Abstract
Background and objectives
Staphylococcus aureus (S. aureus) nasal carriage may be responsible for some serious infections in hemodialyzed patients. The main target of this study was to estimate the prevalence of S. aureus nasal carriage in hemodialysis outpatients and medical staff in hemodialysis centers specifically in Fez region. The second target is to identify the risks of colonization, resistance pattern of isolates and their virulence toxin genes.
Patients and Methods
Nasal swab specimens were obtained from 143 hemodialyzed outpatients and 32 medical staff from January to June 2012. Each participant completed a short questionnaire. Nasal carriage of S. aureus was demographically related (age, gender, hemodialysis duration), comorbidity (diabetes, malignancy) and exposure to health care (dialysis staff, hospitalization). PCR (Polymerase Chain Reaction) were used on all the isolates in the research of twelve staphylococcal enterotoxins genes. Also the PCR was used to investigate on the three factors epidermal cell differentiation inhibitors; three exfoliatin toxins; two leukotoxins; the toxic shock syndrome toxin-1 and the hemolysin beta genes.
Results
Nasal screening revealed 38.16%, 50% and 18.75% S. aureus carries in chronic, acute hemodialysis patients and medical staff, respectively. Only young participants were likely to be S. aureus carries (p = 0.002). But there were no gender differences between the isolate carriers and non-carriers or some comorbidity factors such as viral hepatitis B and C, HIV (Human Immunodeficiency Virus) infections, diabetes, chronic smoking, recent hospitalization or antibiotic therapy. Out of all isolates, only one (1.61%) was methicillin-resistant and Twenty-one (33.87%) had at least two virulence toxin genes.
Conclusions
Knowledge and monitoring of antibiotic resistance profile and virulence of S. aureus carriage are essential in the treatment of infections generated by this pathogen, as well as in the control of clonal dissemination and prevent the spread of S. aureus resistance.
Keywords: Nasal carriage, Staphylococcus aureus, hemodialysis, antimicrobial susceptibility, toxin genes
INTRODUCTION
In Morocco, the number of patients with chronic hemodialysis (CHD) treated by machine has increased sharply during the past 30 years. Each year, around 4000 new cases are reported and prevalence was estimated at 300 per million inhabitants (1). This population of patients is at high risk of infection with Staphylococcus aureus due to frequent vascular access, multiple hospital visits, immunosuppressant treatment, frequent use of antibiotics, increased strain skin colonization and central venous catheter use for vascular access (2, 3).
Nasal carriage of S. aureus in the anterior nares, present in over 42% of hemodialyzed (HD) patients, plays a major role in body expansion of this germ and consequently the HD patients infection risk (2, 4). Bacteria harboring in the nose passes to the hands and, from the hands, to the skin (5-7). From the skin, S. aureus may cause infection by any foreign substance such as a graft (introduced with venipuncture) or a dialysis catheter, either in HD patients (who mainly used fistula as their access) or peritoneal dialyzed (PD) patients. In fact, the entry into the blood in HD patients as well as to the peritoneum in PD patients may be from either touch contamination at the time of accessing the catheter, or from entry from exit site through the tunnel. On the other hand, Boelaert et al., showed that 84% of nasal S. aureus patients carried these bacteria on their hands, against only 5% of patients who did not carry it their nose (6). Even more, molecular typing revealed that strains from nares, skin and infectious sites are identical in 91% cases (4, 8).
Several factors are likely to depress the immune system of HD patients, and thus, make them more susceptible to infection. Among those factors, there is old age, concurrent debilitating illnesses, long-term stay in hospital, repeated antibiotic treatment and specific immune defects associated with renal dysfunction (9). Therefore, recognition of persons colonized or infected with S. aureus is recommended for preventing the spread of the microorganism within the hospitals or in the communities. The emergence and dissemination of methicillin-resistant S. aureus (MRSA), which is also often multidrug-resistant, renders the treatment of staphylococcal infections more challenging.
Severity of S. aureus strains is associated with the production of a wide variety of extracellular toxins and virulence factors including staphylococcal enterotoxins (SEs), like enterotoxins (SlEs), Panton-Valentine leukocidin (PVL), toxic shock syndrome toxin-1 (TSST-1), exfoliative toxin (ET), hemolysins, and coagulase (10).
The purpose of this study was firstly, to determine S. aureus nasal carriage prevalence and associated risk factors in hemodialyzed patients and medical staff of 4 hemodialysis centers of Fez city (Morocco); to define antibiotic susceptibility for all S. aureus strains identified; and finally, to define isolates toxinic gene patterns.
MATERIALS AND METHODS
Patients and study period
This cross-sectional study involved two population types: MS and HD patients (chronic and acute) in four hemodialysis centers (two private clinics, Hassan II Academic Medical Center and the Al Ghassani Provincial Hospital Center) localized in Fez city (Morocco). Patients and staff consenting were recorded between January 2012 and June 2012. All patients and staff completed a health questionnaire before undergoing nasal swab. The questionnaire included data related to the identity (name, age, sex and address), some co-morbidities factors such as viral hepatitis B (HBV), hepatitis C (HCV) and Human Immunodeficiency Virus (HIV) infections, diabetes, recent hospitalization, chronic smoking and recent antibiotic therapy or other medical history. The specific questionnaire for dialyzed patients included issues about dialysis type (acute or chronic), dialysis duration, and dialysis method which are catheter (usually femoral) or intravenous fistula.
