 59 minutes (multi-targeted).
Table 1.
Characteristics of the Studies, Participant Samples, and Interventions in the Meta-analysis, by Brief Intervention Target
| Intervention Target: Alcohol k = 7 |
Intervention Target: Alcohol & Other Drugs k = 23 |
||||
|---|---|---|---|---|---|
| M | SD | M | SD | Range | |
| Study/Design Characteristics | |||||
| Publication year a | 2008 | 5.53 | 2008 | 3.03 | 1996–2012 |
| U.S. sample (% yes) a | .57 | 0.53 | .57 | 0.51 | 0 – 1 |
| Journal article publication (% yes) a | .86 | 0.38 | .87 | 0.34 | 0 – 1 |
| Randomized controlled trial (% yes) a | .86 | 0.38 | .87 | 0.34 | 0 – 1 |
| Percent attrition b | .19 | 0.10 | .12 | 0.12 | 0 – .42 |
| Post-intervention follow-up, in weeks b | 30.52 | 16.81 | 26.28 | 23.77 | 1 – 103.2 |
| No treatment control condition (% yes) b | .52 | 0.51 | .37 | 0.49 | 0 – 1 |
| Pretest effect size b | 0.11 | 0.23 | 0.03 | 0.35 | −1.1 – 1.3 |
| Participant Characteristics c | |||||
| Average age | 17.36 | 2.68 | 16.66 | 1.72 | 13.5 –20.5 |
| Percent male composition | .59 | 0.26 | .55 | 0.20 | 0 – 1 |
| Percent White composition | .53 | 0.35 | .56 | 0.23 | 0 – 1 |
| High-risk screened sample (% yes) | .30 | 0.47 | .18 | 0.39 | 0 – 1 |
| Intervention Modality c | |||||
| MET (% yes) | .88 | 0.35 | .76 | 0.44 | 0 – 1 |
| MET + cognitive behavioral therapy (% yes) | .00 | - | .07 | 0.26 | |
| Feedback/information only (% yes) | .00 | - | .07 | 0.26 | 0 – 1 |
| Psycho-educational therapy (% yes) | .13 | 0.35 | .07 | 0.26 | 0 – 1 |
| Intervention Site c | |||||
| Primary care (% yes) | .00 | - | .21 | 0.41 | 0 – 1 |
| School/university (% yes) | .63 | 0.41 | .51 | 0.51 | 0 – 1 |
| Self-administered (% yes) | .00 | - | - | 0 – 1 | |
| Emergency room (% yes) | .13 | 0.35 | .03 | 0.19 | 0 – 1 |
| Other (% yes) | .25 | 0.46 | .21 | 0.41 | 0 – 1 |
| Intervention Format c | |||||
| Participant alone –computerized (% yes) | .00 | - | .03 | 0.19 | 0 – 1 |
| Participant with provider (% yes) | .88 | 0.35 | .76 | 0.44 | 0 – 1 |
| Group with provider (% yes) | .13 | 0.35 | .17 | 0.38 | 0 – 1 |
| Family with provider (% yes) | .00 | - | .03 | 0.19 | 0 – 1 |
| Intervention Length c | |||||
| Duration (minutes) | 50.08 | 55.57 | 60.61 | 59.46 | 2.5 – 200 |
| Total number of sessions | 1.13 | 0.35 | 1.48 | 0.91 | 1 – 4 |
k = number of studies. MET = Motivational enhancement therapy
Estimates calculated at study level
Estimates calculated at effect size level
Estimates calculated at intervention group level
OVERALL EFFECTS
Interventions targeting only alcohol
The mean of the 27 method-adjusted effect sizes2 for all illicit drug use outcomes from the 7 interventions that only targeted alcohol (see Table 2) was close to zero (ḡ= −0.00, 95% CI [−0.14, 0.13], τ2L3 = 0.001, Q = 26.53). The mean of the 13 effect sizes for marijuana use outcomes was similar in magnitude (ḡ = 0.00, 95% CI [−0.07, 0.07], τ2L3 = 0.00, Q = 11.71). The mean of the 10 effect sizes for specific drugs other than marijuana was negative, small, and not statistically significant (ḡ = −0.04, 95% CI [−0.10, 0.02], τ2L3 = 0.00, Q = 6.62). Although these null findings should be interpreted cautiously given the small number of studies, the consistent homogeneity in the effect sizes (as evidenced by the Q, τ2, and I2 values; see Table 2) is notable and indicates that these null effects were consistent across studies and outcome type. Of course, it is important to remember that these brief interventions only targeted alcohol use, and they were indeed effective in reducing alcohol use among participants (ḡ = 0.20, 95% CI [0.13, 0.26], τ2L3 = 0.01, Q = 104.04). Thus, although brief alcohol targeted interventions were successful in leading to significant reductions in youth’s alcohol consumption, there was no evidence that they had secondary effects on untargeted illicit drug use outcomes.
