Abstract
Promotion of healthy eating is an effective public health strategy to prevent chronic disease incidence and progression. However, food prices can impede healthy eating, especially in rural communities. The purpose of this study was to determine whether food costs are associated with nutritional quality, geographic location, and month of year. The Overall Nutritional Quality Index and cost of 92 foods were assessed four times over a 10-month period in the primary grocery stores in four Kentucky counties, two rural and two urban. Repeated measures analysis of variance was used to assess differences in food costs by nutritional quality, county, and month. Among more nutritious food items, costs were lower in urban areas. This was particularly true among foods in the highest quartile of nutritional quality. Across all counties, there was a pattern of highest per-serving costs in the second quartile of nutritional quality, whereas more nutritious foods were less expensive. Strategies that help individuals improve the ability to identify and prepare less costly foods with high nutritional value may be effective in improving dietary habits, particularly in rural, impoverished food deserts.
Keywords: nutrition, health disparities, cardiovascular disease
INTRODUCTION
The Supplemental Nutrition Assistance Program (SNAP) is a federally funded nutrition program to assist low-income individuals and families. Individual state legislatures have flexibility in determining eligibility and methods of SNAP distribution (Falk & Aussenberg, 2013). Policy advocacy aimed at improving the efficiency of SNAP should include awareness of discrepancies in food accessibility and affordability. Food cost is often a precursor to unhealthy eating because foods associated with positive health outcomes may be more expensive than foods known to contribute to chronic disease risk (Darko, Eggett, & Richards, 2013; Drewnoski, 2012). Food cost also fluctuates due to seasonal crop productivity (Plattner, Perez, & Thornsbury, 2012). Although lower cost of fruits, vegetables, and whole grains is associated with greater consumption, individuals with lower incomes often report cost as a barrier to consumption of healthy foods (Caldwell, Miller Kobayashi, DuBow, & Wytinck, 2009; Grimm, Foltz, Blanck, & Scanlon, 2012; Powell, Zhao, & Wang, 2009). Since cost can impede healthy eating, particularly in individuals receiving SNAP funding, the purpose of this study was to assess whether food cost varies by nutritional quality, season of the year, and geographic location in four Kentucky counties with varying rates of poverty and access to healthy foods.
BACKGROUND
Poor nutrition is a chronic disease risk factor that is influenced by environmental disparities (Drewnoski, 2012). Consistently eating a healthy diet is problematic in rural communities where the cost of frequent grocery store commutes to purchase highly perishable foods, such as fresh produce, can inhibit healthy eating. Several counties in Appalachia have been designated rural food deserts (i.e., low-income census tract with a poverty rate ≥20%, where ≥33% of residents reside more than 10 miles from a large grocery store) by the U.S. Department of Agriculture (Ver Ploeg et al., 2009). Many families living in these communities frequently experience food insecurity, which is defined as the state or risk of being unable to provide food for oneself or family. Food insecurity is associated with higher rates of chronic diseases, obesity, poor management of health conditions, and depression (Bengle et al., 2011; Johnson, Sharley, & Dean, 2011; Porter & Johnson, 2011). These rural counties also have high rates of unemployment and numbers of families dependent on SNAP funds to meet their nutrition needs. Currently, there is committee discussion in the Kentucky legislature regarding changes to the frequency of SNAP fund allocation from monthly to every 2 weeks (Kentucky House Republican Caucus, 2013). Although this change in SNAP fund allocation will, in theory, provide SNAP participants with more frequent opportunities to purchase healthy foods, it will also cause an additional burden to those who live more than 10 miles from a grocery store (i.e., rural food desert residents). Transportation to and from the grocery store can be a 60-mile round-trip for some of these individuals, and this legislative committee consideration is being met with mixed reactions (Lentes, 2013).
Individuals with limited financial resources often purchase highly processed foods because of the longer shelf life and less risk of waste. Processed foods, which can have the potential for addiction and increased risk of chronic illness, are sometimes less expensive than nonprocessed foods (Gearhardt, Davis, Kuschner, & Brownell, 2011; Monsivais & Rehm, 2012). Cost contributes to food insecurity, and these economic indicators further compound the inability for many residents to consistently eat a healthy diet. Food cost affects the ability to consistently eat a healthy diet. Therefore, identifying and promoting the consumption of locally available, affordable healthy foods is vital to improving health outcomes (Rehm, Monsivais, & Drewnowski, 2011).