Sampling method and bacterial identification
Samples were collected by sterile swabs. The same swab was used for both nostrils. Sampling was performed by pressing swab at least 1 cm into nostrils and spin at least three times. Sterile physiological water was used to soak swab before sampling in case of dry nose. Immediately after sampling, swabs were transported directly to the laboratory at room temperature and inoculated into Chapman medium and incubated at 37°C for 24–48 hours. Species were identified by colony morphology, Gram staining, catalase test, coagulase activity on rabbit plasma (Coagulase Plasma, Liofichem, Roseta D.A (TE) -Italy) and production of clumping factor (Slidex staph® plus, bioMérieux, France).
Antimicrobial resistance
Susceptibility to penicillin G (PG), kanamycin (K), tobramycin (Tm), gentamicin (Gm), vancomycin (VA), erythromycin (E), lincomycin (L), fusidic acid (FA), pristinamycin (PT), chloramphenicol (C), rifampicin (RF), pefloxacin (Pef), tetracycline (Te), fosfomycin (Fos), cefoxitin (Fox) and moxalactam (Mox) was determined by the standard disc diffusion technique in accordance with the guidelines of the French Society of Microbiology (11). Inhibition diameter around cefoxitin and moxalactam disks less than 27 mm and 24 mm, respectively, reflects MRSA suspicion. The MRSA were confirmed by polymerase chain reaction (PCR) detection of mecA gene. S. aureus ATCC 29213 and S. aureus ATCC 25923 were used as quality control organisms. Isolates were considered as multidrug resistant (MDR) when they were resistant to 3 or more of the antibiotics listed above.
Genomic DNA extraction
All S. aureus isolates were grown on ordinary medium agar for 18-24 hours at 37°C, bacterial cells were suspended in 500 μl of ultrapure water. Suspension was heated at 100°C for 10 min and immediately frozen at 0°C for 5 min. 300 μl of supernatant are then recovered after centrifugation of 20 000 g for 10 min. Supernatant containing DNA was stored at -20°C until further use.
nuc and mecA genes research by PCR
Duplex PCR assay was performed for the detection of the 218 bp fragment nuc gene encoding specific thermonuclease of the S. aureus and the 309 bp fragment mecA gene encoding methicillin resistance, according to protocols previously defined (12, 13).
Detection of staphylococcal toxin genes
Different multiplex PCRs were performed to detect staphylococcal enterotoxins (SE) and SE-like (SEl) genes A, B, C, D, H, K, L, M, O, P, Q, and R (sea, seb, sec, sed, seh, selk, sell, selm, selo, selp, selq, and ser), exfoliative toxins A, B, and D genes (eta, etb, and etd), TSST-1 gene (tst), leukocidins genes (lukS/F-PV and luk-M), epidermal cell differentiation inhibitor genes (edin A, B, C) and beta-hemolysin gene (hlb), as previously described (14, 15). Control chromosomal DNA samples from standard laboratory controls of Pasteur Institute (Casablanca, Morocco) were used as positive control.
Statistical analysis
Statistical study was conducted in collaboration with Fez Laboratory of Epidemiology, Clinical Research and Community Health, Hassan II Academic Medical Center, Fez. Analyzes were performed using SPSS Version 17.0 statistics (IBM, Chicago, USA). A qualitative variable analysis was performed by nonparametric tests. For quantitative variables the Student’s test (T) was used. A difference is considered statistically significant if p-value < 0.05.
RESULTS
A total of 175 nasal swabs were performed in the four hemodialysis centers conducted with 131 (74.86%) CHD, 12 (6.86%) acute hemodialyzed patients (ADH) and 32 (18.38%) in MS. Information collected from survey questionnaires allowed us to draw a summarizing table of demographic characteristics in population study (Table 1).
Table 1.
Demographics and characteristics of different study populations.
| Caracteristic (n = 175) | MS (n = 32) | AHD (n = 12) | CHD (n = 131) |
|---|---|---|---|
| Sex: | |||
| Male | 9 (28.13%) | 6 (50.00%) | 70 (53.44%) |
| Women | 23 (71.87%) | 6 (50.00%) | 61 (46.56%) |
| Age average (years) | 31.87 ± 10.36 | 40.41 ± 23.69 | 51,45 ± 14.38 |
| Diabete : | |||
| Type 1 | No | 1 (8.33%) | 11 (8.39%) |
| Type 2 | No | No | 3 (2.29%) |
| Dialysis duration average (months) | No | 1.67 ± 3.45 | 71.27 ± 52.24 |
| Catheter | No | 12 (100%) | 5 (3.81%) |
| Antibiotic treatment | 1 (3.12%) | 1 (8.33%) | 14 (10.68%) |
| Last 12 months hospitalization | No | 9 (75.00%) | 21 (16.03%) |
| Average duration hospitalization (day) | No | 8.11 ± 8.13 | 14 ± 14.16 |
| Patient shows : | |||
| HCV | No | No | 2 (1.53%) |
| HBV | No | No | 2 (1.53%) |
| HIV | No | No | 1 (0.76%) |
| Tuberculosis | No | No | 3 (2.29%) |
| Urinary tract infection | No | 1 (8.33%) | 2 (1.52%) |
| Chronic angina | No | No | 3 (2.29%) |
| Chronic smoking | No | No | 10 (7.63%) |
*MS : Medical staff, *AHD : Acute Hemodialysis, *CHD : Chronic Hemodialysis
Out of all nasal swabs, sixty-two (35.43%) isolates were identified as S. aureus. Fifty (80.64%) and six (9.68%) of theme were found in CHD and AHD patients, respectively; whereas six (9.68%) were collected from the MS personnel.