Table 2.
Mean Method-Adjusted Effect Sizes and Heterogeneity Statistics, by Brief Intervention Target and Type of Illicit Drug Use Outcome
| Intervention Target: Alcohol |
Intervention Target: Alcohol & Other Drugs |
|||||||
|---|---|---|---|---|---|---|---|---|
| Any Illicit Drug Use |
Marijuana Use |
Other Hard Drug Use |
Alcohol Use |
Any Illicit Drug Use |
Marijuana Use |
Other Hard Drug Use |
Alcohol Use |
|
| ḡ | −0.00 | 0.00 | −0.04 | 0.20* | 0.13* | 0.15* | 0.44* | 0.17* |
| 95% CI | [−0.14, 0.13] | [−0.07, 0.07] | [−0.10, 0.02] | [0.13, 0.26] | [0.03, 0.22] | [0.02, 0.28] | [0.20, 0.67] | [0.05, 0.30] |
| k | 7 | 7 | 2 | 7 | 23 | 19 | 4 | 23 |
| n | 27 | 13 | 10 | 54 | 121 | 58 | 25 | 128 |
| Qdf | 26.5326 | 11.7112 | 6.629 | 104.0453* | 249.50120* | 138.357* | 40.5324* | 747.40127* |
| τ2L2 | 0.001 | 0.00 | 0.00 | 0.01 | 0.00 | 0.00 | 0.00 | 0.04 |
| I2L2 | 10.00 | 2.00 | 0.00 | 44.70 | 0.00 | 0.00 | 0.00 | 30.00 |
| τ2L3 | 0.00 | 0.00 | 0.00 | 0.001 | 0.04 | 0.07 | 0.05 | 0.07 |
| I2L3 | 0.00 | 0.00 | 0.00 | 4.79 | 65.00 | 75.00 | 61.00 | 58.00 |
ḡ = mean effect size; k = number of studies; n = number of effect sizes; Qdf = Q-statistic for effect size homogeneity; τ2L2 = within-study between-effect size variance component; I2L2 = proportion of true within-study between-effect size variance; τ2L3 = between-study variance component; I2L3 = proportion of true between-study variance. “Any illicit drug use” category includes marijuana use, other hard drug use, or any other mixed substance use outcomes.
p < .05
Interventions targeting both alcohol and illicit drugs
As shown in the right panel of Table 2, the mean of the 121 method-adjusted effect sizes for all illicit drug outcomes from the 23 multi-targeted studies was positive and statistically significant (ḡ = 0.13, 95% CI [0.03, 0.22], τ2L3 = 0.00, Q = 249.50). Further division of the effect sizes by illicit drug outcome type showed significant means for the 58 effect sizes for marijuana use (ḡ = 0.15, 95% CI [0.02, 0.28], τ2L3 = 0.00, Q = 138.3) and the 25 effect sizes for other hard drug use (ḡ = 0.44, 95% CI [0.20, 0.67], τ2L3 = 0.00, Q = 40.53). Not only were these multi-targeted interventions effective in reducing illicit drug use, but they were also effective in reducing alcohol use (ḡ = 0.17, 95% CI [0.05, 0.30], τ2L3 = 0.04, Q = 747.40). Thus, brief interventions that targeted both alcohol and illicit drug use were successful in improving both of those targeted behaviors.
The average effect of multi-targeted brief interventions on alcohol use was smaller than that for alcohol only focused interventions (0.17 vs. 0.20, respectively; Table 2), indicating a possible dilution of effects in the multi-targeted interventions. We therefore conducted a post hoc moderator analysis to examine whether these mean effects were significantly different from each other. Results from a meta-regression model predicting all alcohol effect sizes provided no evidence that intervention effects on alcohol use were different for the single-target versus multi-targeted interventions (b = 0.09, 95% CI [−0.12, 0.30]).
