Abstract
Background
The relationship of missed and shortened hemodialysis (HD) to clinical outcomes has not been well characterized in HD patients in the USA. Here we explored the frequency of missed and shortened treatments and their impact on mortality and hospitalization.
Methods
A retrospective review of data from a cohort of 15 340 HD patients treated in facilities operated by Dialysis Clinics, Inc. We compared the frequency of missed and shortened treatments by gender, race, age and treatment schedules [Mondays, Wednesdays, Fridays (MWF) versus Tuesdays, Thursdays, Saturdays (TTS)].
Results
Of the 15 340 patients, 48% were non-Hispanic whites (NHWs), 41% African Americans (AAs), 6% Hispanics, 2% Native American (NA), 2% Asians and 1% other races. The median number of years on HD was 1.8 years and the median follow-up was 12.4 months. The odds of missing at least one treatment in a month were higher in: patients aged <55 years, odds ratio (OR) 1.33 (P<0.0001); in AAs, OR 1.51 (P < 0.0001); in NAs, OR 1.50 (P = 0.0003); and in Hispanics, OR 1.33 (P = 0.0003) compared with NHWs and in patients who dialyzed on TTS compared with MWF, OR 1.33 (P < 0.0001). Similar findings were observed for treatments shortened by at least 10 min per month. Missed and shortened treatments were most prevalent on Saturdays and were also associated with progressive increases in hospitalization and mortality.
Conclusion
Missed and shortened HD treatments pose a challenge to providers. Improved adherence to prescribed dialysis may decrease the morbidity and mortality.
Keywords: adherence, hospitalization, missed/shortened hemodialysis, mortality
Introduction
Although mortality among the United States (US) end-stage renal disease (ESRD) population has declined since 2000 [1], the survival of the US-ESRD population remains inferior to that of their European and Japanese cohorts [2, 3]. Partial explanations for this difference include the higher acceptance rate for US-ESRD, older age with higher co-morbidity and heterogeneity of the US-ESRD population [3]. It has been suggested that the high prevalence of missed and shortened dialysis treatment among the US-ESRD patients may be contributory [4].
Missed or shortened dialysis treatment is universal, but it is disproportionately more frequent in the US-ESRD population [4, 5]. The frequency of missed hemodialysis (HD) was 8.5% in the pooled data from the USRDS case-mix adequacy study [6] and 7.9% in the US arm of the Dialysis Outcomes and Practice Patterns Study (DOPPS), compared with 0.6% in both Europe and Japan [5]. The frequency of shortened dialysis time was also higher, 19.6 versus 9.8% and 5.7% in Europe and Japan, respectively [5].
The association between these non-adherence events and clinical outcomes has remained equivocal. Some reports had noted decreased survival [5, 6], while others did not show an association [7 –9]. Some of these studies were from single centers with small sample sizes. Our study was conducted to re-explore the frequency of missed and shortened dialysis treatments and their relationship to hospitalization and mortality in a nationally representative sample of US dialysis patients.
Materials and methods
This is a retrospective analysis of stored data from the Dialysis Clinic, Inc. (DCI) network of dialysis facilities. The cohort consisted of all prevalent chronic HD patients aged 18 years or older treated at the DCI facilities during the period of January 2007 through June 2008. Incident dialysis patients entered the cohort at 90 days post-initiation of chronic HD. All patients were followed until they transferred out of DCI, switched to peritoneal dialysis, received a renal transplant or expired.
DCI maintains a record of missed treatments and assigns the reason for the missed treatment when possible. We counted all missed HD treatments if they were not rescheduled with exceptions made for patients who failed to show up due to hospitalization or being on vacation, or were known to be receiving treatment elsewhere. In addition, treatments that could not be completed as a result of vascular access problems, equipment failures or clinical instability were not counted as shortened treatments.
In keeping with previously documented definitions [6], we defined a treatment as shortened if the length of dialysis was at least 10 min shorter than the prescribed length of dialysis or missed if a patient missed one or more HD sessions in one month.