We used the precede–proceed model as a guide to identify factors that impede healthy eating in an impoverished Kentucky county. The precede–proceed model is a planning model used to develop and implement behavioral change interventions. The precede phases of the model involve thorough assessment of factors that impede or enable lifestyle behaviors conducive to improved health. The proceed phases provide a basis for development, implementation, and evaluation of educational and ecological interventions (i.e., community education program, policy advocacy, and regulatory modifications). The model can accommodate social science and nursing theory during each phase. The educational and ecological assessment phase of the model includes identification of predisposing (i.e., attitudes and knowledge), reinforcing (i.e., rewards and other benefits), and enabling (i.e., barriers to and facilitators of behavior change) factors (Green & Kreuter, 1999). These constructs align with those of the theory of planned behavior (i.e., attitude, subjective norm, and perceived behavioral control; Ajzen, 1991).
We used the educational and ecological assessment phase of the precede–proceed model in our earlier study aimed at identifying factors that impede healthy eating in a rural Appalachian food desert. Participants identified food cost as a significant barrier to healthy eating (Hardin-Fanning, 2013). Despite the common perception that a healthy diet is cost-prohibitive in areas with high rates of poverty, there are affordable foods that contribute to a decrease in cardiovascular disease (CVD) risk (de Lorgeril & Salen, 2008; Katcher, Hill, Lanford, Yoo, & Kris-Etherton, 2009). Fresh fruits and vegetables, fish, whole grains, low- and nonfat dairy, and unsaturated fats have CVD risk–reducing properties, but in rural Appalachian food deserts, individuals often purchase canned or highly processed versions of these foods because of their longer shelf life and lower cost. Strategies to increase consumption of foods with risk-reducing properties have included community gardens, farmers’ markets, healthy corner stores, and federally funded programs aimed at increasing access to healthy foods (Karpyn, Young, & Weiss, 2012). These strategies have had mixed results and do not address the disparities in food costs experienced by individuals living in rural food deserts (Ver Ploeg et al., 2009).
A successful evidence-based nutrition assistance program in which participants’ purchases are not influenced by cost is the federally funded and regulated Women, Infants, and Children (WIC) program. Foods known to contribute to positive health outcomes in infants and children are eligible for WIC purchases using a portion-based system (i.e., participants purchase a set number of ounces or servings of dairy products, whole grains, and fresh produce each month, irrespective of the prices of those food items). The list of food items eligible for WIC funds is dynamic and based on the most current scientific recommendations (U.S. Department of Agriculture [USDA], 2014). In contrast, Kentucky’s SNAP funds are allocated at a set dollar amount each month with no consideration of the food prices in individual counties. Allocating SNAP funds using a portion-based system has the potential to increase healthy food purchases and remove some of the cost-related disparities in food accessibility. There is little research relevant to providing nutritional counseling to priority populations based on food cost. To our knowledge, there have been little to no geographic-based cost analyses that provide rationale for policy advocacy in changing SNAP funding to a portion-based system. Prior to advising individuals about healthy eating and policy makers about legislation that would increase healthy food purchases with SNAP funds, it is important for public health advocates to be aware of disparities in food costs in rural, impoverished regions in order to determine the feasibility, at individual and policy levels, of incorporating risk-reducing foods into the diet.
METHOD
Sample Food Items
This observational study was completed from September 2011 to May 2012 in four Kentucky counties. Using the USDA Market Basket guidelines (i.e., retail food items purchased by a typical U.S. family to provide a nutritious diet) to form the initial list of foods to be included, additional food items were added to this list in order to provide a full range of nutritional quality (i.e., Overall Nutritional Quality Index [ONQI]). In all, 92 foods were selected for cost assessment. We included only items that had to be restocked at least weekly due to consistent sale rates across the entire 10-month period (USDA, 2013). Sales of these items over the previous 3 months were reviewed in the grocery store located in the food desert county, and only foods available in all four counties were assessed. Only items that were restocked due to consistent sales, (i.e., not food items restocked due to food spoilage or past expiration dates) were selected for cost assessment. Prices were assessed per serving size instead of by weight or volume to represent actual consumption. Serving sizes for fruits (½ cup), vegetables (½ cup), dairy (1 cup), and grains (¾ cup or 1 slice of bread) were determined by using USDA (2011) standards. Protein servings were set at 3 ounces as recommended by the American Heart Association (2012). Food per-serving costs and nutritional quality were examined in the primary grocery stores in each county over 10 months for a total of four times. In the urban counties, the grocery store selected was similar in size and food product variety to the grocery stores in the two rural counties. All four groceries were regional or national chain stores.