VARIABILITY IN EFFECTS
Given the lack of variability in effects for the small number of interventions targeting only alcohol, we elected to examine variability in effects only for the multi-targeted interventions. For these studies, we examined whether any of the intervention components identified a priori moderated the effectiveness of the interventions on youth’s illicit drug use (Table 3), distinguishing between whether or not those components focused on alcohol use or drug use.3 As shown in the left panel of Table 3, there were only two alcohol-focused therapeutic components associated with intervention effects on youth’s illicit drug use at a statistically significant level. Interventions that included the identification of high-risk drinking situations showed larger effects on subsequent illicit drug use (b = 0.17, 95% CI [0.01, 0.33]), as did those that provided information about the consequences of heavy drinking (b = 0.19, 95% CI [0.01, 0.37]). As shown in the right panel of Table 3, the presence of only one drug-focused therapeutic component was associated with the effects on illicit drug use: interventions that involved discussion of drug moderation strategies showed larger effects on subsequent illicit drug use (b = 0.33, 95% CI [0.12, 0.54]). Otherwise, there was no evidence that the presence/absence of the other therapeutic components were associated with effects on youth’s illicit drug use outcomes.
Table 3.
Effects of Therapeutic Intervention Components on Drug Use Effect Sizes, for Interventions Targeting Alcohol & Other Drugs (k = 23, n = 121)
| Alcohol-Focused Components |
Drug-Focused Components |
|||
|---|---|---|---|---|
| Therapeutic component | b | 95% CI | b | 95% CI |
| Decisional balance exercise | 0.12 | [−0.07, 0.31] | 0.07 | [−0.03, 0.23] |
| Generic education/information | 0.07 | [−0.08, 0.22] | 0.16 | [−0.02, 0.34] |
| Goal-setting exercise | 0.08 | [−0.10, 0.26] | 0.16 | [−0.03, 0.36] |
| Identifying high-risk situations | 0.17* | [0.01, 0.33] | 0.10 | [−0.11, 0.32] |
| Information on consequences of heavy use | 0.19* | [0.01, 0.37] | - | |
| Information on risk factors for use disorders | −0.04 | [−0.23, 0.16] | −0.14 | [−0.40, 0.13] |
| Moderation strategies discussion | 0.12 | [−0.16, 0.39] | 0.33* | [0.12, 0.54] |
| Norm referencing related | −0.06 | [−0.27, 0.15] | −0.14 | [−0.35, 0.08] |
| Personalized feedback about use | 0.11 | [−0.06, 0.28] | 0.13 | [−0.07, 0.33] |
b = unstandardized meta-regression coefficient; k = number of studies, n = number of effect sizes. Coefficients are from bivariate meta-regression models examining the effects of a single therapeutic intervention component, in turn. Results not estimable for information on consequences of heavy drug use because no studies reported that therapeutic component for drug use.
p < .05
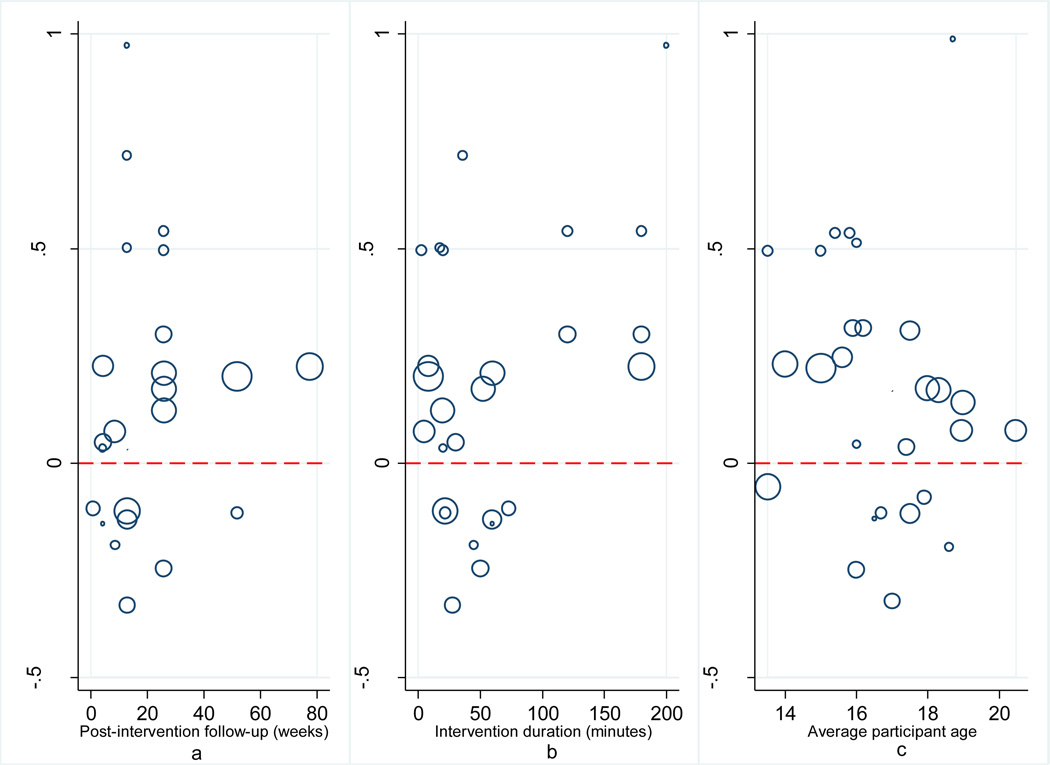
We next examined whether follow-up timing or intervention length (Figure 2, panels a and b) were associated with the effects of the multi-targeted interventions on illicit drug use outcomes. There was no evidence that effect size magnitude was associated with the timing of the posttest follow-up measurement (b = 0.00, 95% CI [−0.001, 0.001]), or intervention length (b = 0.00, 95% CI [−0.001, 0.004]).