Statistical analysis
Missed and shortened treatment rates were computed by pooling across all patient months of observation and were stratified by age, gender, race and dialysis schedule—[Mondays, Wednesdays and Fridays (MWF) versus Tuesdays, Thursdays and Saturdays (TTS)]. Race was classified into six categories: Non-Hispanic whites (NHWs); Hispanics; African Americans (AAs); Native Americans (NAs); Asians and others. Logistic regression models were computed where the outcome measure was the odds of having at least one missed (or shortened) treatment during the month. Predictor variables for the logistic regression models were age, gender, race/ethnicity, month of year and dialysis schedule. General estimating equation methods [10] were used to account for having multiple months of observation for each patient. Mortality and hospitalization rates were also computed and stratified by the number of missed (or shortened) treatments in the previous month. Rates were standardized to the marginal distribution of age for the cohort using age categories of: <45 years; 45–54 years; 55–64 years; 65–74 years; 75–84 years; and 85 years or older. Proportional hazards models were also used to model mortality and hospitalization as a function of the number of missed (or shortened) treatments in the prior month. The software SAS version 9·2 (SAS Institute, Cary, NC, USA) was utilized for all analyses. The study was approved both by the Morehouse School of Medicine Institutional Review Board and the DCI internal Review Board.
Results
The baseline demographic variables of the patients are shown in Table 1. The median age of the patients was 63 years during the study period and they were followed for an average of 12.4 months per patient. The median number of years on dialysis was 1.8 years. There were 2 297 227 HD treatments of which 55 928 (2.4%) were missed treatments and 354 510 (15.4%) were shortened treatments. DCI clinics with high rates of missed treatments showed that patients who missed a treatment were also more likely to have high rates of shortened treatments, r = 0.53, P < 0.0001.
Table 1.
Baseline demographic variables for the cohort
| n | (%) | |
|---|---|---|
| Total | 15 340 | 100.0 |
| Age Categories | ||
| <45 | 2061 | 13.4 |
| 45–54 | 2510 | 16.4 |
| 55–64 | 3530 | 23.0 |
| 65–74 | 3565 | 23.2 |
| 75–84 | 2824 | 18.4 |
| 85+ | 850 | 5.5 |
| Female | 6951 | 45.3 |
| Male | 8389 | 54.7 |
| Non-Hispanic white | 7394 | 48.2 |
| Hispanic | 920 | 6.0 |
| African American | 6274 | 40.9 |
| Native American | 288 | 1.9 |
| Asian | 297 | 1.9 |
| Other race | 159 | 1.1 |
| Diabetes | 6614 | 43.1 |
| HTN | 4188 | 27.3 |
| GN | 1652 | 10.8 |
| Other cause | 2886 | 18.8 |
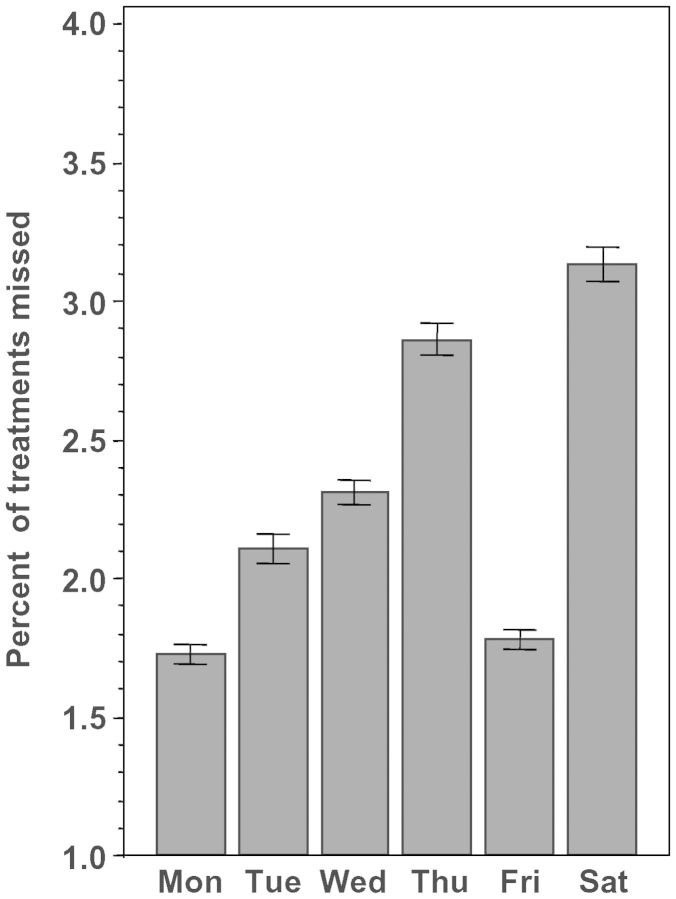
The relationship between race and frequency of missed and shortened treatments is shown in Table 2, whereas Table 3 examines the effect of the dialysis schedule on missed/shortened treatments. Compared with NHWs, these non-adherence events appear to be more common among AAs, Hispanics and NAs. Missed and shortened treatments were also more prevalent in patients who dialyze on the TTS versus the MWF schedule. When individual days of the week were compared, missed treatments were more prevalent on Saturdays, Figure 1. There was no statistical difference in age and gender distributions between the TTS and the MWF schedules.