Sample Counties
The study counties were purposively chosen to include a rural food desert with a high poverty rate (FD-HP), an urban county with a midrange poverty level (U-MP), and the two counties with the state’s highest (HP) and lowest (U-LP) poverty levels (Table 1). Rural–urban continuum codes were used to select counties based on urban or rural designation. The rural–urban continuum codes distinguish metropolitan counties by size and nonmetropolitan counties by degree of urbanization and proximity to metropolitan areas. Metropolitan designation has been subdivided into three categories and nonmetropolitan designation into six categories, resulting in a codification of 1 to 9, with higher numbers being associated with greater degrees of rurality (USDA, 2003).
TABLE 1.
County Demographics
| County | Population | Area (mi2) | Density (per mi2) | RUCa Code | Poverty Rate | Per Capita Income, $ | SNAP Cases/1,000 Population |
|---|---|---|---|---|---|---|---|
| FD-HP | 16,100 | 495.1 | 32.5 | 7 | 30.0 | 24,635 | 187.7 |
| U-MP | 260,512 | 284.5 | 915.6 | 2 | 17.9 | 37,254 | 69.8 |
| HP | 12,578 | 230.7 | 54.5 | 7 | 37.6 | 24,147 | 172.8 |
| U-LP | 46,178 | 189.1 | 244.0 | 1 | 5.5 | 41,816 | 26.1 |
NOTE: SNAP = Supplemental Nutrition Assistance Program; FD-HP = rural food desert with a high poverty rate; U-MP = urban county with a midrange poverty level; HP = highest poverty; U-LP = urban county with lowest poverty level.
Rural–urban continuum.
Measures
County demographic characteristics were determined using census data (National Institutes of Health, 2012; U.S. Census Bureau, 2010). The ONQI, a scoring system developed to measure the health-contributing properties of foods and beverages, was used to quantify nutritional value of foods available in all four counties (Katz et al., 2007). The index quantifies how each food contributes to or protects from disease risk based on an algorithm. Health-promoting nutrients (antioxidants, minerals, fiber, unsaturated fatty acids, carotenoids, and phenolic compounds) comprise the numerator of the index and disease-contributing nutrients (cholesterol, sodium, sugar, and saturated and trans fats) make up the denominator (American Heart Association, 2012; USDA, 2011). Scores of food items range from 1 to 100, with higher scores equating with greater concentrations of CVD risk–reducing nutrients. Food cost was determined by surveying the food items at each selected grocery store.
Procedure
The ONQI for each food was assessed a priori during an initial field observation. Cost assessments were completed seasonally during the first week of September 2011; the third week of January 2012; the second week of March 2012 and the final week of May 2012. Due to potential temporal fluctuations in food costs, we also analyzed season of the year to determine if overall food costs varied by time of year. All field observations were completed during the same week of the month across the four counties. Pricing strategies are different during each week of the month, and observations were purposely completed at different times of each month to prevent this from influencing study outcomes. Brand names/generic products and weight/servings were identical in each of the assessments. The principal investigator assessed all food prices using a printed list. Data were transcribed by both the principal investigator and a second researcher, and accuracy was confirmed by each researcher comparing the two files.
Data Analysis
Descriptive analyses were used to summarize the study data. Repeated measures analysis of variance (ANOVA) was used to assess whether month of the year or county (i.e., geographic area) or the interaction between these variables was associated with per-serving cost of the 92 items, with ONQI score included in the analysis as a covariate. The class variables of month (with four levels) and county (with four levels) were specified as within-subjects fixed effects, and food item identifier (a class variable with 92 levels) was the random effect. Post hoc comparisons for significant effects were made using Fisher’s least significant difference procedure.
Pearson’s product–moment correlation and a scat-terplot were used to investigate the relationship between cost and ONQI score for a given combination of month and location. Based on this graphical depiction of the relationship between cost and ONQI, an additional repeated measures ANOVA model was considered: This model included the fixed effects of ONQI quartile (a between-subjects effect), month of year, and county (with year and county as within-subjects effects), and the two-way interactions among these three fixed effects. As in the previous model, food item identifier was included as the random effect. Fisher’s least significant difference was used to compare categories of significant effects in a pairwise fashion. Data analyses were conducted using SAS, Version 9.3; an alpha level of .0005 was used throughout as a protection against Type I errors given multiple comparisons.
RESULTS
The initial repeated measures ANOVA model that was used to assess the variables associated with per-serving cost included the fixed class variables of month of year and county along with their interaction effect; food item identifier was class variable specified as a random effect. ONQI score was included as a continuous variable in this model. This model demonstrated significant main effects for both month of year (F3, 1365 = 10.0; p < .0001) and county (F3, 1365 = 22.9; p < .0001), although their interaction was not significant (p = .4). The effect of ONQI score on food cost was also not significant (p = .6).