The MS personnel mean age was 29.67 ± 6 years. The S. aureus nasal carriage was 33.33% (n = 2) in man and 66.67% (n = 4) in women, the sex ratio was 0.39. The AHD patients average age was 37 ± 26.94 years. Their average hemodialysis duration was 0.94 ± 1.54 months. For men S. aureus nasal carriage was 16.67% (one patient), it’s 83.33% (five patients) for women, the sex ratio was 1. These populations were characterized by dialysis catheter carriage (usually femoral). No significant association on S. aureus carriage was observed.
We paid special attention to the CHD patients because of their greatest weaknesses (n = 131). 50 (38.16%) of them were carriers of S. aureus with the sex ratio of 1.25. No significant difference was observed in groups of patients (carriers and non-carriers S. aureus) by sex, hemodialysis duration (70.23 against 72.96 months), recent hospitalization (last 12 months), catheter harbor, smoking chronic, diabetes type 1, HIV, HCV, HBV infections and recent antibiotic therapy (p > 0.05). Regarding the age, the CHD patients were categorized into 3 classes, the first represented a relatively young population (age between 18 and 35 years), the second forming adult population (36 to 50 years) and finally the third with seniors (51 to 83 years). Comparing S. aureus carriers percentages of the three age groups, we interestingly found that the relatively young population tended to be colonized (p = 0.002), followed by the adult and old people (p > 0.05).
Review of antimicrobial susceptibility patterns in this study demonstrated that seven (11.29%) of all S. aureus isolates had presented a wild phenotype, with sensitivity to all antibiotics tested. Two and five of them were isolated from AHD and CHD patients, respectively. Bacterial strains expressed a high level of sensitivity to macrolides and related antibiotics, aminoglycosides, pefloxacin, chloramphenicol, fosfomycine and glycopeptides (vancomycin) (Table 2). However, 16.13% of our strains showed resistance to tetracycline and 4.83% of them were resistant to rifampicin and fusidic acid. Interestingly, only one strain (1.64%) expressed an inhibition less than 27 mm and 24 mm around cefoxitin and moxalactam disks, respectively. It was confirmed as MRSA.
Table 2.
Resistance pattern of 62 S. aureus strains.
| Resistance pattern | Strain number | Origin isolates (CHD) / (AHD) / (MS) |
||
|---|---|---|---|---|
| Wild | 7 | 5 | 2 | 0 |
| P | 43 | 34 | 4 | 5 |
| P-RA | 2 | 1 | 0 | 1 |
| P-TE | 3 | 3 | 0 | 0 |
| FA-TE | 1 | 1 | 0 | 0 |
| P-C-TE | 2 | 2 | 0 | 0 |
| PEF-FA-TE | 1 | 1 | 0 | 0 |
| L-E-PEF-TE | 1 | 1 | 0 | 0 |
| K-FA-TE-RA | 1 | 1 | 0 | 0 |
| P-TE-FOX-MOX | 1 | 1 | 0 | 0 |
P: Penicillin G, K: Kanamycin, TM: Tobramycin, TE: Tétracycline, E: Erythromycin, L: Lincomycin, C: Chloramphenicol, PEF: Pefloxacin, FOX: Cefoxitin, FA: Fusidique acid, RA: Rifampicin, MOX: Moxalactam.
AHD: Acute Hemodialysis, CHD: Chronic Hemodialysis, MS: Medical Staff.
In this work, the resistance to penicillin G was the dominant pattern phenotype (69.35%). Only six strains classified as multidrug resistant (MDR). These strains showed resistance to at least 3 antibiotics (Table 2) and contained selm, selo, sed, selr, lukM. We observed that the strains from AHD patients showed only “penicillin” (4/6) phenotype or wild type (2/6). Unlike in the CHD patient strains, the resistant rate is rather high with varying resistance patterns. All MDR strains were isolated from chronic hemodialyzed patients. Virulence genes study revealed sixteen toxin genes (sea, seb, sec, sed, seh, ser, selk, sell, selm, selo, etd, hlb, tst, edinABC, lukM, luk-PV) distributed in different profiles between strains isolated (Table 3).
Table 3.