Table 2.
Comparison of the percent of treatment missed and shortened according to race/ethnicitya
| Race/ethnicity | AA | NA | Hispanic | NHW | Asian |
|---|---|---|---|---|---|
| Missed treatments | 3.1* | 2.9* | 2.8* | 1.8 | 0.9* |
| Shortened treatments | 18.4* | 15.0* | 17.0* | 12.6 | 8.9* |
aAA, African American; NA, Native American; NHW, Non-Hispanic white.
*P< 0.0001 versus NHW.
Table 3.
Comparison of the percent of treatments missed or shortened according to the dialysis treatment schedulea
| Dialysis schedule | MWF | TTS | P-value or 95% CI |
|---|---|---|---|
| Missed treatments (%) | 2.1 | 2.9 | <0.0001 |
| Shortened treatments (%) | 14.9 | 16.4 | <0.0001 |
| Missed treatments (OR) | 1.0 (Ref) | 1.33 | 1.24–1.43 |
| Shortened treatments (OR) | 1.0 (Ref) | 1.13 | 1.08–1.18 |
aAlso shown are ORs with 95% confidence intervals for the odds of missing or shortening ≥ 1 treatment during the month.
MWF, Monday/Wednesday/Friday; TTS, Tuesday/Thursday/Saturday.
Fig. 1.
The percent of missed dialysis treatments by the day of the week; comparisons among all days of the week were significant (P < 0.0001), except Monday versus Friday (P < 0.05). The observations were similar for shortened treatments.
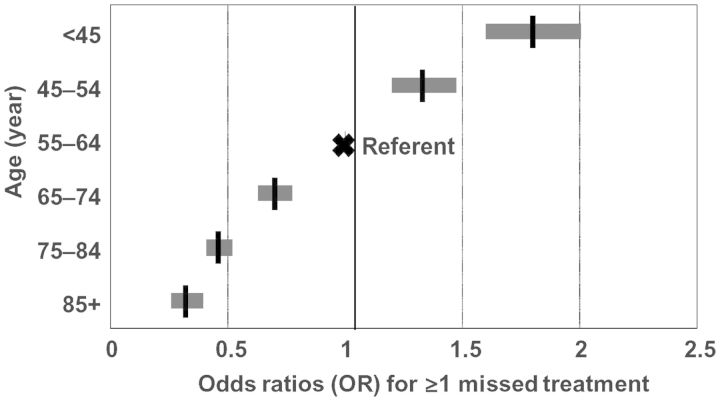
The effect of age on the rate of missed treatments is shown in Figure 2, while the effect of age on shortened treatments is shown in Table 4. Patients aged <55 years were more likely to miss or shorten their treatments.
Fig. 2.
The relationship between age categories and missed dialysis treatments; ORs and 95% CIs for ≥1 missed treatments during the month using 55–64 years as the reference age category are shown.
Table 4.
Comparison of the percent of treatments shortened according to the age categorya
| Age category | % Shortened | OR | 95% CI |
|---|---|---|---|
| <45 | 23.9 | 1.7 | 1.57–1.83 |
| 45–54 | 20.3 | 1.3 | 1.22–1–39 |
| 55–64 | 15.9 | 1.0 | Ref |
| 65–74 | 12.0 | 0.79 | 0.75–0.84 |
| 75–84 | 9.5 | 0.66 | 0.62–0.7 |
| ≥85 | 7.4 | 0.51 | 0.47–0.56 |
aAlso shown are ORs with 95% confidence intervals for the odds of shortening ≥1 treatment during the month.