Post hoc analysis of the month of year effect indicated that food cost in September (with an average of $0.40 per serving) was significantly higher compared with January, March, and May (with a mean of $0.37 per serving at each of these earlier months of the year and each post hoc comparison significant at p < .0001). The pairwise comparisons for the county effect indicated that average food cost in the food desert (County FD-HP, with a mean of $0.40 per serving) exceeded average cost in both urban counties (County U-MP and County U-LP, each of which had an average food cost of $0.36 per serving; p values for these two comparisons were < .0001) and in the county with the highest poverty (County HP with an average cost of $0.38; p value for the comparison with FD-HP was .0002). In addition, the urban county with low poverty (U-LP) had significantly lower average food cost compared with the high-poverty county (HP); the p value for this comparisons was .0003.
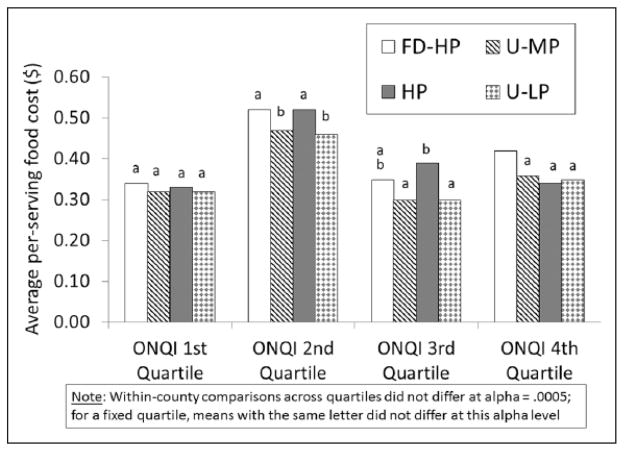
Given the unexpected lack of association between nutritional quality and cost in this model, the relationship between these two variables was investigated using correlation analysis and scatterplot graphing. For data from the month of January, the correlation between ONQI score and cost was very small within each of the counties, ranging from .019 in County HP to .084 in Count U-MP; the p values for these correlation coefficients ranged from .4 to .9. Cost versus ONQI score within each county exhibited a consistent lack of association for the other three months included in the study. Many of the food items with a per-serving cost of $1 or more have ONQI scores that are in the second quartile, namely, those foods that were between the 25th and 49th percentile in terms of nutritional quality (Figure 1). Of the 38 food items that met or exceeded the price threshold of $1 per serving, more than three quarters (76%) had ONQI scores in the second quartile range of 25 to 49.
FIGURE 1.
Food Cost/Serving by Overall Nutritional Quality Index
The typical food items within each of the quartiles defined by ONQI scores are shown in Table 2. The foods lowest in nutritional value (i.e., first quartile) include saturated fats, processed meats, and white bread, whereas those in the highest quartile of nutritional value include fresh fruits and vegetables and whole-grain brown rice. Using these quartiles of ONQI scores as indicators of nutritional value, along with month of year and county, an additional repeated measures ANOVA model was run to determine how these were related to per-serving food cost; the model also contained the three two-way interactions of these fixed effects class variables as well as the random effect of food item identifier. The significant main effects in this model were month of year (F3, 1347 = 8.1; p < .0001) and county (i.e., location of grocery store; F3, 1347 = 24.5; p < .0001). However, the latter was not interpretable given the significant interaction between quartile of nutritional value and county (F9, 1347 = 6.7; p < .0001). The other effects in the model (including the two remaining two-way interactions) were not significant at the .0005 level.
TABLE 2.
Food Categories by Overall Nutritional Quality Index Score Quartiles
| Score 1–24 | Score 25–49 | Score 50–74 | Score 75–100 |
|---|---|---|---|
| Saturated cooking fats | Processed meats | Protein cereals | Almonds |
| Canned fruits in heavy syrup | Fresh meats | Whole-grain bran cereals | Long-grain brown rice |
| Crackers | Walnuts | ||
| White rice | Raisins | ||
| High-fructose corn syrup cereals | High-fructose corn syrup cereals | Oats | Fresh fruits |
| Nut butters | Canned beans | Yogurt | Fresh vegetables |
| Canned vegetables | Breakfast bars | Low-fat dairy | Nonfat dairy |
| Processed meats | Poultry | Pecans | No sugar-added cereals |
| Dried legumes | |||
| White bread | Canned soups | ||
| Canned vegetables | |||
| Dehydrated meals | Pasta sauce | Frozen Fish | Canned fish |
| Eggs |
Post hoc comparisons for the main effect of month of year were consistent with the prior model that included nutritional value as a continuous variable. In particular, average cost in September was $0.40, compared with $0.37 for each of January, March, and May. The post hoc comparisons for September to each of the other months were significant at p < .0001, whereas pairwise comparisons among January, March, and May were not.