Toxinic gene pattern of nasal carriage S. aureus strains in hemodialyzed patients.
| Toxinic gene Pattern | Strains number (N = 62) |
|---|---|
| (Wild) | (9) |
| (selo) | (3) |
| (selo-selm) / (selo-sell) / (selo-tst) / (selo-seh) / (selo-selk) /(selo-lukPV) / (selm-hlb) / (sell-seh) / (seh-hlb) | (12) / (1) / (2) / (1) / (1) /(1) / (1) / (1) / (1) |
| (selo-selm-sec) / (selo-selm-tst) / (selo-selm-lukM) / (selo-sell-sec) / (selo-seh-tst) / (selo-sed-ser) / (selm-selk- tst) / (lukPV-tst-edinABC) | (2) / (2) / (1) / (1) /(2) / (2) / (1) / (1) |
| (selo-selm-sell-sec) / (selo-selm-sed-ser) / (selo-sell-seh-sec) / (selo-selk-seh-seb) | (7) / (2) / (1) /(1) |
| (selo-selm-sell-sec-hlb) / (selo-selm-sed-ser-lukM) / (selo-selm-sec-etd-sea) | (2) / (2) /(1) |
| (selo-selm-selk-sea-tst-ser) | (1) |
Among these genes, we have nine tst genes (two in AHD and seven in CHD S. aureus isolates) and two luk-PV genes (one for each of AHD and CHD S. aureus isolate). In addition, 80.6% of strains (all populations combined) contained at least two toxin genes.
MDR isolates in this study harbored at least three toxin genes. Gene frequency was dispersed, the most frequent were selo gene with 72.6% (45 strains), followed by selm (n = 37, 60%) (Fig 1). It’s interesting to note that none of the isolates undertaken in this study had any of eta, etb and etd genes.
Fig1.
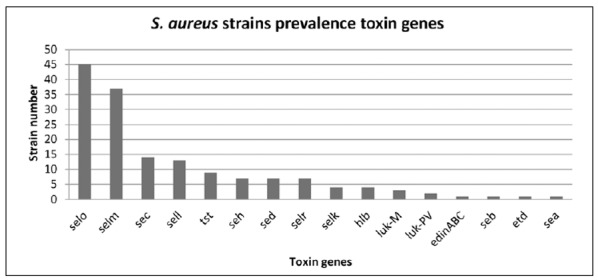
toxin genes Prevalence of S. aureus stains isolated in the population study.
DISCUSSION
S. aureus nasal carriage plays an important role in epidemiology and pathogenesis in chronic hemodialyzed patient infections, especially in patients requiring vascular access for prolonged periods. A causal relation between S. aureus nasal carriage and infection is supported by the fact that the nasal S aureus strain and the infecting strain share the same phage type or genotype (3, 16). These staphylococcal infections present a serious clinical problem in the routine management of hemodialyzed patients. That is why, a greater understanding of S. aureus colonization prevalence and microbiology is essential to guide efforts in reducing antibiotic resistant strains spread. Furthermore, nasal application of an antistaphylococcal drug temporarily decolonizes the nose and other body sites, which prevents infection (17).
The rate of S. aureus nasal carriage in this study was 35.43% (whole study population combined). It is 38.16%, 50.0% and 18.75% in CHD, AHD and MS patients, respectively. Nevertheless, the chronic or acute hemodialysis S. aureus carriage is quite high compared to medical personnel. This tells us that the hemodialysis incriminating factor is responsible in increasing of S. aureus carriage, as previously confirmed by Nouwen et al., (18). Moreover, since the manpower of the CHD patients is more important, we have focused our work on this population. The rate of 38.16% in this study is comparable to other reported range (19). However, in previous reports, the S. aureus nasal carriage prevalence rate among patients receiving hemodialysis was relatively lower, between 11.25% and 31.4% (20-22) and the rate was between 44.0% and 84.0% in others studies (23-26). One explanation for this variability may be that factors in the host, such as nutritional status, HLA (human leukocyte antigen) system, race, sex, age, hormonal factors, anatomical alterations, bactericidal activity of nasal secretions, epithelial cells receptors and/or local immunity associated with IgA predispose some patients to be S. aureus nasal carriage. Other reasons may be related to bacteria and/or environment (27, 28).
In this work, no significant correlation was found regarding the nasal carriage of S. aureus and hemodialysis duration, diabetes, sex and recent hospitalization in patients on hemodialysis (p > 0.05). Publications differ on this issue; some authors have not found diabetes or hemodialysis duration as a risk factor (19-23) while others have found it as a risk factor (29). No additional significant risk factor was identified, either, among patients expressed HIV, HBV or HCV infections, or smoking patients or dialyzed with urinary disorders. Though, most recently Alexander et al., confirms an increased risk on S. aureus carriage with these factors (30). We can explain this result by the no representative patient number with these risk factors.
In our study, the young patients had a higher risk for S. aureus carriage (p = 0.002). Whereas, Saxena and coworkers (31) found a significant correlation between old age and nasal carrier state, they established that patients aged 75 to 84 years had the highest (84.6%) prevalence of S. aureus nasal carriage. Those aged 65 to 74 years had the next highest (49.0%) nasal carriage rates while patients aged 15 to 24 years had the lowest (12.8%) prevalence of nasal carriage.