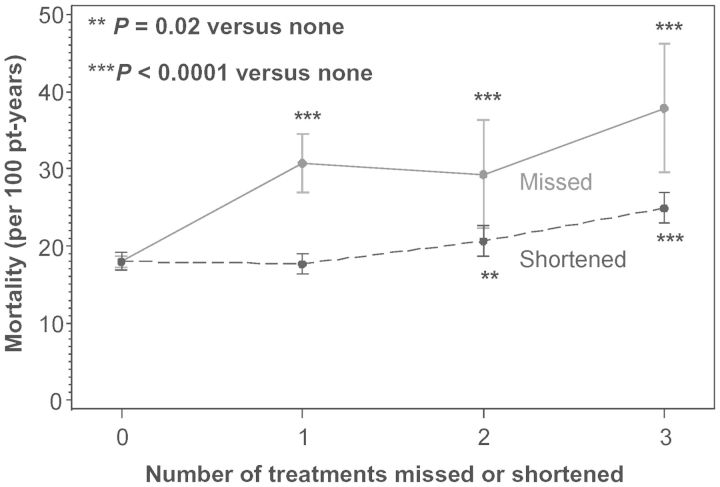
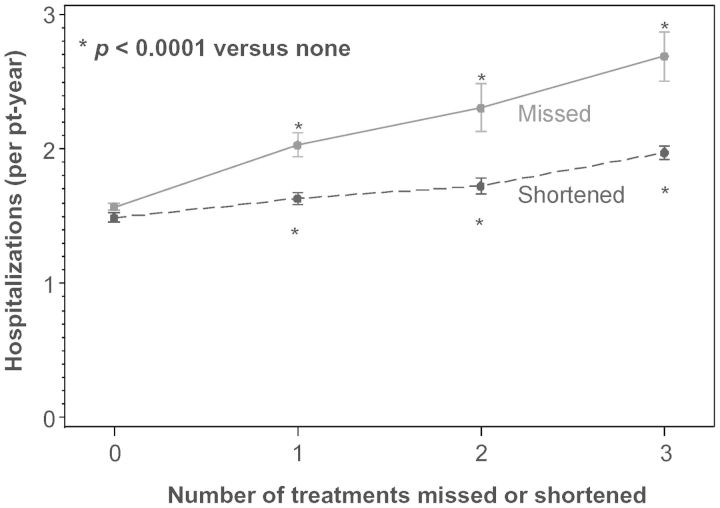
The mortality risks associated with missed or shortened treatments increase as the number of missed or shortened treatments increases (Figure 3). Similarly, the risks associated with hospitalization also increase with the number of missed or shortened treatments (Figure 4).
Fig. 3.
The escalating effects of the number of missed or shortened dialysis treatments in the previous month on age-adjusted mortality rates.
Fig. 4.
The escalating effects of the number of missed or shortened dialysis treatments in the previous month on age-adjusted hospitalization rates.
Discussion
The main observations from this study are that missed and shortened dialysis treatments are more prevalent among the minority populations (AA, Hispanic and NA patients), younger patients aged <55 years and patients who dialyze on the TTS schedule. The frequency of those two non-adherence events continues to surpass that in Europe and Japan [2, 3]. Logical explanations for these events have been lacking. It has been suggested that the size of the dialysis facility may play a role in that larger facilities may not provide optimum attention to ‘problem’ patients [5]. We are currently evaluating our data for association between facility sizes and missed or shortened treatments.
Compared with the US arm of the DOPPS [5] and the USRDS case-mix adequacy study [6], our observed rate of missed treatments at 2.4% appears to be modest. The rates were 7.9 and 8.5%, respectively, in the DOPPS and USRDS. However, our 15.4% rate of shortened treatments was comparable with the 19.6 and 20% rates, respectively, from the same earlier reports. It is not uncommon that patients who miss treatments also tend to shorten treatments. Thus, we were able to show a significant association between these events across the DCI network of dialysis units.