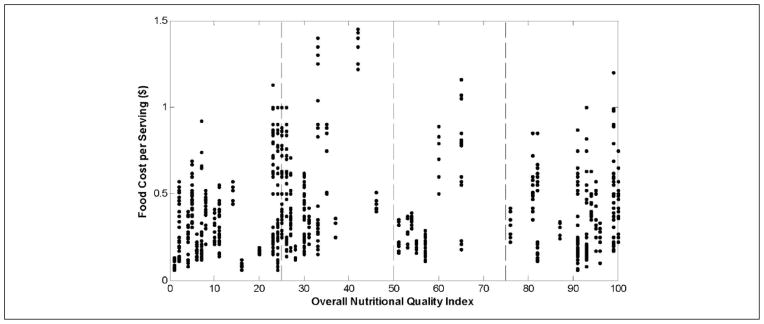
Average food costs for each combination of quartile of nutritional value (ONQI) and county are shown in Figure 2. For each of the four counties, the pairwise comparisons of cost across the four ONQI quartiles were not significant, that is, there were no significant differences in cost by nutritional value quartile within each county. As an additional protection against Type I error, the only other post hoc pairwise comparisons that were evaluated were between each pair of counties for a fixed ONQI quartile level. There were no differences among the four counties for food cost in the lowest ONQI quartile. At the second quartile of nutritional value, County FD-HP had significantly higher average cost compared with both County U-MP and County U-LP. In addition, County HP had a higher mean cost in this quartile compared with both County U-MP and County U-LP. Other comparisons within the second ONQI quartile were not significant. For foods in the third quartile of ONQI, the cost was significantly higher in County HP compared with both urban counties (U-MP and U-LP). Other comparisons within the third quartile were not significant. For food items with the highest nutritional value (fourth quartile of ONQI), the cost in County FD-HP was significantly higher than in each of the other three counties, and none of the other three (U-MP, HP, and U-LP) differed from each other on food cost in this high-quality category. These observations underscore the inequities in food cost by nutritional quality and location of grocery store; this is particularly apparent among high-quality foods, for which the per-serving cost in the food desert county is between 6 and 8 cents higher compared to the other counties included in the study.
FIGURE 2.
Means for Per-Serving Food Costs for the Interaction Effect of Quartile of Overall Nutritional Quality Index by County
DISCUSSION
The results underscore the phenomenon of higher food costs in rural impoverished counties, compared with urban counties in the same state. Although foods very low in nutritional value (i.e., first quartile of ONQI) had relatively low cost and were uniformly priced among the four counties, items with greater nutritional value (based on ONQI quartile) showed a greater cost disparity among counties. In particular, foods in the second quartile of ONQI scores, which consists largely of highly processed convenience foods, were more expensive in rural impoverished counties (whether an identified food desert or not), compared with urban counties. In addition, food items in the third quartile of ONQI scores exhibited higher costs in the rural county with the highest poverty rate, compared with the urban counties. Perhaps the most striking finding of the post hoc analysis of the significant interaction between quartile of ONQI and county was the finding that the rural food desert had significantly higher per-serving costs among the most nutritious food items, compared with any of the other three counties.
Although the cost differences among the four quartiles within each county were not statistically significant at the .0005 level, the average costs across the four quartiles demonstrate a trend toward highest cost for the second quartile, as shown in Figures 1 and 2. Particularly for the two urban counties, average costs in the top two quartiles of ONQI scores were consistent with costs of the food in the bottom quartile, whereas the highly processed convenience food in the second quartile was more expensive. These results suggest that particularly for those with greater access to grocery stores, consumption of a diet high in certain nutritious foods may be more affordable than a diet consisting of processed convenience foods. These findings are consistent with the USDA report that individuals may be able to eat healthier without incurring additional cost (Carlson, Lino, & Fungwe, 2008), though this may be more difficult for those without easy access to stores. Poor diet is a significant contributor to the disproportionately higher rates of chronic disease in rural food deserts (Kentucky Institute of Medicine, 2007). The results of this study indicate that individuals living in rural areas, particularly food deserts, may be at increased risk of negative health effects as a result of more limited access to higher quality foods compared to those living in urban areas. For those living in urban areas, purchasing more plant-based foods and fewer processed foods is an effective strategy to improve overall dietary quality without increasing food budgets (Bernstein, Bloom, Rosner, Franz, & Willett, 2010).