Moreover, this study provides important data on current antimicrobial resistance, including methicillin-resistance. Resistance to tetracycline, widely used in Morocco, was found in ten HDC strains (16.13%). This rate remains very lower than one study reported in Poland (21). Nevertheless, four antibiotics (chloramphenicol, rifampicin, fusidic acid and pefloxacine) also actively used in Morocco, are more or less active (with 96%, 95.16%; 95.16% and 77% of sensitivity, respectively). All resistant strains have been developed in HDC patients except one person medical staff wearing a S. aureus resistant to rifampicin and penicillin. Such rates of resistance were lacking in most African countries (32, 33). We speculate that many factors may have contributed to the emergence of these resistances in Morocco, namely the self medication, the low costs, and availability of antibiotics without a prescription.
Throughout our study, particular attention has been focused for MRSA research. Methicillin resistance in staphylococci is conferred by the mecA gene, which is easily transferred horizontally and encodes for an altered penicillin-binding protein (PBP2a) that has a low binding affinity for all β-lactam antibiotics. One interesting finding to note was the high sensitivity rate (98.39%) of HD nasal carriage S. aureus to cefoxitin (MRSA) despite the worldwide reports of its high resistant rate to this drug (19, 23, 34). Our MRSA strain presented simultaneous resistance to only penicillin and tetracycline; it was isolated from a men chronic hemodialysis patient, tuberculosis, aged 32 years. He had not been hospitalized in the twelve months preceding organism isolation. The strain resistance pattern (P-TE-FOX) was very different from those reported in hospital-acquired (HA) or community-acquired (CA) MRSA. CA-MRSA resistance is usually limited to β-lactams, and the strains remain susceptible to clindamycin, gentamicin, sulfamethoxazole-trimethoprim, vancomycin, rifampin, tetracycline, and linezolid compared with HA-MRSA isolates (35-37). Moreover, our strain does not possess luk-PV neither epidermolysin genes which are often associated with CA-MRSA (36, 38).
Besides the antibiotics resistance of S. aureus, it can be surprising how this bacterium is also armed to annihilate many defenses that his host could oppose him. In the current work, in agreement with Holtfreter and his teammates (14) selo and selm genes were more frequently detected in all isolates. Both genes belong to the recently described enterotoxin gene cluster (egc) that harbours 5 to 6 genes (seg, sei, selm, seln, selo, and sometimes selu), which cluster on a staphylococcal pathogenicity island type I γSaβ.(10, 39) this cluster will be found without all of the egc components (40, 41).
The tst gene is carried by a family of closely related pathogenicity islands that interact in highly specific way with certain staphylococcal phages. Most often associated with sec, sell, selq or selk genes (14), this gene encoding for TSST-1, was found in 14.5% of all isolates. Secreted toxin responsible of staphylococcal toxic shock syndrome can cause, on body spread, fever higher than 39°C, hypotension and generalized scarlatiniform, erythroderma followed by 7 until 14 days later by intense scaling and a multi-organs damage.
The gene encoding Panton-Valentine leukocidin (PVL) was present in two (3.22%) S. aureus isolates. PVL is cytotoxic to human polymorphonuclear cells, monocytes, macrophages and erythrocytes (42). It is also strongly associated with skin infections, such as furuncles, but also osteomyelitis (43) and necrotizing pneumonia mainly (44).
With low resistance rate to antibiotics tested, strains harboring these two toxin genes (tst and luk-PV) are not a direct danger to patients who wear them. But acquisition of any resistance antibiotic makes these strains a potential danger against hemodialyzed patients.
Another strain isolated from a female patient 66 old years, carries sec, sea, seh and sell genes. In literature, we find that sec and sell genes are localized with tst gene on pathogenicity islet of island SaPIm1/SaPIn1 family (10, 14). The most plausible explanation we can move forward to account for this pattern is that strain has probably kept genetic element (SaPIm1/SaPIn1) but lost the tst gene.
Regarding lukM gene, a leukocidin synergohymenotrope activity, was isolated from three strains. However, in literature, lukM gene is bovine native and is carried by mobile genetic element (45). Its presence in CHD patient strains may be due to contact with bovine, thus inducing a transfer of bovine strains to humans, or simply a mobile genetic element transfer from bovine strains to human strains, and by several other mechanisms lukM positive strains were colonizing our three dialyzed patients.
Conclusion
On the basis of all these data and investigation, and taking account hemodialysis as a major risk factor in S. aureus nasal colonization, only subtle balance between host defenses “immunocompetent” and S. aureus ability to express virulence factors, depending on environmental conditions, which will determine success or eradication infection.
These studies can therefore open way for prophylaxis or antibacterial therapy adapted according to each patient status. Thus, screening will allow to implement individual and collective hygiene directives, as well as clinical monitoring and S. aureus nasal carriage bacteriological in long-term in hemodialysis units.