In a previous single-center study, we had reported a high frequency of missed dialysis on Saturdays [9]. This appears to be a nationwide phenomenon that defies logical explanations. Since non-adherence is more prevalent in younger patients, such patients may feel they are physically healthier than the older patients and thus can ‘get away’ with missed treatments [11]. It has also been suggested that a missed or shortened treatment may represent a subtle expression of control over their health status [12]. Other factors that have been associated with a high frequency of non-adherence are: smoking [5, 6, 9, 13]; use of illicit drugs and substances [9, 13]; poor adjustment to the diagnosis of ESRD and the dialysis treatment [14]; poor perception of satisfaction with the nephrologist [15]; and depression and psychosocial problems [16, 17]. The impact of psychosocial problems in ESRD has not been fully investigated. It has been reported that almost 10% of a prevalent cohort of US-HD patients were hospitalized with a psychiatric diagnosis over a 1-year observation period [18]. Our study was not designed to evaluate these issues, but ESRD providers should be cognizant of such issues. The retrospective design of this study did not allow for an accurate record of the specific reasons for the missed or shortened dialysis treatments. Many patients will often shorten their treatments because they feel poorly, have muscle cramps, have other appointments or do not want to miss their transportation. Generally, these reasons are not recorded. However, in a single-center prospective study, we utilized a direct patient questionnaire to document explanations for early termination of dialysis or skipped HD. Noted explanations include: family emergencies; transportation- or weather-related issues; feeling poorly; oversleeping; other doctor's appointment; and in a few patients, no reason at all [9].
The high frequency of non-adherence in AA and Hispanic patients has been well documented [5, 6, 9, 13, 19]. It is well known that socioeconomic status affects the incidence and prevalence of ESRD and that the ethnic minorities are disproportionately affected by both ESRD and low socioeconomic status [20, 21]. Although there is an association between low socioeconomic class and ‘cost related medication non-adherence’ [22], the effect of low socioeconomic class on dialysis adherence has not been clearly defined. Findings may vary according to patient groups and in different geographic areas [23]. Thus, the impact of sociodemographic and economic issues on poor adherence to dialysis remains unclear.
The adverse relationship between hospitalization and missed/shortened dialysis treatments is unequivocal. However, the relationship between mortality and missed/shortened treatments has not been consistent. While some reports noted a higher mortality [5, 6, 13, 24], others failed to show an association [7–9]. In this report, we have been able to demonstrate the adverse effect of missed/shortened treatments on both hospitalization and mortality. In addition, we also showed that the risks of both hospitalization and mortality increase as the number of these events increase. Cardiovascular-related causes continue to account for the majority of the mortalities among the US-ESRD population [20]. Patients who miss dialysis are more likely to have poor control of their anemia, bone mineral milieu and blood pressure, more severe electrolyte imbalance with resultant life-threatening arrhythmias and recurrent volume overload. All these factors have been well documented as risk factors for cardiovascular morbidity and mortality [25, 26, 27, 28].
The high prevalence of missed/shortened treatments among the US-ESRD population has been blamed for the high mortality rate seen among the US patients [4]. The observation that non-adherence was more prevalent among younger patients aged <55 who had lower mortality than the more adherent elderly would contradict that suggestion. However, the morbidity and mortality effects of missed/shortened dialysis cannot be overlooked. Frequent hospitalization unquestionably contributes immensely to the accelerating cost of ESRD care in the US.
Limitations of this study include the fact that it is a retrospective analysis of stored data and could not determine the specific reasons for the missed or shortened treatments. Confounding by indication is a possible explanation of the associations observed in this study. It also narrowly focused on missed/shortened treatments while other adherence issues such as interdialytic weight gains, serum phosphorus levels and medication compliance were not evaluated. The effects of these other factors on morbidity and mortality are inconsistent. It was noted that Japanese patients with excessive interdialytic weight gain had better nutrition and lower mortality [5, 29]. In the DOPPS, the Japanese had the highest rate of excessive weight gain, 34.5 versus 11% in the European and US arms of the study, respectively [5]. A recent post hoc analysis of data from the HEMO Study noted that phosphate restriction was associated with a greater mortality rate in a subgroup of HD patients [30].
In conclusion, missed and shortened dialysis treatments continue to pose challenges to providers. The frequency of missed and shortened treatments differs by race, age and dialysis schedule. New innovative ways are needed to help reduce the frequency as improved adherence to prescribed dialysis is likely to ameliorate morbidity and mortality.
Acknowledgements
This study was funded in part by Dialysis Clinics Inc., a not-for-profit corporation. We thank all DCI patients, facilities and medical directors for allowing access to their patients' records. Special thanks to Ms. Peggie Turner and Kelly Utterback for their technical support.