Current SNAP policies do not account for food cost differences between regions within each state. These discrepancies can further contribute to the inability of individuals with limited food budgets to eat healthy diets. Federal food assistance programs based on participants’ acquisition of monthly portions of food items successfully promote healthy eating, as cost is no longer the only consideration under this system. Modeling SNAP legislation after these federal programs has the potential to adequately meet all participants’ nutritional needs, irrespective of differences in food prices. The primary limitation of this study is the relatively small number of counties included. Future research with more than one county per profile type (i.e., with county profile determined by poverty and food desert status) will build on these findings and provide a more detailed look at the relationships between food availability, cost, and nutritional content. A larger study may also provide more definitive comparisons within counties across ONQI food quartiles, which may provide additional evidence that healthier foods are not necessarily more expensive.
CONCLUSIONS
Affordable foods that reduce the risk of CVD are less available in rural counties where poverty and reliance on SNAP benefits influence food buying practices. This challenge is magnified in rural food deserts. Current SNAP policy does not address food cost disparities in these counties, where rates of chronic disease prevalence, poverty, and SNAP participation are much higher than in other regions. Increasing the frequency of SNAP fund allocation will potentially add additional burden to individuals living in rural, impoverished food deserts since additional monthly trips to grocery stores will be necessary. Individuals living in remote areas of impoverished food deserts must travel up to 60 miles round-trip to the nearest grocery store. Bimonthly allocation of SNAP funds would result in additional transportation costs and further reductions in already limited food budgets. Limiting purchases of convenience and processed foods (which tended to have the highest per-serving cost) while increasing purchases of risk-reducing foods has the potential to extend monthly SNAP benefits and improve dietary nutritional quality (Stewart, Hyman, Frazao, & Carlson, 2011). However, in impoverished rural food deserts, increasing access to healthy foods is unlikely to be successful if the reality of disparate food costs is not addressed. Policy advocates and legislators must take into account region-specific disparities in food accessibility and affordability when regulating SNAP allocation. A “one-size-fits-all” approach can result in an elevated risk of food insecurity in individuals and families who are already most at risk.
Risk of food insecurity has been a reality in Appalachia for generations. Individuals who live in this region often continue traditional strategies that “stretch the food dollar.” More often than not, these strategies include preservation techniques that deplete foods of their health-promoting nutrients (e.g., canning fresh produce with sugar or salt, brining meats), which further contribute to the risk of CVD. Strategies aimed at improving dietary habits in this region must address both economic and cultural aspects of the traditional diet. The administrative, policy assessment and intervention alignment phase of the precede-proceed model provides a framework to implement educational strategies and advocate for policy regulation to improve health outcomes (Green & Kreuter, 1999).
Further research, using behavioral change theory (e.g., theory of planned behavior) is needed to determine if providing individuals with “healthy” recipes using locally available, affordable food items and helping them interpret food labels are effective strategies that may improve dietary habits in rural, impoverished regions. Within the precede–proceed model, the theory of planned behavior provides the framework to address predisposing (i.e., attitudes), reinforcing (i.e., subjective norms), and enabling (i.e., perceived behavioral control) factors that impede healthy eating at the levels of the individual and family. Strategies that address all identified factors that affect healthy eating are more likely to be successful than those based on a “one-size-fits-all” approach.
A significant barrier to healthy food accessibility in this region is geographical isolation (i.e., distance from interstate highways), which limits the degree to which food costs can be lowered. However, for many individuals, changes in SNAP policy to more closely mimic WIC may have the potential to minimize discrepancies in food accessibility due to cost. Advocacy for SNAP policy improvements requires a thorough understanding of policy development processes. Kingdon’s (1995) Policy Streams approach can assist the advocate with identification of the problem stream (i.e., food cost disparities), policy stream (i.e., proposal to improve SNAP regulations by using a portion-based allocation rather than a flat benefit amount), and politics stream (i.e., recent budget cuts to food assistance programs). When a problem is identified, a solution is proposed, and the political climate is conducive to change, a policy window (i.e., opportunity for change) opens and policy change is facilitated (Kingdon, 1995). There has been recent debate in both federal and state legislatures about the budgetary need to cut funding to food assistance programs. Policies that increase accessibility to healthy foods have the potential to improve health outcomes and subsequently decrease federal and state health care expenditures. Although bimonthly allocation of SNAP funds may result in greater transportation expense for participants, a portion-based program can provide participants the opportunity to purchase healthier foods with a longer shelf life (e.g., frozen fruits, vegetables and whole-grain products; and canned omega-3 fatty fish) at the beginning of the month, resulting in fewer monthly trips to the grocery store.