Fig. 2.
Scatterplot of Method-Adjusted Effect Sizes, Intervention Follow-up Timing, Intervention Duration, and Participant Age
Notes The figures depict the average effect size for each unique study sample at each (a) follow-up wave (b) intervention duration and (c) average participant age. Effects are shown proportionate to each study’s average weight in the meta-analysis.
Given the wide age range of participants in the included studies, we also conducted post hoc analyses to examine whether participant age was associated with the effects of multi-targeted interventions on illicit drug use outcomes (Figure 2, panel c). There was no evidence that effect size magnitude was associated with the average age of participants in the studies (b = −0.02, 95% CI [−0.07, 0.04]).
SENSITIVITY ANALYSES
Publication bias, or the tendency to publish research findings that are statistically significant and/or are confirmatory in direction, is important to consider in any meta-analysis (Rothstein et al. 2005). We therefore used a contour-enhanced funnel plot (Palmer et al. 2008) and trim and fill analysis (Duval and Tweedie 2000) to explore the possibility of small study bias, or the potential for the meta-analysis results to be biased due to omission of studies with small sample sizes and null/negative results (not shown, available upon request). We used one synthetic mean effect size per study, examining effects separately for the alcohol and drug use effect sizes. The funnel plots for both types of outcomes were asymmetric, indicating possible small study bias. However, there was a general lack of small sample size studies reporting statistically significant effects (positive or negative). Further, results from the trim and fill analyses provided no strong evidence of publication bias, such that the average effect sizes for alcohol use and any illicit drug use reported in Table 2 were substantively unchanged after the trim and fill procedure.
Discussion
Alcohol and illicit drug use are major public health concerns during the sensitive developmental periods of adolescence and early adulthood. Brief alcohol interventions are one promising approach for preventing the initiation of alcohol use, or interrupting the progression to clinical levels of alcohol use disorders. Despite cogent evidence that brief alcohol focused interventions can reduce alcohol use among youth (Carey et al. 2009; Tait and Hulse 2003; Tanner-Smith and Lipsey 2014), to date it has been unclear whether these interventions can have secondary effects on other illicit drug use outcomes. Such generalization or spillover effects would be desirable for researchers and practitioners interested in maximizing the health benefits of preventive interventions for youth.
This meta-analysis synthesized findings from 30 experimental and quasi-experimental studies about the effects of brief alcohol interventions on illicit drug use among youth. Some of those interventions (k = 7) only targeted alcohol but also examined outcomes for other drugs; others (k = 23) targeted both alcohol and other drugs and measured outcomes for both. Overall, results indicated that brief interventions were effective in changing the targeted substance use behaviors, but not the untargeted ones. Namely, brief alcohol-targeted interventions were effective in reducing alcohol use, but had negligible effects on untargeted illicit drug use. Likewise, brief interventions that targeted both alcohol and illicit drugs were effective in reducing both of those targeted outcomes. Results across studies were remarkably homogeneous, and there was little evidence that effects varied according to the presence/absence of several therapeutic intervention components, time until follow-up, intervention length, and average age of participants.
For the alcohol outcomes, these findings are consistent with prior research indicating the effectiveness of brief alcohol interventions for reducing alcohol consumption among adolescents and young adults (Carey et al. 2007; Tait and Hulse 2003; Tanner-Smith and Lipsey 2014). Further, the results are consistent with prior evidence in adult populations that brief alcohol interventions do not have secondary effects on untargeted outcomes (McCambridge and Jenkins 2008). These results also mirror findings from prior meta-analyses of multi-targeted interventions for adolescents that have demonstrated positive but relatively small effects on substance use outcomes (Carney and Myers 2012; Hale et al. 2014; Jensen et al. 2011).