Finally, multidrug resistance is not itself additional virulence factor in S. aureus. But infections associated with these strains exhibit frequently significant gravity related to environment, inefficiency to probabilistic treatment or initial therapeutic choice often restricted. In this way, S. aureus multi-resistant and multi-virulent lethality is significantly higher than identical wild germs infections.
Knowledge and monitoring of S. aureus sensitivity and virulence pattern are essential in the treatment of infections generated by this specie of bacteria, as well as control of clonal dissemination. Each hemodialysis center must make a periodic assessment of S. aureus antibiotics sensitivity currently used.
References
- 1. [January 10, 2012];Registre de l’Insuffisance Rénale Chronique Terminale. N°1. 2004 Available from: http://nephro-maroc.org/pages/static/morrocanNephrology/magredial.
- 2.Wertheim HF, Melles DC, Vos MC, van Leeuwen W, van Belkum A, Verbrugh HA, Nouwen JL. The role of nasal carriage in Staphylococcus aureus infections. Lancet Infect Dis. 2005;5:751–762. doi: 10.1016/S1473-3099(05)70295-4. [DOI] [PubMed] [Google Scholar]
- 3.von Eiff C, Becker K, Machka K, Stammer H, Peters G. Nasal carriage as a source of Staphylococcus aureus bacteremia. Study Group. New Engl J Med. 2001;344:11–16. doi: 10.1056/NEJM200101043440102. [DOI] [PubMed] [Google Scholar]
- 4.Vandecasteele SJ, Boelaert JR, De Vriese AS. Staphylococcus aureus infections in hemodialysis: what a nephrologist should know. Clin J Am Soc Nephrol. 2009;4:1388–1400. doi: 10.2215/CJN.01590309. [DOI] [PubMed] [Google Scholar]
- 5.Doebbeling BN. Nasal and hand carriage of Staphylococcus aureus in healthcare workers. J Chemother. 1994;6(Suppl 2):11–17. [PubMed] [Google Scholar]
- 6.Boelaert JR, Van Landuyt HW, Gordts BZ, De Baere YA, Messer SA, Herwaldt LA. Nasal and cutaneous carriage of Staphylococcus aureus in hemodialysis patients: the effect of nasal mupirocin. Infect Control Hosp Epidemiol. 1996;17:809–811. doi: 10.1086/647241. [DOI] [PubMed] [Google Scholar]
- 7.Goldblum SE, Ulrich JA, Goldman RS, Reed WP. Nasal and cutaneous flora among emodialysis patients and personnel: quantitative and qualitative characterization and patterns of Staphylococcal carriage. Am J Kidney Dis. 2:281–286. doi: 10.1016/s0272-6386(82)80075-9. [DOI] [PubMed] [Google Scholar]
- 8.Ena J, Boelaert JR, Boyken LD, Van Landuyt HW, Godard CA, Herwaldt LA. Epidemiology of Staphylococcus aureus infections in patients on hemodialysis. Infect Control Hosp Epidemiol. 1994;15:78–81. doi: 10.1086/646865. [DOI] [PubMed] [Google Scholar]
- 9.Koziol-Montewka M, Chudnicka A, Ksiazek A, Majdan M. Rate of Staphylococcus aureus nasal carriage in immunocompromised patients receiving haemodialysis treatment. Int J Antimicrob Agents. 2001;18:193–196. doi: 10.1016/s0924-8579(01)00350-8. [DOI] [PubMed] [Google Scholar]
- 10.D L, Omoe K, Inoue F, Kasai T, Yasujima M, Shinagawa K, Nakane A. Comparative prevalence of superantigenic toxin genes in meticillin-resistant and meticillin-susceptible Staphylococcus aureus isolates. J Med Microbiol. 2008;57(Pt 9):110–1112. doi: 10.1099/jmm.0.2008/002790-0. [DOI] [PubMed] [Google Scholar]
- 11.CA-SFM. Recommandations du Comite d’Antibiogramme de la Société Française de Microbiologie. 2011 http://www.sfm.asso.fr/
- 12.Brakstad OG, Aasbakk K, Maeland JA. Detection of Staphylococcus aureus by polymerase chain reaction amplification of the nuc gene. J Clin Microbiol. 1992;30:1654–1660. doi: 10.1128/jcm.30.7.1654-1660.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Vannuffel P, Gigi J, Ezzedine H, Vandercam B, Delmee M, Wauters G, Gala JL. Specific detection of methicillin-resistant Staphylococcus species by multiplex PCR. J Clin Microbiol. 1995;33:2864–2867. doi: 10.1128/jcm.33.11.2864-2867.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Holtfreter S, Grumann D, Schmudde M, Nguyen HT, Eichler P, Strommenger B, et al. Clonal distribution of superantigen genes in clinical Staphylococcus aureus isolates. Clin Microbiol. 2007;45(8):2669–2680. doi: 10.1128/JCM.00204-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jarraud S, Mougel C, Thioulouse J, Lina G, Meugnier H, Forey F, et al. Relationships between Staphylococcus aureus genetic background, virulence factors, agr groups (alleles), and human disease. Infect Immun. 2002;70:631–641. doi: 10.1128/IAI.70.2.631-641.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Valentine FC, Hall-Smith SP. Superficial staphylococcal infection. Lancet. 1952;2(6730):351–354. doi: 10.1016/s0140-6736(52)92245-9. [DOI] [PubMed] [Google Scholar]