There are also several possible venues for individual and environmental strategies to improve dietary habits in rural, impoverished regions. These include collaborations with USDA Cooperative Extension Family & Consumer Science specialists to deliver educational programs aimed at helping individuals identify healthy, low-cost foods; provision of incentives for families to grow and sell produce to local grocers or via farmers markets; and community-based programs that emphasis the cost-effectiveness and positive health outcomes of consistently eating food that reduce risk of CVD. This study adds to the literature by highlighting the disparity in food cost faced by those in rural areas while also describing the trend toward highest costs among convenience foods with relatively poor nutritional value. It has been our experience that individuals living in these rural regions, which have disproportionately high morbidity and mortality rates, are eager to learn food shopping and dietary strategies that improve their health outcomes and quality of life.
Acknowledgments
This study was funded by the University of Kentucky College of Nursing. The authors wish to thank Ellen Hahn, PhD, RN, FAAN, for her assistance in the preparation of this article.
References
- Ajzen I. The theory of planned behavior. Organizational Behavior and Human Decision Processes. 1991;50:179–211. [Google Scholar]
- American Heart Association. What is a serving? 2012 Retrieved from http://www.heart.org/HEARTORG/Caregiver/Replenish/WhatisaServing/What-is-a-Serving_UCM_301838_Article.jsp.
- Bengle R, Sinnett S, Johnson T, Johnson MA, Brown A, Lee JS. Food insecurity is associated with cost-related medication non-adherence in community-dwelling, low-income older adults in Georgia. Journal of Nutrition for the Elderly. 2011;29:170–191. doi: 10.1080/01639361003772400. [DOI] [PubMed] [Google Scholar]
- Bernstein AM, Bloom DE, Rosner BA, Franz M, Willett WC. Relation of food cost to healthfulness of diet among US women. American Journal of Clinical Nutrition. 2010;92:1197–1203. doi: 10.3945/ajcn.2010.29854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caldwell EM, Miller Kobayashi M, DuBow WM, Wytinck SM. Perceived access to fruits and vegetables associated with increased consumption. Public Health Nutrition. 2009;12:1743–1750. doi: 10.1017/S1368980008004308. [DOI] [PubMed] [Google Scholar]
- Carlson A, Lino M, Fungwe T. USDA’s low-cost, moderate-cost, and liberal food plans: Development and expenditure shares. Orlando, FL: American Agricultural Economics Association; 2008. [Google Scholar]
- Darko J, Eggett DL, Richards R. Shopping behaviors of low-income families during a 1-month period of time. Journal of Nutrition Education and Behavior. 2013;45(1):20–29. doi: 10.1016/j.jneb.2012.05.016. [DOI] [PubMed] [Google Scholar]
- de Lorgeril M, Salen P. The Mediterranean diet: Rationale and evidence for its benefit. Current Atherosclerosis Reports. 2008;10:518–522. doi: 10.1007/s11883-008-0080-5. [DOI] [PubMed] [Google Scholar]
- Drewnoski A. The economics of food choice behavior: Why poverty and obesity are linked. Nestle Nutrition Institute Workshop Series. 2012;73:95–112. doi: 10.1159/000341303. [DOI] [PubMed] [Google Scholar]
- Falk G, Aussenberg RA. The Supplemental Nutrition Assistance Program: Categorical eligibility (Congressional Research Service, 7–5700. R42054) 2013 Retrieved from http://www.fas.org/sgp/crs/misc/R42054.pdf.
- Gearhardt AN, Davis C, Kuschner R, Brownell KD. The addiction potential of hyperpalatable foods. Current Drug Abuse Reviews. 2011;4:140–145. doi: 10.2174/1874473711104030140. [DOI] [PubMed] [Google Scholar]
- Green LW, Kreuter MW. Health promotion planning: An educational and ecological approach. Mountain View, CA: Mayfield; 1999. [Google Scholar]
- Grimm KA, Foltz JL, Blanck HM, Scanlon KS. Household income disparities in fruit and vegetable consumption by state and territory: Results of the 2009 Behavioral Risk Factor Surveillance System. Journal of Academy of Nutrition & Diet. 2012;112:2014–2021. doi: 10.1016/j.jand.2012.08.030. [DOI] [PubMed] [Google Scholar]
- Hardin-Fanning F. Adherence to a Mediterranean diet in a rural Appalachian food desert. Rural and Remote Health. 2013;13:2293. [PubMed] [Google Scholar]
- Johnson CM, Sharley JR, Dean WR. Indicators of material hardship and depressive symptoms among homebound older adults living in North Carolina. Journal of Nutrition in Gerontology and Geriatrics. 2011;30:154–168. doi: 10.1080/21551197.2011.566527. [DOI] [PubMed] [Google Scholar]
- Katcher HI, Hill AM, Lanford JL, Yoo JS, Kris-Etherton PM. Lifestyle approaches and dietary strategies to lower LDL-cholesterol and triglycerides and raise HDL-cholesterol. Endocrinology and Metabolism Clinics of North America. 2009;38:45–78. doi: 10.1016/j.ecl.2008.11.010. [DOI] [PubMed] [Google Scholar]
- Karpyn A, Young C, Weiss S. Reestablishing healthy food retail: Changing the landscape of food deserts. Childhood Obesity. 2012;8:28–30. doi: 10.1089/chi.2011.0113. [DOI] [PubMed] [Google Scholar]
- Katz DL, Njike VY, Kennedy D, Faridi Z, Treu J, Rhee LQ. Overall Nutritional Quality Index (Version 1 Reference Manual) Derby, CT: Yale University School of Medicine; 2007. [Google Scholar]
- Kentucky House Republican Caucus. Legislative committee discusses possible bi-monthly ration of SNAP funds. 2013 Retrieved from http://www.kentuckyhouserepublicans.org/index.cfm/article_157.htm.