One concern about brief alcohol interventions that also target drug use is that this broader focus might diminish effects on alcohol outcomes. Namely, the minimal dosage of brief interventions may inherently limit the ability to address multiple targets simultaneously. Given the prevalence of heavy alcohol use among youth and the intent of these interventions to address that problem, any dilution of the effects on alcohol use would be a serious drawback for multi-targeted brief interventions. The evidence summarized in this meta-analysis, albeit somewhat limited, provides no cause for concern on this point. Although the mean effect size for alcohol outcomes was slightly smaller for interventions targeting both alcohol and other drugs than for those targeting only alcohol, that difference was not statistically significant nor is it likely to be substantively significant. Furthermore, the magnitude of effects on alcohol outcomes was similar to findings from the larger parent meta-analysis of brief alcohol interventions for youth (Tanner-Smith and Lipsey 2014). Although there is no evidence in the current study that multi-targeted interventions for alcohol and drugs lead to dilution in effects, more research is nevertheless needed to examine other possible dilution effects that may occur with different intervention targets relevant for adolescents and young adults (e.g., mental health, risky sexual behavior, nutrition).
Results from the current meta-analysis must be considered alongside the strengths and weaknesses of the study. The primary limitation of this meta-analysis was the relatively small number of studies of brief interventions targeting only alcohol that nonetheless also reported effects on illicit drug use outcomes (k = 7). Along with the homogeneity in observed effects from these seven studies, this small sample size precluded us from conducting any sophisticated moderator analysis. It is possible that some studies of alcohol-only targeted interventions assessed other drug outcomes but did not report them because the findings were null or negative, resulting in outcome reporting bias. Unfortunately, we are unable to assess potential reporting bias with the data available. Another limitation of this study is that the literature search is only current through December 31, 2012; newer studies on the topic may have since been reported that are not included in this research synthesis. It will therefore be important to update the current meta-analysis as new research becomes available on the generalization of brief alcohol intervention effects for youth.
Nonetheless, the primary strengths of this meta-analysis were the extensive systematic literature search used to identify all relevant studies on the topic, the application of advanced statistical techniques that permitted the inclusion of multiple effect sizes from each study, and the control of methodological confounds. Taken together, these strengths provide confidence that the results of the mean effect estimates and the exploratory moderator analyses used to examine variability in effects (or rather, the lack thereof) are representative of the current available research evidence.
CONCLUSIONS
Adolescence is a sensitive developmental period for interventions aimed at preventing the initiation of alcohol and other drug use. Given the limited time and resources available for implementing substance use prevention and early intervention efforts, brief interventions are gaining popularity as a cost-effective way to stimulate youth’s abilities and motivations to self-evaluate and self-regulate their substance-using behaviors. This meta-analysis provides a comprehensive synthesis of 30 study samples that examined the effects of brief alcohol interventions on illicit drug use for adolescents and young adults. The study’s results indicated that brief alcohol interventions that also target other drug use appear to be effective in improving both the targeted alcohol and other drug outcomes among youth. However, brief interventions with a sole alcohol focus do not appear to have spillover or generalized effects on untargeted illicit drug use. Researchers and practitioners can use these findings to further refine developmentally appropriate intervention strategies for reducing alcohol and drug use among youth. Namely, those advancing screening, brief intervention, and referral to treatment efforts may want to consider multi-targeted intervention strategies when both targeted outcomes are appropriate to the population and circumstances.
Supplementary Material
Acknowledgements
This work was supported by Award Number R01AA020286 from the National Institute on Alcohol Abuse and Alcoholism. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute on Alcohol Abuse and Alcoholism or the National Institutes of Health.
Footnotes
Research Interests
Emily Tanner-Smith major research interests include the social epidemiology, prevention, and treatment of adolescent substance use; and systematic reviewing and meta-analysis methodology.
Katarzyna Steinka-Fry primary research interests focus on program evaluation research in the areas of social and public health interventions.
Emily Hennessy main research interests are adolescent health and development within the school setting, including the evaluation of programs that encourage healthy choices among youth.
Mark Lipsey professional interests are in the areas of public policy, program evaluation research, social intervention, field research methodology, and research synthesis methods.
Ken C. Winters primary research interests are the assessment and treatment of adolescent drug abuse, including brief interventions.