- 17.Kluytmans JA, Wertheim HF. Nasal carriage of Staphylococcus aureus and prevention of nosocomial infections. Infection. 2005;33:3–8. doi: 10.1007/s15010-005-4012-9. [DOI] [PubMed] [Google Scholar]
- 18.Nouwen JL, Ott A, Kluytmans-Vandenbergh MF, Boelens HA, Hofman A, van Belkum A, et al. HA. Predicting the Staphylococcus aureus nasal carrier state: derivation and validation of a “culture rule”. Clin Infect Dis. 2004;39:806–811. doi: 10.1086/423376. [DOI] [PubMed] [Google Scholar]
- 19.Ghasemian R, Najafi N, Makhlough A, Khademloo M. Frequency of nasal carriage of Staphylococcus aureus and its antimicrobial resistance pattern in patients on hemodialysis. Iran J Kidney Dis. 2010;4:218–222. [PubMed] [Google Scholar]
- 20.Ternois I, Geffroy S, Brun Y, Lemeland JF, Etienne I, Fleurette J, et al. Evaluation of the carriage of Staphylococcus aureus in patients and the personnel of a hemodialysis center for the prevention of infections. Pathologie-biologie. 1993;41:428–433. [PubMed] [Google Scholar]
- 21.Koziol-Montewka M, Szczepanik A, Baranowicz I, Jozwiak L, Ksiazek A, Kaczor D. The investigation of Staphylococcus aureus and coagulase-negative staphylococci nasal carriage among patients undergoing haemodialysis. Microbiol Res. 2006;161:281–287. doi: 10.1016/j.micres.2005.10.002. [DOI] [PubMed] [Google Scholar]
- 22.Montagnac R, Eloy C, Schillinger F, Croix JC, Milcent T. Repeated studies of the prevalence of Staphylococcus aureus in the nasal cavity in hemodialysed patients. Presse Med. 1995;24:1075–1077. [PubMed] [Google Scholar]
- 23.Souly K, Ait el kadi M, Lahmadi K, Biougnach H, Boughaidi A, Zouhdi M, et al. Epidemiology and prevention of Staphylococcus aureus nasal carriage in hemodialyzed patients. Med Mal Infect. 2011;41:469–474. doi: 10.1016/j.medmal.2011.05.005. [DOI] [PubMed] [Google Scholar]
- 24.Yu VL, Goetz A, Wagener M, Smith PB, Rihs JD, Hanchett J, et al. Staphylococcus aureus nasal carriage and infection in patients on hemodialysis. Efficacy of antibiotic prophylaxis. N Engl J Med. 1986;315:91–96. doi: 10.1056/NEJM198607103150204. [DOI] [PubMed] [Google Scholar]
- 25.Kaplowitz LG, Comstock JA, Landwehr DM, Dalton HP, Mayhall CG. Prospective study of microbial colonization of the nose and skin and infection of the vascular access site in hemodialysis patients. J Clin Microbiol. 1988;26:1257–1262. doi: 10.1128/jcm.26.7.1257-1262.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pena C, Fernandez-Sabe N, Dominguez MA, Pujol M, Martinez-Castelao A, Ayats J, et al. Staphylococcus aureus nasal carriage in patients on haemodialysis: role of cutaneous colonization. J Hosp Infect. 2004;58:20–27. doi: 10.1016/j.jhin.2004.04.018. [DOI] [PubMed] [Google Scholar]
- 27.Peacock SJ, Mandal S, Bowler IC. Preventing Staphylococcus aureus infection in the renal unit. QJM. 2002;95:405–410. doi: 10.1093/qjmed/95.6.405. [DOI] [PubMed] [Google Scholar]
- 28.Weidenmaier C, Kokai-Kun JF, Kristian SA, Chanturiya T, Kalbacher H, Gross M, et al. Role of teichoic acids in Staphylococcus aureus nasal colonization, a major risk factor in nosocomial infections. Nat Med. 2004;10:243–245. doi: 10.1038/nm991. [DOI] [PubMed] [Google Scholar]
- 29.Watanakunakorn C, Brandt J, Durkin P, Santore S, Bota B, Stahl CJ. The efficacy of mupirocin ointment and chlorhexidine body scrubs in the eradication of nasal carriage of Staphylococcus aureus among patients undergoing long-term hemodialysis. Am J Infect Control. 1992;20:138–141. doi: 10.1016/s0196-6553(05)80180-4. [DOI] [PubMed] [Google Scholar]