- Kentucky Institute of Medicine. The health of Kentucky: A county assessment. 2007 Retrieved from http://www.healthy-ky.org/sites/default/files/The%20Health%20of%20Ky.pdf.
- Kingdon JW. Agendas, alternatives and public policies. New York, NY: Harper-Collins; 1995. [Google Scholar]
- Lentes M. Community reacts to possible change in SNAP program. 2013 Retrieved from http://www.wkyt.com/wymt/home/headlines/Community-reacts-to-possible-change-in-SNAP-program-214414381.html.
- Monsivais P, Rehm CD. Potential nutritional and economic effects of replacing juice with fruit in the diets of children in the United States. Archives of Pediatrics & Adolescent Medicine. 2012;166:459–464. doi: 10.1001/archpediatrics.2011.1599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institutes of Health. Surveillance epidemiology and end results. Rural-urban continuum codes. 2012 Retrieved from http://seer.cancer.gov/seerstat/variables/countyattribs/ruralurban.html.
- Plattner K, Perez A, Thornsbury S. Seasonal farm price patterns in selected U.S. fresh fruit markets. Poster presented at the annual meeting of Agricultural & Applied Economics Association; Seattle, Washington. 2012. Aug, Retrieved from http://ageconsearch.umn.edu/bitstream/124024/2/AAEA2012%20poster%20_Plattner_Perez_Thornsbury.pdf. [Google Scholar]
- Porter KN, Johnson MA. Obesity is more strongly associated with inappropriate eating behaviors than with mental health in older adults receiving congregate meals. Journal of Nutrition in Gerontology and Geriatrics. 2011;30:403–415. doi: 10.1080/21551197.2011.623960. [DOI] [PubMed] [Google Scholar]
- Powell LM, Zhao Z, Wang Y. Food prices and fruit and vegetable consumption among young American adults. Health Place. 2009;15:1064–1070. doi: 10.1016/j.healthplace.2009.05.002. [DOI] [PubMed] [Google Scholar]
- Rehm CD, Monsivais P, Drewnowski A. The quality and monetary value of diet consumed by adults in the United States. American Journal of Clinical Nutrition. 2011;94:1333–1339. doi: 10.3945/ajcn.111.015560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stewart H, Hyman J, Frazao EC, Carlson A. Can low-income Americans afford to satisfy MyPyramid fruit and vegetable guidelines? Journal of Nutrition Education and Behavior. 2011;43:173–179. doi: 10.1016/j.jneb.2010.08.011. [DOI] [PubMed] [Google Scholar]
- U.S. Census Bureau. Kentucky quick facts. 2010 Retrieved from http://quickfacts.census.gov/qfd/states/21000.html.
- U.S. Department of Agriculture. Economic Research Service 2003: Overview. 2003 Retrieved from http://www.ers.usda.gov/data-products/rural-urban-continuum-codes.aspx.
- U.S. Department of Agriculture. Dietary guidelines for Americans. 2011 Retrieved from http://www.health.gov/dietaryguidelines.
- U.S. Department of Agriculture. Economic Research Service 2013: Price spreads from farm to consumer. 2013 Retrieved from http://www.ers.usda.gov/data-products/price-spreads-from-farm-to-consumer.aspx.
- U.S. Department of Agriculture. Food and nutrition service—Special supplemental nutrition program for women, infants and children: Revisions in the WIC food packages. Federal Register. 2014 Mar 4;79(42) [Google Scholar]
- Ver Ploeg M, Breneman V, Farrigan T, Hamrick K, Hopkins D, Kaufman P, Tuckermanty T. Access to affordable and nutritious food—Measuring and understanding food deserts and their consequences: Report to Congress. 2009 Retrieved from http://www.ers.usda.gov/publications/ap-administrative-publication/ap-036.aspx#.VB_LXRZ8uxQ.