We chose to include undergraduate college student samples given our conceptual interest in adolescents and young adults, and the fact that many primary studies recruited participants from undergraduate postsecondary educational institutions. Although living arrangements and opportunities for substance use will vary across these adolescent and young adult samples, the final analytic sample (see Table 1) ultimately only included studies with average ages up to 20.5. We also conducted post hoc analyses (see Figure 2) to establish that participant age was not associated with the magnitude of observed effect sizes.
Recall that all analyses use method-adjusted effect sizes that controlled for study design, attrition, effect size estimation method, comparison group type, pretest differences between groups, and level of estimation in effect size calculation. Sensitivity analyses (not shown) using the unadjusted effect sizes yielded results that were substantively similar to those reported here, so we elected to present the results using the method-adjusted effect sizes that offer a more conservative picture of effects, net of methodological confounds in the primary studies.
The moderator analyses predicted all illicit drug use effect sizes simultaneously; models were not estimated separately for subsets of marijuana or other hard drug use outcomes given the small number of available effect sizes within those subsets. Further, given the high intercorrelations between intervention components and the small number of available effect sizes, all moderator analyses examined the effect of only one therapeutic intervention at a time (i.e., it was not feasible to implement multivariable meta-regression models).
Author Contributions
ETS conceived of the study, participated in its design and coordination, performed the statistical analysis, and drafted the manuscript. KSF participated in the coordination of the study and helped draft the manuscript. EF participated in the coordination of the study and helped draft the manuscript. MWL participated in the design and coordination of the study, and edited the manuscript. KCW helped draft the manuscript. All authors read and approved the final manuscript.
KCW acknowledges that he is an author of two of the primary studies included in the meta-analysis but was not involved in extracting data from those studies; he has no other conflict of interest. ETS, KSF, EH, and MWL declare no conflicts of interest.
Contributor Information
Emily E. Tanner-Smith, Peabody Research Institute and Department of Human and Organizational Development at Vanderbilt University, Peabody Research Institute, Box 0181 GPC, Nashville, TN 37203-5721.
Katarzyna T. Steinka-Fry, Peabody Research Institute at Vanderbilt University, Peabody Research Institute, Box 0181 GPC, Nashville, TN 37203-5721.
Emily A. Hennessy, Community Research and Action program in the Department of Human and Organizational Development at Vanderbilt University, Peabody Research Institute, Box 0181 GPC, Nashville, TN 37203-5721.
Mark W. Lipsey, Peabody Research Institute at Vanderbilt University, Peabody Research Institute, Box 0181 GPC, Nashville, TN 37203-5721.
Ken C. Winters, Department of Psychiatry and Director of the Center for Adolescent Substance Abuse Research at the University of Minnesota Medical School, 2450 Riverside Avenue, Minneapolis, MN 55454.
References
- Albert D, Chein J, Steinberg L. The teenage brain: Peer influences on adolescent decision making. Current Directions in Psychological Science. 2013;22:114–120. doi: 10.1177/0963721412471347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allison PD. Missing data. Thousand Oaks, CA: Sage; 2002. [Google Scholar]
- Beyers JM, Toumbourou JW, Catalano RF, Arthur MW, Hawkins JD. A cross-national comparison of risk and protective factors for adolescent substance use: The United States and Australia. Journal of Adolescent Health. 2004;35:3–16. doi: 10.1016/j.jadohealth.2003.08.015. [DOI] [PubMed] [Google Scholar]
- Burke BL, Dunn CW, Atkins DC, Phelps JS. The emerging evidence base for motivational interviewing: A meta-analytic and qualitative inquiry. Journal of Cognitive Psychotherapy. 2004;18:309–322. [Google Scholar]