- 30.Alexander EL, Morgan DJ, Kesh S, Weisenberg SA, Zaleskas JM, Kaltsas A, et al. Prevalence, persistence, and microbiology of Staphylococcus aureus nasal carriage among hemodialysis outpatients at a major New York Hospital. Diagn Microbiol Infect Dis. 2011;70:37–44. doi: 10.1016/j.diagmicrobio.2010.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Saxena AK, Panhotra BR, Chopra R. Advancing age and the risk of nasal carriage of Staphylococcus aureus among patients on long-term hospital-based hemodialysis. Ann Saudi Med. 2004;24:337–342. doi: 10.5144/0256-4947.2004.337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Randrianirina F, Soares JL, Ratsima E, Carod JF, Combe P, Grosjean P, et al. In vitro activities of 18 antimicrobial agents against Staphylococcus aureus isolates from the Institut Pasteur of Madagascar. Ann Clin Microbiol Antimicrob. 2007;6:5. doi: 10.1186/1476-0711-6-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kesah C, Ben Redjeb S, Odugbemi TO, Boye CS, Dosso M, Ndinya Achola JO, et al. Prevalence of methicillin-resistant Staphylococcus aureus in eight African hospitals and Malta. Clin Microbiol Infect. 2003;9:153–156. doi: 10.1046/j.1469-0691.2003.00531.x. [DOI] [PubMed] [Google Scholar]
- 34.Lederer SR, Riedelsdorf G, Schiffl H. Nasal carriage of meticillin resistant Staphylococcus aureus: the prevalence, patients at risk and the effect of elimination on outcomes among outclinic haemodialysis patients. Eur J Med Res. 2007;12:284–288. [PubMed] [Google Scholar]
- 35.Fridkin SK, Hageman JC, Morrison M, Sanza LT, Como-Sabetti K, Jernigan JA, et al. Methicillin-resistant Staphylococcus aureus disease in three communities. N Engl J Med. 2005;352:1436–1444. doi: 10.1056/NEJMoa043252. [DOI] [PubMed] [Google Scholar]
- 36.Vandenesch F, Naimi T, Enright MC, Lina G, Nimmo GR, Heffernan H, et al. Community-acquired methicillin-resistant Staphylococcus aureus carrying Panton- Valentine leukocidin genes: worldwide emergence. Emerg Infect Dis. 2003;9:978–984. doi: 10.3201/eid0908.030089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Delorme T, Rose S, Senita J, Callahan C, Nasr P. Epidemiology and susceptibilities of methicillin-resistant Staphylococcus aureus in Northeastern Ohio. Am J Clin Pathol. 2009;132(5):668–677. doi: 10.1309/AJCPQ46ZPQXVHHNC. [DOI] [PubMed] [Google Scholar]
- 38.Nour M, Mastouri M, Ben Nejma M. Methicillin resistance in Staphylococcus aureus: emergence and molecular basis. Pathologie-biologie. 2005;53:334–340. doi: 10.1016/j.patbio.2004.08.001. [DOI] [PubMed] [Google Scholar]
- 39.Letertre C, Perelle S, Dilasser F, Fach P. Identification of a new putative enterotoxin SEU encoded by the egc cluster of Staphylococcus aureus. J Appl Microbiol. 2003;95:38–43. doi: 10.1046/j.1365-2672.2003.01957.x. [DOI] [PubMed] [Google Scholar]
- 40.Chiang YC, Liao WW, Fan CM, Pai WY, Chiou CS, Tsen HY. PCR detection of Staphylococcal enterotoxins (SEs) N, O, P, Q, R, U, and survey of SE types in Staphylococcus aureus isolates from food-poisoning cases in Taiwan. Int J Food Microbiol. 2008;121:66–73. doi: 10.1016/j.ijfoodmicro.2007.10.005. [DOI] [PubMed] [Google Scholar]
- 41.Hwang SY, Kim SH, Jang EJ, Kwon NH, Park YK, Koo HC, et al. Novel multiplex PCR for the detection of the Staphylococcus aureus superantigen and its application to raw meat isolates in Korea. Int J Food Microbiol. 2007;117:99–105. doi: 10.1016/j.ijfoodmicro.2007.02.013. [DOI] [PubMed] [Google Scholar]
- 42.Gladstone GP, Van Heyningen WE. Staphylococcal leucocidins. Br J Exp Pathol. 1957;38:123–137. [PMC free article] [PubMed] [Google Scholar]
- 43.Gillet Y, Dohin B, Dumitrescu O, Lina G, Vandenesch F, Etienne J, Floret D. Osteoarticular infections with staphylococcus aureus secreting Panton-Valentine leucocidin. Arch Pediatr. 2007;14(Suppl 2):S102–107. doi: 10.1016/s0929-693x(07)80043-1. [DOI] [PubMed] [Google Scholar]
- 44.Diep BA, Palazzolo-Ballance AM, Tattevin P, Basuino L, Braughton KR, Whitney AR, et al. Contribution of Panton-Valentine leukocidin in community-associated methicillin-r esistant Staphylococcus aureus pathogenesis. PloS one. 2008;3:e3198. doi: 10.1371/journal.pone.0003198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kaneko J, Muramoto K, Kamio Y. Gene of LukF-PV-like component of Panton-Valentine leukocidin in Staphylococcus aureus P83 is linked with lukM. Biosci Biotechnol Biochem. 1997;61:541–544. doi: 10.1271/bbb.61.541. [DOI] [PubMed] [Google Scholar]