Conflict of interest statement. C.I.O. and P.G.Z. receive salary support via their respective institutions from DCI.
References
- 1.Collins AJ, Foley RN, Gilbertson DT, et al. The state of Chronic Kidney Disease, end stage renal disease and morbidity and mortality in the first year of dialysis. J Am Soc Nephrol. 2009;4:S5–S11. doi: 10.2215/CJN.05980809. [DOI] [PubMed] [Google Scholar]
- 2.Held PJ, Brunner F, Odaka M, et al. 5 year survival for end stage renal disease patients in the United States, Europe and Japan, 1982–1987. Am J Kidney Dis. 1990;15:451–457. doi: 10.1016/s0272-6386(12)70363-3. [DOI] [PubMed] [Google Scholar]
- 3.Goodkin DA, Bragg-Gresham JL, Koening KG, et al. Association of comorbid conditions and mortality in hemodialysis patients in Europe, Japan and United States: the Dialysis Outcomes and Practice Patterns Study (DOPPS) J Am Soc Nephrol. 2003;14:3270–3277. doi: 10.1097/01.asn.0000100127.54107.57. [DOI] [PubMed] [Google Scholar]
- 4.Bleyer A, Hylander B, Sudo H, et al. An International study of patient compliance with hemodialysis. J Am Med Assoc. 1999;281:1211–1213. doi: 10.1001/jama.281.13.1211. [DOI] [PubMed] [Google Scholar]
- 5.Saran R, Bragg-Gresham JL, Rayner HC, et al. Non-adherence in hemodialysis; associations with mortality, hospitalization, and practice patterns in the DOPPS. Kidney Int. 2003;64:254–262. doi: 10.1046/j.1523-1755.2003.00064.x. [DOI] [PubMed] [Google Scholar]
- 6.Leggat JE, Orzol SM, Hulbert-Shearon TE, et al. Non-compliance in hemodialysis: predictors and survival anelysis. Am J Kidney Dis. 1998;32:139–145. doi: 10.1053/ajkd.1998.v32.pm9669435. [DOI] [PubMed] [Google Scholar]
- 7.Ifudu O, Paul HR. Effect of missed hemodialysis treatment on mortality in patients with end stage renal disease. Nephron. 1998;79:385–386. doi: 10.1159/000045082. [DOI] [PubMed] [Google Scholar]
- 8.O'Brien ME. Compliance behavior and long-term maintenance dialysis. Am J Kidney Dis. 1990;15:209–214. doi: 10.1016/s0272-6386(12)80764-5. [DOI] [PubMed] [Google Scholar]
- 9.Obialo CI, Bashir K, Goring S, et al. “No Show” on saturdays: implications of the weekly hemodialysis schedules on non-adherence and outcomes. J. Nat Med Assoc. 2008;100:412–419. doi: 10.1016/s0027-9684(15)31274-8. [DOI] [PubMed] [Google Scholar]
- 10.Liang KY, Zeger SL. Longitudinal data analysis using generalized linear models. Biometrika. 1986;73:13–22. [Google Scholar]
- 11.De Oreo PB. Hemodialysis patient assessed functional health status predicts continued survival, hospitalization, and dialysis-attendance compliance. Am J Kidney Dis. 1997;30:204–212. doi: 10.1016/s0272-6386(97)90053-6. [DOI] [PubMed] [Google Scholar]
- 12.Kutner NG, Zhang R, McClellan WM, et al. Psychosocial predictors of non-compliance in hemodialysis and peritoneal dialysis. Nephrol Dial Transpl. 2002;17:93–99. doi: 10.1093/ndt/17.1.93. [DOI] [PubMed] [Google Scholar]
- 13.Unruh ML, Evans IV, Fink NE, et al. Skipped treatments, markers of nutritional non-adherence and survival among incident hemodialysis patients. Am J Kidney Dis. 2005;46:1107–1116. doi: 10.1053/j.ajkd.2005.09.002. [DOI] [PubMed] [Google Scholar]
- 14.Brownbridge G, Fielding DM. Psychosocial adjustment and adherence to dialysis treatment regimens. Pediatr Nephrol. 1994;8:741–749. doi: 10.1007/BF00869109. [DOI] [PubMed] [Google Scholar]