- Carey KB, Scott-Sheldon LAJ, Carey MP, DeMartini KS. Individual-level interventions to reduce college student drinking: A meta-analytic review. Addictive Behaviors. 2007;32:2469–2494. doi: 10.1016/j.addbeh.2007.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carey KB, Scott-Sheldon LAJ, Elliott JC, Bolles JR, Carey MP. Computer-delivered interventions to reduce college student drinking: A meta-analysis. Addiction. 2009;104:1807–1819. doi: 10.1111/j.1360-0443.2009.02691.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carney T, Myers B. Effectiveness of early interventions for substance-using adolescents: Findings from a systematic review and meta-analysis. Substance Abuse Treatment, Prevention, and Policy. 2012;7:1–28. doi: 10.1186/1747-597X-7-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Center for Substance Abuse Treatment (CSAT) Brief interventions and brief therapies for substance abuse (Treatment Improvement Protocol (TIP) Series, No. 34) Rockville, MD: Substance Abuse and Mental Health Services Administration; 1999. [PubMed] [Google Scholar]
- Cheung MW-L. metaSEM: An R package for meta-analysis using structural equation modeling. Frontiers in Psychology. 2014a;5:1521. doi: 10.3389/fpsyg.2014.01521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheung MW-L. Modeling dependent effect sizes with three-level meta-analyses: A structural equation modeling approach. Psychological Methods. 2014b;19:211–229. doi: 10.1037/a0032968. [DOI] [PubMed] [Google Scholar]
- Clark D, Winters KC. Measuring risks and outcomes in substance use disorders prevention research. Journal of Consulting and Clinical Psychology. 2002;70:1207–1223. doi: 10.1037//0022-006x.70.6.1207. [DOI] [PubMed] [Google Scholar]
- Cuijpers P, Riper H, Lemmers L. The effects on mortality of brief interventions for problem drinking: A meta-analysis. Addiction. 2004;99:839–845. doi: 10.1111/j.1360-0443.2004.00778.x. [DOI] [PubMed] [Google Scholar]
- Duval S, Tweedie R. Trim and fill: A simple funnel-plot–based method of testing and adjusting for publication bias in meta-analysis. Biometrics. 2000;56:455–463. doi: 10.1111/j.0006-341x.2000.00455.x. [DOI] [PubMed] [Google Scholar]
- Fleming MF, Mundt MP, French MT, Manwell LB, Stauffacher EA, Barry KL. Benefit-cost analysis of brief physician advice with problem drinkers in primary care settings. Medical Care. 2000;38:7–18. doi: 10.1097/00005650-200001000-00003. [DOI] [PubMed] [Google Scholar]
- Fleming MF, Mundt MP, French MT, Manwell LB, Stauffacher EA, Barry KL. Brief physician advice for problem drinkers: Long-term efficacy and benefit-cost analysis. Alcoholism: Clinical and Experimental Research. 2002;26:36–43. [PubMed] [Google Scholar]
- Hale DR, Fitzgerald-Yau N, Viner M. A systematic review of effective interventions for reducing multiple health risk behaviors in adolescence. American Journal of Public Health. 2014;104:e19–e41. doi: 10.2105/AJPH.2014.301874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heather N. Interpreting the evidence on brief interventions for excessive drinkers: The need for caution. Alcohol & Alcoholism. 1995;30:287–296. [PubMed] [Google Scholar]
- Hedges LV. Distribution theory for Glass's estimator of effect size and related estimators. Journal of Educational Statistics. 1981;6:107–128. [Google Scholar]
- Jensen CD, Cushing CC, Aylward BS, Craig JT, Sorell DM, Steele RG. Effectiveness of motivational interviewing interventions for adolescent substance use behavior change: A meta-analytic review. Journal of Consulting and Clinical Psychology. 2011;79:433–440. doi: 10.1037/a0023992. [DOI] [PubMed] [Google Scholar]
- Khan MR, Berger AT, Wells BE, Cleland CM. Longitudinal associations between adolescent alcohol use and adulthood sexual risk behavior and sexually transmitted infection in the United States: Assessment of differences by race. American Journal of Public Health. 2012;102:867–876. doi: 10.2105/AJPH.2011.300373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Konstantopoulos S. Fixed effects and variance components estimation in three-level meta-analysis. Research Synthesis Methods. 2011;2:61–76. doi: 10.1002/jrsm.35. [DOI] [PubMed] [Google Scholar]
- Lipsey MW, Wilson DB. Practical meta-analysis. Thousand Oaks, CA: Sage; 2001. [Google Scholar]
- McCambridge J, Jenkins RJ. Do brief interventions which target alcohol consumption also reduce cigarette smoking? Systematic review and meta-analysis. Drug and Alcohol Dependence. 2008;96:263–270. doi: 10.1016/j.drugalcdep.2008.03.011. [DOI] [PubMed] [Google Scholar]
- Miller WR, Rollnick S. Motivational interviewing: Preparing people to change addictive behavior. New York, NY: Guilford Press; 1991. [Google Scholar]
- Moreira MT, Smith LA, Foxcroft D. Social norms interventions to reduce alcohol misuse in university or college students. Cochrane Database of Systematic Reviews. 2009;3 doi: 10.1002/14651858.CD006748.pub2. Art. No.: CD006748. [DOI] [PubMed] [Google Scholar]
- Neighbors CJ, Barnett NP, Rohsenow DJ, Colby SM, Monti PM. Cost-effectiveness of a motivational intervention for alcohol-involved youth in a hospital emergency department. Journal of Studies on Alcohol and Drugs. 2010;71:384–394. doi: 10.15288/jsad.2010.71.384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palmer TM, Peters JL, Sutton AJ, Moreno SG. Contour-enhanced funnel plots for meta-analysis. Stata Journal. 2008;8:242–254. [Google Scholar]
- Prochaska JO, DiClemente CC. The transtheoretical approach. In: Norcross JC, Goldfried MR, editors. Handbook of psychotherapy integration, second edition. New York, NY: Oxford University Press; 2005. pp. 147–171. [Google Scholar]
- Rothstein HR, Sutton AJ, Borenstein M, editors. Publication bias in meta-analysis: Prevention, assessment and adjustments. Chichester, UK: John Wiley & Sons; 2005. [Google Scholar]
- Sánchez-Meca J, Marín-Martínez F, Chacón-Moscoso S. Effect-size indices for dichotomized outcomes in meta-analysis. Psychological Methods. 2003;8:448–467. doi: 10.1037/1082-989X.8.4.448. [DOI] [PubMed] [Google Scholar]
- Scott-Sheldon LAJ, DeMartini KS, Carey KB, Carey MP. Alcohol interventions for college students improves antecedents of behavioral change: Results from a meta-analysis of 34 randomized controlled trials. Journal of Social and Clinical Psychology. 2009;7:799–823. doi: 10.1521/jscp.2009.28.7.799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smedslund G, Berg RC, Hammerstrøm KT, Steiro A, Leiknes KA, Dahl HM, Karlsen K. Motivational interviewing for substance abuse. Cochrane Database of Systematic Reviews. 2011;5 doi: 10.1002/14651858.CD008063.pub2. Art. No.: CD008063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Somerville LH, Jones RM, Casey BJ. A time of change: Behavioral and neural correlates of adolescent sensitivity to appetitive and aversive environmental cues. Brain and Cognition. 2010;72:124. doi: 10.1016/j.bandc.2009.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Squeglia LM, Jacobus J, Tapert SF. The influence of substance use on adolescent brain development. Clinical EEG and Neuroscience. 2009;40:31–38. doi: 10.1177/155005940904000110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein MD, Hagerty CE, Herman DS, Phipps MG, Anderson BJ. A brief marijuana intervention for non-treatment-seeking young adult women. Journal of Substance Abuse Treatment. 2011;40:189–198. doi: 10.1016/j.jsat.2010.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinberg L. A dual systems model of adolescent risk-taking. Developmental Psychobiology. 2010;52:216–224. doi: 10.1002/dev.20445. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration (SAMHSA) Results from the 2012 National Survey on Drug Use and Health: Summary of national findings (NSDUH Series H-46, HHS Publication No. (SMA) 13-4795) Rockville, MD: Substance Abuse and Mental Health Services Administration; 2013. [Google Scholar]
- Substance Abuse and Mental Health Services Administration (SAMHSA) Screening, Brief Intervention, and Referral to Treatment (SBIRT) 2014 Retrieved from http://beta.samhsa.gov/sbirt.
- Tait RJ, Hulse GK. A systematic review of the effectiveness of brief interventions with substance using adolescents by type of drug. Drug and Alcohol Review. 2003;22:337–346. doi: 10.1080/0959523031000154481. [DOI] [PubMed] [Google Scholar]
- Tanner-Smith EE, Lipsey MW. Brief alcohol interventions for adolescents and young adults: A systematic review and meta-analysis. Journal of Substance Abuse Treatment. 2014 doi: 10.1016/j.jsat.2014.09.001. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van den Noortgate W, López-López JA, Marín-Martínez F, Sánchez-Meca J. Three-level meta-analysis of dependent effect sizes. Behavior Research Methods. 2013;45:576–594. doi: 10.3758/s13428-012-0261-6. [DOI] [PubMed] [Google Scholar]
- Walters ST, Lee CM, Walker DD. Brief interventions for marijuana use. In: White HR, Rabiner DL, editors. Duke series in child development and public policy: College drinking and drug use. New York, NY: Guilford Press; 2012. pp. 184–202. [Google Scholar]
- Wetherill R, Tapert SF. Adolescent brain development, substance use, psychotherapeutic change. Psychology of Addictive Behaviors. 2013;27:393–402. doi: 10.1037/a0029111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winters KC, Tanner-Smith EE, Bresani E, Myers K. Current advances in the treatment of adolescent substance use. Adolescent Health, Medicine and Therapeutics. 2014;5:199–210. doi: 10.2147/AHMT.S48053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. Global health risks: Mortality and burden of disease attributable to selected major risks. Geneva, Switzerland: World Health Organization; 2009. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.