- 15.Kovac JA, Patel SS, Peterson RA, et al. Patient satisfaction with care and behavioral compliance in end-stage renal disease patients treated with hemodialysis. Am J Kidney Dis. 2002;39:1236–1244. doi: 10.1053/ajkd.2002.33397. [DOI] [PubMed] [Google Scholar]
- 16.Cukor D, Cohen SD, Peterson RA, et al. Psychosocial aspects of chronic disease: ESRD as a paradigmatic illness. J Am Soc Nephrol. 2007;18:3042–3055. doi: 10.1681/ASN.2007030345. [DOI] [PubMed] [Google Scholar]
- 17.Cukor D, Rosenthal DS, Jindal RM, et al. Depression is an important contributor to low medication adherence in hemodialysis patients and transplant recipients. Kidney Int. 2009;75:1223–1229. doi: 10.1038/ki.2009.51. [DOI] [PubMed] [Google Scholar]
- 18.Kimmel PL, Thamer M, Richard CM, et al. Psychiatric illness in patients with end-stage renal disease. Am J Med. 1998;105:214–221. doi: 10.1016/s0002-9343(98)00245-9. [DOI] [PubMed] [Google Scholar]
- 19.Tijerina MS. Mexican American Women's adherence to hemodialysis treatment: a social constructivist perspective. Soc Work. 2009;54:232–242. doi: 10.1093/sw/54.3.232. [DOI] [PubMed] [Google Scholar]
- 20.US Renal Data System. Bethesda: National Institute of Health, national Institute of Diabetes and Digestive and Kidney Diseases; 2009. USRDS 2009. Annual Data Report: Atlas of End Stage Renal Disease in the United States. [Google Scholar]
- 21.Ward MM. Socioeconomic status and the incidence of ESRD. Am J Kidney Dis. 2008;51:563–572. doi: 10.1053/j.ajkd.2007.11.023. [DOI] [PubMed] [Google Scholar]
- 22.Frankenfield DL, Howell BL, Wei II, et al. Cost-related nonadherence to prescribed medication therapy among Medicare Part D beneficiaries with end-stage renal disease. Am J Health-Syst Pharm. 2011;68:1339–1348. doi: 10.2146/ajhp100400. [DOI] [PubMed] [Google Scholar]
- 23.Kimmel PL. Psychosocial factors in adult end-stage renal disease patients treated with hemodialysis: Correlation and outcomes. Am J Kidney Dis. 2000;35(Suppl 1):S132–S140. doi: 10.1016/s0272-6386(00)70240-x. [DOI] [PubMed] [Google Scholar]
- 24.Denhaerynck K, Manhaeve D, Dobbels F, et al. Prevalence and consequences of non-adherence to hemodialysis. Am J Crit Care. 2007;16:222–235. [PubMed] [Google Scholar]
- 25.Cheung AK, Sarnak MJ, Yan G, et al. Cardiac diseases in maintenance hemodialysis patients: results of the HEMO Study. Kidney Int. 2004;65:2380–2389. doi: 10.1111/j.1523-1755.2004.00657.x. [DOI] [PubMed] [Google Scholar]
- 26.McCullough PA. Cardio-renal risk: an important clinical intersection. Rev Cardiovasc Med. 2002;3:71–76. [PubMed] [Google Scholar]
- 27.Block GA, Port FK. Re-evaluation of risks associated with hyperphosphatemia and hyperparathyroidism in dialysis patients: recommendations for a change in management. Am J Kidney Dis. 2000;35:1478–1483. doi: 10.1016/s0272-6386(00)70064-3. [DOI] [PubMed] [Google Scholar]
- 28.Obialo CI. Cardio-renal consideration as a risk factor for heart failure. Am J Cardiol. 2007;99(Suppl):21D–24D. doi: 10.1016/j.amjcard.2006.12.016. [DOI] [PubMed] [Google Scholar]
- 29.Teraoka S, Toma H, Nihei H, et al. Current Status of renal replacement therapy in Japan. Am J Kidney Dis. 1995;25:151–164. doi: 10.1016/0272-6386(95)90640-1. [DOI] [PubMed] [Google Scholar]
- 30.Lynch KE, Lynch R, Curham GC, et al. Prescribed dietary phosphate restriction and survival among hemodialysis patients. Clin J Am Soc Nephrol. 2011;6:620–629. doi: 10.2215/CJN.04620510. [DOI] [PMC free article] [PubMed] [Google Scholar]